Household Composition and Inequalities in COVID-19 Vaccination in Wales, UK
Abstract
1. Introduction
2. Materials and Methods
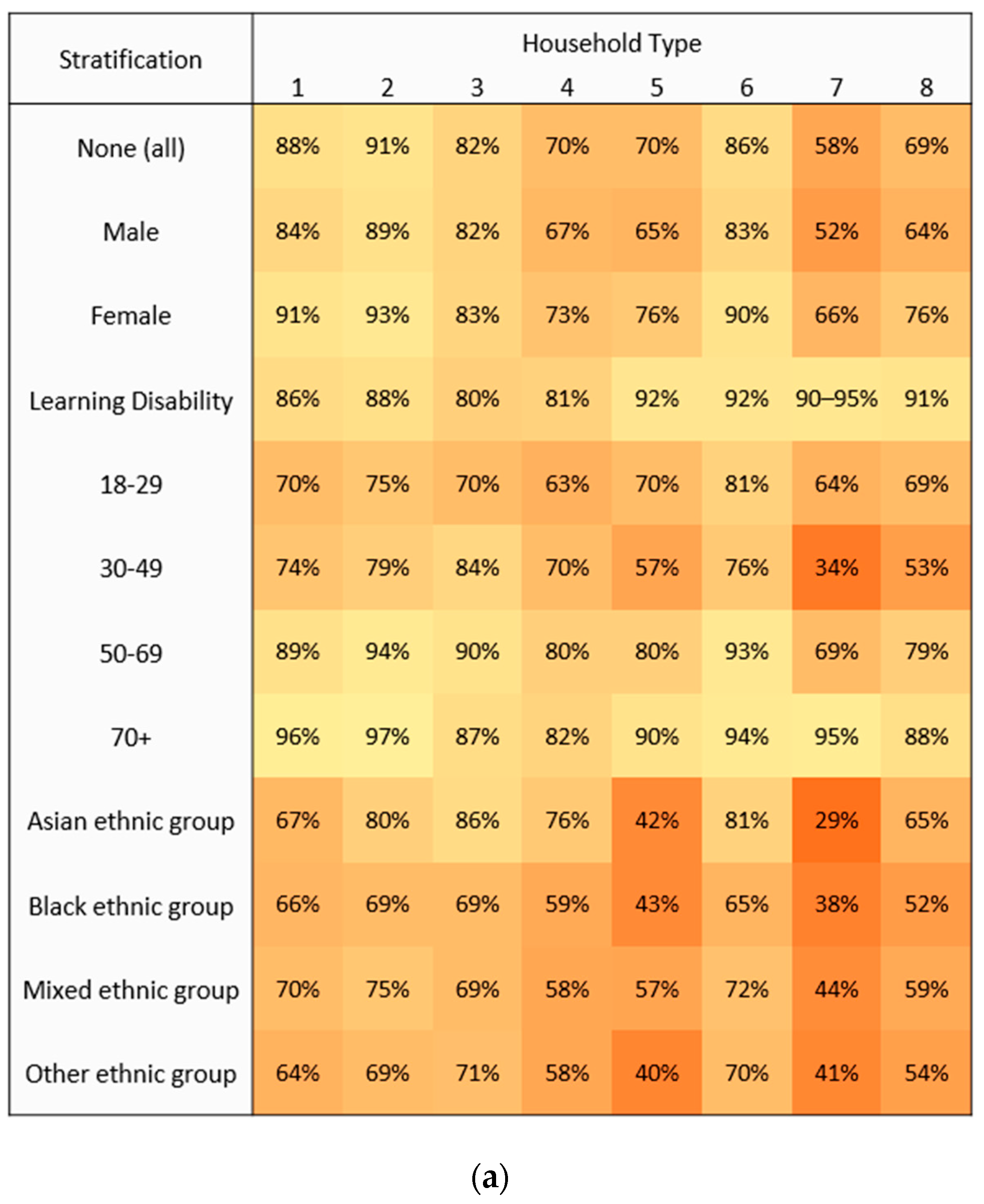
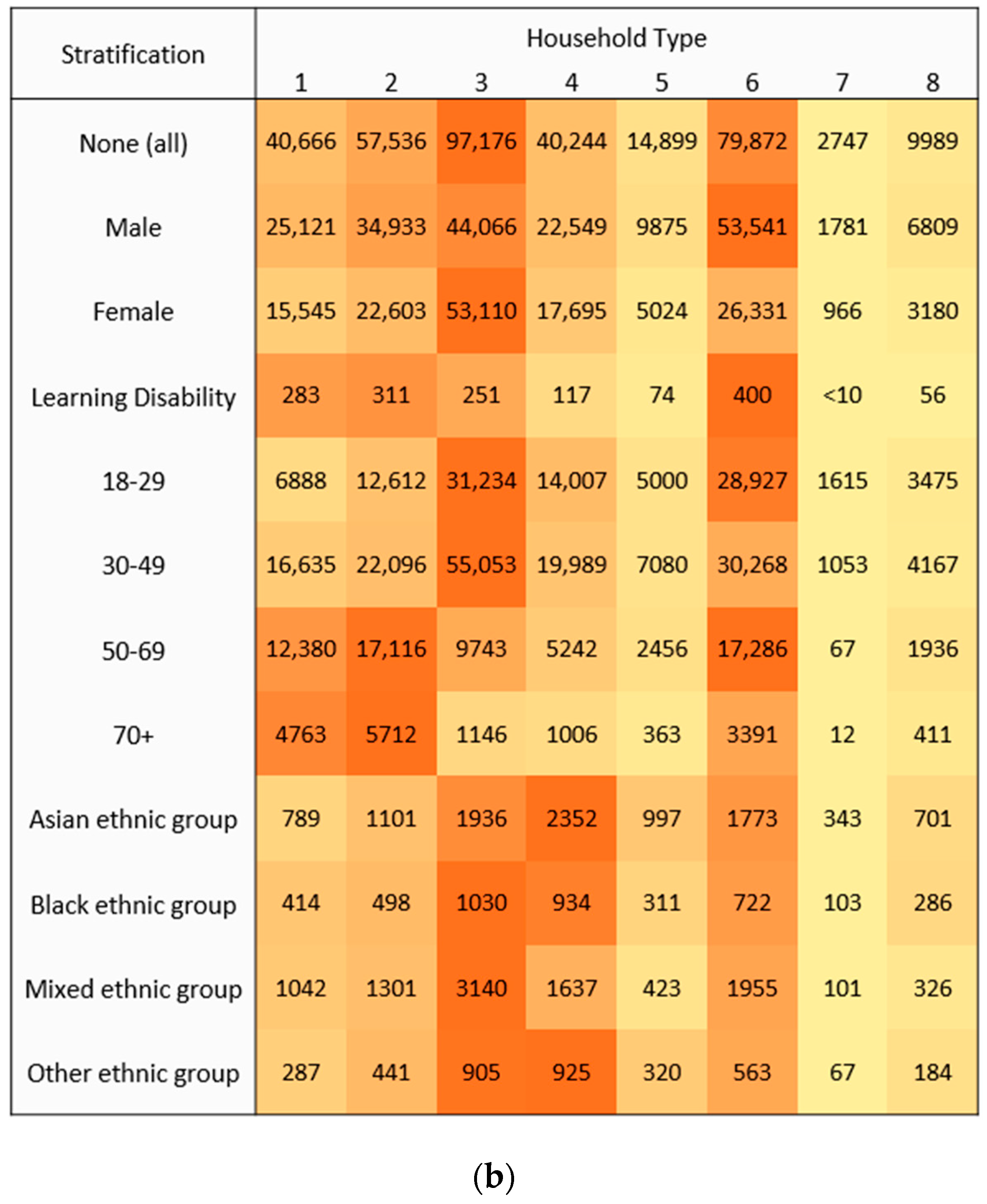
3. Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Perry, M.; Akbari, A.; Cottrell, S.; Gravenor, M.B.; Roberts, R.; Lyons, R.A.; Bedston, S.; Torabi, F.; Griffiths, L. Inequalities in coverage of COVID-19 vaccination: A population register based cross-sectional study in Wales, UK. Vaccine 2021, 39, 6256–6261. [Google Scholar] [CrossRef]
- Viswanath, K.; Bekalu, M.; Dhawan, D.; Pinnamaneni, R.; Lang, J.; Mcloud, R. Individual and social determinants of COVID-19 vaccine uptake. BMC Public Health 2021, 21, 818. [Google Scholar] [CrossRef] [PubMed]
- Whitehead, M.; Dahlgren, G. What can be done about inequalities in health? Lancet 1991, 338, 1059–1063. [Google Scholar] [CrossRef] [PubMed]
- Holt-Lunstad, J. Social isolation and health. Health Aff. 2020. [Google Scholar] [CrossRef]
- Muennig, P.; Jiao, B.; Singer, E. Living with parents or grandparents increases social capital and survival: 2014 General Social Survey-National Death Index. SSM Popul. Health 2017, 4, 71–75. [Google Scholar] [CrossRef] [PubMed]
- Cabinet Office. Ethnicity Facts and Figures: Overcrowded Households. 2020. Available online: https://www.ethnicity-facts-figures.service.gov.uk/housing/housing-conditions/overcrowded-households/latest (accessed on 11 January 2023).
- Rodgers, S.E.; Lyons, R.A.; Dsilva, R.; Jones, K.H.; Brooks, C.J.; Ford, D.V.; John, G.; Verplancke, J.-P. Residential Anonymous Linking Fields (RALFs): A novel information infrastructure to study the interaction between the environment and individuals’ health. J. Public Health 2009, 31, 582–588. [Google Scholar] [CrossRef] [PubMed]
- Ford, D.V.; Jones, K.H.; Verplancke, J.P.; Lyons, R.A.; John, G.; Brown, G.; Brooks, C.J.; Thompson, S.; Bodger, O.; Couch, T.; et al. The SAIL Databank: Building a national architecture for e-health research and evaluation. BMC Health Serv. Res. 2009, 9, 157. [Google Scholar] [CrossRef] [PubMed]
- Johnson, R.D.; Griffiths, L.J.; Hollinghurst, J.P.; Akbari, A.; Lee, A.; Thompson, D.A.; Lyons, R.A.; Fry, R. Deriving household composition using population-scale electronic health record data—A reproducible methodology. PLoS ONE 2021, 16, e0248195. [Google Scholar] [CrossRef] [PubMed]
- Jones, K.H.; Ford, D.V.; Thompson, S.; Lyons, R.A. A Profile of the SAIL Databank on the UK Secure Research Platform. Int. J. Popul. Data Sci. 2019, 4, 1134. [Google Scholar] [CrossRef] [PubMed]
- Lyons, J.; Akbari, A.; Torabi, F.; Davies, G.I.; North, L.; Griffiths, R.; Bailey, R.; Hollinghurst, J.; Fry, R.; Turner, S.L.; et al. Understanding and responding to COVID-19 in Wales: Protocol for a privacy-protecting data platform for enhanced epidemiology and evaluation of interventions. BMJ Open 2020, 10, e043010. [Google Scholar] [CrossRef] [PubMed]
- Office for National Statistics. 2011 Census Variable and Classification Information: Part 6. 2013. Available online: https://www.ons.gov.uk/census/2011census/2011censusdata/2011censususerguide/variablesandclassifications (accessed on 11 January 2023).
- Open Code Lists, Wider Learning Disability. Available online: https://www.opencodelists.org/codelist/primis-covid19-vacc-uptake/learndis/v.1.5.3/ (accessed on 29 January 2023).
- lm.cluster: Cluster Robust Standard Errors for Linear Models and General Linear Models. Available online: https://www.rdocumentation.org/packages/miceadds/versions/3.16-18/topics/lm.cluster (accessed on 29 January 2023).
- Jain, A.; van Hoek, A.J.; Boccia, D.; Thomas, S.L. Lower vaccine uptake amongst older individuals living alone: A systematic review and meta-analysis of social determinants of vaccine uptake. Vaccine 2017, 35, 2315–2328. [Google Scholar] [CrossRef] [PubMed]
- Endrich, M.M.; Blank, P.R.; Szucs, T.D. Influenza vaccination uptake and socioeconomic determinants in 11 European countries. Vaccine 2009, 27, 4018–4024. [Google Scholar] [CrossRef] [PubMed]
- Jain, A.; Walker, J.L.; Mathur, R.; Forbes, H.J.; Langan, S.M.; Smeeth, L.; van Hoek, A.J.; Thomas, S.L. Zoster vaccination inequalities: A population based cohort study using linked data from the UK Clinical Practice Research Datalink. PLoS ONE 2018, 13, e0207183. [Google Scholar] [CrossRef] [PubMed]
- Epperson, A.E.; Carson, S.L.; Garcia, A.N.; Casillas, A.; Castellon-Lopez, Y.; Brown, A.F.; Nanibaa’A, G. A qualitative study of COVID-19 vaccine decision making among urban Native Americans. Vaccine X 2022, 12, 100212. [Google Scholar] [CrossRef] [PubMed]
- Balasuriya, L.; Santilli, A.; Morone, J.; Ainooson, J.; Roy, B.; Njoku, A.; Mendiola-Iparraguirre, A.; O’Connor Duffany, K.; Macklin, B.; Higginbottom, J.; et al. COVID-19 Vaccine Acceptance and Access Among Black and Latinx Communities. JAMA Netw. Open 2021, 4, e2128575. [Google Scholar] [CrossRef] [PubMed]
- Clifford, S. Coronavirus (COVID-19) and the Black, Asian and Minority Ethnic (BAME) Population in Wales. 2020. Available online: https://www.gov.wales/sites/default/files/statistics-and-research/2020-06/coronavirus-COVID-19-and-the-black-asian-and-minority-ethnic-population-154.pdf (accessed on 11 January 2023).
- Addison, K.; Batt, B.; Stock, K. Housing Overcrowding and Ethnicity: A Literature Review. 2022. Available online: https://gov.wales/housing-overcrowding-and-ethnicity-literature-review (accessed on 11 January 2023).
| Household Type | Definition | Relevant Housing Classifications |
|---|---|---|
| 1. Single occupancy | Size 1 | Lone dwelling. |
| 2. Two adults | Size 2, no <18 | Partnership. Cohabitation. |
| 3. Adults/children | Size 2–5, <18 present | Family a |
| 4. Large adults/children | Size 6–9, <18 present | Large family a |
| 5. Adult group, single generation | Size 3–5, no <18, age difference <19 years | Communal residence. |
| 6. Adult group, multiple generations | Size 3–5, no <18, age difference >18 years | Family with adult children. Communal residence. |
| 7. Large adult group, single generation | Size 6–9, no <18, 1 generation, age difference <19 years | Large communal residence. |
| 8. Large adult group, multiple generations | Size 6–9, no <18, >1 generation, age difference >18 years | Large family with adult children. Large communal residence. |
| Household Type | Population (n) | Vaccinated (n) | Uptake (%) | OR (95% CI) |
|---|---|---|---|---|
| 1. Single occupancy | 327,629 | 286,963 | 87.6% | 0.70 (0.69–0.71) |
| 2. Two adults | 639,882 | 582,346 | 91.0% | Baseline |
| 3. Adults/children | 549,758 | 452,582 | 82.3% | 0.46 (0.46–0.47) |
| 4. Large adults/children | 135,043 | 94,799 | 70.2% | 0.23 (0.23–0.24) |
| 5. Adult group, single generation | 48,892 | 33,993 | 69.5% | 0.23 (0.22–0.23) |
| 6. Adult group, multiple generations | 577,057 | 497,185 | 86.2% | 0.62 (0.61–0.62) |
| 7. Large adult group, single generation | 6553 | 3806 | 58.1% | 0.14 (0.13–0.14) |
| 8. Large adult group, multiple generations | 32,461 | 22,472 | 69.2% | 0.22 (0.22–0.23) |
| Variable | Category | Population (n) | Vaccinated (n) | aOR (95% CI) |
|---|---|---|---|---|
| Household Type | 1. Single occupancy | 327,629 | 286,963 | 0.70 (0.69–0.71) |
| 2. Two adults | 639,882 | 582,346 | Baseline | |
| 3. Adults/children | 549,758 | 452,582 | 0.83 (0.82–0.84) | |
| 4. Large adults/children | 135,043 | 94,799 | 0.48 (0.47–0.49) | |
| 5. Adult group, single generation | 48,892 | 33,993 | 0.53 (0.52–0.54) | |
| 6. Adult group, multiple generations | 577,057 | 497,185 | 0.89 (0.88–0.90) | |
| 7. Large adult group, single generation | 6553 | 3806 | 0.52 (0.49–0.55) | |
| 8. Large adult group, multiple generations | 32,461 | 22,472 | 0.45 (0.43–0.46) | |
| Gender | Female | 1,161,191 | 1,016,737 | Baseline |
| Male | 1,156,084 | 957,409 | 0.73 (0.72–0.74) | |
| Age Group | 18–29 | 402,223 | 298,465 | 0.30 (0.30–0.30) |
| 30–49 | 731,813 | 575,472 | 0.39 (0.39–0.40) | |
| 50–69 | 760,289 | 694,063 | Baseline | |
| 70+ | 422,950 | 406,146 | 2.05 (2.01–2.08) | |
| Health Board | Health Board 1 | 438,803 | 380,953 | Baseline |
| Health Board 2 | 502,623 | 427,760 | 0.72 (0.71–0.73) | |
| Health Board 3 | 369,837 | 303,933 | 0.86 (0.85–0.88) | |
| Health Board 4 | 336,450 | 294,497 | 1.04 (1.03–1.06) | |
| Health Board 5 | 281,646 | 241,400 | 0.73 (0.72–0.74) | |
| Health Board 6 | 94,642 | 81,317 | 0.67 (0.65–0.68) | |
| Health Board 7 | 293,274 | 244,286 | 0.74 (0.73–0.75) | |
| Location Classification | Rural | 712,806 | 626,082 | 1.15 (1.14–1.16) |
| Urban | 1,604,469 | 1,348,064 | Baseline | |
| Ethnic Group | Asian | 44,767 | 34,775 | 0.75 (0.73–0.77) |
| Black | 11,773 | 7475 | 0.39 (0.37–0.40) | |
| Mixed | 31,523 | 21,598 | 0.46 (0.45–0.47) | |
| Other | 10,432 | 6740 | 0.40 (0.39–0.42) | |
| Unknown | 235,552 | 158,880 | 0.33 (0.32–0.33) | |
| White | 1,983,228 | 1,744,678 | Baseline | |
| Deprivation Quintile | 1 (Most deprived) | 452,962 | 356,673 | 0.47 (0.46–0.47) |
| 2 | 461,071 | 386,911 | 0.60 (0.59–0.61) | |
| 3 | 468,108 | 397,891 | 0.68 (0.67–0.69) | |
| 4 | 465,345 | 409,365 | 0.80 (0.79–0.81) | |
| 5 (Least deprived) | 469,789 | 423,306 | Baseline |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lench, A.; Perry, M.; Johnson, R.D.; Fry, R.; Richardson, G.; Lyons, R.A.; Akbari, A.; Edwards, A.; Collins, B.; Joseph-Williams, N.; et al. Household Composition and Inequalities in COVID-19 Vaccination in Wales, UK. Vaccines 2023, 11, 604. https://doi.org/10.3390/vaccines11030604
Lench A, Perry M, Johnson RD, Fry R, Richardson G, Lyons RA, Akbari A, Edwards A, Collins B, Joseph-Williams N, et al. Household Composition and Inequalities in COVID-19 Vaccination in Wales, UK. Vaccines. 2023; 11(3):604. https://doi.org/10.3390/vaccines11030604
Chicago/Turabian StyleLench, Alex, Malorie Perry, Rhodri D. Johnson, Richard Fry, Gill Richardson, Ronan A. Lyons, Ashley Akbari, Adrian Edwards, Brendan Collins, Natalie Joseph-Williams, and et al. 2023. "Household Composition and Inequalities in COVID-19 Vaccination in Wales, UK" Vaccines 11, no. 3: 604. https://doi.org/10.3390/vaccines11030604
APA StyleLench, A., Perry, M., Johnson, R. D., Fry, R., Richardson, G., Lyons, R. A., Akbari, A., Edwards, A., Collins, B., Joseph-Williams, N., Cooper, A., & Cottrell, S. (2023). Household Composition and Inequalities in COVID-19 Vaccination in Wales, UK. Vaccines, 11(3), 604. https://doi.org/10.3390/vaccines11030604







