Determinants of Acceptance of COVID-19 Vaccination in Healthcare and Public Health Professionals: A Review
Abstract
1. Introduction
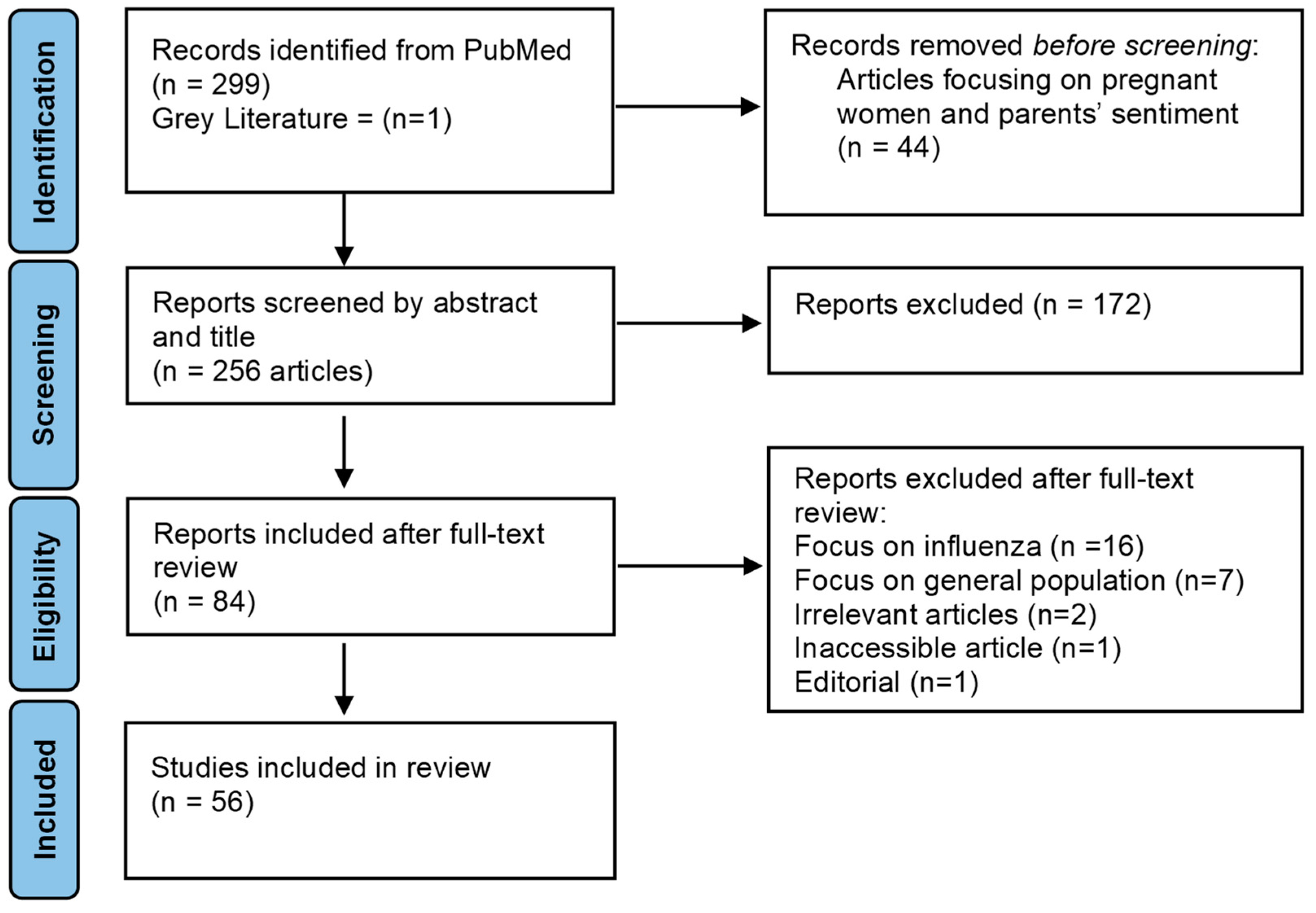
2. Materials and Methods
- Primary studies (cross-sectional, cohort, and longitudinal) and reviews (scoping reviews, systematic reviews, and meta-analysis) with access to the full text;
- Population: Healthcare workers or public health professionals;
- Outcome: Articles examining the sentiments of HCWs towards COVID-19 vaccines and their uptake;
- English language articles from any country.
- Exclusion Criteria:
- HCWs are solely listed as an occupational determinant of vaccine acceptance and there is no in-depth analysis of COVID-19 vaccination sentiments within this population;
- Focus is not on the sentiments of HCWs regarding the COVID-19 vaccines;
- Focus is on the influence of influenza on COVID-19 and not vice versa;
- Inaccessible articles, letters, and non-original research articles were excluded.
3. Results
3.1. Characteristics of Studies
3.2. Determinants of COVID-19 Vaccine Acceptance
3.2.1. Gender
3.2.2. Age
3.2.3. Occupation
3.2.4. Ethnicity
| Determinants | Total Studies (n) | Country * | Reviews/Reports/Multi-National Studies |
|---|---|---|---|
| Age | |||
| 18–30 | 5 | China, Egypt, Italy, Palestine [14,15,18,31,37] | |
| 30–50 | 24 | China, Cyprus, Czech Republic, France, Germany, Greece, India, Saudi Arabia, Spain, Turkey, UK, US [12,13,16,19,21,26,27,38,47,48,50,51,54,58,59,60,62] | Biswas et al., Hajure et al., Khubchandani et al., Leigh et al., Li et al., Luo et al., PAHO [8,25,29,32,34,35,64] |
| >60 | 4 | Azerbaijan, Germany, Switzerland, UK [10,17,43,63] | |
| Gender | |||
| Male | 25 | Albania, Cyprus, Czech Republic, Egypt, France, Germany, Greece, Kosovo, Lebanon, Palestine, Spain, Switzerland, Turkey, UAE, UK, US [10,16,18,21,23,24,26,36,37,38,42,43,44,46,49,52,54,59,61,63] | Biswas et al., Hajure et al., Khubchandani et al., Li et al., Luo et al. [8,25,29,34,35] |
| Female | 3 | Cyprus, Greece, Saudi Arabia [13,19,22] | |
| Education | 12 | China, Germany, Greece, Italy, Turkey, US [20,23,27,43,46,55,60] | Biswas et al., Hajure et al., Khubchandani et al., Li et al., Shakeel et al. [8,25,29,34,53] |
| Occupation | |||
| Nurses | 18 | China, Egypt, France, Germany, Greece, India, Israel, Italy, Palestine, Switzerland, Turkey, UK, US [10,12,14,16,18,21,27,36,37,46,48,50,59,60,62,63] | Li et al., PAHO [34,64] |
| Physicians | 31 | China, Cyprus, Czech Republic, Egypt, France, Germany, Greece, India, Israel, Italy, Palestine, Slovakia, Spain, Switzerland, Turkey, UK, US [10,12,14,15,16,18,20,21,23,26,27,36,37,38,40,46,47,48,50,51,54,56,57,60,62,63] | Biswas et al., Hajure et al., Leigh et al., Li et al., PAHO [8,25,32,34,64] |
| Ethnicity | 5 | UK, US [10,23,59] | Hajure et al., Li et al. [25,34] |
| Comorbidities | 9 | Azerbaijan, China, Egypt, Greece, US [17,18,23,36,57] | Biswas et al., Hajure et al., Khubchandani et al., Li et al., [8,25,29,34] |
| Previous Influenza Vaccination | 39 | Albania, Azerbaijan, China, Cyprus, Czech Republic, Egypt, France, Greece, Italy, Kosovo, Lebanon, Palestine, Slovakia, Spain, Switzerland, Tunisia, Turkey, UAE, UK, US [10,14,15,16,17,18,19,21,22,23,24,26,27,28,36,37,38,40,41,44,45,47,48,49,52,54,55,56,57,59,60,61,63] | Biswas et al., Hajure et al., Khubchandani et al., Li et al., Luo et al., Shakeel et al. [8,25,29,34,35,53] |
| Previous COVID-19 Infection | 16 | Azerbaijan, Albania, Cyprus, Czech Republic, Egypt, France, Greece, Italy, Kosovo, Lebanon, Turkey, Slovakia, Spain, UK, US [16,17,18,27,40,44,47,48,49,54,56,58,61] | Biswas et al., Hajure et al., Li et al. [8,25,34] |
3.2.5. Education
3.2.6. Chronic Diseases/Comorbidities
3.3. Influenza Vaccination as a Factor for COVID-19 Vaccination
3.4. Factors and Barriers of Intention to Taking a COVID-19 Vaccine
3.5. Interventions
3.6. Vaccine Brands as a Factor for COVID-19 Vaccination
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Key Concepts | PubMed MeSH Terms | PubMed Keywords |
|---|---|---|
| COVID-19 | COVID-19 OR SARS-CoV-2 OR COVID-19 Vaccines | COVID-19 OR “COVID-19 pandemic” OR “coronavirus pandemic” OR “COVID-19 virus” OR “COVID-19 vaccine*” |
| Influenza | Influenza OR Vaccines | influenza OR flu OR “influenza vaccine*” OR “flu vaccine*” |
| Sentiment/Acceptance | Health Knowledge, Attitudes, Practice OR Acceptability of Healthcare OR Health Personnel Attitude | accept* OR sentiment OR belief* |
| Health Workers | Health Personnel OR Professional Role | “Healthcare worker*” OR “Health care worker*” OR “health professional*” OR “public health care worker*” OR “public healthcare worker*” |
| Vaccine Hesitancy | Vaccine OR Vaccination OR Immunization OR Vaccination Refusal | Immunis* OR Immuniz* OR Vaccin* OR “vaccine hesitan*” |
References
- COVID-19 Data Explorer. Available online: https://ourworldindata.org/explorers/coronavirus-data-explorer (accessed on 2 December 2022).
- Mathieu, E.; Ritchie, H.; Rodés-Guirao, L.; Appel, C.; Giattino, C.; Hasell, J.; Macdonald, B.; Dattani, S.; Beltekian, D.; Ortiz-Ospina, E.; et al. Coronavirus Pandemic (COVID-19). Available online: https://ourworldindata.org/covid-vaccinations (accessed on 2 December 2022).
- Larson, H.J.; Gakidou, E.; Murray, C.J.L. The Vaccine-Hesitant Moment. N. Engl. J. Med. 2022, 387, 58–65. [Google Scholar] [CrossRef]
- Thompson, J.; Wattam, S. Estimating the Impact of Interventions against COVID-19: From Lockdown to Vaccination. PLoS ONE 2021, 16, e0261330. [Google Scholar] [CrossRef] [PubMed]
- MacDonald, N.E.; Eskola, J.; Liang, X.; Chaudhuri, M.; Dube, E.; Gellin, B.; Goldstein, S.; Larson, H.; Manzo, M.L.; Reingold, A.; et al. Vaccine Hesitancy: Definition, Scope and Determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef]
- Ten Threats to Global Health in 2019. Available online: https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019 (accessed on 2 December 2022).
- WHO SAGE Roadmap for Prioritizing Uses of COVID-19 Vaccines: An Approach to Optimize the Global Impact of COVID-19 Vaccines, Based on Public Health Goals, Global and National Equity, and Vaccine Access and Coverage Scenarios. Available online: https://www.who.int/publications-detail-redirect/WHO-2019-nCoV-Vaccines-SAGE-Prioritization-2022.1 (accessed on 2 December 2022).
- Biswas, N.; Mustapha, T.; Khubchandani, J.; Price, J.H. The Nature and Extent of COVID-19 Vaccination Hesitancy in Healthcare Workers. J. Community Health 2021, 46, 1244–1251. [Google Scholar] [CrossRef] [PubMed]
- Montagna, M.T.; De Giglio, O.; Napoli, C.; Fasano, F.; Diella, G.; Donnoli, R.; Caggiano, G.; Tafuri, S.; Lopalco, P.L.; Agodi, A.; et al. Adherence to Vaccination Policy among Public Health Professionals: Results of a National Survey in Italy. Vaccines 2020, 8, 379. [Google Scholar] [CrossRef]
- Abuown, A.; Ellis, T.; Miller, J.; Davidson, R.; Kachwala, Q.; Medeiros, M.; Mejia, K.; Manoraj, S.; Sidhu, M.; Whittington, A.M.; et al. COVID-19 Vaccination Intent among London Healthcare Workers. Occup. Med. 2021, 71, 211–214. [Google Scholar] [CrossRef] [PubMed]
- Al-Metwali, B.Z.; Al-Jumaili, A.A.; Al-Alag, Z.A.; Sorofman, B. Exploring the Acceptance of COVID-19 Vaccine among Healthcare Workers and General Population Using Health Belief Model. J. Eval. Clin. Pract. 2021, 27, 1112–1122. [Google Scholar] [CrossRef]
- Ashok, N.; Krishnamurthy, K.; Singh, K.; Rahman, S.; Majumder, M.A.A. High COVID-19 Vaccine Hesitancy Among Healthcare Workers: Should Such a Trend Require Closer Attention by Policymakers? Cureus 2021, 13, e17990. [Google Scholar] [CrossRef]
- Baghdadi, L.R.; Alghaihb, S.G.; Abuhaimed, A.A.; Alkelabi, D.M.; Alqahtani, R.S. Healthcare Workers’ Perspectives on the Upcoming COVID-19 Vaccine in Terms of Their Exposure to the Influenza Vaccine in Riyadh, Saudi Arabia: A Cross-Sectional Study. Vaccines 2021, 9, 465. [Google Scholar] [CrossRef]
- Di Gennaro, F.; Murri, R.; Segala, F.V.; Cerruti, L.; Abdulle, A.; Saracino, A.; Bavaro, D.F.; Fantoni, M. Attitudes towards Anti-SARS-CoV2 Vaccination among Healthcare Workers: Results from a National Survey in Italy. Viruses 2021, 13, 371. [Google Scholar] [CrossRef]
- Di Valerio, Z.; Montalti, M.; Guaraldi, F.; Tedesco, D.; Nreu, B.; Mannucci, E.; Monami, M.; Gori, D. Trust of Italian Healthcare Professionals in COVID-19 (Anti-SARS-CoV-2) Vaccination. Ann. Ig. 2022, 34, 217–226. [Google Scholar] [CrossRef] [PubMed]
- Do, T.V.C.; Thota Kammili, S.; Reep, M.; Wisnieski, L.; Ganti, S.S.; Depa, J. COVID-19 Vaccine Acceptance Among Rural Appalachian Healthcare Workers (Eastern Kentucky/West Virginia): A Cross-Sectional Study. Cureus 2021, 13, e16842. [Google Scholar] [CrossRef] [PubMed]
- Doran, J.; Seyidov, N.; Mehdiyev, S.; Gon, G.; Kissling, E.; Herdman, T.; Suleymanova, J.; Rehse, A.P.C.; Pebody, R.; Katz, M.A.; et al. Factors Associated with Early Uptake of COVID-19 Vaccination among Healthcare Workers in Azerbaijan, 2021. Influenza Other Respir. Viruses 2022, 16, 626–631. [Google Scholar] [CrossRef]
- Elkhayat, M.R.; Hashem, M.K.; Helal, A.T.; Shaaban, O.M.; Ibrahim, A.K.; Meshref, T.S.; Elkhayat, H.; Moustafa, M.; Mohammed, M.N.A.; Ezzeldin, A.M.; et al. Determinants of Obtaining COVID-19 Vaccination among Health Care Workers with Access to Free COVID-19 Vaccination: A Cross-Sectional Study. Vaccines 2021, 10, 39. [Google Scholar] [CrossRef]
- Fakonti, G.; Kyprianidou, M.; Toumbis, G.; Giannakou, K. Attitudes and Acceptance of COVID-19 Vaccination Among Nurses and Midwives in Cyprus: A Cross-Sectional Survey. Front. Public Health 2021, 9, 656138. [Google Scholar] [CrossRef]
- Fotiadis, K.; Dadouli, K.; Avakian, I.; Bogogiannidou, Z.; Mouchtouri, V.A.; Gogosis, K.; Speletas, M.; Koureas, M.; Lagoudaki, E.; Kokkini, S.; et al. Factors Associated with Healthcare Workers’ (HCWs) Acceptance of COVID-19 Vaccinations and Indications of a Role Model towards Population Vaccinations from a Cross-Sectional Survey in Greece, May 2021. Int. J. Environ. Res. Public Health 2021, 18, 10558. [Google Scholar] [CrossRef] [PubMed]
- Gagneux-Brunon, A.; Detoc, M.; Bruel, S.; Tardy, B.; Rozaire, O.; Frappe, P.; Botelho-Nevers, E. Intention to Get Vaccinations against COVID-19 in French Healthcare Workers during the First Pandemic Wave: A Cross-Sectional Survey. J. Hosp. Infect. 2021, 108, 168–173. [Google Scholar] [CrossRef]
- Galanis, P.; Moisoglou, I.; Vraka, I.; Siskou, O.; Konstantakopoulou, O.; Katsiroumpa, A.; Kaitelidou, D. Predictors of COVID-19 Vaccine Uptake in Healthcare Workers: A Cross-Sectional Study in Greece. J. Occup. Environ. Med. 2022, 64, e191–e196. [Google Scholar] [CrossRef]
- Gatto, N.M.; Lee, J.E.; Massai, D.; Zamarripa, S.; Sasaninia, B.; Khurana, D.; Michaels, K.; Freund, D.; Nightingale, J.; Firek, A. Correlates of COVID-19 Vaccine Acceptance, Hesitancy and Refusal among Employees of a Safety Net California County Health System with an Early and Aggressive Vaccination Program: Results from a Cross-Sectional Survey. Vaccines 2021, 9, 1152. [Google Scholar] [CrossRef]
- Gönüllü, E.; Soysal, A.; Atıcı, S.; Engin, M.; Yeşilbaş, O.; Kasap, T.; Fedakar, A.; Bilgiç, E.; Tavil, E.B.; Tutak, E.; et al. Pediatricians’ COVID-19 Experiences and Views on the Willingness to Receive COVID-19 Vaccines: A Cross-Sectional Survey in Turkey. Hum. Vaccin. Immunother. 2021, 17, 2389–2396. [Google Scholar] [CrossRef]
- Hajure, M.; Tariku, M.; Bekele, F.; Abdu, Z.; Dule, A.; Mohammedhussein, M.; Tsegaye, T. Attitude Towards COVID-19 Vaccination Among Healthcare Workers: A Systematic Review. Infect. Drug. Resist. 2021, 14, 3883–3897. [Google Scholar] [CrossRef] [PubMed]
- İkiışık, H.; Sezerol, M.A.; Taşçı, Y.; Maral, I. COVID-19 Vaccine Hesitancy and Related Factors among Primary Healthcare Workers in a District of Istanbul: A Cross-Sectional Study from Turkey. Fam. Med. Community Health 2022, 10, e001430. [Google Scholar] [CrossRef] [PubMed]
- Kara Esen, B.; Can, G.; Pirdal, B.Z.; Aydin, S.N.; Ozdil, A.; Balkan, I.I.; Budak, B.; Keskindemirci, Y.; Karaali, R.; Saltoglu, N. COVID-19 Vaccine Hesitancy in Healthcare Personnel: A University Hospital Experience. Vaccines 2021, 9, 1343. [Google Scholar] [CrossRef] [PubMed]
- Kefi, H.E.; Kefi, K.; Krir, M.W.; Brahim, C.B.; Baatout, A.; Bouzouita, I.; Azaiz, M.B.; Bouguerra, C.; Khoufi, M.T.; Gharsallah, H.; et al. Acceptability of COVID-19 Vaccine: A Cross-Sectional Study in a Tunisian General Hospital. Pan Afr. Med. J. 2021, 39, 245. [Google Scholar] [CrossRef]
- Khubchandani, J.; Bustos, E.; Chowdhury, S.; Biswas, N.; Keller, T. COVID-19 Vaccine Refusal among Nurses Worldwide: Review of Trends and Predictors. Vaccines 2022, 10, 230. [Google Scholar] [CrossRef]
- Koh, S.W.C.; Liow, Y.; Loh, V.W.K.; Liew, S.J.; Chan, Y.-H.; Young, D. COVID-19 Vaccine Acceptance and Hesitancy among Primary Healthcare Workers in Singapore. BMC Prim. Care 2022, 23, 81. [Google Scholar] [CrossRef]
- Kwok, K.O.; Li, K.-K.; Wei, W.I.; Tang, A.; Wong, S.Y.S.; Lee, S.S. Editor’s Choice: Influenza Vaccine Uptake, COVID-19 Vaccination Intention and Vaccine Hesitancy among Nurses: A Survey. Int. J. Nurs. Stud. 2021, 114, 103854. [Google Scholar] [CrossRef]
- Leigh, J.P.; Moss, S.J.; White, T.M.; Picchio, C.A.; Rabin, K.H.; Ratzan, S.C.; Wyka, K.; El-Mohandes, A.; Lazarus, J.V. Factors Affecting COVID-19 Vaccine Hesitancy among Healthcare Providers in 23 Countries. Vaccine 2022, 40, 4081–4089. [Google Scholar] [CrossRef]
- Leung, C.L.K.; Li, K.-K.; Wei, V.W.I.; Tang, A.; Wong, S.Y.S.; Lee, S.S.; Kwok, K.O. Profiling Vaccine Believers and Skeptics in Nurses: A Latent Profile Analysis. Int. J. Nurs. Stud. 2022, 126, 104142. [Google Scholar] [CrossRef]
- Li, M.; Luo, Y.; Watson, R.; Zheng, Y.; Ren, J.; Tang, J.; Chen, Y. Healthcare Workers’ (HCWs) Attitudes and Related Factors towards COVID-19 Vaccination: A Rapid Systematic Review. Postgrad. Med. J. 2021. [Google Scholar] [CrossRef]
- Luo, C.; Yang, Y.; Liu, Y.; Zheng, D.; Shao, L.; Jin, J.; He, Q. Intention to COVID-19 Vaccination and Associated Factors among Health Care Workers: A Systematic Review and Meta-Analysis of Cross-Sectional Studies. Am. J. Infect. Control 2021, 49, 1295–1304. [Google Scholar] [CrossRef]
- Maltezou, H.C.; Pavli, A.; Dedoukou, X.; Georgakopoulou, T.; Raftopoulos, V.; Drositis, I.; Bolikas, E.; Ledda, C.; Adamis, G.; Spyrou, A.; et al. Determinants of Intention to Get Vaccinated against COVID-19 among Healthcare Personnel in Hospitals in Greece. Infect. Dis. Health 2021, 26, 189–197. [Google Scholar] [CrossRef] [PubMed]
- Maraqa, B.; Nazzal, Z.; Rabi, R.; Sarhan, N.; Al-Shakhra, K.; Al-Kaila, M. COVID-19 Vaccine Hesitancy among Health Care Workers in Palestine: A Call for Action. Prev. Med. 2021, 149, 106618. [Google Scholar] [CrossRef]
- Mena, G.; Blanco, B.; Casas, I.; Huertas, A.; Sánchez, M.-A.; Auñón, M.; Viñas, J.; Esteve, M. Attitudes of Spanish Hospital Staff towards COVID-19 Vaccination and Vaccination Rates. PLoS ONE 2021, 16, e0257002. [Google Scholar] [CrossRef] [PubMed]
- Moirangthem, S.; Olivier, C.; Gagneux-Brunon, A.; Péllissier, G.; Abiteboul, D.; Bonmarin, I.; Rouveix, E.; Botelho-Nevers, E.; Mueller, J.E. Social Conformism and Confidence in Systems as Additional Psychological Antecedents of Vaccination: A Survey to Explain Intention for COVID-19 Vaccination among Healthcare and Welfare Sector Workers, France, December 2020 to February 2021. Eurosurveillance 2022, 27, 2100617. [Google Scholar] [CrossRef]
- Monami, M.; Gori, D.; Guaraldi, F.; Montalti, M.; Nreu, B.; Burioni, R.; Mannucci, E. COVID-19 Vaccine Hesitancy and Early Adverse Events Reported in a Cohort of 7,881 Italian Physicians. Ann. Ig. 2021, 4, 344–357. [Google Scholar] [CrossRef]
- Nasr, L.; Saleh, N.; Hleyhel, M.; El-Outa, A.; Noujeim, Z. Acceptance of COVID-19 Vaccination and Its Determinants among Lebanese Dentists: A Cross-Sectional Study. BMC Oral Health 2021, 21, 484. [Google Scholar] [CrossRef]
- Navarre, C.; Roy, P.; Ledochowski, S.; Fabre, M.; Esparcieux, A.; Issartel, B.; Dutertre, M.; Blanc-Gruyelle, A.-L.; Suy, F.; Adelaide, L.; et al. Determinants of COVID-19 Vaccine Hesitancy in French Hospitals. Infect. Dis. Now 2021, 51, 647–653. [Google Scholar] [CrossRef]
- Nohl, A.; Afflerbach, C.; Lurz, C.; Brune, B.; Ohmann, T.; Weichert, V.; Zeiger, S.; Dudda, M. Acceptance of COVID-19 Vaccination among Front-Line Health Care Workers: A Nationwide Survey of Emergency Medical Services Personnel from Germany. Vaccines 2021, 9, 424. [Google Scholar] [CrossRef]
- Okuyan, B.; Bektay, M.Y.; Demirci, M.Y.; Ay, P.; Sancar, M. Factors Associated with Turkish Pharmacists’ Intention to Receive COVID-19 Vaccine: An Observational Study. Int. J. Clin. Pharm. 2022, 44, 247–255. [Google Scholar] [CrossRef]
- Papagiannis, D.; Rachiotis, G.; Malli, F.; Papathanasiou, I.V.; Kotsiou, O.; Fradelos, E.C.; Giannakopoulos, K.; Gourgoulianis, K.I. Acceptability of COVID-19 Vaccination among Greek Health Professionals. Vaccines 2021, 9, 200. [Google Scholar] [CrossRef] [PubMed]
- Papini, F.; Mazzilli, S.; Paganini, D.; Rago, L.; Arzilli, G.; Pan, A.; Goglio, A.; Tuvo, B.; Privitera, G.; Casini, B. Healthcare Workers Attitudes, Practices and Sources of Information for COVID-19 Vaccination: An Italian National Survey. Int. J. Environ. Res. Public Health 2022, 19, 733. [Google Scholar] [CrossRef] [PubMed]
- Paris, C.; Saade, A.; Tadié, E.; Nguyen Van, R.; Turmel, V.; Garlantezec, R.; Tattevin, P. Determinants of the Willingness to Get the Third COVID-19 Vaccine Dose among Health Care Workers. Infect. Dis. Now 2022, 52, 223–226. [Google Scholar] [CrossRef] [PubMed]
- Paris, C.; Bénézit, F.; Geslin, M.; Polard, E.; Baldeyrou, M.; Turmel, V.; Tadié, É.; Garlantezec, R.; Tattevin, P. COVID-19 Vaccine Hesitancy among Healthcare Workers. Infect. Dis. Now 2021, 51, 484–487. [Google Scholar] [CrossRef] [PubMed]
- Patelarou, A.; Saliaj, A.; Galanis, P.; Pulomenaj, V.; Prifti, V.; Sopjani, I.; Mechili, E.A.; Laredo-Aguilera, J.A.; Kicaj, E.; Kalokairinou, A.; et al. Predictors of Nurses’ Intention to Accept COVID-19 Vaccination: A Cross-Sectional Study in Five European Countries. J. Clin. Nurs. 2022, 31, 1258–1266. [Google Scholar] [CrossRef]
- Presotto, M.A.; Jörres, R.A.; Gesierich, W.; Bullwinkel, J.; Rabe, K.F.; Schultz, K.; Kaestner, F.; Harzheim, D.; Kreuter, M.; Herth, F.J.F.; et al. Gender Differences in Health Care Workers’ Risk-Benefit Trade-Offs for COVID-19 Vaccination. Respiration 2022, 101, 646–653. [Google Scholar] [CrossRef]
- Raftopoulos, V.; Iordanou, S.; Katsapi, A.; Dedoukou, X.; Maltezou, H.C. A Comparative Online Survey on the Intention to Get COVID-19 Vaccine between Greek and Cypriot Healthcare Personnel: Is the Country a Predictor? Hum. Vaccin. Immunother. 2021, 17, 2397–2404. [Google Scholar] [CrossRef]
- Saddik, B.; Al-Bluwi, N.; Shukla, A.; Barqawi, H.; Alsayed, H.A.H.; Sharif-Askari, N.S.; Temsah, M.-H.; Bendardaf, R.; Hamid, Q.; Halwani, R. Determinants of Healthcare Workers Perceptions, Acceptance and Choice of COVID-19 Vaccines: A Cross-Sectional Study from the United Arab Emirates. Hum. Vaccin. Immunother. 2022, 18, 1–9. [Google Scholar] [CrossRef]
- Shakeel, C.S.; Mujeeb, A.A.; Mirza, M.S.; Chaudhry, B.; Khan, S.J. Global COVID-19 Vaccine Acceptance: A Systematic Review of Associated Social and Behavioral Factors. Vaccines 2022, 10, 110. [Google Scholar] [CrossRef]
- Štěpánek, L.; Janošíková, M.; Nakládalová, M.; Boriková, A.; Vildová, H. Motivation to COVID-19 Vaccination and Reasons for Hesitancy in Employees of a Czech Tertiary Care Hospital: A Cross-Sectional Survey. Vaccines 2021, 9, 863. [Google Scholar] [CrossRef]
- Sun, Y.; Chen, X.; Cao, M.; Xiang, T.; Zhang, J.; Wang, P.; Dai, H. Will Healthcare Workers Accept a COVID-19 Vaccine When It Becomes Available? A Cross-Sectional Study in China. Front. Public Health 2021, 9, 664905. [Google Scholar] [CrossRef]
- Ulbrichtova, R.; Svihrova, V.; Tatarkova, M.; Hudeckova, H.; Svihra, J. Acceptance of COVID-19 Vaccination among Healthcare and Non-Healthcare Workers of Hospitals and Outpatient Clinics in the Northern Region of Slovakia. Int. J. Environ. Res. Public Health 2021, 18, 12695. [Google Scholar] [CrossRef] [PubMed]
- Wang, K.; Wong, E.L.Y.; Ho, K.F.; Cheung, A.W.L.; Chan, E.Y.Y.; Yeoh, E.K.; Wong, S.Y.S. Intention of Nurses to Accept Coronavirus Disease 2019 Vaccination and Change of Intention to Accept Seasonal Influenza Vaccination during the Coronavirus Disease 2019 Pandemic: A Cross-Sectional Survey. Vaccine 2020, 38, 7049–7056. [Google Scholar] [CrossRef] [PubMed]
- Woolf, K.; Gogoi, M.; Martin, C.A.; Papineni, P.; Lagrata, S.; Nellums, L.B.; McManus, I.C.; Guyatt, A.L.; Melbourne, C.; Bryant, L.; et al. Healthcare Workers’ Views on Mandatory SARS-CoV-2 Vaccination in the UK: A Cross-Sectional, Mixed-Methods Analysis from the UK-REACH Study. EClinicalMedicine 2022, 46, 101346. [Google Scholar] [CrossRef]
- Woolf, K.; McManus, I.C.; Martin, C.A.; Nellums, L.B.; Guyatt, A.L.; Melbourne, C.; Bryant, L.; Gogoi, M.; Wobi, F.; Al-Oraibi, A.; et al. Ethnic Differences in SARS-CoV-2 Vaccine Hesitancy in United Kingdom Healthcare Workers: Results from the UK-REACH Prospective Nationwide Cohort Study. Lancet Reg. Health Eur. 2021, 9, 100180. [Google Scholar] [CrossRef] [PubMed]
- Ye, X.; Ye, W.; Yu, J.; Gao, Y.; Ren, Z.; Chen, L.; Dong, A.; Yi, Q.; Zhan, C.; Lin, Y.; et al. The Landscape of COVID-19 Vaccination among Healthcare Workers at the First Round of COVID-19 Vaccination in China: Willingness, Acceptance and Self-Reported Adverse Effects. Hum. Vaccin. Immunother. 2021, 17, 4846–4856. [Google Scholar] [CrossRef]
- Youssef, D.; Abou-Abbas, L.; Berry, A.; Youssef, J.; Hassan, H. Determinants of Acceptance of Coronavirus Disease-2019 (COVID-19) Vaccine among Lebanese Health Care Workers Using Health Belief Model. PLoS ONE 2022, 17, e0264128. [Google Scholar] [CrossRef] [PubMed]
- Zaitoon, H.; Sharkansky, L.; Ganaim, L.; Chistyakov, I.; Srugo, I.; Bamberger, E. Evaluation of Israeli Healthcare Workers Knowledge and Attitudes toward the COVID-19 Vaccine. Public Health Nurs. 2022, 39, 415–422. [Google Scholar] [CrossRef]
- Zürcher, K.; Mugglin, C.; Egger, M.; Müller, S.; Fluri, M.; Bolick, L.; Piso, R.J.; Hoffmann, M.; Fenner, L. Vaccination Willingness for COVID-19 among Healthcare Workers: A Cross-Sectional Survey in a Swiss Canton. Swiss. Med. Wkly. 2021, 151, w30061. [Google Scholar] [CrossRef]
- Puertas, E.B.; Velandia, M. Concerns, Attitudes, and Intended Practices of Healthcare Workers toward COVID-19 Vaccination in the Caribbean; Pan American Health Organization: Washington, DC, USA, 2021. [Google Scholar]
- Dror, A.A.; Eisenbach, N.; Taiber, S.; Morozov, N.G.; Mizrachi, M.; Zigron, A.; Srouji, S.; Sela, E. Vaccine Hesitancy: The next Challenge in the Fight against COVID-19. Eur. J. Epidemiol. 2020, 35, 775–779. [Google Scholar] [CrossRef] [PubMed]
- Levin, A.T.; Hanage, W.P.; Owusu-Boaitey, N.; Cochran, K.B.; Walsh, S.P.; Meyerowitz-Katz, G. Assessing the Age Specificity of Infection Fatality Rates for COVID-19: Systematic Review, Meta-Analysis, and Public Policy Implications. Eur. J. Epidemiol. 2020, 35, 1123–1138. [Google Scholar] [CrossRef] [PubMed]
- Moran, K.R.; Del Valle, S.Y. A Meta-Analysis of the Association between Gender and Protective Behaviors in Response to Respiratory Epidemics and Pandemics. PLoS ONE 2016, 11, e0164541. [Google Scholar] [CrossRef] [PubMed]
- Galbadage, T.; Peterson, B.M.; Awada, J.; Buck, A.S.; Ramirez, D.A.; Wilson, J.; Gunasekera, R.S. Systematic Review and Meta-Analysis of Sex-Specific COVID-19 Clinical Outcomes. Front. Med. 2020, 7, 348. [Google Scholar] [CrossRef] [PubMed]
- Di Giuseppe, G.; Pelullo, C.P.; Paolantonio, A.; Della Polla, G.; Pavia, M. Healthcare Workers’ Willingness to Receive Influenza Vaccination in the Context of the COVID-19 Pandemic: A Survey in Southern Italy. Vaccines 2021, 9, 766. [Google Scholar] [CrossRef] [PubMed]
| Regions | Country | Author | Number of Studies (n) |
|---|---|---|---|
| Europe | Albania | Patelarou et al. [49] | 1 |
| Cyprus | Fakonti et al., Patelarou et al., Raftopolous et al. [19,49,51] | 3 | |
| Czech Republic | Štěpánek et al. [54] | 1 | |
| France | Gagneux-Brunon et al., Moirangthem et al., Navarre et al., Paris(a) et al., Paris(b) et al. [21,39,42,47,48] | 5 | |
| Germany | Nohl et al., Presotto et al. [43,50] | 2 | |
| Greece | Fotiadis et al., Galanis et al., Maltezou et al., Papagiannis et al., Patelarou et al., Raftopolous et al. [20,22,36,45,49,51] | 6 | |
| Italy | Di Gennaro et al., Di Valerio et al., Monami et al., Papini et al. [14,15,40,46] | 4 | |
| Kosovo | Patelarou et al. [49] | 1 | |
| Slovakia | Ulbrichtova et al. [56] | 1 | |
| Spain | Mena et al., Patelarou et al. [38,49] | 2 | |
| Switzerland | Zürcher et al. [63] | 1 | |
| UK | Abuown et al., Woolf (a) et al., Woolf (b) et al. [10,58,59] | 3 | |
| Middle East | Azerbaijan | Doran et al. [17] | 1 |
| Iraq | Al-Metwali et al. [11] | 1 | |
| Israel | Zaitoon et al. [62] | 1 | |
| Lebanon | Nasr et al., Youssef et al. [41,61] | 2 | |
| Palestine | Maraqa et al. [37] | 1 | |
| Saudi Arabia | Baghdadi et al. [13] | 1 | |
| Turkey | Gönüllü et al., Kara Esen et al., İkiışık et al., Okuyan et al. [24,26,27,44] | 4 | |
| UAE | Saddik et al. [52] | 1 | |
| Africa | Egypt | Elkhayat et al. [18] | 1 |
| Tunisia | Kefi et al. [28] | 1 | |
| Asia | China | Leung et al., Kwok et al., Sun et al., Wang et al., Ye et al. [31,33,55,57,60] | 5 |
| India | Ashok et al. [12] | 1 | |
| Singapore | Koh et al. [30] | 1 | |
| North America | US | Do et al., Gatto et al. [16,23] | 2 |
| Reviews/Multi-Country Study/Report | Biswas et al., Hajure et al., Khubchandani et al., Leigh et al., Li et al., Luo et al., Shakeel et al., Report by PAHO [8,25,29,32,34,35,53,64] | 8 |
| Positive Factors | Total Studies (n) | Country |
|---|---|---|
| Protection of Others | 15 | Cyprus, Czech Republic, France, Greece, US, Egypt, Tunisia, Singapore, Lebanon, Palestine, UAE |
| Control Pandemic/Disease | 11 | Cyprus, China, Czech Republic, Egypt, France, Greece, Lebanon, Switzerland, Turkey, UAE |
| Protect Themselves | 11 | Cyprus, Greece, Switzerland, Egypt, Tunisia, China, Singapore, Lebanon |
| Knowledge of COVID-19 and the Vaccine | 11 | Albania, Cyprus, Greece, Kosovo, Spain, US, China, Azerbaijan, Lebanon |
| Increased Perception of Risk | 11 | France, China, Singapore, Saudi Arabia, UAE |
| Trust in Government and Health Authorities | 10 | Albania, Cyprus, Greece, Kosovo, Spain, Tunisia, China, Lebanon |
| Increased Fear of COVID-19 | 9 | Albania, Cyprus, Czech Republic, France, Greece, Kosovo, Spain, Lebanon, Palestine |
| Vaccine Safety | 9 | China, Greece, India, Azerbaijan, Saudi Arabia, Turkey |
| Increased Susceptibility to Disease | 6 | Switzerland, Egypt, China, Iraq, Lebanon, Palestine, Turkey |
| Negative Factors | ||
| Vaccine Safety/Side Effects | 32 | Albania, Cyprus, Czech Republic, France, Germany, Greece, Italy, Kosovo, Slovakia, Spain, Switzerland, UK, US, Tunisia, Lebanon, China, Palestine, Turkey, UAE |
| Effectiveness and Efficacy | 18 | Albania, Cyprus, Czech Republic, Greece, Italy, Kosovo, Slovakia, Spain, UK, US, Tunisia, China, Lebanon, Palestine, Turkey |
| Previous COVID-19 Infection | 16 | Albania, Cyprus, Czech Republic, France, Greece, Italy, Kosovo, Slovakia, Spain, UK, US, Egypt, Azerbaijan, Lebanon, Turkey |
| Quick Vaccine Development | 11 | Cyprus, France, Greece, Italy, UK, India, Lebanon |
| Lack of Trust | 11 | Cyprus, Czech Republic, Greece, Italy, UK, Turkey |
| Lack of Information/Knowledge | 10 | Cyprus, Germany, Greece, India, Palestine |
| Misinformation | 7 | Switzerland, Egypt, Palestine |
| Infection not Severe/Harmful to Self | 6 | Cyprus, Switzerland, Egypt, UAE |
| Vaccine Content | 4 | France, Italy, Lebanon, Turkey |
| Vaccine Novelty | 4 | US |
| Wanting Others to take it First | 4 | US |
| Insufficient Time | 3 | Egypt, China |
| Vaccine Approval Process | 2 | Cyprus |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ghare, F.; Meckawy, R.; Moore, M.; Lomazzi, M. Determinants of Acceptance of COVID-19 Vaccination in Healthcare and Public Health Professionals: A Review. Vaccines 2023, 11, 311. https://doi.org/10.3390/vaccines11020311
Ghare F, Meckawy R, Moore M, Lomazzi M. Determinants of Acceptance of COVID-19 Vaccination in Healthcare and Public Health Professionals: A Review. Vaccines. 2023; 11(2):311. https://doi.org/10.3390/vaccines11020311
Chicago/Turabian StyleGhare, Fathema, Rehab Meckawy, Michael Moore, and Marta Lomazzi. 2023. "Determinants of Acceptance of COVID-19 Vaccination in Healthcare and Public Health Professionals: A Review" Vaccines 11, no. 2: 311. https://doi.org/10.3390/vaccines11020311
APA StyleGhare, F., Meckawy, R., Moore, M., & Lomazzi, M. (2023). Determinants of Acceptance of COVID-19 Vaccination in Healthcare and Public Health Professionals: A Review. Vaccines, 11(2), 311. https://doi.org/10.3390/vaccines11020311






