Vaccine Communication: Appeals and Messengers Most Effective for COVID-19 Vaccine Uptake in Ukraine
Abstract
1. Introduction
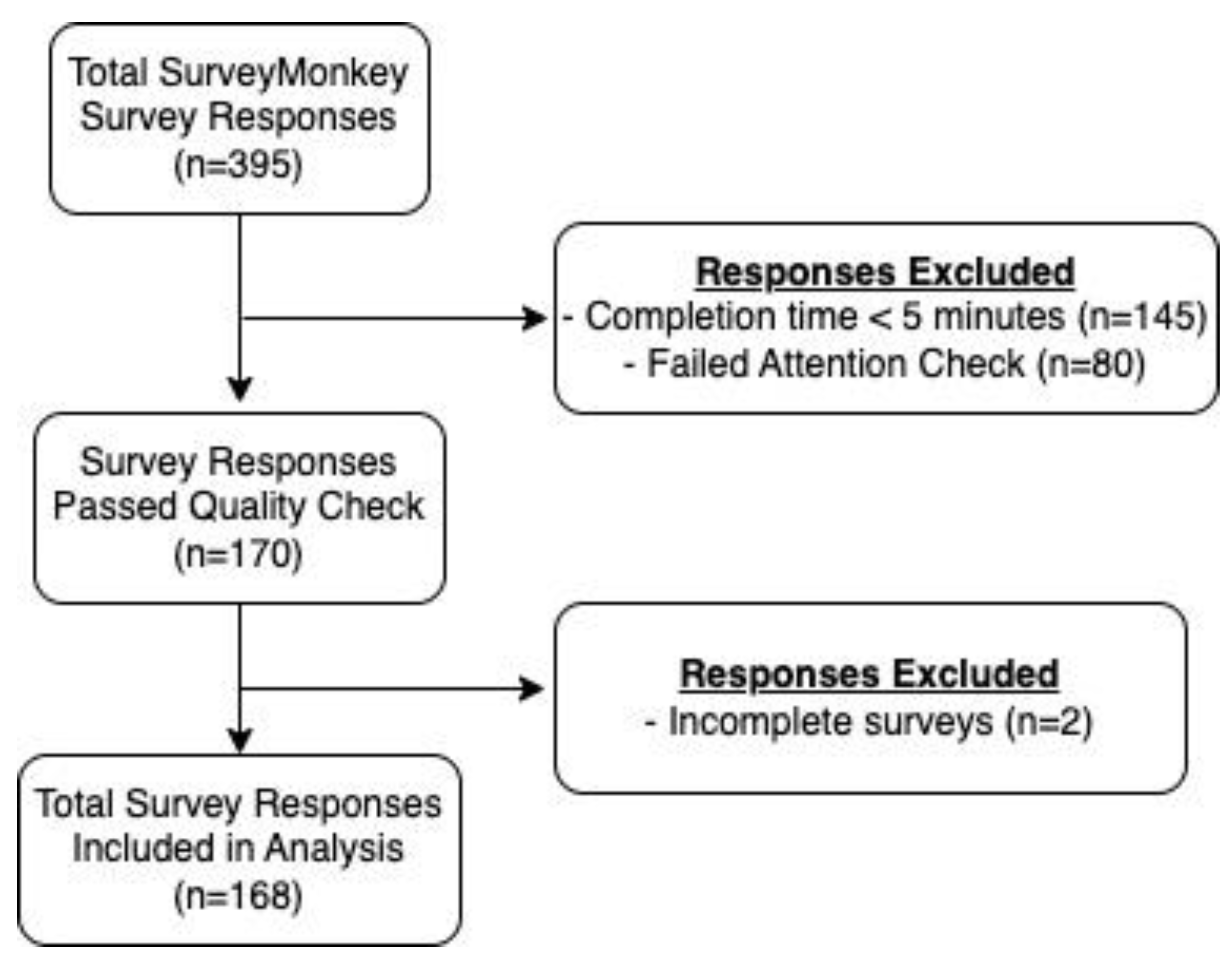
2. Methods
2.1. Survey Items
2.2. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A. Messaging Appeal Images

| Adjusted Relative Risk Ratios (95% CI) | |||||
|---|---|---|---|---|---|
| Health Outcome Peer | Economic Healthcare Provider | Economic Peer | Social Norm Healthcare Provider | Social Norm Peer | |
| Vaccine hesitancy | |||||
| Lower | Ref | Ref | Ref | Ref | Ref |
| Higher | 1.53 (0.35, 6.63) | 1.84 (0.44, 7.66) | Too small | 0.63 (0.22, 1.87) | 1.06 (0.23, 4.83) |
| Age | |||||
| <40 | Ref | Ref | Ref | Ref | Ref |
| 40+ | 0.57 (0.16, 2.06) | 0.79 (0.26, 2.44) | 2.87 (0.70, 11.86) | 1.77 (0.68, 4.62) | 1.53 (0.41, 5.63) |
| Gender | |||||
| Female | Ref | Ref | Ref | Ref | Ref |
| Male | 0.55 (0.19, 1.58) | 0.77 (0.29, 2.00) | 0.50 (0.12, 2.08) | 0.95 (0.38, 2.35) | 0.21 (0.05, 0.87) |
| Education | |||||
| Secondary | Ref | Ref | Ref | Ref | Ref |
| Bachelor’s Degree | Too small | 3.50 (0.81, 15.04) | 1.13 (0.16, 8.12) | 1.30 (0.37, 4.57) | 0.49 (0.07, 3.47) |
| Graduate Degree | Too small | 2.51 (0.58, 10.85) | 1.58 (0.25, 9.83) | 1.43 (0.47, 5.07) | 1.84 (0.40, 8.43) |
References
- Rozek, L.S.; Jones, P.; Menon, A.; Hicken, A.; Apsley, S.; King, E.J. Understanding Vaccine Hesitancy in the Context of COVID-19: The Role of Trust and Confidence in a Seventeen-Country Survey. Int. J. Public Health 2021, 66, 636255. [Google Scholar] [CrossRef] [PubMed]
- Lazarus, J.V.; Wyka, K.; White, T.M.; Picchio, C.A.; Rabin, K.; Ratzan, S.C.; Parsons Leigh, J.; Hu, J.; El-Mohandes, A. Revisiting COVID-19 vaccine hesitancy around the world using data from 23 countries in 2021. Nat. Commun. 2022, 13, 3801. [Google Scholar] [CrossRef] [PubMed]
- Relief Web. Global Rise in Vaccine-Preventable Diseases Highlights Urgent Actions Needed to Save Lives and Alleviate Future Suffering. Available online: https://reliefweb.int/report/world/global-rise-vaccine-preventable-diseases-highlights-urgent-actions-needed-save-lives (accessed on 19 September 2022).
- Puri, N.; Coomes, E.A.; Haghbayan, H.; Gunaratne, K. Social media and vaccine hesitancy: New updates for the era of COVID-19 and globalized infectious diseases. Hum. Vaccin. Immunother. 2020, 16, 2586–2593. [Google Scholar] [CrossRef] [PubMed]
- Cascini, F.; Pantovic, A.; Al-Ajlouni, Y.; Failla, G.; Ricciardi, W. Attitudes, acceptance and hesitancy among the general population worldwide to receive the COVID-19 vaccines and their contributing factors: A systematic review. EClinicalMedicine 2021, 40, 101113. [Google Scholar] [CrossRef]
- Holt, E. COVID-19 vaccination in Ukraine. Lancet Infect. Dis. 2021, 21, 462. [Google Scholar] [CrossRef]
- Hill, M.; Vanderslott, S.; Volokha, A.; Pollard, A.J. Addressing vaccine inequities among Ukrainian refugees. Lancet Infect. Dis. 2022, 22, 935–936. [Google Scholar] [CrossRef]
- Sallam, M.; Al-Sanafi, M. A Global Map of COVID-19 Vaccine Acceptance Rates per Country: An Updated Concise Narrative Review. J. Multidiscip. Healthc. 2022, 15, 21–45. [Google Scholar] [CrossRef]
- Zoaib Habib, T.; Ennab, F.; Matiashova, L.; Nawaz, F.A.; Volkova, A.; Trill, V.; Essar, M.Y. Double trouble: COVID-19 vaccine misinformation amidst conflict in Ukraine. Ann. Med. Surg. 2022, 80, 104127. [Google Scholar] [CrossRef]
- Benham, J.L.; Lang, R.; Kovacs Burns, K.; MacKean, G.; Léveillé, T.; McCormack, B.; Sheikh, H.; Fullerton, M.M.; Tang, T.; Boucher, J.C.; et al. Attitudes, current behaviours and barriers to public health measures that reduce COVID-19 transmission: A qualitative study to inform public health messaging. PLoS ONE 2021, 16, e0246941. [Google Scholar] [CrossRef]
- Holroyd, T.A.; Oloko, O.K.; Salmon, D.A.; Omer, S.B.; Limaye, R.J. Communicating Recommendations in Public Health Emergencies: The Role of Public Health Authorities. Health Secur. 2020, 18, 21–28. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.; Whetten, K.; Omer, S.; Pan, W.; Salmon, D. Hurdles to herd immunity: Distrust of government and vaccine refusal in the US, 2002-2003. Vaccine 2016, 34, 3972–3978. [Google Scholar] [CrossRef]
- Dubé, E.; Gagnon, D.; MacDonald, N.E.; Sage Working Group on Vaccine Hesitancy. Strategies intended to address vaccine hesitancy: Review of published reviews. Vaccine 2015, 33, 4191–4203. [Google Scholar] [CrossRef] [PubMed]
- Limaye, R.J.; Holroyd, T.A.; Blunt, M.; Jamison, A.F.; Sauer, M.; Weeks, R.; Wahl, B.; Christenson, K.; Smith, C.; Minchin, J.; et al. Social media strategies to affect vaccine acceptance: A systematic literature review. Expert Rev. Vaccines 2021, 20, 959–973. [Google Scholar] [CrossRef]
- Broniatowski, D.A.; Dredze, M.; Ayers, J.W. "First Do No Harm": Effective Communication About COVID-19 Vaccines. Am. J. Public Health 2021, 111, 1055–1057. [Google Scholar] [CrossRef] [PubMed]
- Solís Arce, J.S.; Warren, S.S.; Meriggi, N.F.; Scacco, A.; McMurry, N.; Voors, M.; Syunyaev, G.; Malik, A.A.; Aboutajdine, S.; Adeojo, O.; et al. COVID-19 vaccine acceptance and hesitancy in low- and middle-income countries. Nat. Med. 2021, 27, 1385–1394. [Google Scholar] [CrossRef]
- Thomas, K.A.; Clifford, S. Validity and Mechanical Turk: An assessment of exclusion methods and interactive experiments. Comput. Hum. Behav. 2017, 77, 184–197. [Google Scholar] [CrossRef]
- Chandler, J.; Rosenzweig, C.; Moss, A.J.; Robinson, J.; Litman, L. Online panels in social science research: Expanding sampling methods beyond Mechanical Turk. Behav. Res. 2019, 51, 2022–2038. [Google Scholar] [CrossRef]
- Sethi, S.; Kumar, A.; Mandal, A.; Shaikh, M.; Hall, C.A.; Kirk, J.M.W.; Moss, P.; Brookes, M.J.; Basu, S. The UPTAKE study: Implications for the future of COVID-19 vaccination trial recruitment in UK and beyond. Trials 2021, 22, 296. [Google Scholar] [CrossRef]
- Wang, J.; Jing, R.; Lai, X.; Zhang, H.; Lyu, Y.; Knoll, M.D.; Fang, H. Acceptance of COVID-19 Vaccination during the COVID-19 Pandemic in China. Vaccines 2020, 8, 482. [Google Scholar] [CrossRef] [PubMed]
- UNICEF. 42 Percent of Unvaccinated Ukrainians are Ready to Get Vaccinated against COVID-19, UNICEF Study Says. 2021. Available online: https://www.unicef.org/ukraine/en/press-releases/42-percent-unvaccinated-ukrainians-are-ready-get-vaccinated-against-covid-19-unicef (accessed on 18 January 2023).
- Diament, S.M.; Kaya, A.; Magenheim, E.B. Frames that matter: Increasing the willingness to get the Covid-19 vaccines. Soc. Sci. Med. 2022, 292, 114562. [Google Scholar] [CrossRef] [PubMed]
- Hlatshwako, T.G.; Shah, S.J.; Kosana, P.; Adebayo, E.; Hendriks, J.; Larsson, E.C.; Hensel, D.J.; Erausquin, J.T.; Marks, M.; Michielsen, K.; et al. Online health survey research during COVID-19. Lancet Digit. Health 2021, 3, e76–e77. [Google Scholar] [CrossRef] [PubMed]
- Oh, N.L.; Biddell, C.B.; Rhodes, B.E.; Brewer, N.T. Provider communication and HPV vaccine uptake: A meta-analysis and systematic review. Prev. Med. 2021, 148, 106554. [Google Scholar] [CrossRef] [PubMed]
- Brewer, N.T. What Works to Increase Vaccination Uptake. Acad. Pediatr. 2021, 21, S9–S16. [Google Scholar] [CrossRef]
- Hadjipanayis, A.; van Esso, D.; Del Torso, S.; Dornbusch, H.J.; Michailidou, K.; Minicuci, N.; Pancheva, R.; Mujkic, A.; Geitmann, K.; Syridou, G.; et al. Vaccine confidence among parents: Large scale study in eighteen European countries. Vaccine 2020, 38, 1505–1512. [Google Scholar] [CrossRef]
| Characteristic | No. (%) |
|---|---|
| Age | |
| 18–24 | 28 (16.7%) |
| 24–39 | 91 (54.2%) |
| 40–64 | 45 (26.8%) |
| 65+ | 4 (2.3%) |
| Gender | |
| Female | 91 (54.8%) |
| Male | 75 (45.2%) |
| Prefer not to say | 2 (1.2%) |
| Education | |
| Secondary | 28 (16.7%) |
| Bachelor’s degree | 58 (34.5%) |
| Graduate degree | 70 (41.7%) |
| Other | 12 (7.1%) |
| Currently Pregnant | |
| No | 113 (67.3%) |
| Yes | 39 (23.2%) |
| Not applicable | 16 (9.5%) |
| COVID-19 Vaccinated | |
| No | 51 (30.4%) |
| Yes | 106 (63.1%) |
| It is not available in my country | 6 (3.5%) |
| I am not eligible to receive the vaccine | 5 (3.0%) |
| Vaccine Hesitancy | |
| Lower Hesitancy | 30 (17.9%) |
| Higher Hesitancy | 138 (82.1%) |
| Ever delayed recommended vaccine | |
| No | 86 (51.2%) |
| Yes | 63 (37.5%) |
| I do not know | 19 (11.3%) |
| Concerned COVID-19 vaccine might not prevent the disease | |
| Extremely/Moderately | 50 (29.8%) |
| Slightly/Not at all | 118 (70.2%) |
| Concerned COVID-19 vaccine might not be safe | |
| Extremely/Moderately | 40 (23.8%) |
| Slightly/Not at all | 128 (76.2%) |
| Concerned COVID-19 vaccine might not be safe for pregnant women | |
| Extremely/Moderately | 81 (48.2%) |
| Slightly/Not at all | 87 (51.8) |
| Concerned COVID-19 vaccine might not be safe for children | |
| Extremely/Moderately | 75 (44.6%) |
| Slightly/Not at all | 93 (55.4%) |
| Characteristic | Low Hesitancy No. (%) | High Hesitancy No. (%) | Total |
|---|---|---|---|
| Age | |||
| 18–24 | 5 (17.9%) | 23 (82.1%) | 28 (16.7%) |
| 24–39 | 14 (15.4%) | 77 (84.6%) | 91 (54.2%) |
| 40+ | 11 (22.4%) | 38 (77.6%) | 49 (29.2%) |
| Gender | |||
| Female | 17 (18.7%) | 74 (81.3%) | 91 (54.2%) |
| Male | 11 (22.4%) | 38 (77.6%) | 75 (44.6%) |
| Prefer not to say | - | - | 2 (1.2%) |
| Education | |||
| Secondary | 5 (17.9%) | 23 (82.1%) | 28 (16.7%) |
| Bachelor’s degree | 8 (13.8%) | 50 (86.2%) | 58 (34.5%) |
| Graduate degree | 15 (21.4%) | 55 (78.6%) | 70 (41.7%) |
| Other | - | - | 12 (7.1%) |
| Ad Preference | Frequency (%) |
|---|---|
| Health Outcome—Healthcare Provider | 53 (31.5%) |
| Health Outcome—Peer | 25 (14.9%) |
| Economic—Healthcare Provider | 29 (17.3%) |
| Economic—Peer | 11 (6.6%) |
| Social Norm—Healthcare Provider | 35 (20.8%) |
| Social Norm—Peer | 15 (8.9%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schulz, G.; Balgobin, K.; Michel, A.; Limaye, R.J. Vaccine Communication: Appeals and Messengers Most Effective for COVID-19 Vaccine Uptake in Ukraine. Vaccines 2023, 11, 279. https://doi.org/10.3390/vaccines11020279
Schulz G, Balgobin K, Michel A, Limaye RJ. Vaccine Communication: Appeals and Messengers Most Effective for COVID-19 Vaccine Uptake in Ukraine. Vaccines. 2023; 11(2):279. https://doi.org/10.3390/vaccines11020279
Chicago/Turabian StyleSchulz, Gretchen, Kristian Balgobin, Alexandra Michel, and Rupali J. Limaye. 2023. "Vaccine Communication: Appeals and Messengers Most Effective for COVID-19 Vaccine Uptake in Ukraine" Vaccines 11, no. 2: 279. https://doi.org/10.3390/vaccines11020279
APA StyleSchulz, G., Balgobin, K., Michel, A., & Limaye, R. J. (2023). Vaccine Communication: Appeals and Messengers Most Effective for COVID-19 Vaccine Uptake in Ukraine. Vaccines, 11(2), 279. https://doi.org/10.3390/vaccines11020279






