Vaccination and COVID-19 in Polish Dialysis Patients: Results from the European Clinical Dialysis Database
Abstract
:1. Background
2. Objective
3. Patients and Methods
3.1. Patients
3.2. Methods
3.3. Statistical Analysis
4. Results
5. Discussion
Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Benedetti, C.; Waldman, M.; Zaza, G.; Riella, L.V.; Cravedi, P. COVID-19 and the Kidneys: An Update. Front. Med. 2020, 7, 423. [Google Scholar] [CrossRef] [PubMed]
- WHO. Coronavirus Disease (COVID-2019) Situation Reports. 2020. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports (accessed on 1 August 2022).
- Wu, C.; Chen, X.; Cai, Y.; Xia, J.; Zhou, X.; Xu, S.; Huang, H.; Zhang, L.; Zhou, X.; Du, C.; et al. Risk Factors Associated With Acute Respiratory Distress Syndrome and Death in Patients With Coronavirus Disease 2019 Pneumonia in Wuhan, China. JAMA Intern. Med. 2020, 180, 934. [Google Scholar] [CrossRef] [PubMed]
- Hu, B.; Guo, H.; Zhou, P.; Shi, Z.-L. Characteristics of SARS-CoV-2 and COVID-19. Nat. Rev. Microbiol. 2021, 19, 141–154. [Google Scholar] [CrossRef] [PubMed]
- Betjes, M.G.H. Immune cell dysfunction and inflammation in end-stage renal disease. Nat. Rev. Nephrol. 2013, 9, 255–265. [Google Scholar] [CrossRef] [PubMed]
- Naicker, S.; Yang, C.-W.; Hwang, S.-J.; Liu, B.-C.; Chen, J.-H.; Jha, V. The Novel Coronavirus 2019 epidemic and kidneys. Kidney Int. 2020, 97, 824–828. [Google Scholar] [CrossRef]
- GUS Population. Size and Structure and Vital Statistics in Poland by Territorial Division. As of December 31, 2020. Available online: https://stat.gov.pl/en/topics/population/population/population-size-and-structure-and-vital-statistics-in-poland-by-territorial-division-as-of-december-31-2020,3,29.html (accessed on 14 August 2021).
- Website of the Republic of Poland, Coronavirus: Information and Recommendations. Available online: https://www.gov.pl/web/coronavirus (accessed on 16 August 2021).
- Tharwat, S.; Khairallah, M.K.; Nassar, M.K.; Nassar, D.K.; Nagy, E. Acceptance of COVID-19 vaccination among maintenance hemodialysis patients: An Egyptian survey study. Trop. Med. Health 2022, 50, 42. [Google Scholar] [CrossRef]
- Agur, T.; Zingerman, B.; Ben-Dor, N.; Alkeesh, W.; Steinmetz, T.; Rachamimov, R.; Korzets, A.; Rozen-Zvi, B.; Herman-Edelstein, M. Humoral Response to the Third Dose of BNT162b2 COVID-19 Vaccine among Hemodialysis Patients. Nephron 2022, 1–8. [Google Scholar] [CrossRef]
- Cappuccilli, M.; Semprini, S.; Fabbri, E.; Fantini, M.; Bruno, P.F.; Spazzoli, A.; Righini, M.; Flachi, M.; La Manna, G.; Sambri, V.; et al. Antibody Responses after Two Doses of COVID-19 mRNA Vaccine in Dialysis and Kidney Transplantation Patients Recovered from SARS-CoV-2 Infection. Medicina 2022, 58, 893. [Google Scholar] [CrossRef]
- Yang, I.N.; Lu, C.L.; Tang, H.J.; Kuo, Y.C.; Tsai, L.H.; Tu, K.C.; Wang, J.J.; Chien, C.C. Safety of ChAdOx1 nCoV-19 vaccination in patients with end-stage renal disease on hemodialysis. PLoS ONE 2022, 17, e0273676. [Google Scholar] [CrossRef]
- Attias, P.; Azzaoui, I.; El Karoui, K.; de La Selle, A.; Sokal, A.; Chappert, P.; Grimbert, P.; Fernandez, I.; Bouvier, M.; Samson, C.; et al. Immune Responses after a Third Dose of mRNA Vaccine Differ in Virus-Naive versus SARS-CoV-2–Recovered Dialysis Patients. Clin. J. Am. Soc. Nephrol. 2022, 17, 1008–1016. [Google Scholar] [CrossRef] [PubMed]
- Torres, R.; Toro, L.; Sanhueza, M.E.; Lorca, E.; Ortiz, M.; Pefaur, J.; Clavero, R.; Machuca, E.; Gonzalez, F.; Herrera, P.; et al. Clinical efficacy of SARS-CoV-2 vaccination in hemodialysis patients. Kidney Int. Rep. 2022; Epub ahead of print. [Google Scholar] [CrossRef]
- Haug, N.; Geyrhofer, L.; Londei, A.; Dervic, E.; Desvars-Larrive, A.; Loreto, V.; Pinior, B.; Thurner, S.; Klimek, P. Ranking the effectiveness of worldwide COVID-19 government interventions. Nat. Hum. Behav. 2020, 4, 1303–1312. [Google Scholar] [CrossRef]
- Wang, R.; Liao, C.; He, H.; Hu, C.; Wei, Z.; Hong, Z.; Zhang, C.; Liao, M.; Shui, H. COVID-19 in Hemodialysis Patients: A Report of 5 Cases. Am. J. Kidney Dis. 2020, 76, 141–143. [Google Scholar] [CrossRef] [PubMed]
- Jager, K.J.; Kramer, A.; Chesnaye, N.C.; Couchoud, C.; Sánchez-Álvarez, J.E.; Garneata, L.; Collart, F.; Hemmelder, M.H.; Ambühl, P.; Kerschbaum, J.; et al. Results from the ERA-EDTA Registry indicate a high mortality due to COVID-19 in dialysis patients and kidney transplant recipients across Europe. Kidney Int. 2020, 98, 1540–1548. [Google Scholar] [CrossRef] [PubMed]
- Debska-Slizien, A.; Rutkowski, B.; Rutkowski, P.; Jagodziński, P.; Korejwo, G.; Przygoda, J.; Lewandowska, D.; Czewiński, J.; Kamiński, A.; Gellert, R. Current status of renal replacement therapy in Poland in 2019. Nefrol. Dial. Pol. 2020, 24, 38–50. [Google Scholar]
- Puchalska-Reglińska, E.; Dębska-Ślizień, A.; Biedunkiewicz, B.; Tylicki, P.; Polewska, K.; Jagodziński, P.; Rutkowski, B.; Gellert, R.; Tylicki, L. Extremely High Mortality in COVID-19 Hemodialyzed Patients in before Anty-SARS-CoV-2 Vaccination Era. First Large Database Poland. Pol. Arch. Intern. Med. 2021, 131, 643–648. [Google Scholar]
- Sánchez-Álvarez, J.E.; Pérez Fontán, M.; Jiménez Martín, C.; Blasco Pelícano, M.; Cabezas Reina, C.J.; Sevillano Prieto, Á.M.; Melilli, E.; Crespo Barrios, M.; Macía Heras, M.; del Pino y Pino, M.D. Situación de la infección por SARS-CoV-2 en pacientes en tratamiento renal sustitutivo. Informe del Registro COVID-19 de la Sociedad Española de Nefrología (SEN). Nefrología 2020, 40, 272–278. [Google Scholar] [CrossRef]
- Bell, S.; Campbell, J.; McDonald, J.; O’Neill, M.; Watters, C.; Buck, K.; Cousland, Z.; Findlay, M.; Lone, N.I.; Metcalfe, W.; et al. COVID-19 in patients undergoing chronic kidney replacement therapy and kidney transplant recipients in Scotland: Findings and experience from the Scottish renal registry. BMC Nephrol. 2020, 21, 419. [Google Scholar] [CrossRef]
- Pio-Abreu, A.; Nascimento, M.M.D.; Vieira, M.A.; Neves, P.D.M.D.M.; Lugon, J.R.; Sesso, R. High mortality of CKD patients on hemodialysis with COVID-19 in Brazil. J. Nephrol. 2020, 33, 875–877. [Google Scholar] [CrossRef]
- Latz, C.A.; DeCarlo, C.; Boitano, L.; Png, C.Y.M.; Patell, R.; Conrad, M.F.; Eagleton, M.; Dua, A. Blood type and outcomes in patients with COVID-19. Ann. Hematol. 2020, 99, 2113–2118. [Google Scholar] [CrossRef] [PubMed]
- Carrero, J.J.; de Jager, D.J.; Verduijn, M.; Ravani, P.; De Meester, J.; Heaf, J.G.; Finne, P.; Hoitsma, A.J.; Pascual, J.; Jarraya, F.; et al. Cardiovascular and Noncardiovascular Mortality among Men and Women Starting Dialysis. Clin. J. Am. Soc. Nephrol. 2011, 6, 1722–1730. [Google Scholar] [CrossRef] [PubMed]
- Corbett, R.W.; Blakey, S.; Nitsch, D.; Loucaidou, M.; McLean, A.; Duncan, N.; Ashby, D.R. West London Renal and Transplant Centre Epidemiology of COVID-19 in an Urban Dialysis Center. J. Am. Soc. Nephrol. 2020, 31, 1815–1823. [Google Scholar] [CrossRef] [PubMed]
- Taji, L.; Thomas, D.; Oliver, M.J.; Ip, J.; Tang, Y.; Yeung, A.; Cooper, R.; House, A.A.; McFarlane, P.; Blake, P.G. COVID-19 in patients undergoing long-term dialysis in Ontario. Can. Med. Assoc. J. 2021, 193, E278–E284. [Google Scholar] [CrossRef] [PubMed]
- Barello, S.; Palamenghi, L.; Graffigna, G. Burnout and somatic symptoms among frontline healthcare professionals at the peak of the Italian COVID-19 pandemic. Psychiatry Res. 2020, 290, 113129. [Google Scholar] [CrossRef] [PubMed]
- Walczak, R.; Kludacz-Alessandri, M.; Hawrysz, L. Use of Telemedicine Technology among General Practitioners during COVID-19: A Modified Technology Acceptance Model Study in Poland. Int. J. Environ. Res. Public Health 2022, 19, 10937. [Google Scholar] [CrossRef]
- Gallego-Valcarce, E.; Shabaka, A.; Leon-Poo, M.; Gruss, E.; Acedo-Sanz, J.M.; Cordón, A.; Cases-Corona, C.; Fernandez-Juarez, G. Humoral Response Following Triple Dose of mRNA Vaccines Against SARS-CoV-2 in Hemodialysis Patients: Results After 1 Year of Follow-Up. Front. Med. 2022, 12, 927546. [Google Scholar] [CrossRef]
- Piotrowska, M.; Zieliński, M.; Tylicki, L.; Biedunkiewicz, B.; Kubanek, A.; Ślizień, Z.; Polewska, K.; Tylicki, P.; Muchlado, M.; Sakowska, J.; et al. Local and Systemic Immunity Are Impaired in End-Stage-Renal-Disease Patients Treated With Hemodialysis, Peritoneal Dialysis and Kidney Transplant Recipients Immunized With BNT162b2 Pfizer-BioNTech SARS-CoV-2 Vaccine. Front. Immunol. 2022, 22, 832924. [Google Scholar] [CrossRef]
- Dimitrov, Y.; Krummel, T.; Chantrel, F.; Faller, A.L.; Ott, J.; David, D.; Bazin-Kara, D.; Hannedouche, T.; Borni, C. Protective antibody response to mRNA-1273 and BNT162b2 vaccines in patients on maintenance haemodialysis: A prospective cohort study. Clin. Kidney J. 2022, 15, 1720–1726. [Google Scholar] [CrossRef]
- Esposito, P.; Picciotto, D.; Cappadona, F.; Russo, E.; Falqui, V.; Conti, N.E.; Parodi, A.; Mallia, L.; Cavagnaro, S.; Battaglia, Y.; et al. The Evolving Scenario of COVID-19 in Hemodialysis Patients. Int. J. Environ. Res. Public Health 2022, 19, 10836. [Google Scholar] [CrossRef]
| Hemodialysis Population in 2019 | Hemodialysis Population in 2020 | Hemodialysis Population in 2021 | Adult General Population 2020 [7,8] | Adult General Population 2021 | |
|---|---|---|---|---|---|
| Overall adult population, n | 5901 | 5886 | 5534 | 32,139,021 | 31,223,400 |
| COVID-19 cases, n | N/A B | 1493 | 1224 | 1,294,878 | 2,813,449 |
| COVID-19 deaths, n | N/A B | 191 | 260 | 28,554 | 67,698 |
| Overall deaths, n | 1089 | 1426 | 1603 | 477,355 | 518,664 |
| Deaths without COVID, n | 1089 | 1235 | 1343 | 448,801 | 450,966 |
| Mean age of deceased patients, y (SD) | 72.59 (12.38) | 72.01 (12.34) | 71.41 (12.41) | 76.65 (N/D) A | 72.61 |
| COVID-19 mortality rate per 1000, crude | N/A B | 31.91 | 47.28 | 0.88 | 2.16 |
| Mortality rate per 1000 excluding COVID-19, crude | 184.54 | 206.32 | 244.22 | 13.96 | 14.44 |
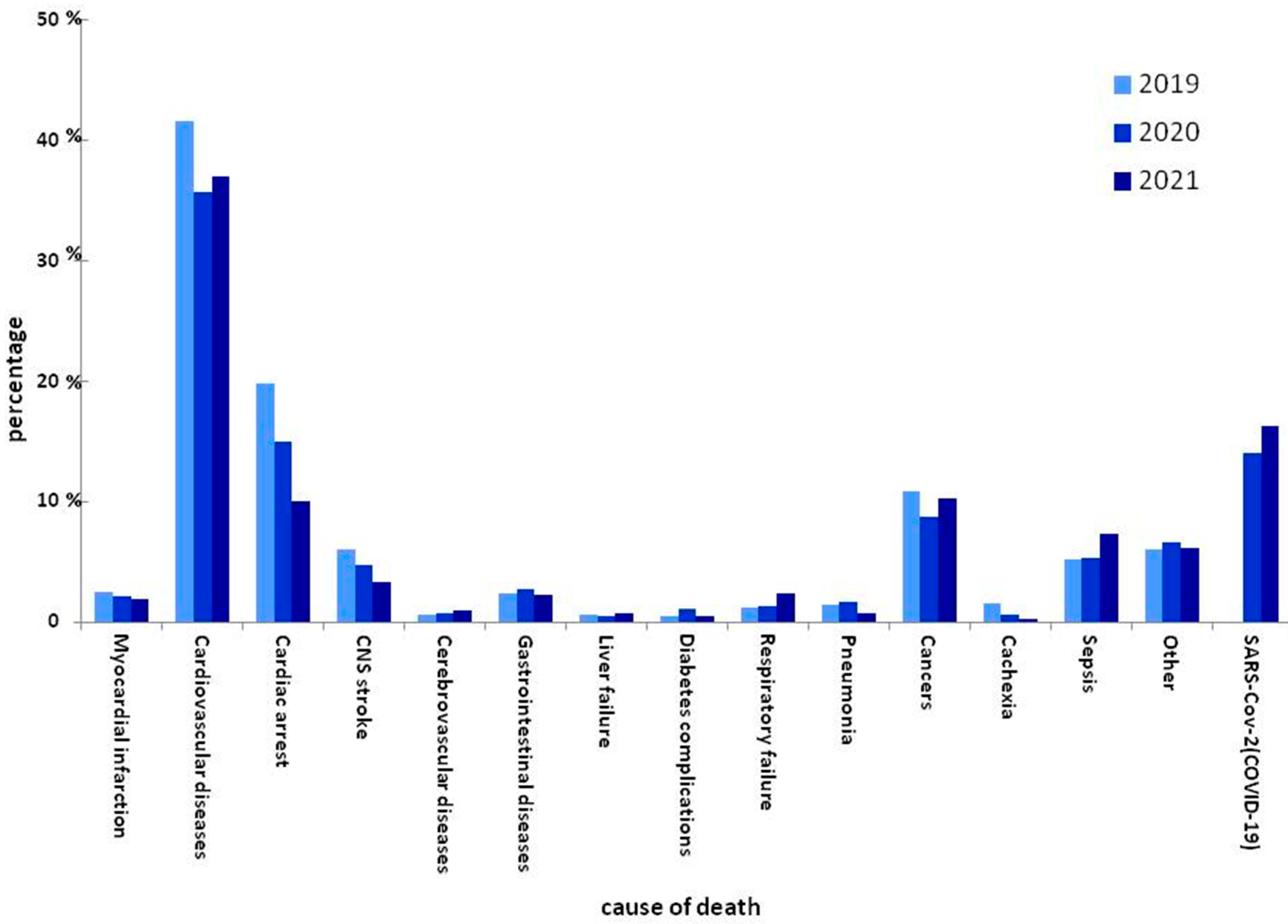
| Cause | Hemodialysis Population in 2019 | % | Hemodialysis Population in 2020 | % | Hemodialysis Population in 2021 | % | Hemodialysis Population in 2020 (%) without COVID Deaths | Hemodialysis Population in 2021 (%) without COVID Deaths | The Proportion of Deaths without COVID in 2020 to the Proportion of Deaths in 2019 | The Proportion of Deaths without COVID in 2021 to the Proportion of Deaths in 2020 |
|---|---|---|---|---|---|---|---|---|---|---|
| Myocardial infraction | 27 | 2.48% | 30 | 2.10% | 30 | 1.87% | 2.43% | 2.23% | 1.0 | 1.2 |
| Cardiovascular Diseases | 453 | 41.60% | 508 | 35.62% | 593 | 36.99% | 41.13% | 44.15% | 1.0 | 1.1 |
| Cardiac arrest | 215 | 19.74% | 214 | 15.01% | 161 | 10.04% | 17.33% | 11.99% | 0.9 | 0.7 |
| CNS Stroke | 66 | 6.06% | 67 | 4.70% | 53 | 3.31% | 5.43% | 3.95% | 0.9 | 0.7 |
| Cerebrovascular diseases | 6 | 0.55% | 10 | 0.70% | 16 | 1.00% | 0.81% | 1.19% | 1.5 | 1.5 |
| Gastrointestinal diseases | 26 | 2.39% | 39 | 2.73% | 36 | 2.25% | 3.16% | 2.68% | 1.3 | 0.8 |
| Liver failure | 7 | 0.64% | 6 | 0.42% | 12 | 0.75% | 0.49% | 0.89% | 0.8 | 1.8 |
| Diabetes complications | 5 | 0.46% | 15 | 1.05% | 8 | 0.50% | 1.21% | 0.60% | 2.6 | 0.5 |
| Respiratory failure | 13 | 1.19% | 18 | 1.26% | 38 | 2.37% | 1.46% | 2.83% | 1.2 | 1.9 |
| Pneumonia | 15 | 1.38% | 24 | 1.68% | 11 | 0.69% | 1.94% | 0.82% | 1.4 | 0.4 |
| Cancers | 118 | 10.84% | 125 | 8.77% | 164 | 10.23% | 10.12% | 12.21% | 0.9 | 1.2 |
| Cachexia | 17 | 1.56% | 9 | 0.63% | 4 | 0.25% | 0.73% | 0.30% | 0.5 | 0.4 |
| Sepsis | 56 | 5.14% | 76 | 5.33% | 118 | 7.36% | 6.15% | 8.79% | 1.2 | 1.4 |
| Other | 65 | 5.97% | 94 | 6.59% | 99 | 6.18% | 7.61% | 7.37% | 1.3 | 1.0 |
| SARS-CoV-2 (COVID-19) | N/A | N/A | 191 | 13.39% | 260 | 16.22% | N/A | N/A | 1.0 | 1.0 |
| Total | 1089 | 100% | 1426 | 100% | 1603 | 100% | 100% | 100% | N/A | N/A |
| Basal Data | Year | ||
|---|---|---|---|
| 2019 | 2020 | 2021 | |
| Deaths (n) | 1089 | 1426 | 1603 |
| Annual numer of patients | 5901 | 5886 | 5534 |
| Mortality (%) | 18.5 | 23.8 ** | 28.96 *** |
| COVID-19 deaths (n) | 0 | 191 | 260 |
| Mortality without COVID-19 (%) | 18.5 | 20.6 * | 24.26 ** |
| 2019 | Mortality Total | COVID | 2020 | Mortality Total | COVID | 2021 | Mortality Total | COVID |
|---|---|---|---|---|---|---|---|---|
| Age <45 | 25 | 0 | <45 | 52 | 3 | <45 | 53 | 2 |
| Age 45–64 | 214 | 0 | 45–64 | 268 | 37 | 45–64 | 363 | 32 |
| Age ≥65 | 850 | 0 | ≥65 | 1106 | 151 | ≥65 | 1188 | 154 |
| 2019 | 2020 | 2021 | 2020 without Patients Died of COVID-19 | 2021 without Patients Died of COVID-19 | 2020 Died of COVID-19 | 2021 Died of COVID-19 | |
|---|---|---|---|---|---|---|---|
| Patients, n | 1089 | 1426 | 1603 | 1235 | 1343 | 191 | 260 |
| Mean age, y (SD) | 72.59 (12.38) | 72.01 (12.34) | 71.4 (12.42) | 71.91 (13) | 72.26 (12.46) | 72.67 (11) | 72.26 (11.76) |
| Time from the onset of RRT to death (months) | 58 | 61 | 50 | 61 | 49 | 62 | 56 |
| Time from the start of RRT in the unit (months) | 48 | 51 | 50 | 51 | 49 | 54 | 56 |
| Time from diagnosis of kidney disease (months) | 81 | 94 | 71 | 92 | 71 | 101 | 69 |
| Female, n | 418 | 580 | 642 | 504 | 532 | 76 | 110 |
| Female (%) | 38.4 | 40.7 | 40.0 | 40.8 | 39.6 | 39.8 | 42.3 |
| Male, n | 671 | 846 | 961 | 731 | 811 | 115 | 150 |
| Male (%) | 61.6 | 59.3 | 60.0 | 59.2 | 60.4 | 60.2 | 57.7 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marcinkowski, W.; Zuzda, K.; Zawierucha, J.; Prystacki, T.; Żebrowski, P.; Małyszko, J.S.; Wojtaszek, E.; Małyszko, J. Vaccination and COVID-19 in Polish Dialysis Patients: Results from the European Clinical Dialysis Database. Vaccines 2022, 10, 1565. https://doi.org/10.3390/vaccines10091565
Marcinkowski W, Zuzda K, Zawierucha J, Prystacki T, Żebrowski P, Małyszko JS, Wojtaszek E, Małyszko J. Vaccination and COVID-19 in Polish Dialysis Patients: Results from the European Clinical Dialysis Database. Vaccines. 2022; 10(9):1565. https://doi.org/10.3390/vaccines10091565
Chicago/Turabian StyleMarcinkowski, Wojciech, Konrad Zuzda, Jacek Zawierucha, Tomasz Prystacki, Paweł Żebrowski, Jacek S. Małyszko, Ewa Wojtaszek, and Jolanta Małyszko. 2022. "Vaccination and COVID-19 in Polish Dialysis Patients: Results from the European Clinical Dialysis Database" Vaccines 10, no. 9: 1565. https://doi.org/10.3390/vaccines10091565
APA StyleMarcinkowski, W., Zuzda, K., Zawierucha, J., Prystacki, T., Żebrowski, P., Małyszko, J. S., Wojtaszek, E., & Małyszko, J. (2022). Vaccination and COVID-19 in Polish Dialysis Patients: Results from the European Clinical Dialysis Database. Vaccines, 10(9), 1565. https://doi.org/10.3390/vaccines10091565








