The Coverage and Acceptance Spectrum of COVID-19 Vaccines among Healthcare Professionals in Western Tanzania: What Can We Learn from This Pandemic?
Abstract
:1. Introduction
2. Materials and Methods
3. Results
3.1. Demographic Characteristics and General Health Behavior of Participants
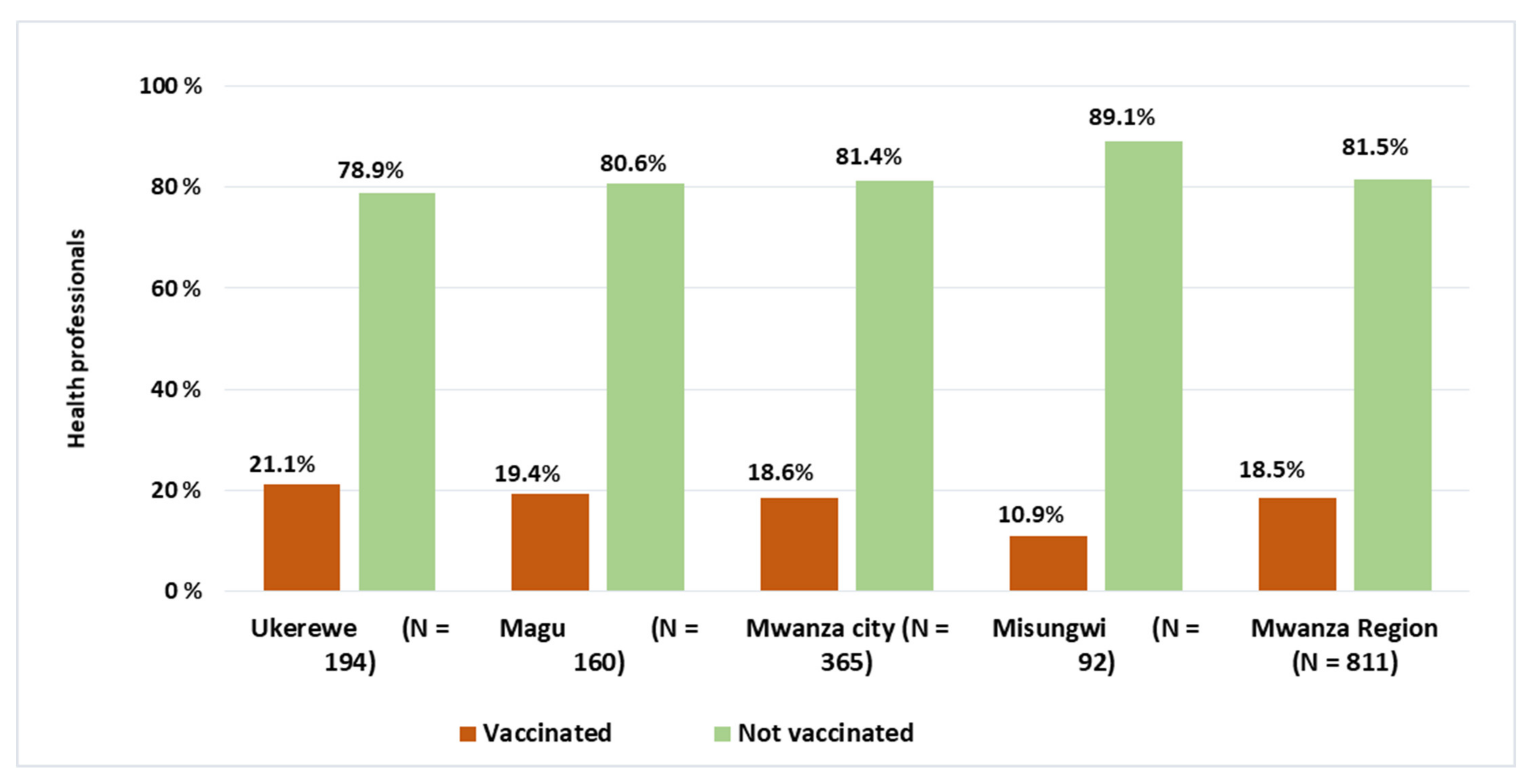
3.2. COVID-19 Vaccine Status among Health Professionals in Mwanza Western Tanzania
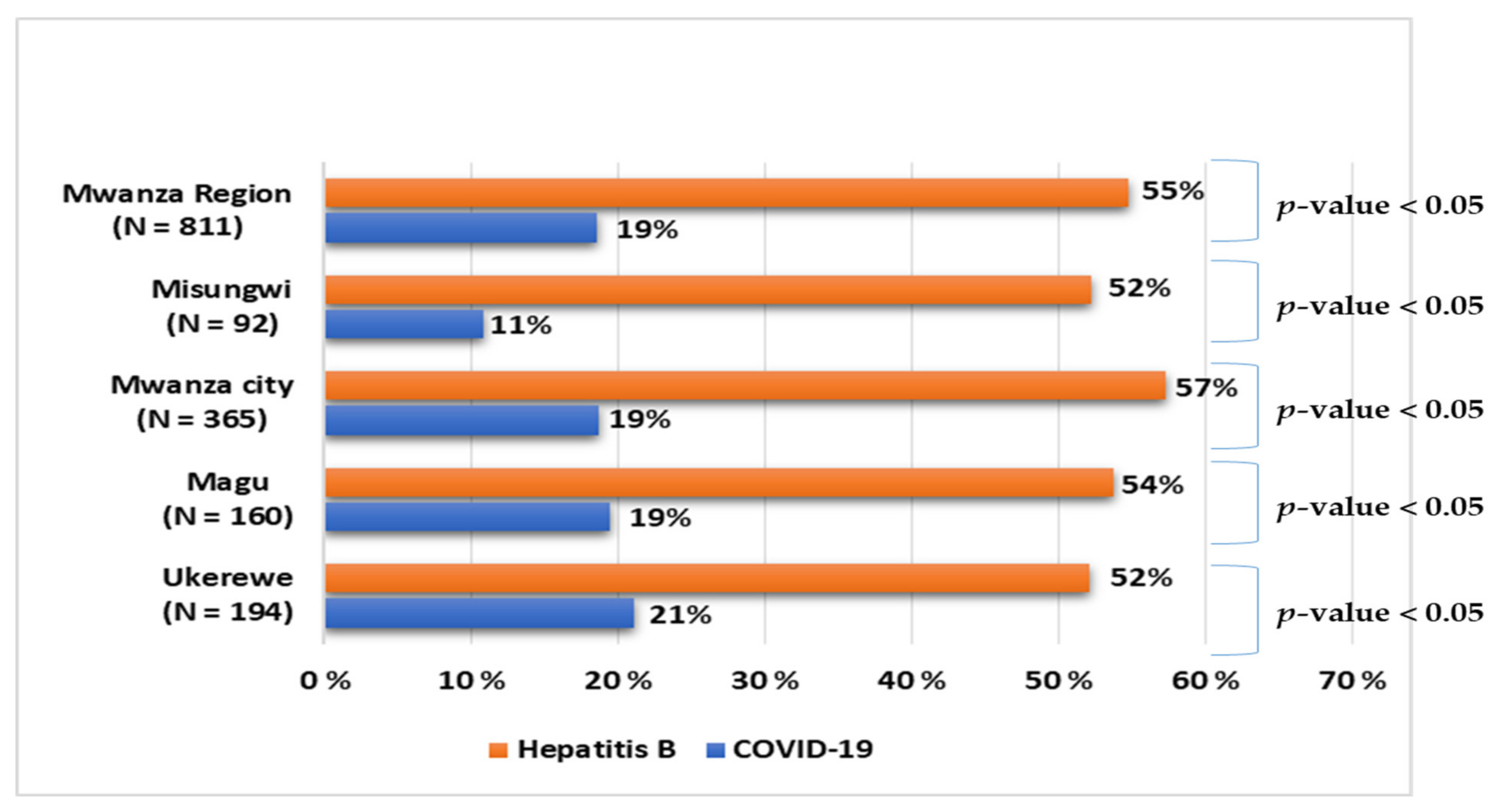
3.3. COVID-19 Vaccine Acceptance Level among Health Professionals in Western Tanzania
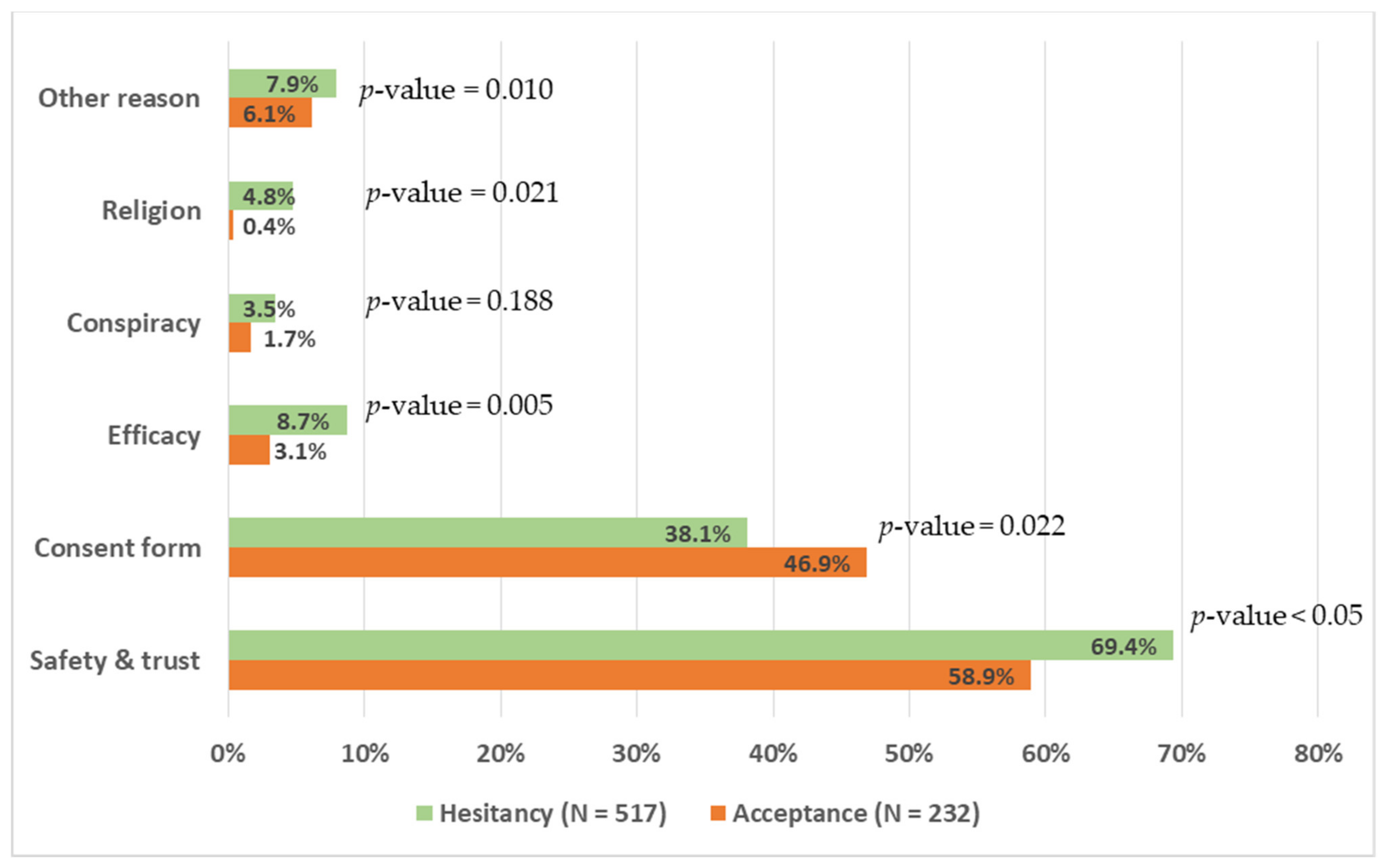
3.4. Perceived Barriers for Not Taking the COVID-19 Vaccine among Health Professionals
3.5. Factors Associated with Hesitancy of COVID-19 Vaccine among Health Professionals
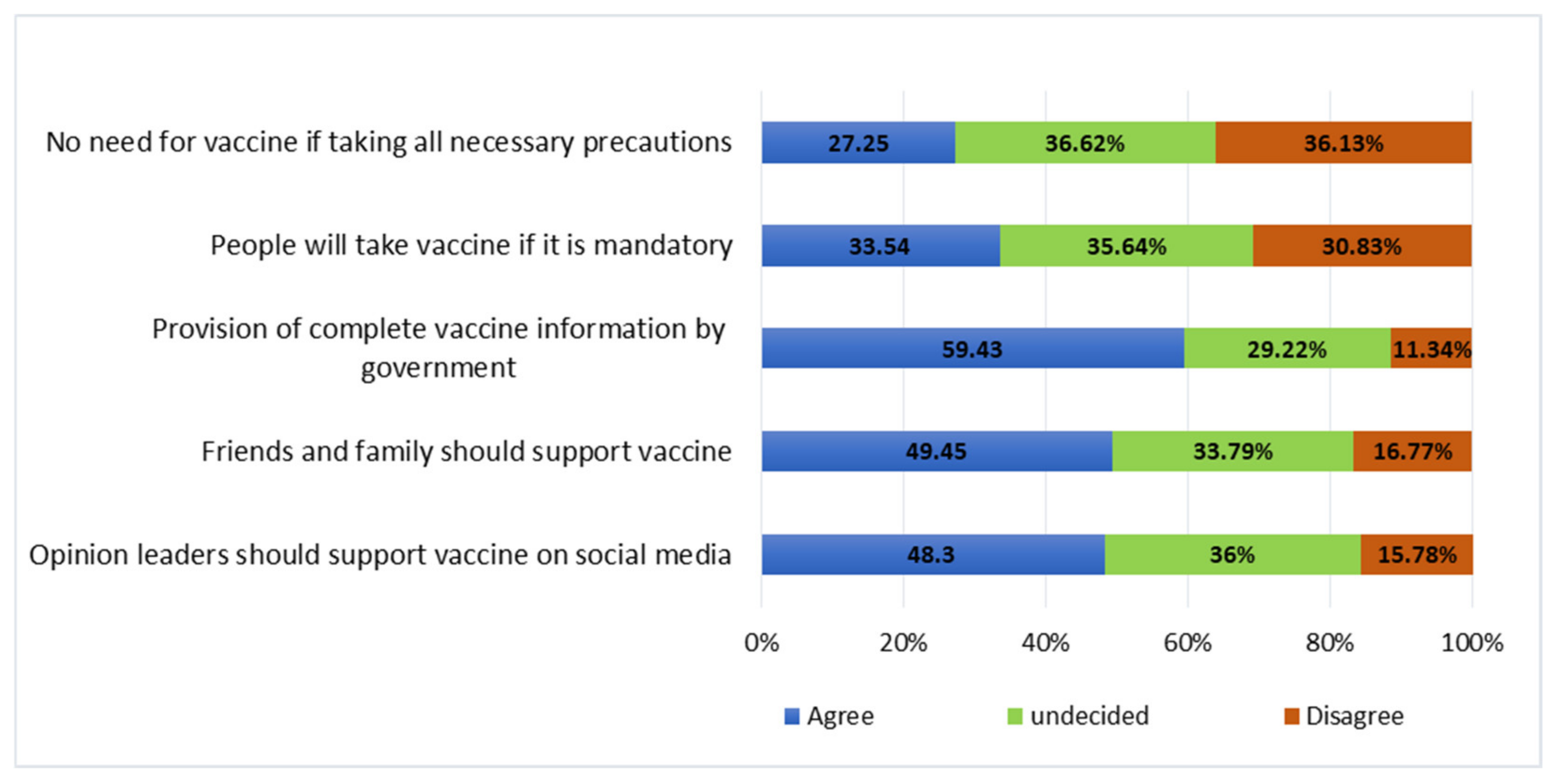
3.6. Cues for Actions on Improving COVID-19 Vaccine Uptake among Health Professionals
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. COVID-19 Weekly Epidemiological Update. 2022. Available online: https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19---22-june-2022 (accessed on 23 June 2022).
- Omer, S.B.; Salmon, D.A.; Orenstein, W.A.; Halsey, N. Vaccine Refusal, Mandatory Immunization, and the Risks of Vaccine-Preventable Diseases. N. Engl. J. Med. 2009, 360, 1981–1988. [Google Scholar] [CrossRef] [PubMed]
- WHO. Strategy to Achieve Global COVID-19 Vaccination by Mid-2022. 2022. Available online: https://cdn.who.int/media/docs/default-source/immunization/covid-19/strategy-to-achieve-global-covid-19-vaccination-by-mid-2022.pdf?sfvrsn=5a68433c_5 (accessed on 23 June 2022).
- Lazarus, J.V.; Ratzan, S.C.; Palayew, A.; Gostin, L.O.; Larson, H.J.; Rabin, K.; Kimball, S.; El-Mohandes, A. A global survey of potential acceptance of a COVID-19 vaccine. Nat. Med. 2021, 27, 225–228. [Google Scholar] [CrossRef] [PubMed]
- Lane, S.; MacDonald, N.E.; Marti, M.; Dumolard, L. Vaccine hesitancy around the globe: Analysis of three years of WHO/UNICEF Joint Reporting Form data-2015–2017. Vaccine 2018, 36, 3861–3867. [Google Scholar] [CrossRef] [PubMed]
- Altmann, D.M.; Douek, D.C.; Boyton, R.J. What policy makers need to know about COVID-19 protective immunity. Lancet 2020, 395, 1527–1529. [Google Scholar] [CrossRef]
- Mathieu, E.; Ritchie, H.; Ortiz-Ospina, E.; Roser, M.; Hasell, J.; Appel, C.; Giattino, C.; Rodés-Guirao, L. A global database of COVID-19 vaccinations. Nat. Hum. Behav. 2021, 5, 947–953. [Google Scholar] [CrossRef]
- World Health Organization (WHO); World Bank (WB); Vaccine Alliance; UNICEF; International Monetary Fund (IMF); World Trade Organization (WTO). Accelerating COVID-19 Vaccine Deployment: Removing Obstacles to Increase Coverage Levels and Protect Those at High Risk. 2022. Available online: https://www.who.int/publications/m/item/accelerating-covid-19-vaccine-deployment (accessed on 24 June 2022).
- Wang, Q.; Yang, L.; Jin, H.; Lin, L. Vaccination against COVID-19: A systematic review and meta-analysis of acceptability and its predictors. Prev. Med. 2021, 150. [Google Scholar] [CrossRef]
- MacDonald, N.E. Vaccine hesitancy: Definition, scope and determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef]
- Wallace, L.J.; Nouvet, E.; Bortolussi, R.; Arthur, J.A.; Amporfu, E.; Arthur, E.; Barimah, K.B.; Bitouga, B.A.; Chemusto, H.; Ikechebelu, J.; et al. COVID-19 in sub-Saharan Africa: Impacts on vulnerable populations and sustaining home-grown solutions. Can. J. Public Health 2020, 111, 649–653. [Google Scholar] [CrossRef]
- Mfinanga, S.G.; Mnyambwa, N.P.; Minja, D.T.; Ntinginya, N.E.; Ngadaya, E.; Makani, J.; Makubi, A.N. Tanzania’s postion on the COVID-19 pandemic. Lancet 2021, 387, 1542–1543. [Google Scholar] [CrossRef]
- Kish, L. Survey Sampling; John Wiley and Sons, Inc.: New York, NY, USA, 1965. [Google Scholar]
- Yendewa, S.A.; Ghazzawi, M.; James, P.B.; Smith, M.; Massaquoi, S.P.; Babawo, L.S.; Deen, G.F.; Russell, J.B.W.; Samai, M.; Sahr, F.; et al. COVID-19 Vaccine Hesitancy among Healthcare Workers and Trainees in Freetown, Sierra Leone: A Cross-Sectional Study. Vaccines 2022, 10, 757. [Google Scholar] [CrossRef]
- Rikitu, D.T.; Shama, A.T.; Feyisa, B.R.; Ewunetu, D.A.; Geta, E.T.; Chego, M.C.; Tamiru, E.A. COVID-19 Vaccine Uptake and Associated Factors Among Health Professionals in Ethiopia. Infect. Drug Resist. 2021, 14, 5531–5541. [Google Scholar] [CrossRef] [PubMed]
- Moucheraud, C.; Phiri, K.; Whitehead, H.S.; Songo, J.; Lungu, E.; Chikuse, E.; Phiri, S.; van Oosterhout, J.J.; Hoffman, R.M. Uptake of the COVID-19 vaccine among healthcare workers in Malawi. Int. Health 2022, ihac007. [Google Scholar] [CrossRef] [PubMed]
- Patwary, M.M.; Alam, M.A.; Bardhan, M.; Disha, A.S.; Haque, M.Z.; Billah, S.M.; Kabir, M.P.; Browning, M.H.E.M.; Rahman, M.M.; Parsa, A.D.; et al. COVID-19 Vaccine Acceptance among Low- and Lower-Middle-Income Countries: A Rapid Systematic Review and Meta-Analysis. Vaccines 2022, 10, 427. [Google Scholar] [CrossRef] [PubMed]
- Sallam, M.; Al-Sanafi, M.; Sallam, M. A Global Map of COVID-19 Vaccine Acceptance Rates per Country: An Updated Concise Narrative Review. J. Multidiscip. Healthc. 2022, 15, 21–45. [Google Scholar] [CrossRef] [PubMed]
- Ackah, M.; Ameyaw, L.; Gazali Salifu, M.; Afi Asubonteng, D.P.; Osei Yeboah, C.; Narkotey Annor, E.; Abena Kwartemaa Ankapong, E.; Boakye, H. COVID-19 vaccine acceptance among health care workers in Africa: A systematic review and meta-analysis. PLoS ONE 2022, 17, e0268711. [Google Scholar] [CrossRef]
- CDC. Latest Updates from Africa CDC on Progress Made in COVID-19 Vaccinations on the Continent. Available online: https://africacdc.org/covid-19-vaccination/ (accessed on 24 June 2022).
- Baniak, L.M.; Luyster, F.S.; Raible, C.A.; McCray, E.E.; Strollo, P.J. COVID-19 Vaccine Hesitancy and Uptake among Nursing Staff during an Active Vaccine Rollout. Vaccines 2021, 9, 858. [Google Scholar] [CrossRef]
- Bianchi, F.P.; Stefanizzi, P.; Brescia, N.; Lattanzio, S.; Martinelli, A.; Tafuri, S. COVID-19 vaccination hesitancy in Italian healthcare workers: A systematic review and meta-analysis. Expert Rev. Vaccines 2022, 1–12. [Google Scholar] [CrossRef]
- Dong, Y.; He, Z.; Liu, T.; Huang, J.; Zhang, C.J.P.; Akinwunmi, B.; Ming, W.K. Acceptance of and Preference for COVID-19 Vaccination in India, the United Kingdom, Germany, Italy, and Spain: An International Cross-Sectional Study. Vaccines 2022, 10, 832. [Google Scholar] [CrossRef]
- Dzieciolowska, S.; Hamel, D.; Gadio, S.; Dionne, M.; Gagnon, D.; Robitaille, L.; Cook, E.; Caron, I.; Talib, A.; Parkes, L.; et al. Covid-19 vaccine acceptance, hesitancy, and refusal among Canadian healthcare workers: A multicenter survey. Am. J. Infect. Control. 2021, 49, 1152–1157. [Google Scholar] [CrossRef]
- Holzmann-Littig, C.; Braunisch, M.C.; Kranke, P.; Popp, M.; Seeber, C.; Fichtner, F.; Littig, B.; Carbajo-Lozoya, J.; Allwang, C.; Frank, T.; et al. COVID-19 Vaccination Acceptance and Hesitancy among Healthcare Workers in Germany. Vaccines 2021, 9, 777. [Google Scholar] [CrossRef]
- Lavoie, K.; Gosselin-Boucher, V.; Stojanovic, J.; Gupta, S.; Gagné, M.; Joyal-Desmarais, K.; Séguin, K.; Gorin, S.S.; Ribeiro, P.; Voisard, B.; et al. Understanding national trends in COVID-19 vaccine hesitancy in Canada: Results from five sequential cross-sectional representative surveys spanning April 2020–March 2021. BMJ Open 2022, 12, e059411. [Google Scholar] [CrossRef] [PubMed]
- Adhikari, B.; Cheah, P.Y. Vaccine hesitancy in the COVID-19 era. Lancet Infect. Dis. 2021, 21, 1086. [Google Scholar] [CrossRef]
- Goldenberg, M.J. Public Misunderstanding of Science? Reframing the Problem of Vaccine Hesitancy. Perspect. Sci. 2016, 24, 552–581. [Google Scholar] [CrossRef]
- Wiysonge, C.S.; Ndwandwe, D.; Ryan, J.; Jaca, A.; Batouré, O.; Anya, B.-P.M.; Cooper, S. Vaccine hesitancy in the era of COVID-19: Could lessons from the past help in divining the future? Hum. Vaccines Immunother. 2022, 18, 1–3. [Google Scholar] [CrossRef]
- Lawal, L.; Aminu Bello, M.; Murwira, T.; Avoka, C.; Yusuf Ma’aruf, S.; Harrison Omonhinmin, I.; Maluleke, P.; Tsagkaris, C.; Onyeaka, H. Low coverage of COVID-19 vaccines in Africa: Current evidence and the way forward. Hum. Vaccines Immunother. 2022, 18, 2034457. [Google Scholar] [CrossRef]
- Kabakama, S.; Konje, E.T.; Dinga, J.N.; Kishamawe, C.; Morhason-Bello, I.; Hayombe, P.; Adeyemi, O.; Chimuka, E.; Lumu, I.; Amuasi, J.; et al. Commentary on COVID-19 Vaccine Hesitancy in sub-Saharan Africa. Trop. Med. Infect. Dis. 2022, 7, 130. [Google Scholar] [CrossRef]
- Kamazima, S.; Kakoko, D.; Kazaura, M. Manifold Tactics are used to Control and Prevent Pandemics in Contemporary Africa”: A Case of Tanzania’s Fight against COVID-19. Int. J. Adv. Sci. Res. Manag. 2020, 5, 20. [Google Scholar] [CrossRef]
- Wise, J. COVID-19: France and Greece Make Vaccination Mandatory for Healthcare Workers. BMJ 2021, 374, n1797. [Google Scholar] [CrossRef]
- Paterlini, M. COVID-19: Italy Makes Vaccination Mandatory for Healthcare Workers. BMJ 2021, 373, n905. [Google Scholar] [CrossRef]
- Rimmer, A. COVID Vaccination to Be Mandatory for NHS Staff in England from Spring 2022. BMJ 2021, 375, n2733. [Google Scholar] [CrossRef]
- Woolf, K.; Gogoi, M.; Martin, C.A.; Papineni, P.; Lagrata, S.; Nellums, L.B.; McManus, I.C.; Guyatt, A.L.; Melbourne, C.; Gupta, A.; et al. Healthcare workers’ views on mandatory SARS-CoV-2 vaccination in the UK: A cross-sectional, mixed-methods analysis from the UK-REACH study. eClinicalMedicine 2022, 46, 101346. [Google Scholar] [CrossRef]
- Smith, P.J.; Kennedy, A.M.; Wooten, K.; Gust, D.A.; Pickering, L.K. Association between health care providers’ influence on parents who have concerns about vaccine safety and vaccination coverage. Pediatrics 2006, 118, e1287-92. [Google Scholar] [CrossRef]
- Vorsters, A.; Bonanni, P.; Maltezou, H.C.; Yarwood, J.; Brewer, N.T.; Bosch, F.X.; Hanley, S.; Cameron, R.; Franco, E.L.; Arbyn, M.; et al. The role of healthcare providers in HPV vaccination programs—A meeting report. Papillomavirus Res. 2019, 8, 100183. [Google Scholar] [CrossRef]
- Troiano, G.; Nardi, A. Vaccine hesitancy in the era of COVID-19. Public Health 2021, 194, 245–251. [Google Scholar] [CrossRef]
- WHO. Coronavirus (COVID-19) Dashboard. Geneva: World Health Organization. 2020. Available online: https://covid19.who.int/ (accessed on 6 July 2022).
- Omer, S.B.; Benjamin, R.M.; Brewer, N.T.; Buttenheim, A.M.; Callaghan, T.; Caplan, A.; Carpiano, R.M.; Clinton, C.; DiResta, R.; Elharake, J.A.; et al. Promoting COVID-19 vaccine acceptance: Recommendations from the Lancet Commission on Vaccine Refusal, Acceptance, and Demand in the USA. Lancet 2021, 398, 2186–2192. [Google Scholar] [CrossRef]
- Kricorian, K.; Civen, R.; Equils, O. COVID-19 vaccine hesitancy: Misinformation and perceptions of vaccine safety. Hum. Vaccines Immunother. 2022, 18, 1950504. [Google Scholar] [CrossRef]
- Maraqa, B.; Nazzal, Z.; Rabi, R.; Sarhan, N.; Al-Shakhra, K.; Al-Kaila, M. COVID-19 vaccine hesitancy among health care workers in Palestine: A call for action. Prev. Med. 2021, 149, 106618. [Google Scholar] [CrossRef]
- Farshbafnadi, M.; Kamali Zonouzi, S.; Sabahi, M.; Dolatshahi, M.; Aarabi, M.H. Aging & COVID-19 susceptibility, disease severity, and clinical outcomes: The role of entangled risk factors. Exp. Gerontol. 2021, 154, 111507. [Google Scholar]
- Yanez, N.D.; Weiss, N.S.; Romand, J.-A.; Treggiari, M.M. COVID-19 mortality risk for older men and women. BMC Public Health 2020, 20, 1742. [Google Scholar] [CrossRef]
- Goel, A.; Gupta, L. Social Media in the Times of COVID-19. J. Clin. Rheumatol. 2020, 26, 220–223. [Google Scholar] [CrossRef]
- Machmud, P.B.; Glasauer, S.; Gottschick, C.; Mikolajczyk, R. Knowledge, Vaccination Status, and Reasons for Avoiding Vaccinations against Hepatitis B in Developing Countries: A Systematic Review. Vaccines 2021, 9, 625. [Google Scholar] [CrossRef] [PubMed]
- Kafeero, H.M.; Ndagire, D.; Ocama, P.; Kudamba, A.; Walusansa, A.; Sendagire, H. Prevalence and predictors of hepatitis B virus (HBV) infection in east Africa: Evidence from a systematic review and meta-analysis of epidemiological studies published from 2005 to 2020. Arch. Public Health 2021, 79, 167. [Google Scholar] [CrossRef] [PubMed]
- Atlaw, D.; Sahiledengle, B.; Tariku, Z. Hepatitis B and C virus infection among healthcare workers in Africa: A systematic review and meta-analysis. Environ. Health Prev. Med. 2021, 26, 61. [Google Scholar] [CrossRef] [PubMed]

| Characteristic | N (%) | Acceptance, N = 323 N (%) | Hesitancy, N = 579 N (%) | Chi2 p-Value |
|---|---|---|---|---|
| Level of health facility | ||||
| Tertiary hospital | 233 (28.7) | 63 (27.2) | 170 (29.4) | 0.001 |
| Regional hospital | 132 (16.3) | 20 (8.6) | 112 (19.3) | |
| District hospital | 214 (26.4) | 66 (28.5) | 148 (25.6) | |
| Health center | 184 (22.7) | 64 (27.6) | 120 (20.7) | |
| Dispensary | 48 (5.9) | 19 (8.2) | 29 (5.0) | |
| Age group | ||||
| Less than 30 years | 295 (36.4) | 60 (25.9) | 235 (40.6) | 0.000 |
| 30–49 years | 446 (55.0) | 135 (58.1) | 311 (53.7) | |
| 50 years and above | 70 (8.6) | 37 (16.0) | 33 (5.7) | |
| Gender | ||||
| Female | 388 (47.8) | 119 (51.3) | 269 (46.5) | 0.213 |
| Male | 423 (52.2) | 113 (48.7) | 310 (53.5) | |
| Education level | ||||
| Primary | 51 (6.3) | 22 (9.5) | 29 (5.0) | 0.011 |
| Secondary | 54 (6.7) | 22 (9.5) | 32 (5.5) | |
| Certificate/diploma | 419 (51.7) | 107 (46.1) | 312 (53.9) | |
| Degree/Master’s/PhD | 287 (35.4) | 81 (34.9) | 206 (35.6) | |
| Cadre | ||||
| Medical attendant | 105 (12.9) | 44 (18.9) | 61 (10.5) | 0.004 |
| Nurse/clinical officer | 419 (51.7) | 107 (46.1) | 312 (53.9) | |
| Doctor/specialist | 287 (35.4) | 81 (34.9) | 206 (35.6) | |
| Smoking status (yes) | 47 (5.8) | 15 (6.5) | 32 (5.5) | 0.605 |
| Exercise regularly (yes) | 465 (57.3) | 133 (57.3) | 332 (57.3) | 0.997 |
| Chronic conditions (yes) | 113 (13.9) | 45 (19.40) | 68 (11.7) | 0.004 |
| Name of conditions | ||||
| Hypertension | 51 (45.1) | |||
| Diabetes mellitus | 24 (21.2) | |||
| Asthma | 17 (15.0) | |||
| Heart disease | 7 (6.2) | |||
| Cancer | 4 (3.5) | |||
| Others | 10 (8.9) |
| Variable | Univariate Analysis | Multivariate Analysis | ||||
|---|---|---|---|---|---|---|
| OR | 95% C.I. | p Value | aOR | 95% C.I. | p-Value | |
| Sex | ||||||
| Female | 1 | |||||
| Male | 1.21 | 0.90–1.66 | 0.196 | |||
| Age group | ||||||
| ≥50 years | 1 | |||||
| 30–49 years | 2.58 | 1.55–4.31 | 0.000 | 2.20 | 1.28–3.76 | 0.004 |
| <30 years | 4.39 | 2.54–7.60 | 0.000 | 3.31 | 1.83–5.98 | 0.000 |
| Education level | ||||||
| Degree and above | 1 | |||||
| Certificate/Diploma | 1.15 | 0.82–1.61 | 0.428 | 1.45 | 0.99–2.12 | 0.055 |
| Primary/Secondary | 0.55 | 0.34–0.87 | 0.011 | 0.86 | 0.49–1.51 | 0.595 |
| Presence of chronic Disease | ||||||
| Yes | 1 | 1 | ||||
| No | 1.81 | 1.19–2.73 | 0.005 | 1.29 | 0.83–2.02 | 0.251 |
| Uptake of Hepatitis B vaccine | ||||||
| Yes | 1 | 1 | ||||
| No | 2.25 | 1.63–3.09 | 0.000 | 2.19 | 1.56–3.06 | 0.000 |
| Facility Level | ||||||
| Dispensary | 1 | |||||
| Health Center | 1.23 | 0.64–2.36 | 0.537 | 0.97 | 0.48–1.96 | 0.938 |
| Hospital | 1.89 | 1.03–3.47 | 0.040 | 1.66 | 0.83–3.31 | 0.151 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Konje, E.T.; Basinda, N.; Kapesa, A.; Mugassa, S.; Nyawale, H.A.; Mirambo, M.M.; Moremi, N.; Morona, D.; Mshana, S.E. The Coverage and Acceptance Spectrum of COVID-19 Vaccines among Healthcare Professionals in Western Tanzania: What Can We Learn from This Pandemic? Vaccines 2022, 10, 1429. https://doi.org/10.3390/vaccines10091429
Konje ET, Basinda N, Kapesa A, Mugassa S, Nyawale HA, Mirambo MM, Moremi N, Morona D, Mshana SE. The Coverage and Acceptance Spectrum of COVID-19 Vaccines among Healthcare Professionals in Western Tanzania: What Can We Learn from This Pandemic? Vaccines. 2022; 10(9):1429. https://doi.org/10.3390/vaccines10091429
Chicago/Turabian StyleKonje, Eveline T., Namanya Basinda, Anthony Kapesa, Stella Mugassa, Helmut A. Nyawale, Mariam M. Mirambo, Nyambura Moremi, Domenica Morona, and Stephen E. Mshana. 2022. "The Coverage and Acceptance Spectrum of COVID-19 Vaccines among Healthcare Professionals in Western Tanzania: What Can We Learn from This Pandemic?" Vaccines 10, no. 9: 1429. https://doi.org/10.3390/vaccines10091429
APA StyleKonje, E. T., Basinda, N., Kapesa, A., Mugassa, S., Nyawale, H. A., Mirambo, M. M., Moremi, N., Morona, D., & Mshana, S. E. (2022). The Coverage and Acceptance Spectrum of COVID-19 Vaccines among Healthcare Professionals in Western Tanzania: What Can We Learn from This Pandemic? Vaccines, 10(9), 1429. https://doi.org/10.3390/vaccines10091429






