Attitudes to Vaccine Mandates among Late Adopters of COVID-19 Vaccines in Zimbabwe
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Sites and Sampling
2.3. Statistical Analysis
2.4. Ethics Approvals
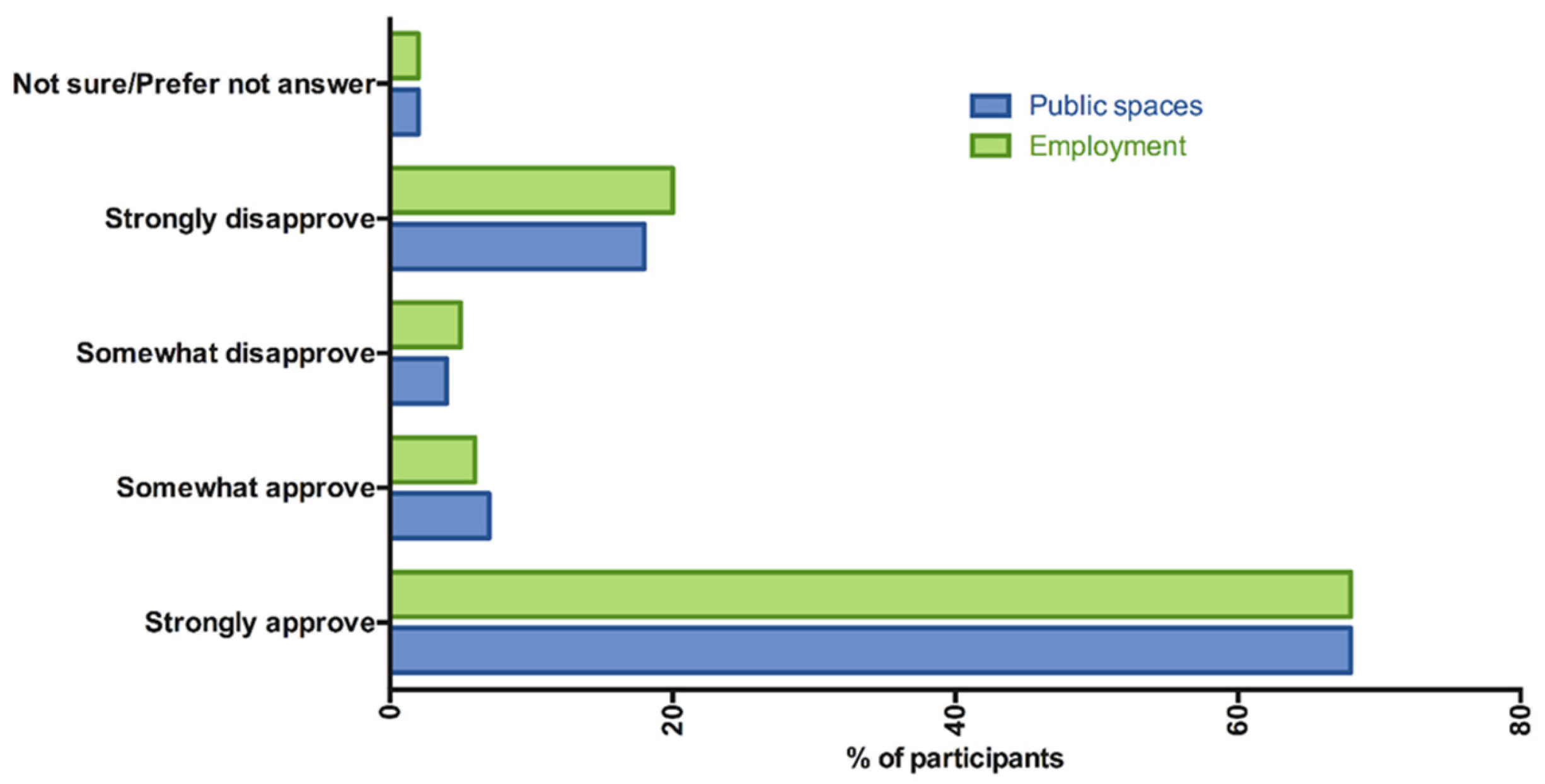
3. Results
4. Discussion
5. Strengths and Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Donnelly, C.A.; Ghani, A.C.; Leung, G.M.; Hedley, A.J.; Fraser, C.; Riley, S.; Abu-Raddad, L.J.; Ho, L.M.; Thach, T.Q.; Chau, P.; et al. Epidemiological determinants of spread of causal agent of severe acute respiratory syndrome in Hong Kong. Lancet 2003, 361, 1761–1766. [Google Scholar] [CrossRef] [Green Version]
- Mohd, H.A.; Al-Tawfiq, J.A.; Memish, Z.A. Middle East Respiratory Syndrome Coronavirus (MERS-CoV) origin and animal reservoir. Virol. J. 2016, 13, 87. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- WHO. Middle East Respiratory Syndrome Coronavirus (MERS CoV). 2022. Available online: https://www.who.int/health-topics/middle-east-respiratory-syndrome-coronavirus-mers#tab=tab_1 (accessed on 1 January 2020).
- World Health Organization. COVID-19 Vaccine Tracker and Landscape. 2022. Available online: https://www.who.int/publications/m/item/draft-landscape-of-covid-19-candidate-vaccines (accessed on 28 May 2022).
- World Health Organization. COVID-19 Vaccines. 2022. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/covid-19-vaccines (accessed on 28 May 2022).
- WHO Africa. WHO Africa Region Numbers at A Glance. 2022. Available online: https://www.afro.who.int/health-topics/coronavirus-covid-19 (accessed on 28 May 2022).
- Sallam, M.; Al-Sanafi, M.; Sallam, M. A Global Map of COVID-19 Vaccine Acceptance Rates per Country: An Updated Concise Narrative Review. J. Multidiscip. Healthc. 2022, 15, 21–45. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Report of the SAGE Working Group on Vaccine Hesitancy. Available online: http://www.who.int/immunization/sage/meetings/2014/october/1_Report_WORKING_GROUP_vaccine_hesitancy_final.pdf.2014 (accessed on 27 March 2022).
- Giannakou, K.; Kyprianidou, M.; Christofi, M.; Kalatzis, A.; Fakonti, G. Mandatory COVID-19 Vaccination for Healthcare Professionals and Its Association With General Vaccination Knowledge: A Nationwide Cross-Sectional Survey in Cyprus. Front. Public Health 2022, 10, 897526. [Google Scholar] [CrossRef] [PubMed]
- Graeber, D.; Schmidt-Petri, C.; Schroder, C. Attitudes on voluntary and mandatory vaccination against COVID-19: Evidence from Germany. PLoS ONE 2021, 16, e0248372. [Google Scholar] [CrossRef] [PubMed]
- Schmelz, K.; Bowles, S. Opposition to voluntary and mandated COVID-19 vaccination as a dynamic process: Evidence and policy implications of changing beliefs. Proc. Natl. Acad. Sci. USA 2022, 119, e2118721119. [Google Scholar] [CrossRef]
- Stead, M.; Ford, A.; Eadie, D.; Biggs, H.; Elliott, C.; Ussher, M.; Bedford, H.; Angus, K.; Hunt, K.; MacKintosh, A.M.; et al. A “step too far” or “perfect sense”? A qualitative study of British adults’ views on mandating COVID-19 vaccination and vaccine passports. Vaccine 2022, in press. [Google Scholar] [CrossRef]
- Mundagowa, P.T.; Tozivepi, S.N.; Chiyaka, E.T.; Mukora-Mutseyekwa, F.; Makurumidze, R. Assessment of COVID-19 vaccine hesitancy among Zimbabweans: A rapid national survey. PLoS ONE 2022, 17, e0266724. [Google Scholar] [CrossRef]
- Orenstein, W.A.; Hinman, A.R. The immunization system in the United States—The role of school immunization laws. Vaccine 1999, 17 (Suppl. S3), S19–S24. [Google Scholar] [CrossRef]
- Blank, C.; Gemeinhart, N.; Dunagan, W.C.; Babcock, H.M. Mandatory employee vaccination as a strategy for early and comprehensive health care personnel immunization coverage: Experience from 10 influenza seasons. Am. J. Infect. Control. 2020, 48, 1133–1138. [Google Scholar] [CrossRef]
- Messenger, H. From Amex to Walmart, Here Are the Companies Mandating the Covid Vaccines For Employees NBC News: NBC. 2022. Available online: https://www.nbcnews.com/business/business-news/amex-walmart-are-companies-mandating-covid-vaccine-employees-rcna11049 (accessed on 12 May 2022).
- Press, A. Africa CDC: Nations Might Turn to COVID-19 Vaccine Mandates. 2022. Available online: https://www.usnews.com/news/world/articles/2021-12-09/africa-cdc-nations-might-turn-to-covid-19-vaccine-mandates (accessed on 12 May 2022).
- Economist. Informal Employment Dominates: Economist Intelligence Unit. 2015. Available online: http://country.eiu.com/article.aspx?articleid=453276029&Country=Zimbabwe&topic=Economy (accessed on 26 June 2022).
- Hamel, L.; Lopes, L.; Brodie, M. KKF COVID-19 Vaccine Monitor: What Do We Know About those who want to "Wait and See" Before Getting at COVID-19 vaccine? 2021. Available online: https://www.kff.org/coronavirus-covid-19/poll-finding/kff-covid-19-vaccine-monitor-wait-and-see/ (accessed on 27 May 2022).
- Makadzange, A.T.; Lau, C.; Dietrich, J.; Hlupeni, A.; Myburgh, N.; Gundidza, P.; Elose, N.; Mahdi, S.; James, W.; Stanberry, L.; et al. Investigating Attitudes, Motivations and Key Influencers for vaccine uptake among late adopters of COVID-19 vaccination in Africa. medRxiv 2022. [Google Scholar] [CrossRef]
- Nkengasong, J. Africa’s Low Vaccination Rates Should Concern Everyone. New York Times, 27 March 2022. [Google Scholar]
- Anjorin, A.A.; Odetokun, I.A.; Abioye, A.I.; Elnadi, H.; Umoren, M.V.; Damaris, B.F.; Eyedo, J.; Umar, H.I.; Nyandwi, J.B.; Abdalla, M.M.; et al. Will Africans take COVID-19 vaccination? PLoS ONE 2021, 16, e0260575. [Google Scholar] [CrossRef] [PubMed]
- Solis Arce, J.S.; Warren, S.S.; Meriggi, N.F.; Scacco, A.; McMurry, N.; Voors, M.; Syunyaev, G.; Malik, A.A.; Aboutajdine, S.; Adeojo, O.; et al. COVID-19 vaccine acceptance and hesitancy in low- and middle-income countries. Nat. Med. 2021, 27, 1385–1394. [Google Scholar] [CrossRef] [PubMed]
- Diekema, D.S. Personal belief exemptions from school vaccination requirements. Annu. Rev. Public Health 2014, 35, 275–292. [Google Scholar] [CrossRef] [Green Version]
- Harris, J.N.; Mauro, C.; Andresen, J.A.; Zimet, G.D.; Rosenthal, S.L. COVID-19 vaccine uptake and attitudes towards mandates in a nationally representative U.S. sample. J. Behav. Med. 2022. [Google Scholar] [CrossRef]
- Sprengholz, P.; Korn, L.; Eitze, S.; Felgendreff, L.; Siegers, R.; Goldhahn, L.; De Bock, F.; Huebl, L.; Böhm, R.; Betsch, C. Attitude toward a mandatory COVID-19 vaccination policy and its determinants: Evidence from serial cross-sectional surveys conducted throughout the pandemic in Germany. Vaccine 2022, in press. [Google Scholar] [CrossRef]
- Giannakou, K.; Kyprianidou, M.; Heraclides, A. Attitudes and Determinants of Mandatory Vaccination against COVID-19 among the General Population of Cyprus: A Nationwide Cross-Sectional Study. Vaccines 2022, 10, 438. [Google Scholar] [CrossRef]
- Iguacel, I.; Alvarez-Najar, J.P.; Vasquez, P.D.C.; Alarcon, J.; Orte, M.A.; Samatan, E.; Martinez-Jarreta, B. Citizen Stance towards Mandatory COVID-19 Vaccination and Vaccine Booster Doses: A Study in Colombia, El Salvador and Spain. Vaccines 2022, 10, 781. [Google Scholar] [CrossRef]
- Pierri, F.; Perry, B.L.; DeVerna, M.R.; Yang, K.C.; Flammini, A.; Menczer, F.; Bryden, J. Online misinformation is linked to early COVID-19 vaccination hesitancy and refusal. Sci. Rep. 2022, 12, 5966. [Google Scholar] [CrossRef]
- Largent, E.A.; Persad, G.; Sangenito, S.; Glickman, A.; Boyle, C.; Emanuel, E.J. US Public Attitudes Toward COVID-19 Vaccine Mandates. JAMA Netw. Open 2020, 3, e2033324. [Google Scholar] [CrossRef]
- Larson, H.J.; de Figueiredo, A.; Xiahong, Z.; Schulz, W.S.; Verger, P.; Johnston, I.G.; Cook, A.R.; Jones, N.S. The State of Vaccine Confidence 2016: Global Insights Through a 67-Country Survey. EBioMedicine 2016, 12, 295–301. [Google Scholar] [CrossRef] [Green Version]
- Bank, W. Zimbabwe Country Profile 2021. Available online: https://data.worldbank.org/country/ZW (accessed on 26 June 2022).

| Question | Response Options |
|---|---|
| Attitudes to vaccine Mandates | |
| Do you approve of the government requiring a COVID-19 vaccine to get on public transportation? | Strongly approve; Somewhat approve; Somewhat disapprove; Strongly disapprove; Not sure; Prefer not to answer |
| Do you approve employers requiring a COVID-19 vaccine to get a job or certain pay allowances? | Strongly approve; Somewhat approve; Somewhat disapprove; Strongly disapprove; Not sure; Prefer not to answer |
| Do you think schools should require students to be vaccinated for COVID-19 as they do for most other diseases like measles and tuberculosis? | Yes, schools should require COVID-19 vaccination; No, schools should not require COVID-19 vaccination |
| Was there a requirement from your employer or school that you be vaccinated? | Yes, No, Don’t know |
| Attitudes to Childhood Vaccines | |
| If the COVID-19 vaccine was available to your child, how likely would you be to get your children vaccinated? | Extremely likely; Very likely; Somewhat likely; Not at all likely; Not sure |
| What concerns about COVID-19 vaccines for children do you have, if any? (Multiple responses accepted) | The vaccine has not been tested enough in children; the vaccine is still new; The vaccine is not effective in children; Immediate side effects; Long-term health effects; children do not need the vaccine because COVID-19 is mild in children; COVID-19 vaccines affect children’s fertility in the future; Other (specify); I have no concerns |
| Perceptions of vaccine safety and efficacy | |
| In general, COVID-19 vaccines are safe | Strongly agree; Somewhat agree; Neutral; Somewhat disagree; Strongly disagree; I do not know; Prefer not to answer |
| I am confident that my country’s regulation process approved the COVID-19 vaccine, only when it was shown to be safe | Strongly agree; Somewhat agree; Neutral; Somewhat disagree; Strongly disagree; I do not know; Prefer not to answer |
| I am confident that COVID-19 vaccines are effective in preventing the disease | Strongly agree; Somewhat agree; Neutral; Somewhat disagree; Strongly disagree; I do not know; Prefer not to answer |
| How safe or unsafe is the Sinovac/Sinopharm vaccine? | Very safe; Somewhat safe; Somewhat unsafe; Very unsafe; I do not know; Prefer not to answer |
| Characteristic | N(%) |
|---|---|
| Gender (Female) | 508 (50%) |
| Median age (IQR) | 30 (22–39) |
| Age groups | |
| 18–25 | 368 (36.2%) |
| 26–39 | 409 (40.3%) |
| >=40 years | 239 (23.5%) |
| Ethnicity (Black African) | 1016 (100%) |
| Highest Level of Education | |
| None + primary | 89 (8.8%) |
| Lower secondary | 735 (72.4%) |
| Higher secondary | 117 (11.5%) |
| Tertiary | 74 (7.3%) |
| Co-morbid conditions | |
| HIV | 126 (12.4%) |
| Socioeconomic status | |
| Higher | 172 (16.9 %) |
| Middle | 598 (58.9%) |
| Lower | 246 (24.2%) |
| Internet use in past 30 days (Y) | 420 (41.4 %) |
| Personal knowledge of someone who was seriously ill/died from COVID-19 | 428 (42.1%) |
| Children under age of 18 in the household (Y) | 866 (85.2%) |
| In general, COVID-19 vaccines are safe (strongly + somewhat agree) | 856 (84.3%) |
| I am confident that my country’s regulation process approved the COVID-19 vaccine only when it was shown to be safe (strongly + somewhat agree) | 838 (82.5%) |
| I am confident that COVID-19 vaccines are effective in preventing the disease (strongly+somewhat agree) | 868 (85.4%) |
| How safe or unsafe is the Sinovac/Sinopharm vaccine? (very + somewhat safe) | 675 (66.4%) |
| Univariate | Multivariate | |||||||
|---|---|---|---|---|---|---|---|---|
| Variables | Category | Proportion That Approves | OR * | 95% CI # | p-Value | OR * | 95% CI # | p-Value |
| Gender | Male | 0.75 | 1 | |||||
| Female | 0.75 | 1.021 | 0.769, 1.357 | 0.885 | ||||
| Age | 18–25 | 0.76 | 1 | |||||
| 26–39 | 0.75 | 0.944 | 0.679, 1.312 | 0.732 | ||||
| ≥40 years | 0.72 | 0.812 | 0.56, 1.177 | 0.271 | ||||
| Education | ≤primary | 0.83 | 1 | |||||
| Lower secondary | 0.76 | 0.644 | 0.360, 1.150 | 0.137 | ||||
| Higher secondary | 0.73 | 0.538 | 0.271, 1.071 | 0.078 | ||||
| Tertiary | 0.58 | 0.281 | 0.137, 0.0579 | 0.001 | ||||
| Economic status | High | 0.65 | 1 | |||||
| Middle | 0.75 | 1.6 | 1.112, 2.303 | 0.011 | 1.588 | 1.083, 2.329 | 0.018 | |
| Low | 0.82 | 2.459 | 1.564, 3.866 | <0.001 | 2.249 | 1.403, 3.607 | 0.001 | |
| Personal COVID Experience | No | 0.73 | 1 | |||||
| Yes | 0.78 | 1.328 | 0.992, 1.779 | 0.057 | ||||
| HIV | Negative | 0.75 | 1 | |||||
| Positive | 0.74 | 0.931 | 0.608, 1.424 | 0.742 | ||||
| Internet use in last 30 days | No | 0.78 | 1 | |||||
| Yes | 0.71 | 0.684 | 0.514, 0.912 | 0.01 | ||||
| Children at home | No | 0.74 | 1 | |||||
| Yes | 0.75 | 1.064 | 0.716, 1.581 | 0.759 | ||||
| No | 0.77 | 1 | ||||||
| Yes | 0.74 | 0.816 | 0.606, 1.098 | 0.179 | ||||
| No | 0.77 | 1 | ||||||
| Yes | 0.72 | 0.796 | 0.595, 1.065 | 0.124 | ||||
| In general, COVID-19 vaccines are safe | Disagree | 0.53 | 1 | |||||
| Agree | 0.79 | 3.337 | 2.348, 4.743 | <0.0001 | ||||
| I am confident that my country’s regulation process approved the COVID-19 vaccine, only when it was shown to be safe | Disagree | 0.56 | 1 | |||||
| Agree | 0.79 | 2.934 | 2.089, 4.12 | <0.0001 | 1.756 | 1.183, 2.605 | 0.005 | |
| I am confident that COVID-19 vaccines are effective in preventing the disease | Disagree | 0.5 | 1 | |||||
| Agree | 0.79 | 3.822 | 2.662, 5.487 | <0.0001 | 2.349 | 1.543, 3.576 | <0.0001 | |
| How safe or unsafe is the Sinovac/Sinopharm vaccine? | Unsafe | 0.64 | 1 | |||||
| Safe | 0.8 | 2.292 | 1.711, 3.068 | <0.0001 | 1.838 | 1.345, 2.511 | <0.0001 | |
| Univariate | Multivariate | |||||||
|---|---|---|---|---|---|---|---|---|
| Variables | Category | Proportion That Approves | OR * | 95% CI # | p-Value | OR * | 95% CI # | p-Value |
| Gender | Male | 0.71 | 1 | |||||
| Female | 0.76 | 1.261 | 0.954, 1.667 | 0.103 | ||||
| Age | 18–25 | 0.74 | 1 | |||||
| 26–39 | 0.74 | 1.009 | 0.732, 1.391 | 0.957 | ||||
| ≥40 years | 0.71 | 0.87 | 0.604, 1.251 | 0.452 | ||||
| Education | ≤primary | 0.84 | 1 | |||||
| Lower secondary | 0.75 | 0.547 | 0.302, 0.991 | 0.047 | ||||
| Higher secondary | 0.67 | 0.373 | 0.188, 0.743 | 0.005 | ||||
| Tertiary | 0.58 | 0.259 | 0.124, 0.539 | <0.001 | ||||
| Economic status | High | 0.66 | 1 | |||||
| Middle | 0.72 | 1.359 | 0.946, 1.952 | 0.097 | 1.332 | 0.904, 1.962 | 0.148 | |
| Low | 0.81 | 2.27 | 1.449, 3.558 | <0.001 | 2.109 | 1.31, 3.395 | 0.002 | |
| Personal COVID Experience | No | 0.72 | 1 | |||||
| Yes | 0.76 | 1.21 | 0.911, 1.608 | 0.188 | ||||
| HIV | Negative | 0.73 | 1 | |||||
| Positive | 0.75 | 1.132 | 0.735, 1.742 | 0.575 | ||||
| Internet use in last 30 days | No | 0.77 | 1 | |||||
| Yes | 0.68 | 0.621 | 0.469, 0.822 | 0.01 | ||||
| Children at home | No | 0.73 | 1 | |||||
| Yes | 0.73 | 1 | 0.675, 1.479 | 0.998 | ||||
| No | 0.76 | 1 | ||||||
| Yes | 0.72 | 0.797 | 0.596, 1.067 | 0.128 | ||||
| No | 0.75 | 1 | ||||||
| Yes | 0.7 | 0.758 | 0.571, 1.008 | 0.057 | ||||
| In general, COVID-19 vaccines are safe | Disagree | 0.52 | 1 | |||||
| Agree | 0.77 | 3.166 | 2.233, 4.488 | <0.0001 | ||||
| I am confident that my country’s regulation process approved the COVID-19 vaccine, only when it was shown to be safe | Disagree | 0.52 | 1 | |||||
| Agree | 0.78 | 3.204 | 2.289, 4.484 | <0.0001 | 1.766 | 1.192, 2.615 | 0.005 | |
| I am confident that COVID-19 vaccines are effective in preventing the disease | Disagree | 0.42 | 1 | |||||
| Agree | 0.79 | 5.121 | 3.556, 7.375 | <0.0001 | 3.201 | 2.11, 4.855 | <0.0001 | |
| How safe or unsafe is the Sinovac/Sinopharm vaccine? | Unsafe | 0.61 | 1 | |||||
| Safe | 0.8 | 2.542 | 1.908, 3.387 | <0.0001 | 1.952 | 1.434, 2.656 | <0.0001 | |
| Univariate | Multivariate | |||||||
|---|---|---|---|---|---|---|---|---|
| Variables | Category | Proportion That Approves | OR * | 95% CI # | p-Value | OR * | 95% CI# | p-Value |
| Gender | Male | 0.78 | 1 | |||||
| Female | 0.8 | 1.129 | 0.816, 1.562 | 0.463 | ||||
| Age | 18–25 | 0.8 | 1 | |||||
| 26–39 | 0.79 | 0.945 | 0.65, 1.375 | 0.769 | ||||
| >=40 years | 0.76 | 0.821 | 0.533, 1.265 | 0.371 | ||||
| Education | ≤primary | 0.82 | 1 | |||||
| Lower secondary | 0.79 | 0.851 | 0.453, 1.599 | 0.616 | ||||
| Higher secondary | 0.83 | 1.121 | 0.506, 2.483 | 0.779 | ||||
| Tertiary | 0.59 | 0.327 | 0.148, 0.724 | 0.006 | ||||
| Economic status | High | 0.7 | 1 | |||||
| Middle | 0.79 | 1.63 | 1.072, 2.48 | 0.022 | 1.589 | 1.071, 2.358 | 0.021 | |
| Low | 0.83 | 2.027 | 1.222, 3.363 | 0.006 | 1.931 | 1.195, 3.121 | 0.007 | |
| Personal COVID Experience | No | 0.76 | 1 | |||||
| Yes | 0.83 | 1.551 | 1.102, 2.183 | 0.012 | 1.384 | 1.003, 1.909 | 0.048 | |
| HIV | Negative | 0.79 | 1 | |||||
| Positive | 0.78 | 0.972 | 0.593, 1.592 | 0.91 | ||||
| Internet use in last 30 days | No | 0.81 | 1 | |||||
| Yes | 0.75 | 0.7 | 0.505, 0.97 | 0.032 | ||||
| No | 0.82 | 1 | ||||||
| Yes | 0.76 | 0.701 | 0.495, 0.992 | 0.045 | ||||
| No | 0.81 | 1 | ||||||
| Yes | 0.75 | 0.68 | 0.489, 0.944 | 0.021 | ||||
| In general, COVID-19 vaccines are safe | Disagree | 0.62 | 1 | |||||
| Agree | 0.81 | 2.701 | 1.88, 3.881 | <0.0001 | ||||
| I am confident that my country’s regulation process approved the COVID-19 vaccine, only when it was shown to be safe | Disagree | 0.62 | 1 | |||||
| Agree | 0.82 | 2.79 | 1.967, 3.958 | <0.0001 | 1.893 | 1.266, 2.831 | 0.002 | |
| I am confident that COVID-19 vaccines are effective in preventing the disease | Disagree | 0.6 | 1 | |||||
| Agree | 0.82 | 2.911 | 2.009, 4.218 | <0.0001 | 1.709 | 1.105, 2.643 | 0.016 | |
| How safe or unsafe is the Sinovac/Sinopharm vaccine? | Unsafe | 0.7 | 1 | |||||
| Safe | 0.83 | 2.064 | 1.521, 2.801 | <0.0001 | 1.751 | 1.265, 2.424 | 0.001 | |
| Univariate | Multivariate | |||||||
|---|---|---|---|---|---|---|---|---|
| Variables | Category | Proportion of Participants | OR * | 95% CI # | p-Value | OR * | 95% CI # | p-Value |
| Gender | Male | 0.71 | 1 | |||||
| Female | 0.75 | 1.21 | 0.916, 1.598 | 0.179 | ||||
| Age | 18–25 | 0.66 | 1 | 1 | ||||
| 26–39 | 0.78 | 1.819 | 1.325, 2.499 | <0.001 | 1.608 | 1.14, 2.267 | 0.007 | |
| ≥40 years | 0.77 | 1.701 | 1.177, 2.46 | 0.005 | 1.694 | 1.126, 2.55 | 0.011 | |
| Education | ≤Primary | 0.79 | 1 | |||||
| Lower secondary | 0.75 | 0.819 | 0.48, 1.396 | 0.463 | ||||
| Higher secondary | 0.68 | 0.587 | 0.31, 1.112 | 0.102 | ||||
| Tertiary | 0.54 | 0.319 | 0.161, 0.632 | 0.001 | ||||
| Economic status | High | 0.63 | 1 | |||||
| Middle | 0.74 | 1.724 | 1.203, 2.469 | 0.003 | 1.568 | 1.062, 2.314 | 0.024 | |
| Low | 0.77 | 2.011 | 1.309, 3.089 | 0.001 | 1.433 | 0.896, 2.293 | 0.134 | |
| Personal COVID Experience | No | 0.72 | 1 | |||||
| Yes | 0.74 | 1.109 | 0.836, 1.47 | 0.473 | ||||
| HIV | Negative | 0.73 | 1 | |||||
| Positive | 0.76 | 1.202 | 0.777, 1.858 | 0.408 | ||||
| Internet use in last 30 days | No | 0.77 | 1 | 1 | ||||
| Yes | 0.67 | 0.589 | 0.445, 0.779 | <0.001 | 0.71 | 0.519, 0.971 | 0.032 | |
| Children at home | No | 0.6 | 1 | 1 | ||||
| Yes | 0.75 | 2.044 | 1.424, 2.934 | <0.001 | 2.091 | 1.417, 3.086 | <0.0001 | |
| No | 0.73 | 1 | ||||||
| Yes | 0.73 | 0.975 | 0.732, 1.299 | 0.863 | ||||
| No | 0.73 | 1 | ||||||
| Yes | 0.73 | 1.017 | 0.62, 1.355 | 0.911 | ||||
| In general COVID-19 vaccines are safe | Disagree | 0.48 | 1 | 1 | ||||
| Agree | 0.78 | 3.901 | 2.749, 5.534 | <0.0001 | 2.021 | 1.287, 3.175 | 0.002 | |
| Confident in regulatory process that approved the vaccines | Disagree | 0.52 | 1 | 1 | ||||
| Agree | 0.78 | 3.254 | 2.326, 4.554 | <0.0001 | 1.762 | 1.165, 2.666 | 0.007 | |
| Confident that vaccines are effective in preventing the disease | Disagree | 0.47 | 1 | 1 | ||||
| Agree | 0.78 | 3.846 | 2.683, 5.512 | <0.0001 | 1.636 | 1.030, 2.598 | 0.037 | |
| How safe or unsafe is the Sinovac/Sinopharm vaccine? | Unsafe | 0.62 | 1 | 1 | ||||
| Safe | 0.79 | 2.244 | 1.686, 2.987 | <0.0001 | 1.795 | 1.305, 2.467 | <0.0001 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Makadzange, A.T.; Gundidza, P.; Lau, C.; Dietrich, J.; Beta, N.; Myburgh, N.; Elose, N.; Ndhlovu, C.; James, W.; Stanberry, L. Attitudes to Vaccine Mandates among Late Adopters of COVID-19 Vaccines in Zimbabwe. Vaccines 2022, 10, 1090. https://doi.org/10.3390/vaccines10071090
Makadzange AT, Gundidza P, Lau C, Dietrich J, Beta N, Myburgh N, Elose N, Ndhlovu C, James W, Stanberry L. Attitudes to Vaccine Mandates among Late Adopters of COVID-19 Vaccines in Zimbabwe. Vaccines. 2022; 10(7):1090. https://doi.org/10.3390/vaccines10071090
Chicago/Turabian StyleMakadzange, Azure Tariro, Patricia Gundidza, Charles Lau, Janan Dietrich, Norest Beta, Nellie Myburgh, Nyasha Elose, Chiratidzo Ndhlovu, Wilmot James, and Lawrence Stanberry. 2022. "Attitudes to Vaccine Mandates among Late Adopters of COVID-19 Vaccines in Zimbabwe" Vaccines 10, no. 7: 1090. https://doi.org/10.3390/vaccines10071090
APA StyleMakadzange, A. T., Gundidza, P., Lau, C., Dietrich, J., Beta, N., Myburgh, N., Elose, N., Ndhlovu, C., James, W., & Stanberry, L. (2022). Attitudes to Vaccine Mandates among Late Adopters of COVID-19 Vaccines in Zimbabwe. Vaccines, 10(7), 1090. https://doi.org/10.3390/vaccines10071090






