Optional Vaccines in Children—Knowledge, Attitudes, and Practices in Romanian Parents
Abstract
1. Introduction
2. Materials and Methods
2.1. Knowledge Score and Knowledge Rating
2.2. Statistical Analysis
2.3. Ethical Approval
3. Results
3.1. General Characteristics of Respondents
3.2. Level of Knowledge
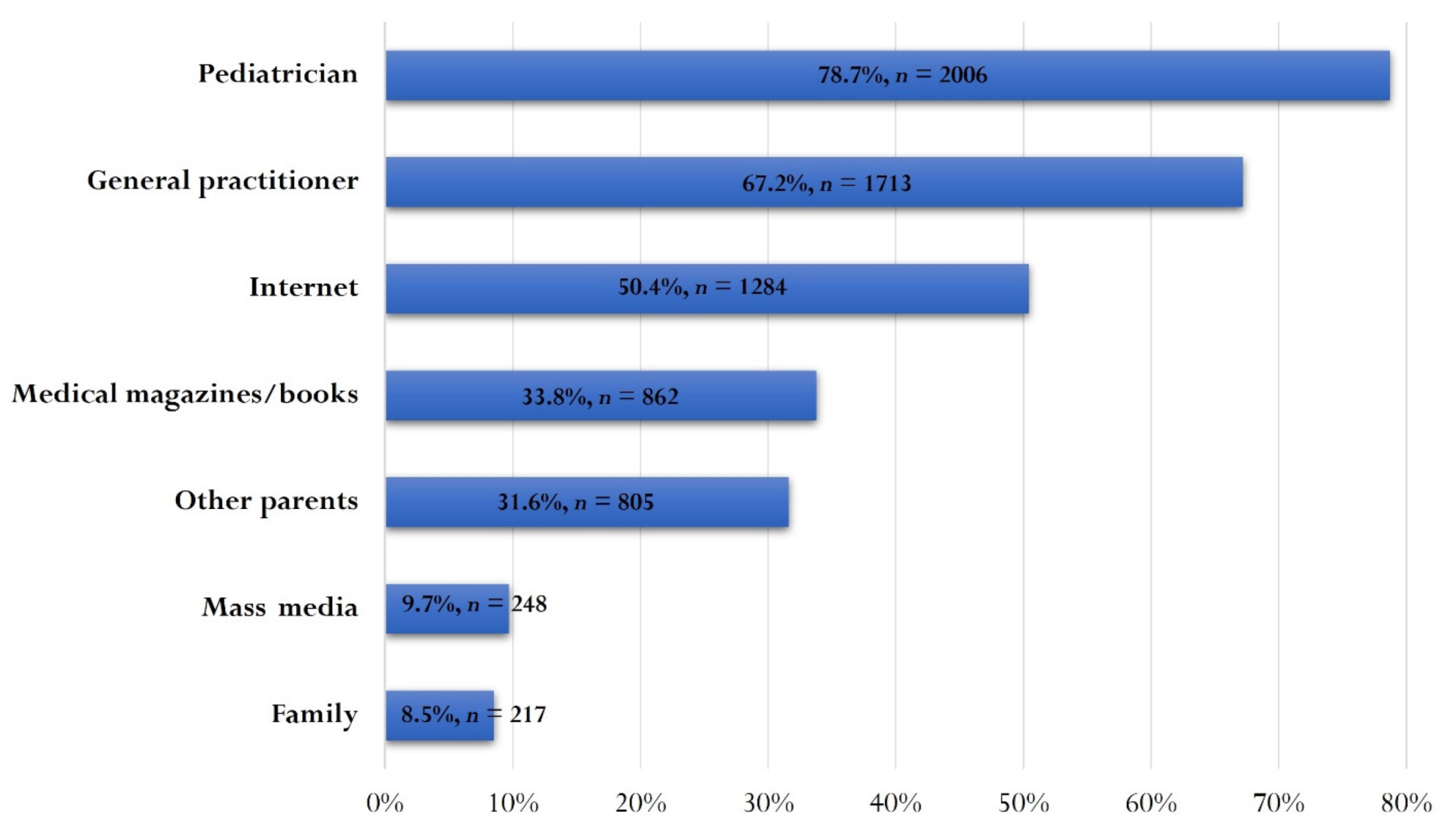
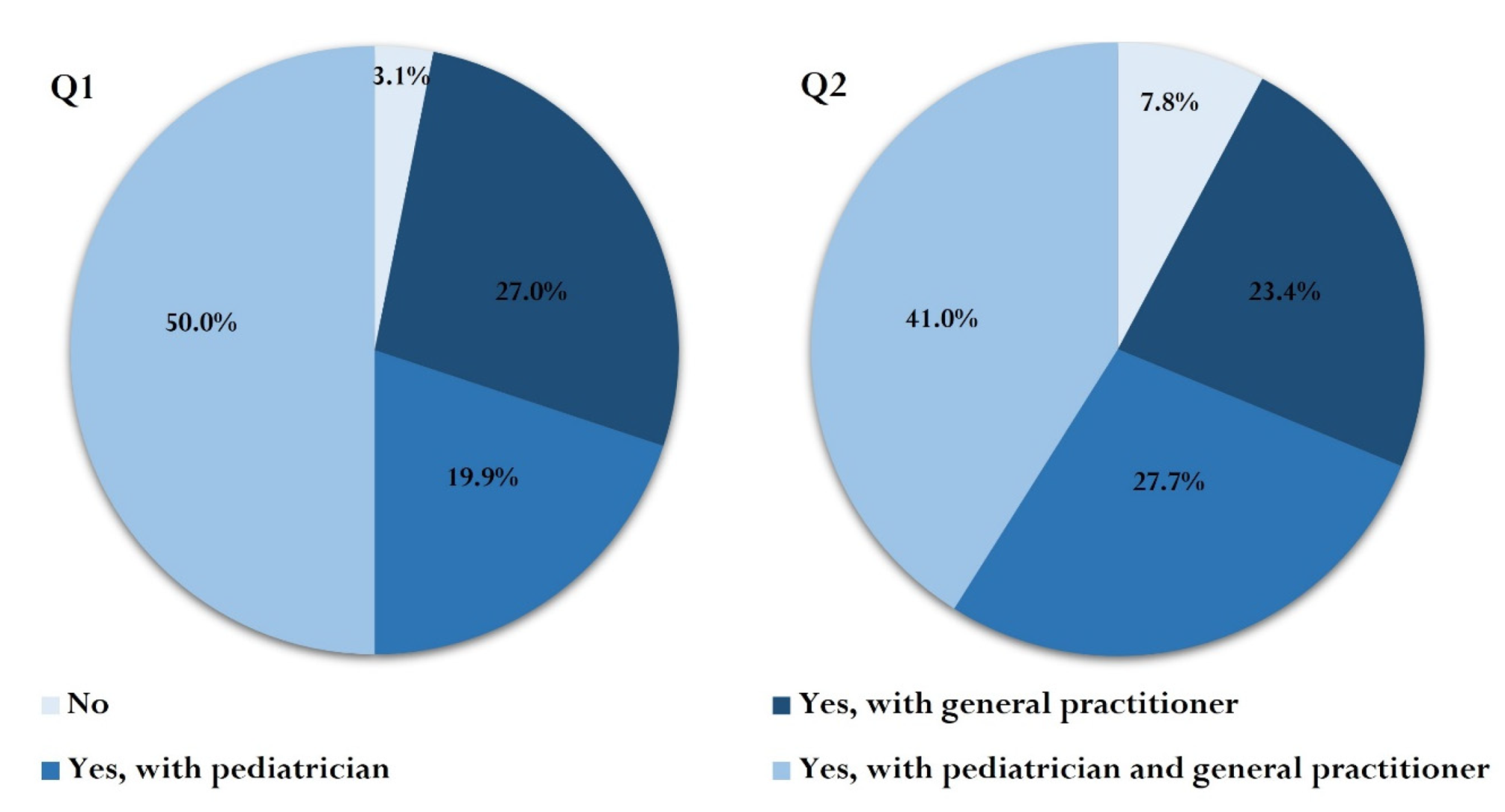
3.3. Information and Communication
3.4. Free Vaccination
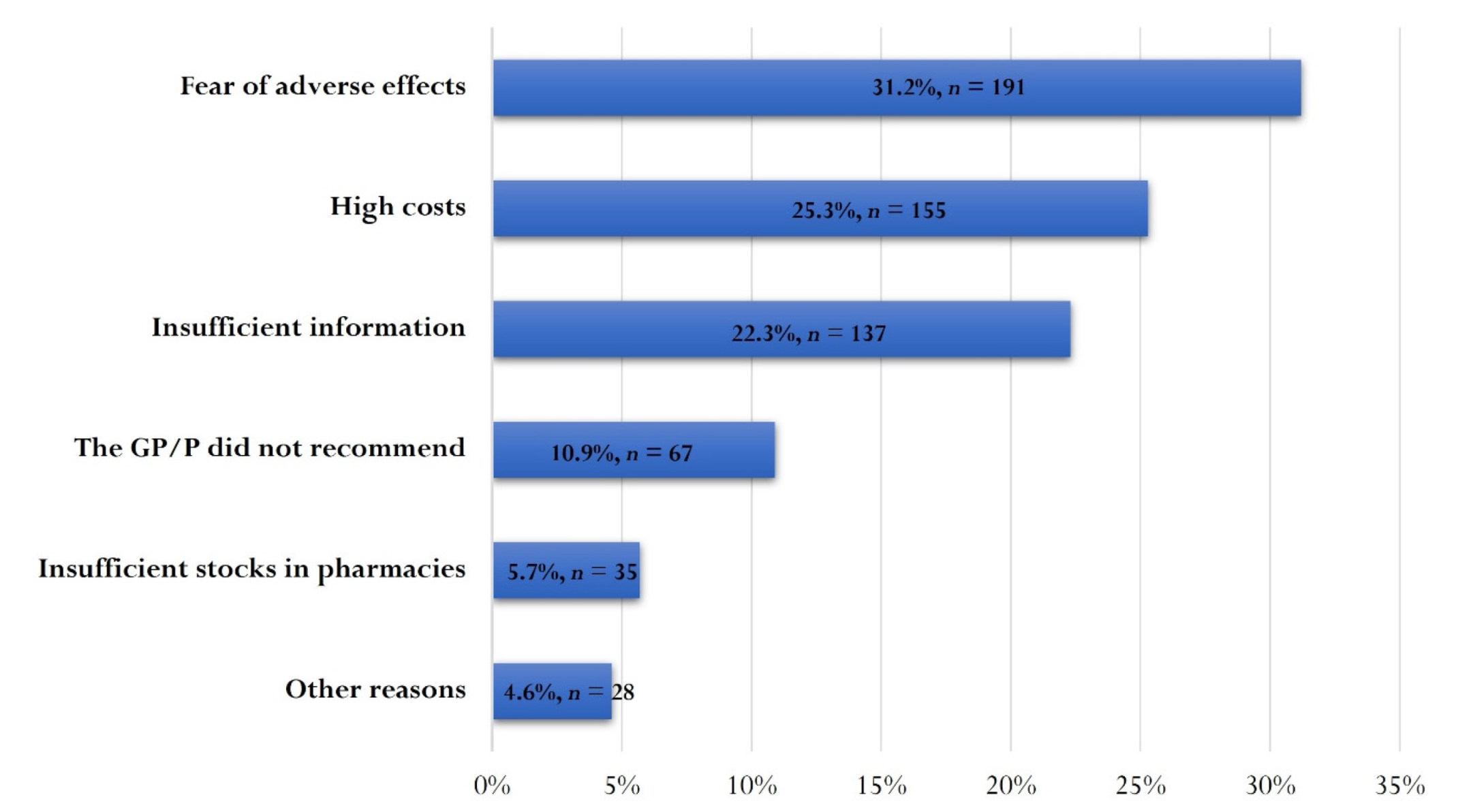
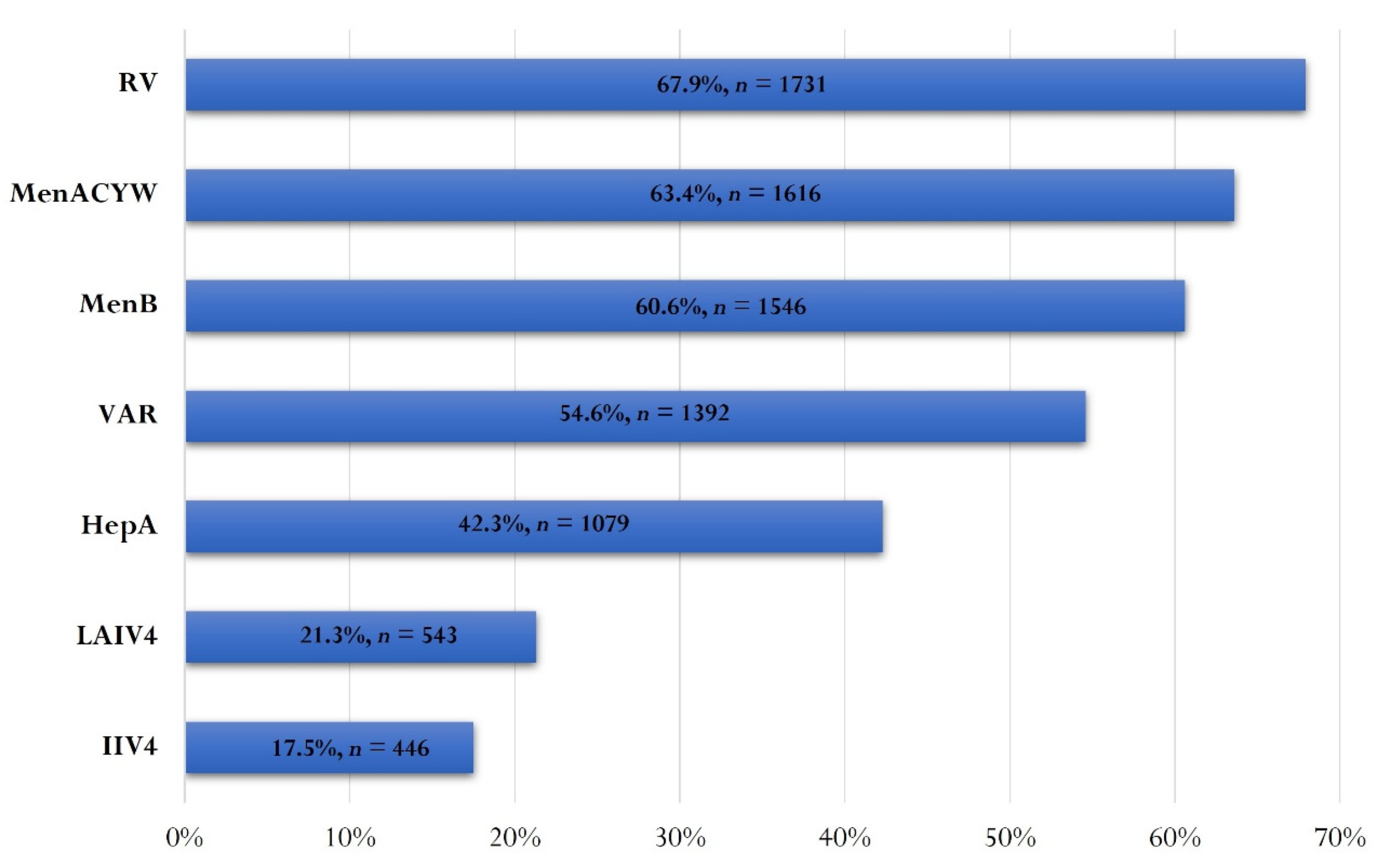
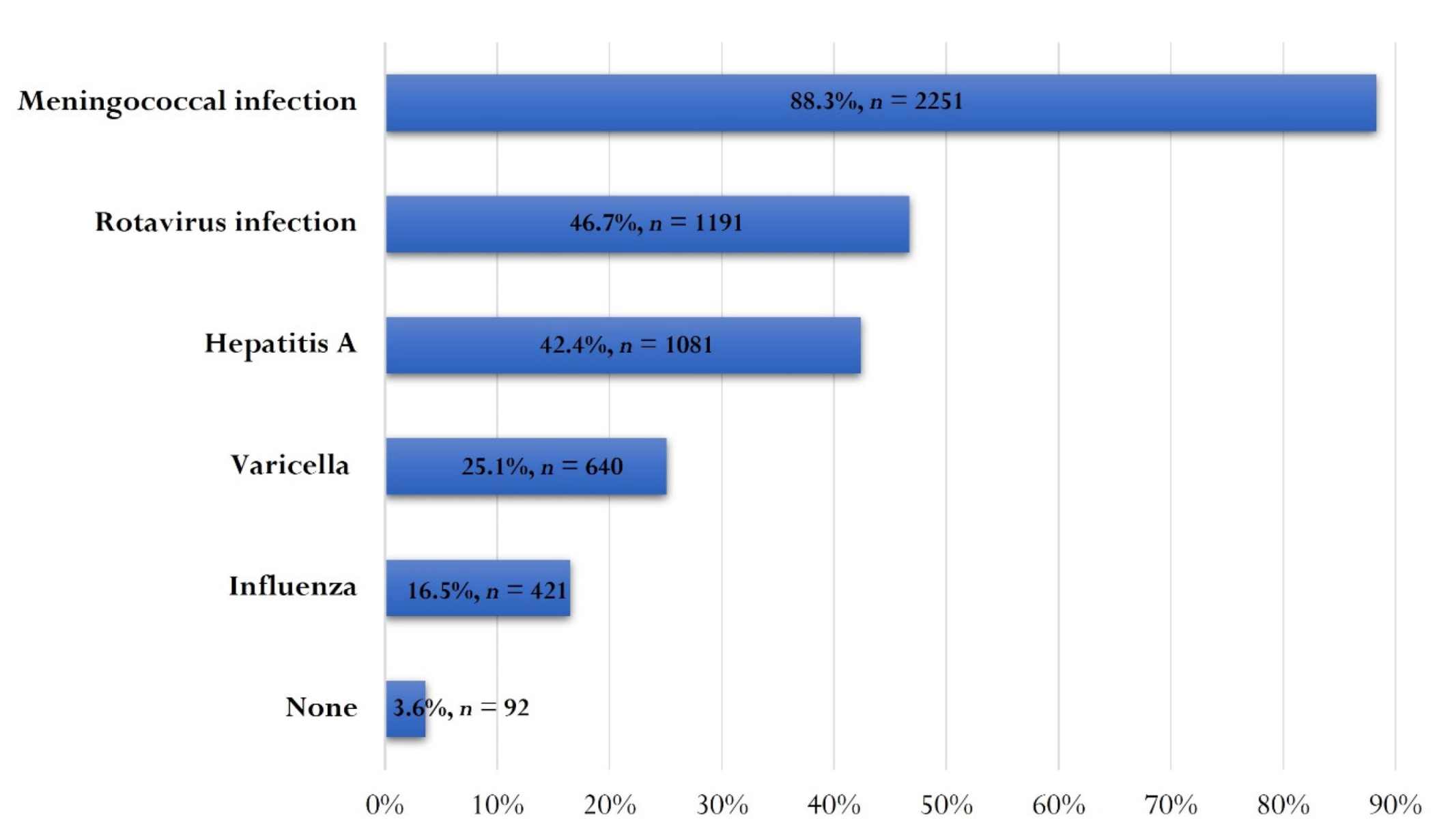
3.5. Optional Vaccination
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Strassburg, M.A. The global eradication of smallpox. Am. J. Infect. Control. 1982, 10, 53–59. [Google Scholar] [CrossRef]
- Modlin, J.F.; Schaffner, W.; Orenstein, W.; Bandyopadhyay, A.S. Triumphs of Immunization. J. Infect. Dis. 2021, 224 (Suppl. 2), S307–S308. [Google Scholar] [CrossRef] [PubMed]
- Centrul Național de Supraveghere și Control al Bolilor Transmisibile. Calendarul Naţional de Vaccinare. 2022. Available online: https://www.cnscbt.ro/index.php/calendarul-national-de-vaccinare (accessed on 20 January 2022).
- Ministery of Health. Vaccinarea Gratuită anti-HPV, Extinsă la Fete Până la 18 Ani. 2021. Available online: http://www.ms.ro/2021/09/03/ministrul-sanatatii-ioana-mihaila-vaccinarea-gratuita-anti-hpv-extinsa-la-fete-pana-la-18-ani/ (accessed on 20 January 2022).
- Stein, R.A. The golden age of anti-vaccine conspiracies. Germs 2017, 7, 168–170. [Google Scholar] [CrossRef] [PubMed]
- Centrul Național de Supraveghere și Control al Bolilor Transmisibile. Analiza Evoluției Bolilor Transmisibile Aflate în Supraveghere—Raport Pentru Anul 2018. 2019. Available online: https://www.cnscbt.ro/index.php/rapoarte-anuale/1302-analiza-bolilor-transmisibile-aflate-in-supraveghere-raport-pentru-anul-2018/file (accessed on 18 January 2022).
- Pițigoi, D.; Săndulescu, O.; Crăciun, M.D.; Drăgănescu, A.; Jugulete, G.; Streinu-Cercel, A.; Vișan, A.; Rîciu, C.; Rafila, A.; Aramă, V.; et al. Measles in Romania—Clinical and epidemiological characteristics of hos-pitalized measles cases during the first three years of the 2016-ongoing epidemic. Virulence 2020, 11, 686–694. [Google Scholar] [CrossRef]
- Centrul National de Supraveghere si Control al Bolilor Transmisibile. Analiza Rezultatelor Estimării Acoperirii Vaccinale la Vârsta de 18 Luni Pentru Copiii Născuți în Luna Iulie 2019. 2021. Available online: https://www.cnscbt.ro/index.php/analiza-date-supraveghere/evaluarea-acoperirii-vaccinale/2551-analiza-rezultatelor-estimarii-acoperirii-vaccinale-la-varsta-de-18-luni-a-copiilor-nascuti-in-luna-iulie-2019-februarie-2021/file (accessed on 16 January 2022).
- Hoogink, J.; Verelst, F.; Kessels, R.; van Hoek, A.J.; Timen, A.; Willem, L.; Beutels, P.; Wallinga, J.; De Wit, G.A. Preferential differences in vaccination decision-making for oneself or one’s child in The Netherlands: A discrete choice experiment. BMC Public Health 2020, 20, 828. [Google Scholar] [CrossRef]
- Kraśnicka, J.; Krajewska-Kułak, E.; Klimaszewska, K.; Cybulski, M.; Guzowski, A.; Lewko, J.; Łukaszuk, C.; Kowalczuk, K.; Doroszkiewicz, H.; Baranowska, A.; et al. The impact of parents’ health behaviours on their preferences regarding vaccinations in Bialystok, Poland. BMC Pediatr. 2020, 20, 354. [Google Scholar] [CrossRef] [PubMed]
- Germani, F.; Biller-Andorno, N. The anti-vaccination infodemic on social media: A behavioral analysis. PLoS ONE 2021, 16, e0247642. [Google Scholar] [CrossRef]
- Vaccines Today. One Doctor’s Social Media Mission to Discuss Vaccination with Parents. 2018. Available online: https://www.vaccinestoday.eu/stories/one-doctors-social-media-mission-to-discuss-vaccination-with-parents/ (accessed on 15 January 2022).
- Tomczak, M.; Tomczak, E.J.T. The need to report effect size estimates revisited. An overview of some recommended measures of effect size. Trends Sport Sci. 2014, 1, 19–25. [Google Scholar]
- World Helath Organization. Immunization Coverage. 2021. Available online: https://www.who.int/news-room/fact-sheets/detail/immunization-coverage (accessed on 16 January 2022).
- Dyda, A.; King, C.; Dey, A.; Leask, J.; Dunn, A.G. A systematic review of studies that measure parental vaccine attitudes and beliefs in childhood vaccination. BMC Public Health 2020, 20, 1253. [Google Scholar] [CrossRef]
- Stahl, J.-P.; Cohen, R.; Denis, F.; Gaudelus, J.; Martinot, A.; Lery, T.; Lepetit, H. The impact of the web and social networks on vaccination. New challenges and opportunities offered to fight against vaccine hesitancy. Med. Mal. Infect. 2016, 46, 117–122. [Google Scholar] [CrossRef]
- Johnson, N.F.; Velásquez, N.; Restrepo, N.J.; Leahy, R.; Gabriel, N.; El Oud, S.; Zheng, M.; Manrique, P.; Wuchty, S.; Lupu, Y. The online competition between pro- and anti-vaccination views. Nature 2020, 582, 230–233. [Google Scholar] [CrossRef]
- World Helath Organization Europe. Dr Mihai Craiu, paediatrician, Bucharest, Romania. Available online: https://www.euro.who.int/en/countries/romania/personal-stories/dr-mihai-craiu,-paediatrician,-bucharest,-romania (accessed on 28 January 2022).
- McNeil, D.A.; Mueller, M.; Macdonald, S.; McDonald, S.; Saini, V.; Kellner, J.D.; Tough, S. Maternal perceptions of childhood vaccination: Explanations of reasons for and against vaccination. BMC Public Health 2019, 19, 49. [Google Scholar] [CrossRef]
- Jung, M. The effect of maternal decisional authority on children’s vaccination in East Asia. PLoS ONE 2018, 13, e0200333. [Google Scholar] [CrossRef]
- O’Leary, S.T.; Barnard, J.; Lockhart, S.; Kolasa, M.; Shmueli, D.; Dickinson, L.M.; Kile, D.; Dibert, E.; Kempe, A. Urban and Rural Differences in Parental Attitudes About Influenza Vac-cination and Vaccine Delivery Models. J. Rural Health Fall 2015, 31, 421–430. [Google Scholar] [CrossRef]
- Institutul Național de Statistică. Populaţia După Domiciliu la 1 Ianuarie 2020. 2020. Available online: https://insse.ro/cms/ro/content/popula%C5%A3ia-dup%C4%83-domiciliu-la-1-ianuarie-2020 (accessed on 16 January 2022).
- Institutul Național de Statistică. Tendințe sociale. 2019. Available online: https://insse.ro/cms/sites/default/files/field/publicatii/tendinte_sociale.pdf (accessed on 16 January 2022).
- Cataldi, J.R.; O’Leary, S.T. Parental vaccine hesitancy: Scope, causes, and potential responses. Curr. Opin. Infect. Dis. 2021, 34, 519–526. [Google Scholar] [CrossRef]
- Shen, S.C.; Dubey, V. Addressing vaccine hesitancy: Clinical guidance for primary care physicians working with parents. Can. Fam. Physician. 2019, 65, 175–181. [Google Scholar]
- Chappuy, H.; Taupin, P.; Dimet, J.; Claessens, Y.E.; Treluyer, J.-M.; Chéron, G.; Gfrup, T. Do parents understand the medical information provided in paediatric emergency departments? A prospective multicenter study. Acta Paediatr. 2012, 101, 1089–1094. [Google Scholar] [CrossRef]
- Anderson, E.L. Recommended solutions to the barriers to immunization in children and adults. Mo. Med. 2014, 111, 344–348. [Google Scholar]
- Balan, A.; Bejan, I.; Bonciu, S.; Eni, C.E.; Ruta, S. Romanian Medical Students’ Attitude towards and Perceived Knowledge on COVID-19 Vaccination. Vaccines 2021, 9, 854. [Google Scholar] [CrossRef]
- Thomas, S.L.; Walker, J.L.; Fenty, J.; Atkins, K.E.; Elliot, A.; Hughes, H.; Stowe, J.; Ladhani, S.; Andrews, N.J. Impact of the national rotavirus vaccination programme on acute gastroenteritis in England and associated costs averted. Vaccine 2017, 35, 680–686. [Google Scholar] [CrossRef]
- De Hoog, M.L.A.; Vesikari, T.; Giaquinto, C.; Huppertz, H.I.; Martinon-Torres, F.; Bruijning-Verhagen, P. Report of the 5th European expert meeting on rotavirus vaccination (EEROVAC). Hum. Vaccin. Immunother. 2018, 14, 1027–1034. [Google Scholar] [CrossRef] [PubMed]
- Anca, I.A.; Furtunescu, F.L.; Plesca, D.; Streinu-Cercel, A.; Rugina, S.; Holl, K. Hospital-based surveillance to estimate the burden of rotavirus gastroenteritis in children below five years of age in Romania. Germs 2014, 4, 30–40. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Miron, V.D. Drugs in COVID-19--life-saving or potentially hazardous approaches. J. Contemp. Clin. Pract. 2020, 6, 47–48. [Google Scholar] [CrossRef]
- Miron, V.D.; Bănică, L.; Săndulescu, O.; Paraschiv, S.; Surleac, M.; Florea, D.; Vlaicu, O.; Milu, P.; Streinu-Cercel, A.; Bilașco, A.; et al. Clinical and molecular epidemiology of influenza viruses from Romanian patients hospitalized during the 2019/20 season. PLoS ONE 2021, 16, e0258798. [Google Scholar] [CrossRef] [PubMed]
- Keske, S.; Mutters, N.T.; Tsioutis, C.; Ergonul, O.; Team Eivs. Influenza vaccination among infection control teams: A EUCIC survey prior to COVID-19 pandemic. Vaccine 2020, 38, 8357–8361. [Google Scholar] [CrossRef] [PubMed]
- Miko, D.; Costache, C.; Colosi, H.A.; Neculicioiu, V.; Colosi, I.A. Qualitative Assessment of Vaccine Hesitancy in Romania. Medicina 2019, 55, 282. [Google Scholar] [CrossRef]
- Mbaeyi, S.A.; Bozio, C.H.; Duffy, J.; Rubin, L.G.; Hariri, S.; Stephens, D.S.; MacNeil, J.R. Meningococcal Vaccination: Recommendations of the Advisory Committee on Immunization Practices, United States, 2020. MMWR Recomm. Rep. 2020, 69, 1–41. [Google Scholar] [CrossRef]
- Jacobsen, K.H. Globalization and the Changing Epidemiology of Hepatitis A Virus. Cold Spring Harb. Perspect. Med. 2018, 8, a031716. [Google Scholar] [CrossRef]
- Coppola, N.; Genovese, D.; Pisaturo, M.; Taffon, S.; Argentini, C.; Pasquale, G.; Sagnelli, C.; Piccinino, F.; Rapicetta, M.; Sagnelli, E. Acute hepatitis with severe cholestasis and prolonged clinical course due to hepatitis A virus Ia and Ib coinfection. Clin. Infect. Dis. 2007, 44, e73–e77. [Google Scholar] [CrossRef]
| Characteristic | Number of Respondents, n(%) |
|---|---|
| Gender | |
| female | 2432 (95.4) |
| male | 118 (4.6) |
| Age (mean in years, ±SD) | |
| all respondents | 36.9 ± 5.3 |
| male | 38.4 ± 5.2 |
| female | 36.8 ± 5.3 |
| Residence | |
| urban | 2268 (88.9) |
| rural | 282 (11.1) |
| Educational level | |
| unfinished general school/without studies | 2 (0.1) |
| completed general school | 6 (0.2) |
| vocational school | 10 (0.4) |
| high school | 146 (5.7) |
| post-high school | 89 (3.5) |
| university studies | 2297 (90.1) |
| Number of children | |
| 1 child | 1398 (54.8) |
| 2 children | 1047 (41.1) |
| 3 children | 93 (3.6) |
| 4 children | 11 (0.4) |
| 5 children | 1 (0.05) |
| Median age of children (median in years, IQR) | |
| first child | 5 (3–9) |
| second child | 4 (2–7) |
| third child | 3 (1–5.3) |
| fourth child | 1 (0.3–4) |
| Characteristic | Knowledge Score, Median (IQR) | Statistical Analysis | Knowledge Rating, n(%) | Statistical Analysis | |||
|---|---|---|---|---|---|---|---|
| Very good | Good | Sufficient | Insufficient | ||||
| All participants (n = 2550) | 10 (8.5–11) | NA | 1406 (55.1) | 910 (35.7) | 211 (8.3) | 23 (0.9) | NA |
| Gender | |||||||
| female (n = 2432) | 10 (8.5–11) | p < 0.001, U = 107,686.5, z = −4.604, r = 0.09 | 1359 (55.9) | 866 (35.6) | 190 (7.8) | 17 (0.7) | p < 0.001, χ2(12) = 42.904, V = 0.130 |
| male (n = 118) | 8.5 (7–10.5) | 47 (39.8) | 44 (37.3) | 21 (17.8) | 6 (5.1) | ||
| Age group | |||||||
| under 30 years (n = 152) | 10 (8–11) | p = 0.049, H(2) = 6.012, d = 0.079 | 78 (51.3) | 55 (36.2) | 18 (11.8) | 1 (0.7) | p = 0.110, χ2(3) = 10.367 |
| 30–39 years (n = 1649) | 10 (8.5–11) | 932 (56.5) | 586 (35.5) | 117 (7.1) | 14 (8.4) | ||
| 40 years and over (n = 749) | 10 (8.5–11) | 396 (52.9) | 269 (35.9) | 76 (10.1) | 8 (1.1) | ||
| Residence | |||||||
| urban (n = 2268) | 10 (8.5–11) | p = 0.187 | 1256 (55.4) | 807 (35.5) | 185 (8.2) | 20 (0.9) | p = 0.870, χ2(3) = 0.715 |
| rural (n = 282) | 10 (8–11) | 150 (53.2) | 103 (36.5) | 26 (9.2) | 3 (1.1) | ||
| Educational level | |||||||
| unfinished general school (n = 2) | NA | p < 0.001, H(4) = 76.221, d = 0.342 | 2 (100) | 0 | 0 | 0 | p < 0.001, χ2(12) = 97.609, V = 0.113 |
| completed general school (n = 6) | 8.5 (7.9–9.5) | 0 | 6 (100) | 0 | 0 | ||
| vocational school (n = 10) | 9 (5.9–10) | 4 (40.0) | 3 (30.0) | 3 (30.0) | 0 | ||
| high school (n = 146) | 8.3 (6.5–10) | 46 (31.5) | 60 (41.1) | 35 (24.0) | 5 (3.4) | ||
| post-high school (n = 89) | 9.5 (8.5–11) | 43 (4.8) | 36 (40.4) | 10 (11.2) | 0 | ||
| university studies (n = 2297) | 10 (8.5–11) | 1311 (57.1) | 805 (35.0) | 163 (7.1) | 18 (0.8) | ||
| Number of children | |||||||
| 1 child (n = 1398) | 10 (8.5–11) | p = 0.189 | 745 (53.3) | 530 (37.9) | 115 (8.2) | 8 (0.6) | p = 0.038, χ2(12) = 21.975, V = 0.054 |
| 2 children (n = 1047) | 10 (8.5–11) | 601 (57.4) | 344 (32.9) | 90 (8.6) | 12 (1.1) | ||
| 3 children (n = 93) | 10.5 (9–11.5) | 53 (57.0) | 32 (34.4) | 6 (6.5) | 2 (2.1) | ||
| 4 children (n = 11) | 10.5 (7.5–11) | 7 (63.6) | 3 (27.3) | 0 | 1 (9.1) | ||
| 5 children (n = 1) | NA | 0 | 1 (100) | 0 | 0 | ||
| Knowledge Rating/Knowledge Score | Have You Given at Least One Optional Vaccine to at Least One of Your Children? | Statistical Analysis | |
|---|---|---|---|
| Yes, n (%) | No, n (%) | ||
| Very good | 1172 (60.5) | 234 (38.2) | p < 0.001, χ2 = 93.9, OR = 2.5, 95% CI: 2.1–3.0 |
| Good | 636 (32.8) | 274 (44.7) | p < 0.001, χ2 = 28.6, OR = 1.7, 95% CI: 1.4–2.0 |
| Sufficient | 120 (6.2) | 91 (14.8) | p < 0.001, χ2 = 45.9, OR = 2.6, 95% CI: 2.0–3.5 |
| Insufficient | 9 (0.5) | 14 (2.3) | p < 0.001, χ2 = 18.0, OR = 5.2, 95% CI: 2.2–12.0 |
| Score | 10 (IQR: 9–11.5) | 9 (IQR: 7–10.5) | p < 0.001, U = 403203, z = −11.014, r = 0.22 |
| Type of Vaccine | Number of Vaccines Administered | Total, n (%) | |||
|---|---|---|---|---|---|
| 1st Child | 2nd Child | 3rd Child | 4th Child | ||
| Rotavirus vaccine | 1165 | 500 | 41 | 2 | 1708 (28.1) |
| Varicella vaccine | 945 | 293 | 28 | 1 | 1267 (20.9) |
| Pneumococcal conjugate vaccine | 0 | 0 | 0 | 0 | 0 (0) |
| Meningococcal vaccine ACYW serogroups | 460 | 125 | 14 | 1 | 600 (9.9) |
| Meningococcal vaccine B serogroup | 316 | 91 | 11 | 0 | 418 (6.9) |
| Live attenuated influenza vaccine | 354 | 107 | 8 | 0 | 469 (7.7) |
| Influenza inactivated vaccine | 834 | 304 | 25 | 1 | 1164 (19.2) |
| Hepatitis A vaccine | 286 | 86 | 8 | 0 | 380 (6.3) |
| I don’t know/I forgot | 34 | 20 | 8 | 0 | 62 (1.0) |
| Total | 4394 | 1526 | 143 | 6 | 6069 (100) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Miron, V.D.; Toma, A.R.; Filimon, C.; Bar, G.; Craiu, M. Optional Vaccines in Children—Knowledge, Attitudes, and Practices in Romanian Parents. Vaccines 2022, 10, 404. https://doi.org/10.3390/vaccines10030404
Miron VD, Toma AR, Filimon C, Bar G, Craiu M. Optional Vaccines in Children—Knowledge, Attitudes, and Practices in Romanian Parents. Vaccines. 2022; 10(3):404. https://doi.org/10.3390/vaccines10030404
Chicago/Turabian StyleMiron, Victor Daniel, Andrei Răzvan Toma, Claudiu Filimon, Gabriela Bar, and Mihai Craiu. 2022. "Optional Vaccines in Children—Knowledge, Attitudes, and Practices in Romanian Parents" Vaccines 10, no. 3: 404. https://doi.org/10.3390/vaccines10030404
APA StyleMiron, V. D., Toma, A. R., Filimon, C., Bar, G., & Craiu, M. (2022). Optional Vaccines in Children—Knowledge, Attitudes, and Practices in Romanian Parents. Vaccines, 10(3), 404. https://doi.org/10.3390/vaccines10030404







