Abstract
Vaccination is vital to protect the public against COVID-19. The aim of this systematic review is to identify and evaluate the effectiveness of interventions to increase COVID-19 vaccine uptake. We searched a range of databases (Embase, Medline, Psychology & Behavioral Science, PsycInfo, Web of Science and NIH Preprints Portfolio) from March 2020 to July 2021 for studies which reported primary quantitative or qualitative research on interventions to increase COVID-19 vaccine uptake. Outcome measures included vaccination uptake and reported intention to vaccinate. Reviews, position papers, conference abstracts, protocol papers and papers not in English were excluded. The NHLBI quality assessment was used to assess risk of bias. In total, 39 studies across 33 papers met the inclusion criteria. A total of 28 were assessed as good quality. They included interventions relating to communication content, communication delivery, communication presentation, policy or vaccination delivery, with 7 measuring vaccination uptake and 32 measuring vaccination intention. A narrative synthesis was conducted, which highlighted that there is reasonable evidence from studies investigating real behaviour suggesting that personalising communications and sending booking reminders via text message increases vaccine uptake. Findings on vaccination intention are mixed but suggest that communicating uncertainty about the vaccine does not decrease intention, whereas making vaccination mandatory could have a negative impact. Although much of the research used experimental designs, very few measured real behavioural outcomes. Understanding which interventions are most effective amongst vaccine-hesitant populations and in the context of booster vaccinations will be important as vaccine roll outs continue across the world.
1. Introduction
A key measure in the fight against COVID-19 is vaccination. Vaccination programmes were launched across the world from December 2020, with many countries having now vaccinated a substantial proportion of their population. At the time of writing, 62.8% of the global population have received at least one dose of the vaccine and 55.4% are fully vaccinated, although there are large discrepancies in vaccination rates between countries [1]. In the UK, 85% of the population aged 12+ have received the first two doses and 66.1% have received a booster dose [2]. Given that high rates of vaccination are required to ensure the population is adequately protected, and in light of the role of booster vaccination in combating the threat of new variants [3], it is necessary to identify how to effectively increase COVID-19 vaccine uptake.
Vaccine hesitancy is complex, with a plethora of underlying concerns. Some of these concerns pertain to vaccinations more broadly [4,5], whilst others are specific to the context of COVID-19. For example, it has been reported that there are concerns regarding the speed at which vaccines were developed [5], as well as worries regarding vaccine effectiveness, side-effects and safety of the COVID-19 vaccine [4,6]. In addition to barriers relating to knowledge and beliefs, there are also environmental barriers, such as vaccine shortages, inaccessible vaccination sites and ability to get time off work, which can serve as barriers even amongst the most willing [7,8]. Barriers are also not universal; therefore, it is important to understand the extent to which interventions are effective amongst specific groups. For example, some younger people do not perceive the vaccine to be necessary for those at low risk of harm from the virus [9]; pregnant women have specific concerns for their baby [10]; and asylum seekers may fear persecution [11].
In addition to understanding the barriers to vaccine uptake, it is also necessary to draw from published literature concerning effective interventions to identify what is likely to work for increasing vaccine intentions and behaviours. Existing interventions have included communication campaigns, incentivisation and reminders. It is important to understand the extent to which these interventions impacted vaccine uptake so that future interventions can build upon their successes and address their limitations. We conducted a systematic review to identify and evaluate the effectiveness of interventions which can increase COVID-19 vaccine uptake. Given that this review is taking place at a time where the published literature on interventions implemented during the vaccine rollout is still in its relative infancy, the scope of this review was broad and included global studies on either COVID-19 vaccination intention or behaviour.
2. Materials and Methods
The research methods of this review are reported following the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRIMSA) statement [12] (the PRISMA checklist for each item is included in Supplementary Table S1). The protocol for this review was prospectively registered on PROSPERO, Internal Prospective Register of Systematic Reviews, registration number: CRD42021266943 (https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=266943 (accessed on 14 January 2022)).
2.1. Eligibility Criteria
Studies were eligible if they were primary quantitative or qualitative research on interventions to increase COVID-19 vaccine uptake. Outcome measures included measures of uptake, either through self-reports, observations or vaccination records; measures of uptake intentions; and measures of vaccine hesitancy. Studies which explored attitudes towards vaccine uptake or the demographic determinants of vaccine uptake without reporting possible interventions were excluded as this review was primarily focused on identifying effective interventions. Published research and pre-publication articles were included. Reviews, position papers, conference abstracts, protocol papers, unpublished studies and studies published in languages other than English were excluded.
2.2. Search
A systematic search was conducted by UKHSA Knowledge and Library Services in July 2021 for papers between March 2020 and July 2021. Sources searched included Embase, Medline, Psychology & Behavioral Science, PsycInfo, Web of Science and NIH Preprints Portfolio. Search terms included terms related to COVID-19 (e.g., COVID-19, coronavirus, and SARS-CoV-2), vaccination (e.g., vaccination, immunisation, and uptake) and interventions (e.g., intervention, message, and behaviour change). A complete list of search terms is available in Supplementary Table S2. A Google search for relevant papers was also conducted by the study authors in July 2021 for any other relevant papers not returned by the search.
2.3. Study Identification
The study identification process is detailed in Figure 1. FM and EB conducted initial title and abstract screening of all records on Rayyan, a review screening website [13]. Two of the reviewers (FM and EB) then screened the full text of relevant records, with each reviewer screening half of the records. The main reasons for exclusion were studies reporting the wrong outcome (e.g., flu vaccine uptake), studies not reporting an intervention or studies being the wrong publication type (e.g., review and protocol). After all texts were independently reviewed, the studies identified as eligible were then discussed by FM and EB to make sure they met the inclusion criteria, at which point a further six reports were excluded. At this stage, studies were excluded either because they focused on outcomes (e.g., vaccine misinformation) or methods (e.g., modelling) outside of our inclusion criteria. By the end of this process, 39 studies were deemed eligible and included in this review. A list of included studies with their methodological characteristics is available in Supplementary Table S3.
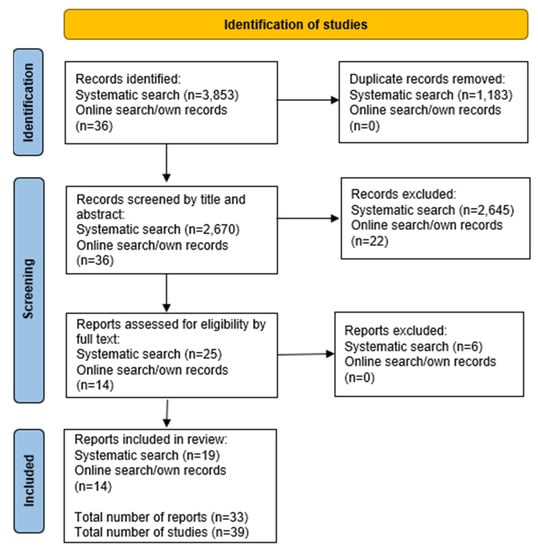
Figure 1.
PRISMA flow diagram of the identification of studies.
2.4. Data Extraction
Two of the reviewers (FM and EB) each independently extracted the data from half of the included studies. FM and EB checked the full extracted dataset for accuracy and completeness. They extracted the following data: author, year of publication, report type, study design, participant characteristics, recruitment method, time point of data collection, country of study, intervention type, intervention description, intervention comparison description, vaccine uptake measure, and effectiveness of intervention. All results relating to vaccination uptake or intentions were included.
2.5. Risk of Bias Assessment
The original protocol considered using RoB-2 for randomised studies and ROBIN-I for non-randomised studies, but the National Heart, Lung and Blood Institute (NHLBI) quality assessment tools were deemed more suitable for the included studies given there were case–control studies [14]. Two reviewers (FM and EB) conducted a risk of bias assessment on the included studies using the NHLBI tools for controlled intervention studies, cross-sectional studies and case–control studies, with each reviewer independently assessing half of the studies. Before assessing the quality of the studies, FM and EB discussed the criteria to ensure consistent rating. Each author then independently assessed the quality of half of the studies each, and classified each study as being of good, fair or poor quality. FM and EB then cross-assessed a further 10 studies, blinded to the first assessment made by the other reviewer, so that 50% of the studies had been independently assessed twice to ensure consistency in the risk of bias assessment. Any disagreements were resolved through discussion by FM and EB.
2.6. Data Synthesis
A systematic narrative synthesis was conducted which summarises the characteristics and findings of the included studies. Studies were categorised by type of intervention by two of the reviewers (FM and EB) and reviewed by the remaining reviewers (LJ, CS, and DW). The final categories were communication content, communication presentation, communication delivery, policy and vaccination delivery. Findings were interpreted by considering the study context, population, methodology and data quality. Due to the variability in interventions and outcomes, the reviewers did not compute summary statistics or effect size estimates.
When assessing the effectiveness of an intervention, the authors considered potential limitations, including outcome measures, study design, lack of comparators and publication status. When considering possible causes of heterogeneity amongst study results, the reviewers used the explanations provided by the study authors. Due to the limited number of papers for each type of outcome and intervention, the reviewers did not perform any formal analysis to assess heterogeneity.
3. Results and Discussion
A summary of the characteristics of each study can be found in Table 1 (full details in Supplementary Table S2). Across the 39 included studies, a range of interventions to increase COVID-19 vaccine uptake were reported relating to communication delivery, communication content, communication presentation, policy and vaccine delivery. In total, 32 studies measured vaccination intention and 7 measured vaccination behaviour (vaccination rates or scheduled appointments). Interventions were tested with a range of methods, most commonly online randomised controlled trials (RCTs) (20 studies) but also including field RCTs, online experiments (including discrete choice experiments, often used in health care [15]), quasi-experimental and cross-sectional studies. The included studies were tested in a range of countries, including the UK, the US, Germany, Japan, China, Hong Kong and Israel. Most studies were from the US (22 studies), with 9 studies from the UK. Findings are presented by type of intervention and outcome measure (real behaviour or intention).

Table 1.
Characteristics of included studies.
3.1. Risk of Bias Assessment
The overall quality of the studies was good. For controlled intervention studies, 24 studies were rated as good and 7 as fair. For cross-sectional studies, 2 studies were rated as good, 1 as fair and 2 as poor. For case–control studies, 2 studies were rated as good and 1 as fair. The most common reason for a fair quality rating was because the studies did not report methodological details such as blinding and drop-out rates. The reason two studies were rated as poor quality was because differences in outcome pre- and post-intervention for cross-sectional studies without a control were inferred from only one measure taken after the intervention. The risk of bias assessment for each study can be found in Supplementary Table S4.
3.2. Communication Content
3.2.1. Benefits of Vaccination
Vaccination Behaviour
A field RCT (pre-print) found that communicating the personal and collective benefits of vaccination did not increase uptake. In particular, it found that text message booking reminders increased uptake regardless of their message content, including whether it referred to protecting oneself and others or to vaccination offering a fresh start after a tough year [16]. However, a further field RCT (pre-print) found that text messages communicating the personal or social benefit increased vaccination uptake [17].
Vaccination Intention
Studies testing whether communicating the personal and collective benefits of vaccination increases vaccination intention have yielded mixed findings. An online RCT found that a news story communicating the personal health risks of not getting vaccinated, and another communicating the collective public health consequences of not getting vaccinated, increased vaccination intention [18]. Another online RCT (pre-print), measuring a digital expression of interest, found that after watching a video promoting the health benefits of the COVID-19 vaccine, 16% of unvaccinated participants wanted more information [19]. This proportion of participants was similar to those who watched a video including the promotion of cash lotteries, although less effective than a video promoting states using cash vouchers. Another online RCT found that messages emphasising personal benefit, collective benefit or both did not affect vaccine hesitancy in their overall sample but did have effects among hesitant individuals, where emphasising personal benefit reduced vaccine hesitancy, as did combining personal and collective benefits, the seriousness of the pandemic and addressing safety concerns, with personal benefit leading to the greatest reduction in hesitancy [20]. They also found demographic differences, as Asian individuals showed a greater reduction in hesitancy when collective and personal benefits were combined, whilst men had less hesitancy than women in the personal benefits condition [20].
Other studies found that communicating the personal and collective benefits of vaccination did not increase uptake. An online RCT found that communicating rapid uptake of the vaccine as being important to reduce infections and protect others did not influence vaccination intentions [21]. Another online RCT (pre-print) found that a fact box communicating the risk of getting a COVID-19 vaccine compared to the risk of getting the COVID-19 virus had no impact on vaccination intention [22]. The authors suggest this could be because the fact box highlighted risks relating to the vaccine which participants paid more attention to or may not have previously been aware of. Finally, a news story communicating the economic costs of not getting vaccinated did not affect vaccination intention in an online RCT [18].
3.2.2. Effectiveness and Safety
Vaccination Behaviour
Communicating the effectiveness and safety of the vaccine can increase uptake. A field experiment (pre-print) found that a booking reminder emphasising vaccine effectiveness was more effective than one emphasising social benefits and others having had the vaccine [17]. Another field RCT found that an email comparing the risks of the COVID-19 vaccine to the more severe risks of the virus increased uptake [23]. However, this intervention had a similar impact on uptake as an email focusing on social norms. The authors also acknowledged that it was difficult to isolate the effects of effectiveness and safety as both emails also had components of personalisation, scarcity and active choice.
Vaccination Intention
Research exploring the role of describing the safety and effectiveness of vaccines on vaccination intention is mixed. A study found that a message emphasising that the NHS declares the vaccine safe and effective increased vaccination intention [24]. This was echoed in an online experiment, particularly amongst vaccine-hesitant individuals [25]. However, neither study can identify whether safety or effectiveness had a greater effect. Similarly, an online RCT found that a news story about the vaccine being safe and effective increased vaccination intention [26]. However, another online RCT found that a range of interventions communicating effectiveness and safety were not more effective than the control [27]. Furthermore, another online experiment presented the risks of the COVID-19 vaccine in comparison to the risks of the COVID-19 virus and found that it did not increase vaccination intention [22]. Finally, two online RCTs tested whether communicating that the COVID-19 vaccine is more effective than the flu vaccine increased vaccination intention. One in the UK found that this was effective [25], whereas one in the US did not [28].
The level of effectiveness and safety of vaccines can impact vaccination intention. An online discrete choice experiment (DCE) found that decreasing effectiveness from 70% to 50% and decreasing duration of immunity from 6 to 3 months reduced vaccine uptake [29]. Similarly, a study (pre-print) found that vaccines with 95% efficacy are preferred to 50% or 70% efficacy [30]. However, an alternative study found no impact of news articles stating 80% vs. 20% effectiveness [31]. Relating to safety, a DCE found that increasing the risk of side-effects reduced intentions [29], while a cross-sectional study (pre-print) found that less risk of side-effects is preferable [30]. This cross-sectional study also found that a protection scheme (i.e., medical insurance) to compensate for side-effects can increase intentions.
3.2.3. Vaccine Development
Vaccination Intention
Addressing concerns about the speed of vaccine development has mixed effects on vaccination intention. In an online RCT, doing so decreased vaccine hesitancy in strongly hesitant individuals [20]. Furthermore, in an online experiment (pre-print), participants were more likely to accept less effective vaccines if the development process took 12 rather than 7 months [32]. However, a message detailing the development process (pre-print) did not increase vaccination intention compared to no message in an online RCT in the US [22]. An online RCT found that a news story highlighting the rigours of clinical trials did not increase vaccination intention, whereas not highlighting the rigours of clinical trials did increase vaccination intention [18]. Finally, a news story highlighting that President Trump pushed for rapid approval of vaccines decreased intention [26].
3.2.4. Social Norms
Vaccination Behaviour
Social norm interventions asking recipients to ‘join the millions’ being vaccinated can be effective. A field experiment (pre-print) found that a booking reminder emphasising to ‘join the 3.5 million vaccinated citizens’ increased vaccine uptake, but to a lesser extent than one emphasising the personal benefit of getting vaccinated [17]. Another field RCT with unvaccinated health care workers found that sending an email telling them that more than 11 million Americans, including many of their colleagues, had been vaccinated increased uptake [23]. However, this effect was similar to the effect of an email comparing the risks of the vaccine to the more severe risks of COVID-19.
Vaccination Intention
Emphasising that others will or have been vaccinated has variable effects on vaccination intention. In an online RCT, a news story about others being willing to get vaccinated increased intention, while a news story about others being unwilling to get vaccinated decreased intention [26]. In an online RCT (pre-print), participants who received accurate information about levels of vaccine acceptance showed increased vaccination acceptance, particularly amongst those unsure about receiving the vaccine and in certain countries (e.g., Pakistan and Vietnam) [33]. The authors suggest this could be due to people underestimating the extent to which others would get vaccinated at the time (October 2020). However, although communicating in an online RCT that 85% of people plan to take the vaccine was more effective than communicating that 45% of people plan to take the vaccine, neither were more effective than no information [24].
3.2.5. Herd Immunity
Vaccination Intention
An online RCT found that a news story emphasising the necessary coverage rate of vaccination to achieve herd immunity increased vaccination intention compared to an unrelated news story [18]. Previous experimental evidence also suggests that communicating about herd immunity can increase vaccine uptake [34,35].
3.3. Communication Presentation
3.3.1. Personalisation
Vaccination Behaviour
Personalising vaccination invitations can be effective. A field RCT (pre-print) found that text message booking reminders emphasising personalisation increased uptake [16]. A follow-up field RCT found that sending a second reminder increased uptake regardless of the message content, including whether it referred to the individual being one of the few to have early access to the vaccine [16].
Vaccination Intention
In an online experiment (pre-print), a text message booking reminder emphasising personalisation did not increase intention [16]. This is particularly noteworthy as an identical field RCT, run concurrently to the online experiment, found the opposite effect, as mentioned in the preceding section [16].
3.3.2. Framing
Vaccination Intention
There was mixed effectiveness of framing on vaccination intention, although the evidence is limited. An online experiment (pre-print) found that positive framing of vaccine safety (95% safe) increased acceptance of less effective vaccines compared to negative framing (5% unsafe) [32]. On the other hand, an online RCT did not find a difference in intention when a news article framed vaccination protection against the virus negatively as opposed to positively [31]. An online RCT did not find a difference in intention when describing a vaccination lottery prize as a gain compared to a loss [36].
3.3.3. Numerical Format
Vaccination Intention
An online RCT did not find a difference in vaccination intention between presenting effectiveness as a percentage or as a frequency [31]. An online RCT did not find a difference between presenting vaccination lottery winners as ‘5 total winners’ to ‘1 winner for each of the 5 weeks’ [36].
3.3.4. Uncertainty
Vaccination Intention
Communicating uncertainty could increase intentions and protect existing intentions in the event of changes in information about the vaccine. An online RCT found some evidence that communicating uncertainty about COVID-19 increased vaccination intentions, which was also the case in the presence of an uncertainty-normalising intervention [37]. Two online RCTs did not find an effect of communicating uncertainty about vaccine effectiveness on vaccination intention compared to communicating with certainty [27,38]. In addition, communicating that there is uncertainty relating to effectiveness at the outset can mitigate a reduction in vaccination intention once conflicting information on effectiveness arises later on (pre-print) [38].
3.4. Communication Delivery
3.4.1. Messenger
Vaccination Intention
There was mixed evidence for the effect of messengers on intention. An online DCE (pre-print) found that text message reminders were preferred if delivered by the NHS or one’s GP, rather than one’s best friend [39]. An online RCT (pre-print) found that a Republican endorsement of the vaccine through a video and short essay was more effective than a Democrat endorsement intentions among Republican or Republican leaning participants [40]. An online RCT found that a news story indicating that President Trump pushed vaccines for rapid approval decreased vaccination intention, regardless of party identification [26]. Finally, whether a newspaper opinion piece about the importance of COVID-19 vaccination was written by a lay person (i.e., ordinary people recounting their experience with the virus) or a medical expert did not affect intention [18].
3.4.2. Chatbot
Vaccination Intention
A cross-sectional study (pre-print) found that a chatbot implemented via the most popular messenger app in Japan increased vaccination intentions. However, this was a low quality study with no control group and pre- and post-vaccine intentions were measured after the intervention [41].
3.4.3. Video
Vaccination Behaviour
A field experiment (pre-print) found that adding educational videos to reminders to schedule COVID-19 vaccines did not increase the effectiveness of the reminders [16].
Vaccination Intention
There is mixed evidence regarding the effectiveness of videos in increasing vaccination intentions. An online experiment (pre-print) found that adding educational videos to reminders to schedule COVID-19 vaccines increased the effectiveness of a reminder and led to an increase in participants reported likelihood of scheduling an appointment [16]. An online RCT (pre-print) found that 22% of unvaccinated respondents expressed wanting further information on the vaccine after watching a video containing information on the health benefits of the vaccine and a cash voucher incentive for vaccination, compared to 14–16% for a video with lottery incentives or a standard information video without an incentive, respectively [19]. An online RCT (pre-print) found that only a male-narrated video providing details about the COVID-19 vaccine and emphasising the altruistic motivations associated with vaccination increased intention [42]. According to the authors, this could be due to politically conservative individuals within the sample who had lower vaccination intentions after a female-narrated video. However, the authors did not provide further information about controlling for extraneous differences between the narrator conditions, such as speaking style, which may have also accounted for the difference in effect. Finally, a study found that patients who watched a video discussing the COVID-19 vaccine were more likely to receive the COVID-19 vaccine than before watching the video, although intentions were only assessed after the intervention with no direct measure of pre-intervention intentions [43].
3.4.4. Reminders
Vaccination Behaviour
Reminders increase vaccine uptake. A field RCT (pre-print) found that sending a second reminder to individuals eligible for vaccination who had not yet scheduled their first dose increased uptake [16]. Reminders with an emphasis on personalisation increased uptake, whereas adding an educational video did not increase uptake. Participants were then sent another reminder which increased uptake further, with all message types increasing uptake to a similar extent [16]. A field experiment (pre-print) found that sending a second reminder increased uptake, with the reminder emphasising personal benefits being more effective than the one emphasising social benefit [17].
Vaccination Intention
In an online experiment (pre-print), a text message booking reminder emphasising personalisation did not increase intention, unlike in the field RCT, of which it was a replication, where it increased uptake [16].
3.5. Policy
3.5.1. Mandatory Vaccination
Vaccination Intention
The impact of mandatory vaccination depends on the initial vaccination intention. Two similar online RCTs found that there is high psychological reactance (i.e., negative emotions) to mandatory vaccination when individuals have a low intention to receive the vaccine [44]. One RCT also found that increased reactance led to higher intentions to avoid the COVID-19 vaccine, particularly for the mandatory condition. Participants were also more likely to take action (e.g., through activism) against the policy when the vaccine was mandatory, compared to unrestricted [44]. This supports research beyond the scope of this review, including a modelling study of COVID-19 vaccine uptake [45] and interviews with care home staff (pre-print) which suggests mandatory vaccination could lead to staff resignations [46].
3.5.2. Vaccination Proof
Vaccination Intention
A DCE found that offering proof of vaccination increased vaccine uptake amongst individuals who want a vaccine card, compared to no proof, but it did not impact uptake amongst those who do not want proof [29].
3.5.3. ‘Opt-Out’ Vaccination
Vaccination Intention
An online experiment found that pre-scheduling a vaccination appointment for an individual increased vaccine intention compared to asking participants if they wanted to receive the vaccine [47]. Another online study (pre-print) found that pre-selecting ‘yes’ or ‘no’ options as responses for wanting to receive the vaccine did not have an impact on vaccine acceptance [32].
3.5.4. Prioritising Vaccination
Vaccination Intention
Two online RCTs reported that individuals with a high intention to receive the vaccine had high psychological reactance (i.e., negative emotions) when the vaccine is scarce and not widely available to them until 2022 [44].
3.5.5. Legal Incentives
Vaccination Intention
An online RCT (pre-print) found that legal incentives, such as no longer being required to wear a face covering or to provide a negative test to access events, did not impact vaccination intention, compared to no legal incentive [48].
3.5.6. Monetary Incentives
Vaccination Behaviour
Three quasi-experimental studies have found mixed results on the impact of monetary incentives on vaccination rates. When comparing the number of vaccine doses administered daily per 100,000 individuals between States with and without monetary incentives, one study (pre-print) found a decline in vaccinations between April and July 2021 in all States, irrespective of monetary incentive [49]. The authors suggest that as 40% of individuals were already fully vaccinated when incentives were introduced, small rewards or low-probability lotteries were perhaps insufficiently persuasive to the unvaccinated individuals.
Two studies have looked more specifically at the effectiveness of Ohio’s ‘Vax a Million’ programme, which awarded five people $1 million. One study found that vaccination rates, per 100,000 individuals, did not increase after the lottery was introduced [50]. They also found a decline in uptake in the rest of the US, but Ohio declined to a greater extent [50]. Another study (pre-print) found that Ohio did not have greater vaccination after the introduction of the incentive when comparing to an average of the US; but when using a synthetic control, they found that Ohio’s initiative did increase vaccinations [51]. They report that the incentive initiative encouraged 1.5% of Ohioans (i.e., 82,000 individuals) to receive the vaccine who would otherwise not be vaccinated [51].
Vaccination Intention
An online experiment found no effect of financial reward on willingness to be vaccinated [21], whilst another study (pre-print) found that a free of charge vaccine with a government subsidy reduced the likelihood of choosing to be vaccinated [30]. However, other evidence suggests that monetary incentives could potentially increase vaccine uptake, although the evidence is not clear on the optimum price. An online experiment (pre-print) found that monetary incentives above 3250 euros increased willingness to get vaccinated [48]. Incentives worked best amongst younger people and those who had less confidence in the vaccine and were more complacent about COVID-19. Similarly, another online experiment in the US found that vaccination intention increased by 4.5 percentage points from 70% with a $100 compensation and by 13.6 percentage points with $500 compared to $0 [47]. Importantly, small compensations backfired; the $20 compensation reduced intentions by 5 percentage points compared to no compensation. Finally, another German online experiment in November 2020 found no effect of financial reward on willingness to be vaccinated, after asking participants to imagine they had received a financial reward for getting vaccinated ranging between 25 and 200 euros, even after controlling for their financial situation [21].
While cash amounts could increase vaccination intentions, the evidence suggests that lotteries are less effective. An online RCT (pre-print) found no difference in expression of further interest in vaccination information between control and lottery conditions, but found that cash vouchers did increase the number of interested individuals [19]. Another online RCT (pre-print) compared 12 conditions varying the distribution of $5million and found that vaccination intention did not differ across conditions; indeed intentions post-incentive were strongly associated with baseline willingness [36]. In a second online RCT, this study altered the message framing of the lottery (e.g., gain vs. loss) and the numeric framing (e.g., 5 total winners vs. 1 winner for each of the 5 weeks) and again found no difference in vaccination intention [36].
3.5.7. Cost
Vaccination Intention
Requiring people to pay for vaccines is likely to reduce vaccine uptake. One study (pre-print) found that charging HKD700 (£65) and HKD400 (£37) made the vaccines less likely to be chosen than a free vaccine [30].
3.6. Vaccination Delivery
3.6.1. Setting
Vaccination Intention
A DCE found that nearby GP surgeries were the most preferred vaccination location, whilst a nearby pharmacy and drive-thru were the least preferred [39]. Additionally, an online experiment found that more participants chose to receive their vaccine in 3 weeks at their local GP compared to in 5 days in a mass vaccination centre [52]. However, more participants chose an earlier appointment at either a local GP or a mass vaccination centre rather than having a health care professional come to their home at a later date. In addition, a US discrete choice experiment suggests that preferred locations vary between individuals, which can impact uptake. Those who prefer a medical setting were less likely to choose a vaccine at a community-based vaccination centre, whereas those who prefer a community setting were less likely to choose a vaccine at a medical vaccination setting [29].
3.6.2. Proximity
Vaccination Intention
A DCE found that a vaccination centre that was 15–30 min away was preferable to a centre less than 15 min away and 30–45 min away [39], which the authors posit could be because individuals had a specific vaccination centre in mind when considering the choices which were more likely to be 15–30 min away. Additionally, more respondents preferred to receive the vaccine within 3 weeks at a centre 10 min away compared to a centre 1 h away within 5 days [52]. This is supported by research (pre-print) published after this review was conducted which found an association between proximity of vaccine centre and vaccine uptake [8].
3.6.3. Appointments
Vaccination Intention
A DCE found that weekday appointments after-hours were least preferred compared to a weekday 9 a.m.–5 p.m. or a weekend, although this had less of an impact on decision making than factors such as setting and proximity (as detailed above) [39]. An online experiment found that people preferred to wait 3 weeks for an appointment if they can choose their appointment time compared to receiving the vaccine within 5 days but not finding out their appointment time until the day [52]. This study also found that individuals preferred to book a specific timeslot, as opposed to attending a vaccination centre without pre-booking a specific time. However, as the walk-in centre was coupled with an appointment in 3 weeks, it is difficult to identify which factor was less desirable.
3.6.4. Waiting Time
Vaccination Intention
A forced-choice study (pre-print) found that a wait of 7 and 14 days after registering to be vaccinated did not affect the likelihood of a vaccine being chosen, compared to no waiting time, but a delay of 30 days reduced the likelihood of a vaccine being chosen [30]. An online experiment identified that optimum waiting time is dependent on other components of the vaccine delivery process, including setting, proximity and control over appointment [52]. In particular, they found that two-thirds of people preferred to wait 3 weeks for an appointment, compared to 5 days, when vaccination sites are nearby, when one can choose their appointment time and when they can go to the local GP.
4. Recommendations
Recommendations for increasing COVID-19 vaccine uptake based on the findings of this review can be found in Table 2. The table specifies whether interventions have been tested on real behaviour and/or intentions, given that intentions do not necessarily translate into behaviour [53]. The average risk of bias assessment for each type of intervention is also provided (good, fair, and poor).

Table 2.
Recommendations for increasing vaccination.
5. Future Implications
Vaccination is vital to protect the public against COVID-19. As vaccine roll outs continue across the world, both for primary and booster doses, it is important to understand the effectiveness of existing interventions aiming to increase COVID-19 vaccine uptake. This review shows that a broad range of interventions have been tested to increase the uptake of COVID-19 vaccination, with reasonable evidence to suggest that personalising communications and sending text message booking reminders are effective interventions. This has implications for local and national health authorities with regards to the way they communicate with the public regarding their eligibility for vaccination. The heterogeneity of results, particularly amongst vaccine hesitant compared to vaccine accepters, also highlights the importance of understanding an intervention’s intended audience, and their existing barriers. Although this has been explored in an intervention addressing safety and effectiveness concerns [25], and one addressing access barriers [52], more research is needed to identify effective and acceptable interventions for encouraging vaccine uptake amongst these groups in particular.
Finally, there were mixed findings for many of the interventions, particularly for studies measuring vaccination intention. Additionally, although much of the research used experimental designs, very few measured real behavioural outcomes, and therefore it is important that future research builds upon the current evidence to identify under which circumstances interventions are effective at increasing vaccine uptake. Understanding which interventions are most effective amongst vaccine-hesitant populations and in the context of booster vaccinations will be important as vaccine roll outs continue across the world.
Future research should also take into consideration the barriers which are unique to booster doses of the COVID-19 vaccine, such as previous experience with side-effects, lack of awareness of the necessity of booster doses and feeling misled regarding the benefits of the primary vaccine doses [70].
6. Limitations
This review examines the cutting-edge and evolving literature concerning COVID-19 vaccination to highlight possible interventions that could be used to increase uptake of the COVID-19 vaccine. Furthermore, the potential utility for this review to also influence the uptake of non-COVID-19 vaccinations moving forwards is undeniable. However, as with all research, there are limitations and caveats that must be borne in mind. First, although much of the research used experimental designs where the intervention was compared to either another intervention or a control group, very few measured scheduled appointments or actual vaccine uptake. Most focused on measures of intention or vaccine hesitancy rather than uptake data, and often involved online experiments presenting participants with hypothetical scenarios. Although this provides preliminary insight into the effectiveness of interventions, it does not always reflect real-life behaviours [16]. In addition, a minority of studies did not include a control group [32,43], so it is not possible to identify the extent of the intervention’s effectiveness.
It is also important to acknowledge that many studies sampled the general population, and therefore are likely to include individuals who already intend to receive the COVID-19 vaccine. Interventions need to tackle the barriers of groups who are more likely to be vaccine hesitant based on previous research, such as those living in a high deprivation area, some ethnic minority groups and those with lower reading ages [9]. Moreover, the studies included here took place at various points throughout the pandemic, which means that participants across studies could have had varying levels of pre-intervention knowledge and beliefs about COVID-19 and the vaccine, which could influence the effectiveness of an intervention [31]. This review also included studies from a range of countries, meaning caution should be used when applying findings from one country to another. Replicating possible interventions in the target country would be beneficial, preferably with well-designed randomised controlled field trials.
This review included studies measuring either general COVID-19 vaccination intention or behaviour or behaviour relating to receiving the first dose but was conducted before the subsequent booster vaccination roll out. While there is no a priori reason to expect that interventions reported herein would be widely ineffective if applied to the context of booster vaccination (indeed, some of the interventions identified above echo barriers and facilitators identified in the pre-COVID-19 vaccination literature [71,72] and the preliminary global insights on booster vaccinations [73,74]), further review work is recommended to bolster the evidence base for effective vaccination interventions. This is particularly pertinent given the novelty of COVID-19 booster vaccinations. Indeed, given the rapidly developing nature of the COVID-19 vaccine rollout and accompanying intervention design and evaluation, it will be important to continue to iterate this review beyond the end of the COVID-19 pandemic in order to capture best evidence for informing future vaccination programmes.
Finally, there are limitations relating to the conduct of this review. Given the range of interventions and outcomes included, it was not possible to provide effect measures for each study and compare these numerically or visually across studies. The two researchers assessing studies for inclusion discussed the set of studies initially identified as eligible after they each independently screened half of the studies. They did not double code or discuss the studies that were not deemed eligible. Formal methods of assessing heterogeneity between studies and confidence in the body of evidence were not used. This was to ensure this review was carried out in a timely manner and could adequately feed into COVID-19 vaccination programmes. Instead, the authors make clear in the table of recommendations (Table 2) which interventions lack clear evidence.
7. Conclusions
Across 39 studies, this systematic review shows that a broad range of interventions have been tested to increase the uptake of COVID-19 vaccination, tackling various aspects of communications, policy and delivery. We find reasonable evidence investigating real behaviour suggesting that personalising communications and sending text message booking reminders are effective. Findings on vaccination intention are mixed but suggest that communicating uncertainty about the vaccine does not decrease intention, whereas making vaccination mandatory could have a negative impact. However, the lack of evidence and the mixed findings in other areas warrant further research, ideally based on observed vaccination behaviour.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/vaccines10030386/s1, Table S1: PRISMA 2020 checklist; Table S2: Search terms; Table S3: Table of included studies; Table S4: Risk of bias.
Author Contributions
Conceptualisation, D.W.; methodology, E.B. and F.M.; formal analysis, E.B. and F.M.; writing—original draft preparation, E.B. and F.M.; writing—review and editing, C.S., L.F.J. and D.W.; visualisation, E.B. and F.M.; supervision, C.S., L.F.J. and D.W.; project administration, E.B. and F.M.; funding acquisition, D.W. All authors have read and agreed to the published version of the manuscript.
Funding
DW is supported by the National Institute for Health Research Health Protection Research Units (NIHR HPRU) in Emergency Preparedness and Response (grant number 200890), a partnership between UK Health Security Agency (UKHSA), King’s College London and the University of East Anglia, and the NIHR HPRU in Behavioural Science and Evaluation (grant number 200877), a partnership between UK Health Security Agency and the University of Bristol. The views expressed are those of the author(s) and not necessarily those of the NIHR, UKHSA or the Department of Health and Social Care. All authors had full access to the data and can take responsibility for the integrity of the data and the accuracy of the data analysis. No external funding organisation had a role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Acknowledgments
We thank the UKHSA Knowledge and Library Services for conducting the systematic search and advising us on the screening process.
Conflicts of Interest
The authors declare no conflict of interest. No external funding organisation had a role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
References
- Our World in Data. Coronavirus (COVID-19) Vaccinations 2021. Available online: https://ourworldindata.org/covid-vaccinations (accessed on 21 February 2022).
- UK Government. Coronavirus (COVID-19) in the UK 2022. Available online: https://coronavirus.data.gov.uk/ (accessed on 21 February 2022).
- Hogan, A.B.; Wu, S.L.; Doohan, P.; Watson, O.J.; Winskill, P.; Charles, G.; Barnsley, G.; Riley, E.M.; Khoury, D.; Ferguson, N.M.; et al. Report 48: The Value of Vaccine Booster Doses to Mitigate the Global Impact of the Omicron SARS-CoV-2 Variant 2021. Available online: https://www.imperial.ac.uk/media/imperial-college/medicine/mrc-gida/2021-12-16-COVID19-Report-48.pdf (accessed on 13 February 2022).
- Sherman, S.M.; Smith, L.E.; Sim, J.; Amlôt, R.; Cutts, M.; Dasch, H.; Rubin, G.J.; Sevdalis, N. COVID-19 vaccination intention in the UK: Results from the COVID-19 vaccination acceptability study (CoVAccS), a nationally representative cross-sectional survey. Hum. Vaccines Immunother. 2021, 17, 1612–1621. [Google Scholar] [CrossRef]
- Jennings, W.; Stoker, G.; Willis, H.; Valgardsson, V.; Gaskell, J.; Devine, D.; McKay, L.; Mills, M.C. Lack of trust and social media echo chambers predict COVID-19 vaccine hesitancy. medRxiv 2021. [Google Scholar] [CrossRef]
- Robertson, E.; Reeve, K.S.; Niedzwiedz, C.L.; Moore, J.; Blake, M.; Green, M.; Katikireddi, S.V.; Benzeval, M.J. Predictors of COVID-19 vaccine hesitancy in the UK household longitudinal study. Brain Behav. Immun. 2021, 94, 41–50. [Google Scholar] [CrossRef]
- Atad, E.; Netzer, I.; Peleg, O.; Landsman, K.; Dalyot, K.; Reuven, S.E.; Baram-Tsabari, A. Vaccine-Hesitant Parents’ Considerations Regarding COVID-19 Vaccination of Adolescents. medRxiv 2021. [Google Scholar] [CrossRef]
- Mazar, A.; Tomaino, G.; Carmon, Z.; Wood, W. Distance to Vaccine Sites is Associated with Lower COVID-19 Vaccine Uptake. PsyArXiv 2022. [Google Scholar] [CrossRef]
- Office for National Statistics. Coronavirus Vaccine Hesitancy in Younger Adults: June 2021. Available online: https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/healthandwellbeing/articles/coronavirusvaccinehesitancyinyoungeradults/june2021 (accessed on 17 February 2022).
- Zoe COVID Study. Would You Have a COVID Jab? 95% of ZOE COVID Symptom Study Users Say Yes 2021. Available online: https://covid.joinzoe.com/post/covid-vaccine-hesitancy (accessed on 17 February 2022).
- Deal, A.; Hayward, S.E.; Huda, M.; Knights, F.; Crawshaw, A.F.; Carter, J.; Hassan, O.B.; Farah, Y.; Ciftci, Y.; Rowland-Pomp, M.; et al. Strategies and action points to ensure equitable uptake of COVID-19 vaccinations: A national qualitative interview study to explore the views of undocumented migrants, asylum seekers, and refugees. J. Migr. Health 2021, 4, 100050. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan—a web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef] [Green Version]
- National Heart, Lung, and Blood Instiute. Study Quality Assessment Tools 2013. Available online: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (accessed on 11 October 2021).
- Clark, M.D.; Determann, D.; Petrou, S.; Moro, D.; de Bekker-Grob, E.W. Discrete choice experiments in health economics: A review of the literature. Pharmacoeconomics 2014, 32, 883–902. [Google Scholar] [CrossRef]
- Dai, H.; Saccardo, S.; Han, M.A.; Roh, L.; Raja, N.; Vangala, S.; Modi, H.; Pandya, S.; Croymans, D.M. Behavioral nudges increase COVID-19 vaccinations: Two randomized controlled trials. medRxiv 2021. [Google Scholar] [CrossRef]
- Berliner Senderey, A.O.R.; Perchik, R.; Erev, I.; Balicer, R. Encouraging Uptake of the COVID-19 Vaccine Through Behaviorally Informed Interventions: National Real-World Evidence from Israel. SSRN 2021. [Google Scholar] [CrossRef]
- Motta, M.; Sylvester, S.; Callaghan, T.; Lunz-Trujillo, K. Encouraging COVID-19 Vaccine Uptake Through Effective Health Communication. Front. Political Sci. 2021, 3, 630133. [Google Scholar] [CrossRef]
- Duch, R.M.; Barnett, A.; Filipek, M.; Roope, L.; Violato, M.; Clarke, P. Cash versus Lotteries: COVID-19 Vaccine Incentives Experiment. medRxiv 2021. [Google Scholar] [CrossRef]
- Freeman, D.; Loe, B.S.; Yu, L.-M.; Freeman, J.; Chadwick, A.; Vaccari, C.; Shanyinde, M.; Harris, V.; Waite, F.; Rosebrock, L.; et al. Effects of different types of written vaccination information on COVID-19 vaccine hesitancy in the UK (OCEANS-III): A single-blind, parallel-group, randomised controlled trial. Lancet Public Health 2021, 6, e416–e427. [Google Scholar] [CrossRef]
- Sprengholz, P.; Eitze, S.; Felgendreff, L.; Korn, L.; Betsch, C. Money is not everything: Experimental evidence that payments do not increase willingness to be vaccinated against COVID-19. J. Med. Ethics 2021, 47, 547–548. [Google Scholar] [CrossRef]
- Thorpe, A.; Fagerlin, A.; Butler, J.; Stevens, V.; Drews, F.A.; Shoemaker, H.; Riddoch, M.; Scherer, L.D. Communicating about COVID-19 vaccine development and safety. medRxiv 2021. [Google Scholar] [CrossRef]
- Santos, H.C.; Goren, A.; Chabris, C.F.; Meyer, M.N. Effect of Targeted Behavioral Science Messages on COVID-19 Vaccination Registration Among Employees of a Large Health System: A Randomized Trial. JAMA Netw. Open 2021, 4, e2118702. [Google Scholar] [CrossRef]
- Sinclair, S.; Agerström, J. Do Social Norms Influence Young People’s Willingness to Take the COVID-19 Vaccine? Health Commun. 2021, 1–8. [Google Scholar] [CrossRef]
- Davis, C.J.; Golding, M.; McKay, R. Efficacy information influences intention to take COVID-19 vaccine. Br. J. Health Psychol. 2021. [Google Scholar] [CrossRef]
- Palm, R.; Bolsen, T.; Kingsland, J.T. The Effect of Frames on COVID-19 Vaccine Resistance. Front. Political Sci. 2021, 3, 661257. [Google Scholar] [CrossRef]
- Kerr, J.R.; Freeman, A.L.J.; Marteau, T.M.; van der Linden, S. Effect of Information about COVID-19 Vaccine Effectiveness and Side Effects on Behavioural Intentions: Two Online Experiments. Vaccines 2021, 9, 379. [Google Scholar] [CrossRef] [PubMed]
- Trueblood, J.S.; Sussman, A.B.; O’Leary, D. The Role of Risk Preferences in Responses to Messaging About COVID-19 Vaccine Take-Up. Soc. Psychol. Personal. Sci. 2021, 13, 311–319. [Google Scholar] [CrossRef]
- Craig, B.M. United States COVID-19 Vaccination Preferences (CVP): 2020 Hindsight. Patient 2021, 14, 309–318. [Google Scholar] [CrossRef]
- Yuen, S.W.H.; Yue, R.P.H.; Lau, B.H.B.; Chan, C.L.W.; Ng, S.-M. When to be vaccinated? What to consider? Modelling decision-making and time preference for COVID-19 vaccine through a conjoint experiment approach. medRxiv 2021. [Google Scholar] [CrossRef]
- Chen, T.; Dai, M.; Xia, S.; Zhou, Y. Do Messages Matter? Investigating the Combined Effects of Framing, Outcome Uncertainty, and Number Format on COVID-19 Vaccination Attitudes and Intention. Health Commun. 2021, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Strickland, J.C.; Reed, D.D.; Hursh, S.R.; Schwartz, L.P.; Foster, R.N.S.; Gelino, B.W.; LeComte, R.S.; Oda, F.S.; Salzer, A.R.; Schneider, T.D.; et al. Integrating Operant and Cognitive Behavioral Economics to Inform Infectious Disease Response: Prevention, Testing, and Vaccination in the COVID-19 Pandemic. medRxiv 2021. [Google Scholar] [CrossRef]
- Moehring, A.; Collis, A.; Garimella, K.; Rahimian, M.; Aral, S.; Eckles, D. Surfacing norms to increase vaccine acceptance. PsyArXiv 2021. [Google Scholar] [CrossRef]
- Betsch, C.; Böhm, R.; Korn, L.; Holtmann, C. On the benefits of explaining herd immunity in vaccine advocacy. Nat. Hum. Behav. 2017, 1, 56. [Google Scholar] [CrossRef]
- Sprengholz, P.; Betsch, C. Herd immunity communication counters detrimental effects of selective vaccination mandates: Experimental evidence. EClinicalMedicine 2020, 22, 100352. [Google Scholar] [CrossRef]
- Taber, J.M.; Thompson, C.A.; Sidney, P.G.; O’Brien, A.; Updegraff, J. Experimental Tests of How Hypothetical Monetary Lottery Incentives Influence Vaccine-Hesitant U.S. Adults’ Intentions to Vaccinate. PsyArXiv 2021. [Google Scholar] [CrossRef]
- Han, P.K.J.; Scharnetzki, E.; Scherer, A.M.; Thorpe, A.; Lary, C.; Waterston, L.B.; Fagerlin, A.; Dieckmann, N.F. Communicating Scientific Uncertainty About the COVID-19 Pandemic: Online Experimental Study of an Uncertainty-Normalizing Strategy. J. Med. Internet Res. 2021, 23, e27832. [Google Scholar] [CrossRef] [PubMed]
- Batteux, E.; Bilovich, A.; Johnson, S.G.B.; Tuckett, D. The negative consequences of failing to communicate uncertainties during a pandemic: The case of COVID-19 vaccines. medRxiv 2021. [Google Scholar] [CrossRef]
- McPhedran, R.; Gold, N.; Bemand, C.; Weston, D.; Rosen, R.; Scott, R.; Chadborn, T.; Amlôt, R.; McMaster, T.; Kume-Holland, C.; et al. Location, location, location: A discrete choice experiment to inform vaccination programme delivery in the UK. Res. Sq. 2021. [Google Scholar] [CrossRef]
- Pink, S.; Chu, J.; Druckman, J.; Rand, D.; Willer, R. Elite party cues increase vaccination intentions among Republicans. PsyArXiv 2021. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, T.; Nishina, Y.; Tomoi, H.; Harada, K.; Tanaka, K.; Matsumoto, E.; Horimukai, K.; Ishihara, J.; Sasaki, S.; Inaba, K.; et al. Corowa-kun: Impact of a COVID-19 vaccine information chatbot on vaccine hesitancy, Japan 2021. medRxiv 2021. [Google Scholar] [CrossRef]
- Witus, L.S.; Larson, E. A randomized controlled trial of a video intervention shows evidence of increasing COVID-19 vaccination intention. medRxiv 2021. [Google Scholar] [CrossRef]
- Bateman, J.; Cox, N.; Rajagopala, L.; Ford, M.; Jasim, M.; Mulherin, D.; Venkatachalam, S.; Douglas, B.; Hirsch, G.; Sheeran, T. COVID-19 vaccination advice via SMS-based video to improve vaccination uncertainty in at-risk groups. Lancet Rheumatol. 2021, 3, e399–e401. [Google Scholar] [CrossRef]
- Sprengholz, P.; Betsch, C.; Böhm, R. Reactance revisited: Consequences of mandatory and scarce vaccination in the case of COVID-19. Appl. Psychol. Health Well-Being 2021, 13, 986–995. [Google Scholar] [CrossRef]
- Schmelz, K.; Bowles, S. Overcoming COVID-19 vaccination resistance when alternative policies affect the dynamics of conformism, social norms, and crowding out. Proc. Natl. Acad. Sci. USA 2021, 118, e2104912118. [Google Scholar] [CrossRef]
- Dennis, A.; Robin, C.; Jones, L.; Carter, H. Exploring Vaccine Hesitancy in Care Home Employees in North West England: A Qualitative Study. medRxiv 2021. [Google Scholar] [CrossRef]
- Serra-Garcia, M.; Szech, N. Choice Architecture and Incentives Increase COVID-19 Vaccine Intentions and Test Demand; Contract No.: 9003. Available online: https://econpapers.wiwi.kit.edu/downloads/KITe_WP_150.pdf (accessed on 28 September 2021).
- Sprengholz, P.; Henkel, L.; Betsch, C. Payments and freedoms: Effects of monetary and legal incentives on COVID-19 vaccination intentions in Germany. PsyArXiv 2021. [Google Scholar] [CrossRef]
- Thirumurthy, H.; Milkman, K.L.; Volpp, K.; Buttenheim, A.; Pope, D.G. Association Between Statewide Financial Incentive Programs and COVID-19 Vaccination Rates. SSRN 2021. [Google Scholar] [CrossRef]
- Walkey, A.J.; Law, A.; Bosch, N.A. Lottery-Based Incentive in Ohio and COVID-19 Vaccination Rates. JAMA 2021, 326, 766–767. [Google Scholar] [CrossRef] [PubMed]
- Barber, A.; West, J. Conditional Cash Lotteries Increase COVID-19 Vaccination Rates. J. Health Econ. 2021, 81, 102578. [Google Scholar] [CrossRef]
- Behavioural Insights Team. Practicalities Are the Most Significant Impediments to People Getting a COVID Vaccine—And the Easiest to Address 2021. Available online: https://www.bi.team/blogs/practicalities-are-the-most-significant-impediments-to-people-getting-a-covid-vaccine-and-the-easiest-to-address/ (accessed on 20 September 2021).
- Sheeran, P.; Webb, T.L. The Intention–Behavior Gap. Soc. Personal. Psychol. Compass 2016, 10, 503–518. [Google Scholar] [CrossRef]
- Yamin, P.; Fei, M.; Lahlou, S.; Levy, S. Using Social Norms to Change Behavior and Increase Sustainability in the Real World: A Systematic Review of the Literature. Sustainability 2019, 11, 5847. [Google Scholar] [CrossRef] [Green Version]
- Neville, F.G.; Templeton, A.; Smith, J.R.; Louis, W.R. Social norms, social identities and the COVID-19 pandemic: Theory and recommendations. Soc. Personal. Psychol. Compass 2021, 15, e12596. [Google Scholar] [CrossRef]
- O’Keefe, D.J.; Nan, X. The Relative Persuasiveness of Gain- and Loss-Framed Messages for Promoting Vaccination: A Meta-Analytic Review. Health Commun. 2012, 27, 776–783. [Google Scholar] [CrossRef]
- Hoffrage, U.; Gigerenzer, G. Using natural frequencies to improve diagnostic inferences. Acad. Med. 1998, 73, 538–540. [Google Scholar] [CrossRef]
- Weber, P.; Binder, K.; Krauss, S. Why Can Only 24% Solve Bayesian Reasoning Problems in Natural Frequencies: Frequency Phobia in Spite of Probability Blindness. Front. Psychol. 2018, 9, 1833. [Google Scholar] [CrossRef]
- The British Psychological Society. Delivering Effective Public Health Campaigns during COVID-19 2020. Available online: https://www.bps.org.uk/sites/www.bps.org.uk/files/Policy/Policy%20-%20Files/Delivering%20effective%20public%20health%20campaigns%20during%20Covid-19.pdf (accessed on 21 February 2022).
- Lawes-Wickwar, S.; Ghio, D.; Tang, M.Y.; Keyworth, C.; Stanescu, S.; Westbrook, J.; Jenkinson, E.; Kassianos, A.P.; Scanlan, D.; Garnett, N.; et al. A Rapid Systematic Review of Public Responses to Health Messages Encouraging Vaccination against Infectious Diseases in a Pandemic or Epidemic. Vaccines 2021, 9, 72. [Google Scholar] [CrossRef] [PubMed]
- Economic and Social Research Council, University of Sussex, University of St Andrews, Canterbury Christ Church University. Evidence-Based Guidance on COVID Communications: Seven Core Principles. Available online: https://www.sussex.ac.uk/webteam/gateway/file.php?name=evidence-based-guidance.pdf&site=629 (accessed on 11 October 2021).
- Milkman, K.L.; Patel, M.S.; Gandhi, L.; Graci, H.N.; Gromet, D.M.; Ho, H.; Kay, J.S.; Lee, T.W.; Akinola, M.; Beshears, J.; et al. A megastudy of text-based nudges encouraging patients to get vaccinated at an upcoming doctor’s appointment. Proc. Natl. Acad. Sci. USA 2021, 118, e2101165118. [Google Scholar] [CrossRef] [PubMed]
- Betsch, C.; Böhm, R. Detrimental effects of introducing partial compulsory vaccination: Experimental evidence. Eur. J. Public Health 2015, 26, 378–381. [Google Scholar] [CrossRef] [Green Version]
- Currenti, R.; Flatley, J. Policing the Pandemic: Detailed Analysis on Police Enforcement of the Public Health Regulations and an Assessment on Disproportionality across Ethnic Groups 2021. Available online: https://www.northyorkshire-pfcc.gov.uk/content/uploads/2020/07/Policing-the-Pandemic-NPCC.pdf (accessed on 11 October 2021).
- Drury, J.; Mao, G.; John, A.; Kamal, A.; Rubin, G.J.; Stott, C.; Vandrevala, T.; Marteau, T.M. Behavioural responses to COVID-19 health certification: A rapid review. BMC Public Health 2021, 21, 1205. [Google Scholar] [CrossRef]
- de Figueiredo, A.; Larson, H.J.; Reicher, S. The potential impact of vaccine passports on inclination to accept COVID-19 vaccinations in the United Kingdom: Evidence from a large cross-sectional survey and modelling study. EClinicalMedicine 2021. [Google Scholar] [CrossRef] [PubMed]
- Largent, E.A.; Miller, F.G. Problems With Paying People to Be Vaccinated Against COVID-19. JAMA 2021, 325, 534–535. [Google Scholar] [CrossRef] [PubMed]
- Healthwatch. Getting to Vaccine Centres more of a Barrier for Black Communities 2021. Available online: https://www.healthwatch.co.uk/news/2021-02-22/getting-vaccine-centres-more-barrier-black-communities (accessed on 11 October 2021).
- Local Government Association. Wiltshire Council: Promoting Vaccination among Traveller and Houseboat Communities. Available online: https://www.local.gov.uk/case-studies/wiltshire-council-promoting-vaccination-among-traveller-and-houseboat-communities (accessed on 11 October 2021).
- Office for National Statistics. Coronavirus and Changing Attitudes towards Vaccination, England: 7 to 16 September 2021. Available online: https://www.ons.gov.uk/Peoplepopulationandcommunity/healthandsocialcare/healthandwellbeing/bulletins/coronavirusandchangingattitudestowardsvaccinationengland/7to16september2021#attitudes-towards-covid-19-booster-vaccines (accessed on 21 February 2022).
- Bish, A.; Yardley, L.; Nicoll, A.; Michie, S. Factors associated with uptake of vaccination against pandemic influenza: A systematic review. Vaccine 2011, 29, 6472–6484. [Google Scholar] [CrossRef]
- Schmid, P.; Rauber, D.; Betsch, C.; Lidolt, G.; Denker, M.-L. Barriers of Influenza Vaccination Intention and Behavior—A Systematic Review of Influenza Vaccine Hesitancy, 2005–2016. PLoS ONE 2017, 12, e0170550. [Google Scholar] [CrossRef]
- Office for National Statistics. Coronavirus (COVID-19) Latest Insights: Vaccines 2022. Available online: https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/articles/coronaviruscovid19latestinsights/vaccines (accessed on 15 February 2022).
- Lai, X.; Zhu, H.; Wang, J.; Huang, Y.; Jing, R.; Lyu, Y.; Zhang, H.; Feng, H.; Guo, J.; Fang, H. Public Perceptions and Acceptance of COVID-19 Booster Vaccination in China: A Cross-Sectional Study. Vaccines 2021, 9, 1461. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).