Antioxidant and Anti-Inflammatory Effects of Curcumin Nanoparticles on Drug-Induced Acute Myocardial Infarction in Diabetic Rats
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethics Statement
2.2. Chemicals and Drugs
2.3. Animals
2.4. Experimental Protocol
2.4.1. Groups of Study
2.4.2. Induction of Diabetes Mellitus
2.4.3. Induction of Acute Myocardial Infarction
2.4.4. Curcumin and Curcumin Nanoparticles Administration
2.5. Biochemical Assays
2.6. Statistical Analysis
3. Results
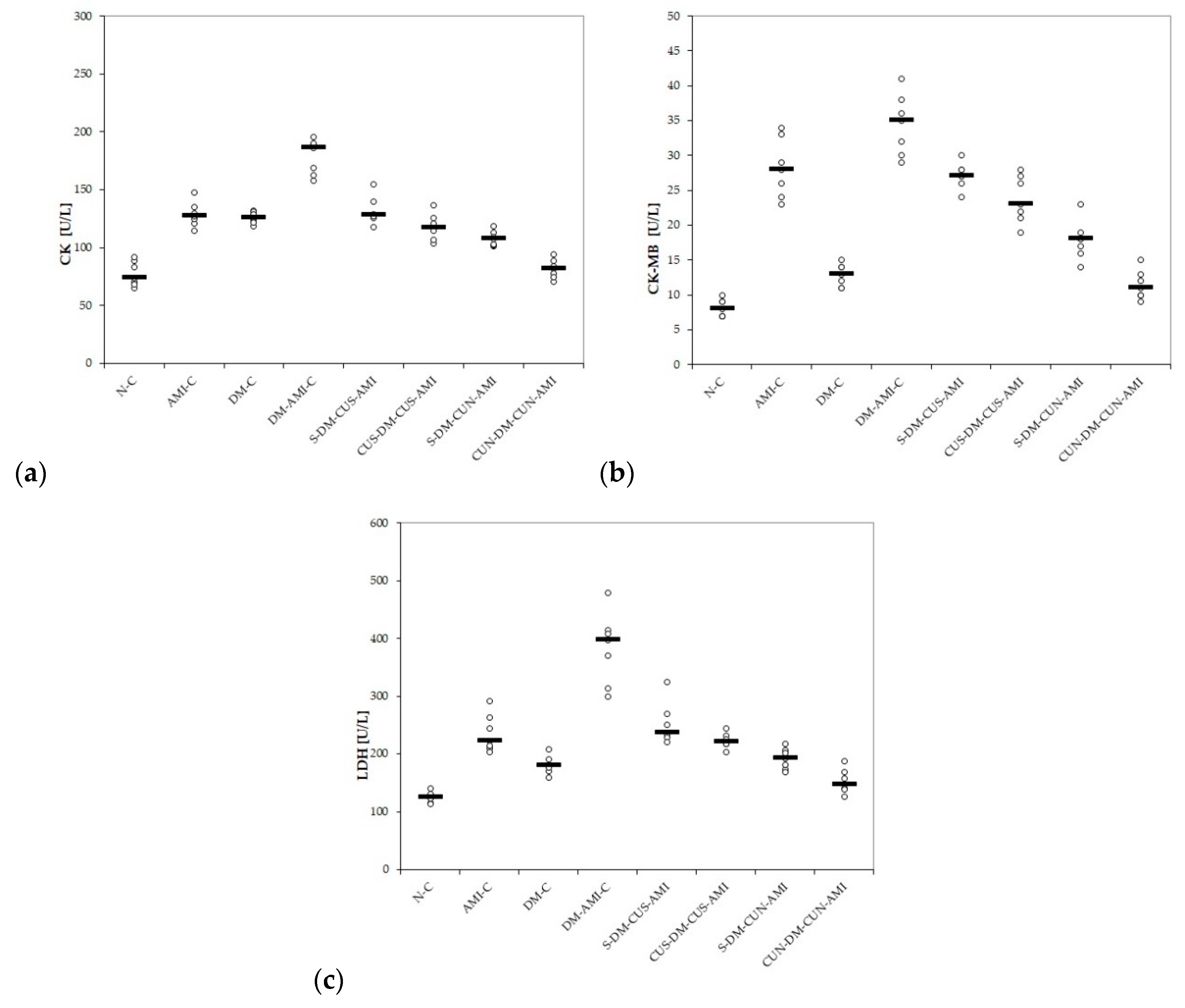
3.1. Serum Levels of Myocardial Infarction Enzymes
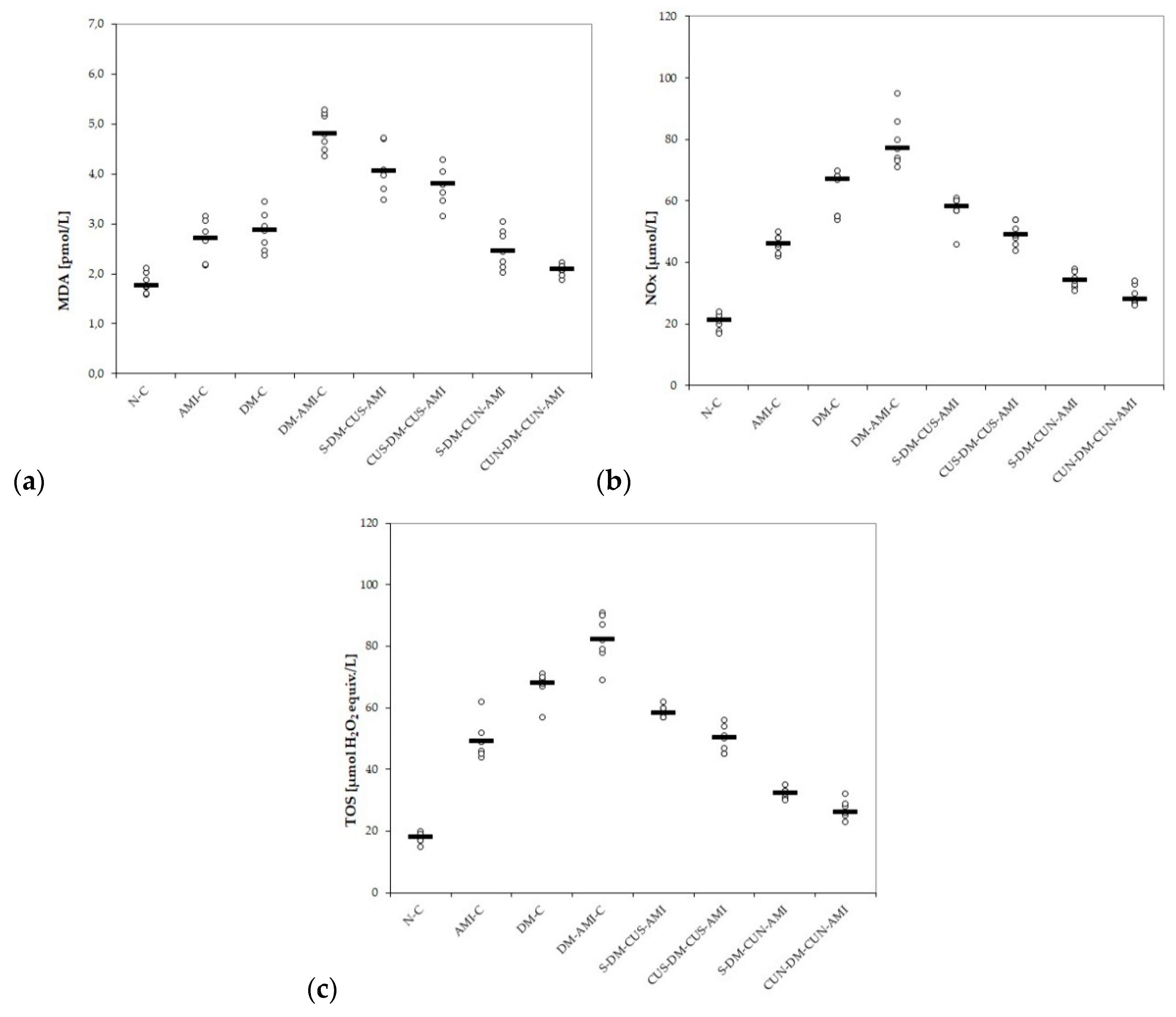
3.2. Serum Levels of Oxidative Stress Parameters
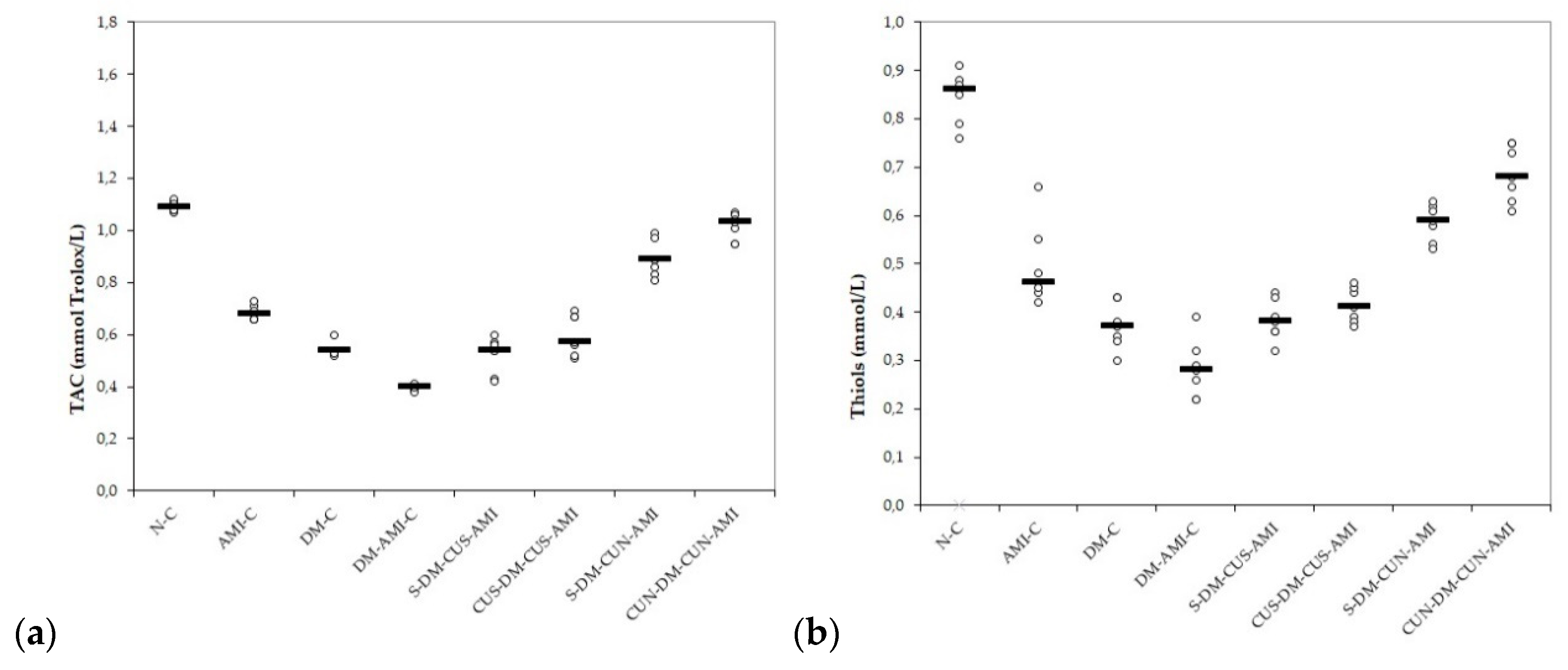
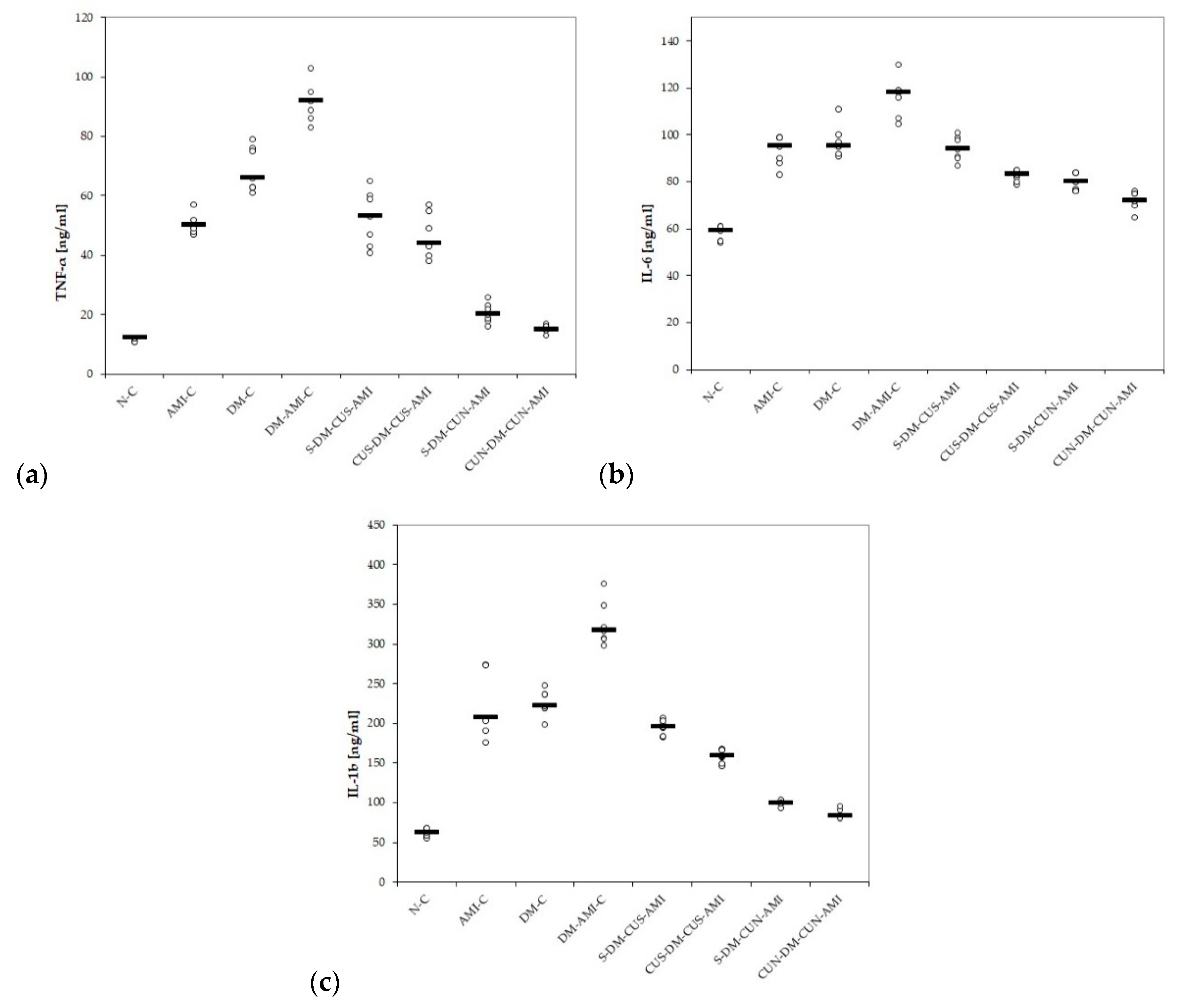
3.3. Serum Levels of Pro-Inflammatory Cytokines
4. Discussion
4.1. Myocardial Infarction Enzymes
4.2. Oxidative Stress Parameters
4.3. Pro-Inflammatory Cytokines
4.4. Potential Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Data Availability
References
- Zhang, D.W.; Fu, M.; Gao, S.H.; Liu, J.L. Curcumin and diabetes, a systematic review. Evid.-Based Complement. Alternat. Med. 2013, 2013, 636053. [Google Scholar] [CrossRef]
- Tripathi, B.K.; Srivastava, A.K. Diabetes mellitus, Complications and therapeutics. Med. Sci. Monit. 2006, 12, 130–147. [Google Scholar]
- Chawla, A.; Chawla, R.; Jaggi, S. Microvasular and macrovascular complications in diabetes mellitus, distinct or continuum? Indian J. Endocrinol. Metab. 2016, 20, 546–551. [Google Scholar] [CrossRef] [PubMed]
- Wei, H.; Li, H.; Wan, S.P.; Zeng, Q.T.; Cheng, L.X.; Jiang, L.L.; Peng, Y.D. Cardioprotective effects of malvidin against isoproterenol–induced myocardial infarction in rats: A mechanistic study. Med. Sci. Monit. 2017, 23, 2007–2016. [Google Scholar] [CrossRef] [PubMed]
- Strain, W.D.; Smith, C. Cardiovascular outcome studies in diabetes: How do we make sense of these new data? Diabetes Ther. 2016, 7, 175–185. [Google Scholar] [CrossRef] [PubMed]
- El Agaty, S.M. Cardioprotective effect of vitamin D2 on isoproterenol-induced myocardial infarction in diabetic rats. Arch. Physiol. Biochem. 2019, 125, 210–219. [Google Scholar] [CrossRef] [PubMed]
- Bulboacă, A.E.; Porfire, A.S.; Tefas, L.R.; Boarescu, P.M.; Bolboacă, S.D.; Stănescu, I.C.; Bulboacă, A.C.; Dogaru, G. Liposomal curcumin is better than curcumin to alleviate complications in experimental diabetic mellitus. Molecules 2019, 24, 846. [Google Scholar] [CrossRef]
- Szkudelski, T. The mechanism of alloxan and streptozotocin action in B cells of the rat pancreas. Physiol. Res. 2001, 50, 537–546. [Google Scholar]
- Al Nahdi, A.M.; John, A.; Raza, H. Elucidation of molecular mechanisms of streptozotocin–induced oxidative stress, apoptosis, and mitochondrial dysfunction in Rin–5F pancreatic β-cells. Oxid. Med. Cell. Longev. 2017, 2017, 7054272. [Google Scholar] [CrossRef]
- Karlsson, F.A.; Berne, C.; Björk, E.; Kullin, M.; Li, Z.; Ma, J.Y.; Schölin, A.; Zhao, L. Beta-cell activity and destruction in type 1 diabetes. Ups. J. Med. Sci. 2000, 105, 85–95. [Google Scholar] [CrossRef]
- Huang, H.; Geng, Q.; Yao, H.; Shen, Z.; Wu, Z.; Miao, X.; Shi, P. Protective effect of scutellarin on myocardial infarction induced by isoprenaline in rats. Iran. J. Basic Med. Sci. 2018, 21, 267–276. [Google Scholar]
- Agrawal, Y.O.; Sharma, P.K.; Shrivastava, B.; Arya, D.S.; Goyal, S.N. Hesperidin blunts streptozotocin-isoproternol induced myocardial toxicity in rats by altering of PPAR-gamma receptor. Chem.-Biol. Interact. 2014, 219, 211–220. [Google Scholar] [CrossRef] [PubMed]
- Boarescu, P.M.; Chirilă, I.; Bulboacă, A.E.; Bocșan, I.C.; Pop, R.M.; Gheban, D.; Bolboacă, S.D. Effects of curcumin nanoparticles in isoproterenol-induced myocardial infarction. Oxid. Med. Cell. Longev. 2019, 2019, 7847142. [Google Scholar] [CrossRef] [PubMed]
- Boarescu, P.-M.; Boarescu, I.; Bocșan, I.C.; Pop, R.M.; Gheban, D.; Bulboacă, A.E.; Nicula, C.; Râjnoveanu, R.-M.; Bolboacă, S.D. Curcumin Nanoparticles Protect against Isoproterenol Induced Myocardial Infarction by Alleviating Myocardial Tissue Oxidative Stress, Electrocardiogram, and Biological Changes. Molecules 2019, 24, 2802. [Google Scholar] [CrossRef]
- Boarescu, P.M.; Boarescu, I.; Bocșan, I.C.; Pop, R.M.; Gheban, D.; Bulboacă, A.E.; Dogaru, G.; Bolboacă, S.D. Experimental model of acute myocardial infarction for evaluation of prevention and rehabilitation strategies in cardiovascular diseases—A pilot study. Balneo Res. J. 2019, 10, 288–293. [Google Scholar] [CrossRef]
- Dogaru, G.; Bulboaca, A.; Stanescu, I.; Rus, V.; Bodizs, G.; Ciumarnean, L.; Munteanu, C.; Boarescu, P.M.; Neagos, A.; Festila, D. The effect of carbonated natural mineral water on oxidative stress in experimental myocardial ischemia. Revista de Chimie 2019, 70, 2677–2680. [Google Scholar]
- Lubrano, V.; Pingitore, A.; Traghella, I.; Storti, S.; Parri, S.; Berti, S.; Ndreu, R.; Andrenelli, A.; Palmieri, C.; Iervasi, G.; et al. Emerging Biomarkers of Oxidative Stress in Acute and Stable Coronary Artery Disease: Levels and Determinants. Antioxidants 2019, 8, 115. [Google Scholar] [CrossRef]
- Goel, A.; Kunnumakkara, A.B.; Aggarwal, B.B. Curcumin as “Curecumin”: From kitchen to clinic. Biochem. Pharmacol. 2008, 75, 787–809. [Google Scholar] [CrossRef]
- Goel, A.; Jhurani, S.; Aggarwal, B.B. Multi-targeted therapy by curcumin: How spicy is it? Mol. Nutr. Food Res. 2008, 52, 1010–1030. [Google Scholar] [CrossRef]
- Hatcher, H.; Planalp, R.; Cho, J.; Torti, F.M.; Torti, S.V. Curcumin: From ancient medicine to current clinical trials. Cell. Mol. Life Sci. 2008, 65, 1631–1652. [Google Scholar] [CrossRef]
- Wang, N.P.; Wang, Z.F.; Tootle, S.; Philip, T.; Zhao, Z.Q. Curcumin promotes cardiac repair and ameliorates cardiac dysfunction following myocardial infarction. Br. J. Pharmacol. 2012, 167, 1550–1562. [Google Scholar] [CrossRef] [PubMed]
- Rahnavard, M.; Hassanpour, M.; Ahmadi, M.; Heidarzadeh, M.; Amini, H.; Javanmard, M.Z.; Nouri, M.; Rahbarghazi, R.; Safaie, N. Curcumin ameliorated myocardial infarction by inhibition of cardiotoxicity in the rat model. J. Cell. Biochem. 2019, 120, 11965–11972. [Google Scholar] [CrossRef] [PubMed]
- Sasaki, H.; Sunagawa, Y.; Takahashi, K.; Imaizumi, A.; Fukuda, H.; Hashimoto, T.; Wada, H.; Katanasaka, Y.; Kakeya, H.; Fujita, M.; et al. Innovative preparation of curcumin for improved oral bioavailability. Biol. Pharm. Bull. 2011, 34, 660–665. [Google Scholar] [CrossRef] [PubMed]
- Anand, P.; Kunnumakkara, A.B.; Newman, R.A.; Aggarwal, B.B. Bioavailability of curcumin: Problems and promises. Mol. Pharm. 2007, 4, 807–818. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Dai, W.T.; He, Z.M.; Gao, L.; Huang, X.; Gong, J.M.; Xing, H.Y.; Chen, W.D. Fabrication and evaluation of curcumin-loaded nanoparticles based on solid lipid as a new type of colloidal drug delivery system. Indian J. Pharm. Sci. 2013, 75, 178–184. [Google Scholar]
- Prasad, S.; Tyagi, A.K.; Aggarwal, B.B. Recent developments in delivery, bioavailability, absorption and metabolism of curcumin: The golden pigment from golden spice. Cancer Res. Treat. 2014, 46, 2–8. [Google Scholar] [CrossRef]
- Silva-Buzanello, R.A.; Souza, M.F.; Oliveira, D.A.; Bona, E.; Leimann, F.V.; Cardozo Filho, L.; de Araújo, P.H.H.; Ferreira, S.R.S.; Gonçalves, O.H. Preparation of curcumin-loaded nanoparticles and determination of the antioxidant potential of curcumin after encapsulation. Polímeros 2016, 26, 207–214. [Google Scholar] [CrossRef]
- Umerska, A.; Gaucher, C.; Oyarzun-Ampuero, F.; Fries-Raeth, I.; Colin, F.; Villamizar-Sarmiento, M.G.; Maincent, P.; Sapin-Minet, A. Polymeric Nanoparticles for Increasing Oral Bioavailability of Curcumin. Antioxidants 2018, 7, 46. [Google Scholar] [CrossRef]
- Bulboacă, A.; Bolboacă, S.D.; Suci, S. Protective effect of curcumin in fructose-induced metabolic syndrome and in streptozotocin-induced diabetes in rats. Iran. J. Basic Med. Sci. 2016, 19, 585–593. [Google Scholar]
- Panda, S.P.; Haldar, P.K.; Bera, S.; Adhikary, S.; Kandar, C.C. Antidiabetic and antioxidant activity of Swietenia mahagoni in streptozotocin-induced diabetic rats. Pharm. Biol. 2010, 48, 974–979. [Google Scholar] [CrossRef]
- Bhandari, U.; Ansari, M.N. Ameliorative effect of an ethanol extract of Embelia ribes fruits on isoproterenol-induced cardiotoxicity in diabetic rats. Pharm. Biol. 2009, 47, 669–674. [Google Scholar] [CrossRef][Green Version]
- Mitev, D.; Gradeva, H.; Stoyanova, Z.; Petrova, N.; Karova, N.; Dimov, D.; Iliev, V.; Koychev, A.; Prakova, G.; Vlaykova, T. Evaluation of thiol compounds and lipid peroxidative products in plasma of patients with COPD. TJS 2010, 8, 306–314. [Google Scholar]
- Miranda, K.M.; Espey, M.G.; Wink, D.A. A rapid, simple spectrophotometric method for simultaneous detection of nitrate and nitrite. Nitric Oxide 2001, 5, 62–71. [Google Scholar] [CrossRef] [PubMed]
- Erel, O. A new automated colorimetric method for measuring total oxidant status. Clin. Biochem. 2005, 38, 1103–1111. [Google Scholar] [CrossRef]
- Erel, O. A novel automated method to measure total antioxidant response against potent free radical reactions. Clin. Biochem. 2004, 37, 112–119. [Google Scholar] [CrossRef]
- Hu, M.L. [41] Measurement of protein thiol groups and glutathione in plasma. Methods Enzymol. 1994, 233, 380–385. [Google Scholar]
- Weissgerber, T.L.; Milic, N.M.; Winham, S.J.; Garovic, V.D. Beyond bar and line graphs: Time for a new data presentation paradigm. PLoS Biol. 2015, 13, e1002128. [Google Scholar] [CrossRef]
- Roy, S.; Mahmood, T.; Siddiqui, H.H.; Bagga, P.; Shamim, A. Effect of Terminalia Chebula (Harad) fruit extract on cardiotoxicity in streptozotocin induced diabetic rats. Int. J. Pharm. Pharm. Sci. 2015, 7, 304–309. [Google Scholar]
- Heinova, D.; Rosival, I.; Avidar, Y.; Bogin, E. Lactate dehydrogenase isoenzyme distribution and patterns in chicken organs. Res. Vet. Sci. 1999, 67, 309–312. [Google Scholar] [CrossRef]
- Aydin, S.; Ugur, K.; Aydin, S.; Sahin, İ.; Yardim, M. Biomarkers in acute myocardial infarction: Current perspectives. Vasc. Health Risk Manag. 2019, 15, 1. [Google Scholar] [CrossRef]
- Ingwall, J.S.; Kramer, M.F.; Fifer, M.A.; Lorell, B.H.; Shemin, R.; Grossman, W.; Allen, P.D. The creatine kinase system in normal and diseased human myocardium. N. Engl. J. Med. 1985, 313, 1050–1054. [Google Scholar] [CrossRef] [PubMed]
- Hawkins, R.C.; Tan, H.L. Comparison of the diagnostic utility of CK, CK-MB (activity and mass), troponin T and troponin I in patients with suspected acute myocardial infarction. Singap. Med. J. 1999, 40, 680–684. [Google Scholar]
- Balea, Ş.S.; Pârvu, A.E.; Pop, N.; Marín, F.Z.; Pârvu, M. Polyphenolic Compounds, Antioxidant, and Cardioprotective Effects of Pomace Extracts from Fetească Neagră Cultivar. Oxid. Med. Cell. Longev. 2018, 2018, 8194721. [Google Scholar] [CrossRef] [PubMed]
- Mythili, S.; Malathi, N. Diagnostic markers of acute myocardial infarction. Biomed. Rep. 2015, 3, 743–748. [Google Scholar] [CrossRef]
- Mostafa, M.E.A. Protective Effect of Curcumin Against Isoproterenol-Induced Myocardial Infarction in Adult Male Albino Rat. Egypt. J. Anat. 2011, 34, 15–29. [Google Scholar] [CrossRef]
- Yu, Y.P.; Huang, X.M.; Fu, Y.F. Curcumin protects H9c2 cardiomyocyte against ischemia/reperfusion injury through inactivation of glycogen synthase kinase-3. Int. J. Clin. Exp. Pathol. 2016, 9, 3226–3232. [Google Scholar]
- Nabofa, W.E.; Alashe, O.O.; Oyeyemi, O.T.; Attah, A.F.; Oyagbemi, A.A.; Omobowale, T.O.; Adedapo, A.A.; Alada, A.R. Cardioprotective Effects of Curcumin-Nisin Based Poly Lactic Acid Nanoparticle on Myocardial Infarction in Guinea Pigs. Sci. Rep. 2018, 8, 16649. [Google Scholar] [CrossRef] [PubMed]
- Samarghandian, S.; Azimi-Nezhad, M.; Farkhondeh, T. Crocin attenuate Tumor Necrosis Factor-alpha (TNF-α) and interleukin-6 (IL-6) in streptozotocin-induced diabetic rat aorta. Cytokine 2016, 88, 20–28. [Google Scholar] [CrossRef] [PubMed]
- Idris, I.; Gray, S.; Donnelly, R. Protein kinase C activation, isozyme–specific effects on metabolism and cardiovascular complications in diabetes. Diabetologia 2001, 44, 659–673. [Google Scholar] [CrossRef] [PubMed]
- Ito, F.; Sono, Y.; Ito, T. Measurement and clinical significance of lipid peroxidation as a biomarker of oxidative stress: Oxidative stress in diabetes, atherosclerosis, and chronic inflammation. Antioxidants 2019, 8, 72. [Google Scholar] [CrossRef]
- Kathyaini, R.; Gayatri, S.; Suleman, D. A study on malondialdehyde as an oxidative stress marker in patients with myocardial infarction at a tertiary care centre. NJLM 2017, 6, 3–16. [Google Scholar]
- Etsuo, N. Lipid peroxidation, Physiological levels and dual biological effects. Free Radic. Biol. Med. 2009, 47, 469–484. [Google Scholar]
- Kurian, G.A.; Rajagopal, R.; Vedantham, S.; Rajesh, M. The role of oxidative stress in myocardial ischemia and reperfusion injury and remodeling, revisited. Oxid. Med. Cell. Longev. 2016, 2016, 656450. [Google Scholar] [CrossRef]
- Ingaramo, P.I.; Ronco, M.T.; Frances, D.E.; Monti, J.A.; Pisani, G.B.; Ceballos, M.P.; Galleano, M.; Carrillo, M.C.; Carnovale, C.E. Tumor necrosis factor alpha pathways develops liver apoptosis in type 1 diabetes mellitus. Mol. Immunol. 2011, 48, 1397–1407. [Google Scholar] [CrossRef] [PubMed]
- Mohan, I.K.; Das, U.N. Oxidant stress, anti-oxidants and nitric oxide in non-insulin dependent diabetes mellitus. Med. Sci. Res. 1997, 25, 55–57. [Google Scholar]
- Yu, X.; Ge, L.; Niu, L.; Lian, X.; Ma, H.; Pang, L. The dual role of inducible nitric oxide synthase in myocardial ischemia/reperfusion injury: Friend or foe? Oxid. Med. Cell. Longev. 2018, 2018, 8364848. [Google Scholar] [CrossRef]
- Ziamajidi, N.; Nasiri, A.; Abbasalipourkabir, R.; Sadeghi Moheb, S. Effects of garlic extract on TNF-α expression and oxidative stress status in the kidneys of rats with STZ+ nicotinamide–induced diabetes. Pharm. Biol. 2017, 55, 526–531. [Google Scholar] [CrossRef]
- Ellidag, H.Y.; Eren, E.; Yılmaz, N.; Cekin, Y. Oxidative stress and ischemia–modified albumin in chronic ischemic heart failure. Redox Rep. 2014, 19, 118–123. [Google Scholar] [CrossRef]
- Bas, H.A.; Aksoy, F.; Icli, A.; Varol, E.; Dogan, A.; Erdogan, D.; Ersoy, I.; Arslan, A.; Ari, H.; Bas, N.; et al. The association of plasma oxidative status and inflammation with the development of atrial fibrillation in patients presenting with ST elevation myocardial infarction. Scand. J. Clin. Lab. Investig. 2017, 77, 77–82. [Google Scholar] [CrossRef]
- Zare–Mirzaie, A.; Kazeminezhad, B.; Ghouchani, M.A. The Correlation Between Serum Vitamin D Level and Total Antioxidant Capacity in diabetic and Non-diabetic Subjects in Iran. Iran. J. Pathol. 2018, 13, 212. [Google Scholar] [CrossRef]
- Sedláková, E.; Rácz, O.; Lovásová, E.; Beòaèka, R.; Kurpas, M.; Chmelárová, A.; Sedlák, J.; Studenèan, M. Markers of oxidative stress in acute myocardial infarction treated by percutaneous coronary intervention. Open Med. 2009, 4, 26–31. [Google Scholar] [CrossRef]
- Bulboacă, A.E.; Bolboacă, S.D.; Stănescu, I.C.; Sfrângeu, C.A.; Bulboacă, A.C. Preemptive analgesic and antioxidative effect of curcumin for experimental migraine. Biomed. Res. Int. 2017, 2017, 4754701. [Google Scholar] [CrossRef] [PubMed]
- Bulboacă, A.E.; Bolboacă, S.D.; Stănescu, I.C.; Sfrângeu, C.A.; Porfire, A.; Tefas, L.; Bulboacă, A.C. The effect of intravenous administration of liposomal curcumin in addition to sumatriptan treatment in an experimental migraine model in rats. Int. J. Nanomed. 2018, 13, 3093–3103. [Google Scholar] [CrossRef] [PubMed]
- Ates, I.; Kaplan, M.; Yuksel, M.; Mese, D.; Alisik, M.; Erel, Ö.; Yilmaz, N.; Guler, S. Determination of thiol/disulphide homeostasis in type 1 diabetes mellitus and the factors associated with thiol oxidation. Endocrine 2016, 51, 47–51. [Google Scholar] [CrossRef]
- Babu, S.; Shetty, J.K.; Mungli, P. Total thiols and MDA levels in patients with acute myocardial infarction before and after reperfusion therapy. OJHAS 2010, 9, 1–4. [Google Scholar]
- Borra, S.K.; Mahendra, J.; Gurumurthy, P. Effect of curcumin against oxidation of biomolecules by hydroxyl radicals. JCDR 2014, 8, CC01. [Google Scholar] [CrossRef]
- Mehta, J.; Rayalam, S.; Wang, X. Cytoprotective Effects of Natural Compounds against Oxidative Stress. Antioxidants 2018, 7, 147. [Google Scholar] [CrossRef]
- Kim, Y.S.; Park, H.J.; Joo, S.Y.; Hong, M.H.; Kim, K.H.; Hong, Y.J.; Kim, J.H.; Park, H.W.; Jeong, M.H.; Cho, J.G.; et al. The protective effect of curcumin on myocardial ischemia–reperfusion injury. Korean Circ. J. 2008, 38, 353–359. [Google Scholar] [CrossRef]
- Eser, A.; Hizli, D.; Haltas, H.; Namuslu, M.; Kosus, A.; Kosus, N.; Kafali, H. Effects of curcumin on ovarian ischemia–reperfusion injury in a rat model. Biomed. Rep. 2015, 3, 807–813. [Google Scholar] [CrossRef]
- Al–Rubaei, Z.M.; Mohammad, T.U.; Ali, L.K. Effects of local curcumin on oxidative stress and total antioxidant capacity in vivo study. Pak. J. Biol. Sci. 2014, 17, 1237–1241. [Google Scholar] [CrossRef]
- Edwards, R.L.; Luis, P.B.; Varuzza, P.V.; Joseph, A.I.; Presley, S.H.; Chaturvedi, R.; Schneider, C. The anti–inflammatory activity of curcumin is mediated by its oxidative metabolites. J. Biol. Chem. 2017, 292, 21243–21252. [Google Scholar] [CrossRef]
- Yu, H.; Li, J.; Shi, K.; Huang, Q. Structure of modified ε–polylysine micelles and their application in improving cellular antioxidant activity of curcuminoids. Food Funct. 2011, 2, 373–380. [Google Scholar] [CrossRef] [PubMed]
- Minnelli, C.; Moretti, P.; Fulgenzi, G.; Mariani, P.; Laudadio, E.; Armeni, T.; Galeazzi, R.; Mobbili, G. A poloxamer-407 modified liposome encapsulating epigallocatechin-3-gallate in the presence of magnesium: Characterization and protective effect against oxidative damage. Int. J. Pharm. 2018, 552, 225–234. [Google Scholar] [CrossRef]
- Peiró, C.; Lorenzo, Ó.; Carraro, R.; Sánchez-Ferrer, C.F. IL-1β inhibition in cardiovascular complications associated to diabetes mellitus. Front. Pharmacol. 2017, 8, 363. [Google Scholar] [CrossRef]
- Dokumacioglu, E.; Iskender, H.; Sen, T.M.; Ince, I.; Dokumacioglu, A.; Kanbay, Y.; Erbas, E.; Saral, S. The effects of hesperidin and quercetin on serum tumor necrosis factor-alpha and interleukin-6 levels in streptozotocin–induced diabetes model. Pharmacogn. Mag. 2018, 14, 167–173. [Google Scholar]
- Tekula, S.; Khurana, A.; Anchi, P.; Godugu, C. Withaferin—A attenuates multiple low doses of Streptozotocin (MLD-STZ) induced type 1 diabetes. Biomed. Pharmacother. 2018, 106, 1428–1440. [Google Scholar] [CrossRef]
- Tian, M.; Yuan, Y.C.; Li, J.Y.; Gionfriddo, M.R.; Huang, R.C. Tumor necrosis factor-α and its role as a mediator in myocardial infarction: A brief review. Chronic. Dis. Transl. Med. 2015, 1, 18–26. [Google Scholar] [CrossRef]
- Puhakka, M.; Magga, J.; Hietakorpi, S.; Penttilä, I.; Uusimaa, P.; Risteli, J.; Peuhkurinen, K. Interleukin-6 and tumor necrosis factor alpha in relation to myocardial infarct size and collagen formation. J. Card. Fail. 2003, 9, 325–332. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Zhang, Q.; Liao, Y.H.; Cao, Z.; Du, Y.M.; Xia, J.D.; Yang, H.; Chen, Z.J. Effect of tumor necrosis factor–α on neutralization of ventricular fibrillation in rats with acute myocardial infarction. Mediat. Inflamm. 2011, 2011, 565238. [Google Scholar] [CrossRef] [PubMed]
- Ritschel, V.N.; Seljeflot, I.; Arnesen, H.; Halvorsen, S.; Weiss, T.; Eritsland, J.; Andersen, G.Ø. IL-6 signalling in patients with acute ST-elevation myocardial infarction. Results Immunol. 2014, 4, 8–13. [Google Scholar] [CrossRef] [PubMed]
- Pomerantz, B.J.; Reznikov, L.L.; Harken, A.H.; Dinarello, C.A. Inhibition of caspase 1 reduces human myocardial ischemic dysfunction via inhibition of IL-18 and IL-1. Proc. Natl. Acad. Sci. USA 2001, 98, 2871–2876. [Google Scholar] [CrossRef] [PubMed]
| Day | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 7 (i.p.) | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | 21 | 22 | 22 (s.c.) | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Group | |||||||||||||||||||||||||
| N-C | saline by gavage | CB | saline by gavage | SS | |||||||||||||||||||||
| AMI-C | CB | ISO | |||||||||||||||||||||||
| DM-C | STZ | SS | |||||||||||||||||||||||
| DM-AMI-C | STZ | ISO | |||||||||||||||||||||||
| S-DM-CUS-AMI | STZ | CUS by gavage | ISO | ||||||||||||||||||||||
| CUS-DM-CUS-AMI | CUS by gavage | STZ | ISO | ||||||||||||||||||||||
| S-DM-CUN-AMI | saline by gavage | STZ | CUN by gavage | ISO | |||||||||||||||||||||
| CUN-DM-CUN-AMI | CUN by gavage | STZ | ISO | ||||||||||||||||||||||
| Rat No. | N-C | AMI-C | DM-C | DM-AMI-C | S-DM-CUS-AMI | CUS-DM-CUS-AMI | S-DM-CUN-AMI | CUN-DM-CUN-AMI |
|---|---|---|---|---|---|---|---|---|
| 1 | 80 | 76 | 544 | 549 | 497 | 419 | 389 | 375 |
| 2 | 75 | 78 | 532 | 498 | 462 | 452 | 362 | 366 |
| 3 | 69 | 79 | 559 | 534 | 526 | 432 | 435 | 324 |
| 4 | 81 | 82 | 562 | 504 | 432 | 417 | 441 | 272 |
| 5 | 82 | 74 | 468 | 518 | 478 | 432 | 360 | 389 |
| 6 | 78 | 75 | 563 | 569 | 508 | 447 | 380 | 262 |
| 7 | 74 | 86 | 434 | 479 | 458 | 440 | 429 | 288 |
| Group Abbreviation | CK (U/L) | CK-MB (U/L) | LDH (U/L) |
|---|---|---|---|
| N-C | 77.43 (10.6) | 8.14 (1.21) | 124.57 (9.48) |
| AMI-C | 128.71 (10.63) | 28.14 (4.22) | 235.86 (32.43) |
| DM-C | 126.14 (4.81) | 12.86 (1.57) | 180.57 (15.46) |
| DM-AMI-C | 178.71 (15.03) | 34.43 (4.35) | 383.43 (61.77) |
| S-DM-CUS-AMI | 131.86 (12.08) | 27.14 (1.86) | 252.00 (36.07) |
| CUS-DM-CUS-AMI | 118.14 (11.26) | 23.71 (3.35) | 222.86 (13.02) |
| S-DM-CUN-AMI | 107.86 (6.54) | 17.86 (2.79) | 191.71 (18.13) |
| CUN-DM-CUN-AMI | 81.86 (7.99) | 11.43 (2.07) | 152.00 (20.84) |
| Group Abbreviation | CK (U/L) | CK-MB (U/L) | LDH (U/L) |
|---|---|---|---|
| S-DM-CUS-AMI vs. | |||
| AMI-C | 0.6544 | 0.7968 | 0.3067 |
| DM-C | 0.5220 | 0.0021 | 0.0022 |
| DM-AMI-C | 0.0022 | 0.0039 | 0.0049 |
| CUS-DM-CUS-AMI vs. | |||
| AMI-C | 0.1244 | 0.0630 | 0.7491 |
| DM-C | 0.1098 | 0.0021 | 0.0033 |
| DM-AMI-C | 0.0022 | 0.0022 | 0.0022 |
| S-DM-CUS-AMI | 0.0348 | 0.0613 | 0.0409 |
| S-DM-CUN-AMI vs. | |||
| AMI-C | 0.0033 | 0.0026 | 0.0106 |
| DM-C | 0.0026 | 0.0047 | 0.3067 |
| DM-AMI-C | 0.0022 | 0.0021 | 0.0022 |
| S-DM-CUS-AMI | 0.0033 | 0.0021 | 0.0022 |
| CUN-DM-CUN-AMI vs. | |||
| AMI-C | 0.0022 | 0.0021 | 0.0022 |
| DM-C | 0.0022 | 0.1754 | 0.0215 |
| DM-AMI-C | 0.0022 | 0.0021 | 0.0022 |
| CUS-DM-CUS-AMI | 0.0022 | 0.0021 | 0.0022 |
| S-DM-CUN-AMI | 0.0022 | 0.0032 | 0.0073 |
| Group Abbreviation | MDA (nmol/L) | NOx (μmol/L) | TOS (μmol H2O2 equiv./L) |
|---|---|---|---|
| N-C | 1.82 (0.20) | 20.86 (2.67) | 17.71 (1.60) |
| AMI-C | 2.69 (0.39) | 46.00 (2.89) | 49.57 (6.13) |
| DM-C | 2.84 (0.39) | 62.43 (7.32) | 67.14 (4.67) |
| DM-AMI-C | 4.85 (0.37) | 79.43 (8.50) | 82.29 (7.78) |
| S-DM-CUS-AMI | 4.10 (0.47) | 57.00 (5.10) | 58.86 (1.86) |
| CUS-DM-CUS-AMI | 3.74 (0.37) | 49.43 (3.82) | 49.71 (4.31) |
| S-DM-CUN-AMI | 2.50 (0.39) | 34.29 (2.56) | 32.14 (1.68) |
| CUN-DM-CUN-AMI | 2.08 (0.11) | 29.43 (3.05) | 27.00 (2.94) |
| MDA (nmol/L) | NOx (μmol/L) | TOS (μmol H2O2 equiv./L) | TAC (mmol Trolox/L) | Thiols (mmol/L) | |
|---|---|---|---|---|---|
| S-DM-CUS-AMI vs. | |||||
| AMI-C | 0.0022 | 0.0085 | 0.0245 | 0.0020 | 0.0059 |
| DM-C | 0.0022 | 0.4413 | 0.0205 | 0.7433 | 0.5627 |
| DM-AMI-C | 0.0215 | 0.0021 | 0.0021 | 0.0020 | 0.0147 |
| CUS-DM-CUS-AMI vs. | |||||
| AMI-C | 0.0026 | 0.1079 | 0.6999 | 0.0825 | 0.0344 |
| DM-C | 0.0049 | 0.0031 | 0.0021 | 0.2737 | 0.0727 |
| DM-AMI-C | 0.0022 | 0.0021 | 0.0021 | 0.0020 | 0.0059 |
| S-DM-CUS-AMI | 0.1792 | 0.0176 | 0.0021 | 0.1994 | 0.1400 |
| S-DM-CUN-AMI vs. | |||||
| AMI-C | 0.4433 | 0.0021 | 0.0021 | 0.0020 | 0.0553 |
| DM-C | 0.1252 | 0.0021 | 0.0021 | 0.0020 | 0.0021 |
| DM-AMI-C | 0.0022 | 0.0022 | 0.0021 | 0.0020 | 0.0021 |
| S-DM-CUS-AMI | 0.0022 | 0.0021 | 0.0020 | 0.0021 | 0.0021 |
| CUN-DM-CUN-AMI vs. | |||||
| AMI-C | 0.0049 | 0.0021 | 0.0021 | 0.0020 | 0.0059 |
| DM-C | 0.0021 | 0.0021 | 0.0021 | 0.0020 | 0.0021 |
| DM-AMI-C | 0.0021 | 0.0021 | 0.0021 | 0.0020 | 0.0021 |
| CUS-DM-CUS-AMI | 0.0021 | 0.0021 | 0.0021 | 0.0021 | 0.0021 |
| S-DM-CUN-AMI | 0.0407 | 0.0210 | 0.0085 | 0.0104 | 0.0071 |
| Group Abbreviation | TAC (mmol Trolox/L) | Thiols (mmol/L) |
|---|---|---|
| N-C | 1.09 (0.02) | 0.85 (0.05) |
| AMI-C | 0.68 (0.03) | 0.49 (0.08) |
| DM-C | 0.54 (0.03) | 0.37 (0.05) |
| DM-AMI-C | 0.40 (0.01) | 0.28 (0.06) |
| S-DM-CUS-AMI | 0.52 (0.07) | 0.38 (0.04) |
| CUS-DM-CUS-AMI | 0.60 (0.08) | 0.41 (0.04) |
| S-DM-CUN-AMI | 0.89 (0.07) | 0.59 (0.04) |
| CUN-DM-CUN-AMI | 1.02 (0.05) | 0.69 (0.06) |
| Group Abbreviation | TNF-α (pg/mL) | IL-6 (pg/mL) | IL-1β (pg/mL) |
|---|---|---|---|
| N-C | 11.71 (0.49) | 58.00 (3.21) | 62.00 (5.00) |
| AMI-C | 50.43 (3.31) | 93.29 (6.40) | 218.71 (39.98) |
| DM-C | 69.00 (7.42) | 97.29 (6.75) | 225.43 (15.99) |
| DM-AMI-C | 91.43 (6.50) | 116.29 (8.36) | 325.00 (27.80) |
| S-DM-CUS-AMI | 52.57 (9.20) | 94.29 (5.22) | 194.86 (9.26) |
| CUS-DM-CUS-AMI | 46.57 (7.32) | 82.43 (2.30) | 157.86 (8.11) |
| S-DM-CUN-AMI | 20.57 (3.36) | 79.57 (3.46) | 99.29 (3.30) |
| CUN-DM-CUN-AMI | 15.29 (1.25) | 72.14 (3.80) | 85.14 (5.64) |
| TNF-α (pg/mL) | IL-6 (pg/mL) | IL-1β (pg/mL) | |
|---|---|---|---|
| S-DM-CUS-AMI vs. | |||
| AMI-C | 0.7489 | 0.8971 | 0.2222 |
| DM-C | 0.0072 | 0.4812 | 0.0058 |
| DM-AMI-C | 0.0021 | 0.0021 | 0.0022 |
| CUS-DM-CUS-AMI vs. | |||
| AMI-C | 0.2486 | 0.0067 | 0.0021 |
| DM-C | 0.0021 | 0.0021 | 0.0021 |
| DM-AMI-C | 0.0021 | 0.0021 | 0.0022 |
| S-DM-CUS-AMI | 0.2243 | 0.0021 | 0.0022 |
| S-DM-CUN-AMI vs. | |||
| AMI-C | 0.0021 | 0.0046 | 0.0020 |
| DM-C | 0.0021 | 0.0021 | 0.0020 |
| DM-AMI-C | 0.0021 | 0.0021 | 0.0021 |
| S-DM-CUS-AMI | 0.0022 | 0.0021 | 0.0021 |
| CUN-DM-CUN-AMI vs. | |||
| AMI-C | 0.0020 | 0.0020 | 0.0021 |
| DM-C | 0.0020 | 0.0021 | 0.0021 |
| DM-AMI-C | 0.0020 | 0.0021 | 0.0022 |
| CUS-DM-CUS-AMI | 0.0020 | 0.0021 | 0.0022 |
| S-DM-CUN-AMI | 0.0046 | 0.0030 | 0.0032 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Boarescu, P.-M.; Boarescu, I.; Bocșan, I.C.; Gheban, D.; Bulboacă, A.E.; Nicula, C.; Pop, R.M.; Râjnoveanu, R.-M.; Bolboacă, S.D. Antioxidant and Anti-Inflammatory Effects of Curcumin Nanoparticles on Drug-Induced Acute Myocardial Infarction in Diabetic Rats. Antioxidants 2019, 8, 504. https://doi.org/10.3390/antiox8100504
Boarescu P-M, Boarescu I, Bocșan IC, Gheban D, Bulboacă AE, Nicula C, Pop RM, Râjnoveanu R-M, Bolboacă SD. Antioxidant and Anti-Inflammatory Effects of Curcumin Nanoparticles on Drug-Induced Acute Myocardial Infarction in Diabetic Rats. Antioxidants. 2019; 8(10):504. https://doi.org/10.3390/antiox8100504
Chicago/Turabian StyleBoarescu, Paul-Mihai, Ioana Boarescu, Ioana Corina Bocșan, Dan Gheban, Adriana Elena Bulboacă, Cristina Nicula, Raluca Maria Pop, Ruxandra-Mioara Râjnoveanu, and Sorana D. Bolboacă. 2019. "Antioxidant and Anti-Inflammatory Effects of Curcumin Nanoparticles on Drug-Induced Acute Myocardial Infarction in Diabetic Rats" Antioxidants 8, no. 10: 504. https://doi.org/10.3390/antiox8100504
APA StyleBoarescu, P.-M., Boarescu, I., Bocșan, I. C., Gheban, D., Bulboacă, A. E., Nicula, C., Pop, R. M., Râjnoveanu, R.-M., & Bolboacă, S. D. (2019). Antioxidant and Anti-Inflammatory Effects of Curcumin Nanoparticles on Drug-Induced Acute Myocardial Infarction in Diabetic Rats. Antioxidants, 8(10), 504. https://doi.org/10.3390/antiox8100504











