Testicular and Haematological Cancer Induce Very High Levels of Sperm Oxidative Stress
Abstract
1. Introduction
2. Materials and Methods
2.1. Reagents and Media
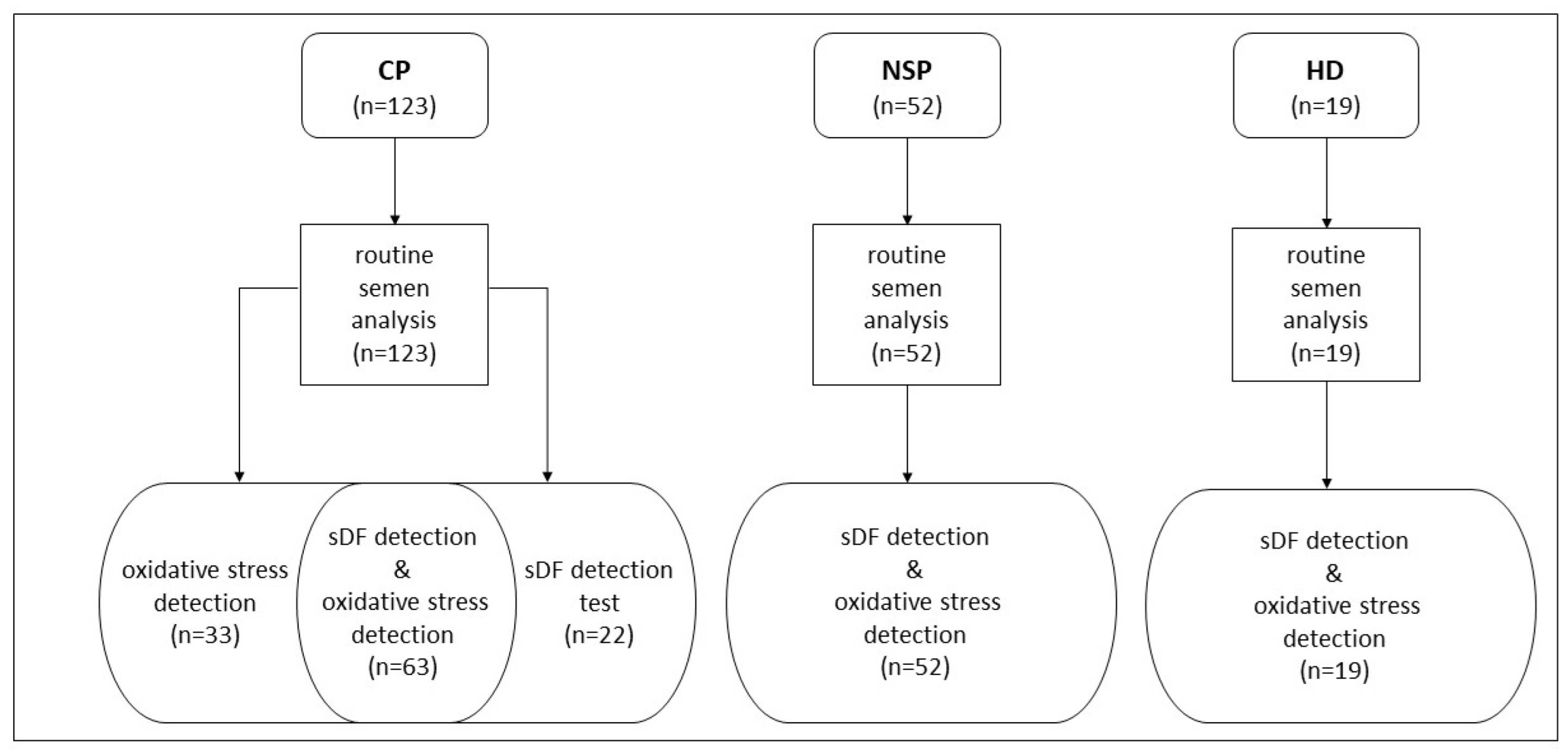
2.2. Study Population and Semen Collection
2.3. Routine Semen Analysis
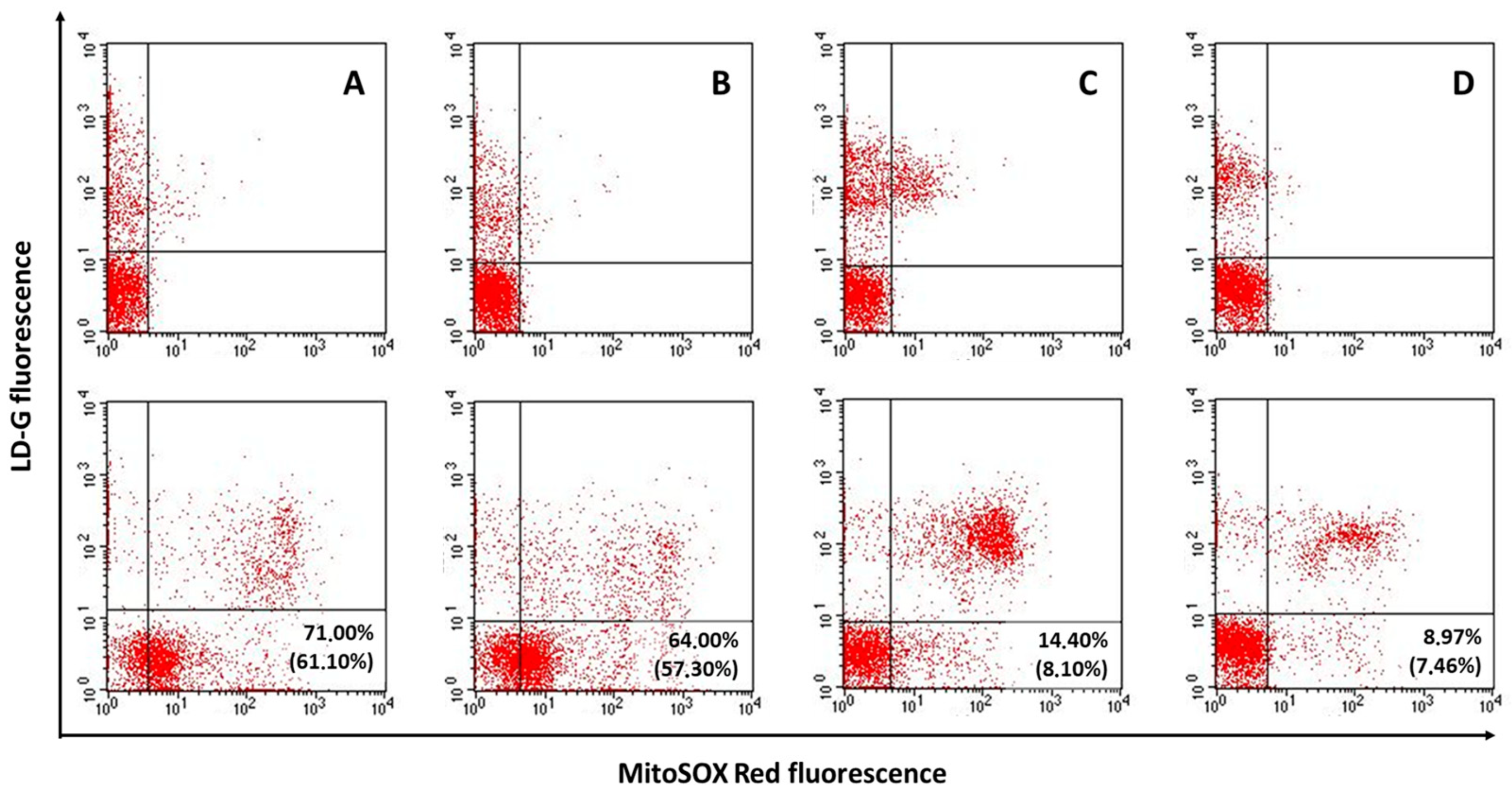
2.4. Determination of Semen Oxidative Stress
2.5. Determination of sDF
2.6. Statistical Analyses
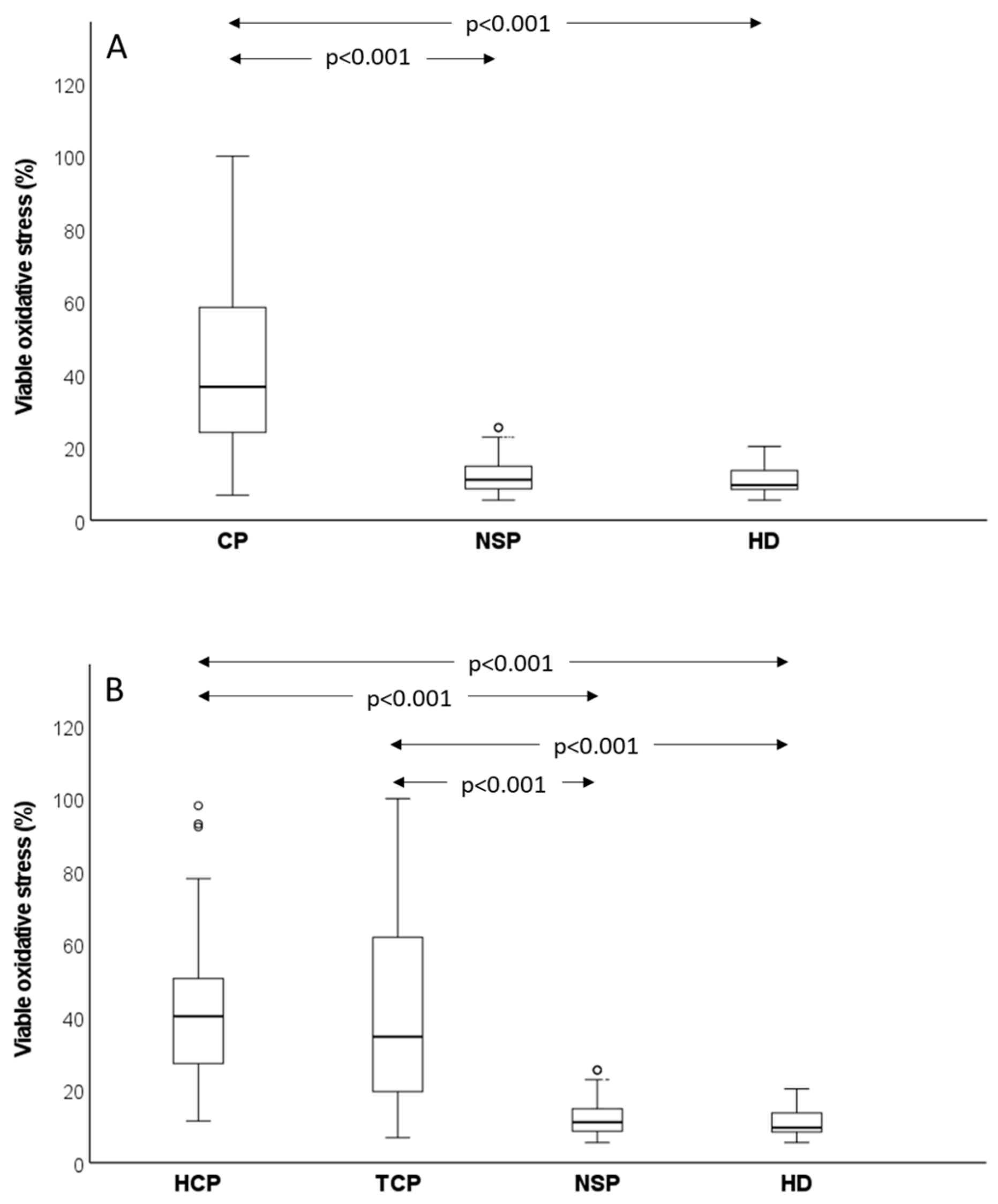
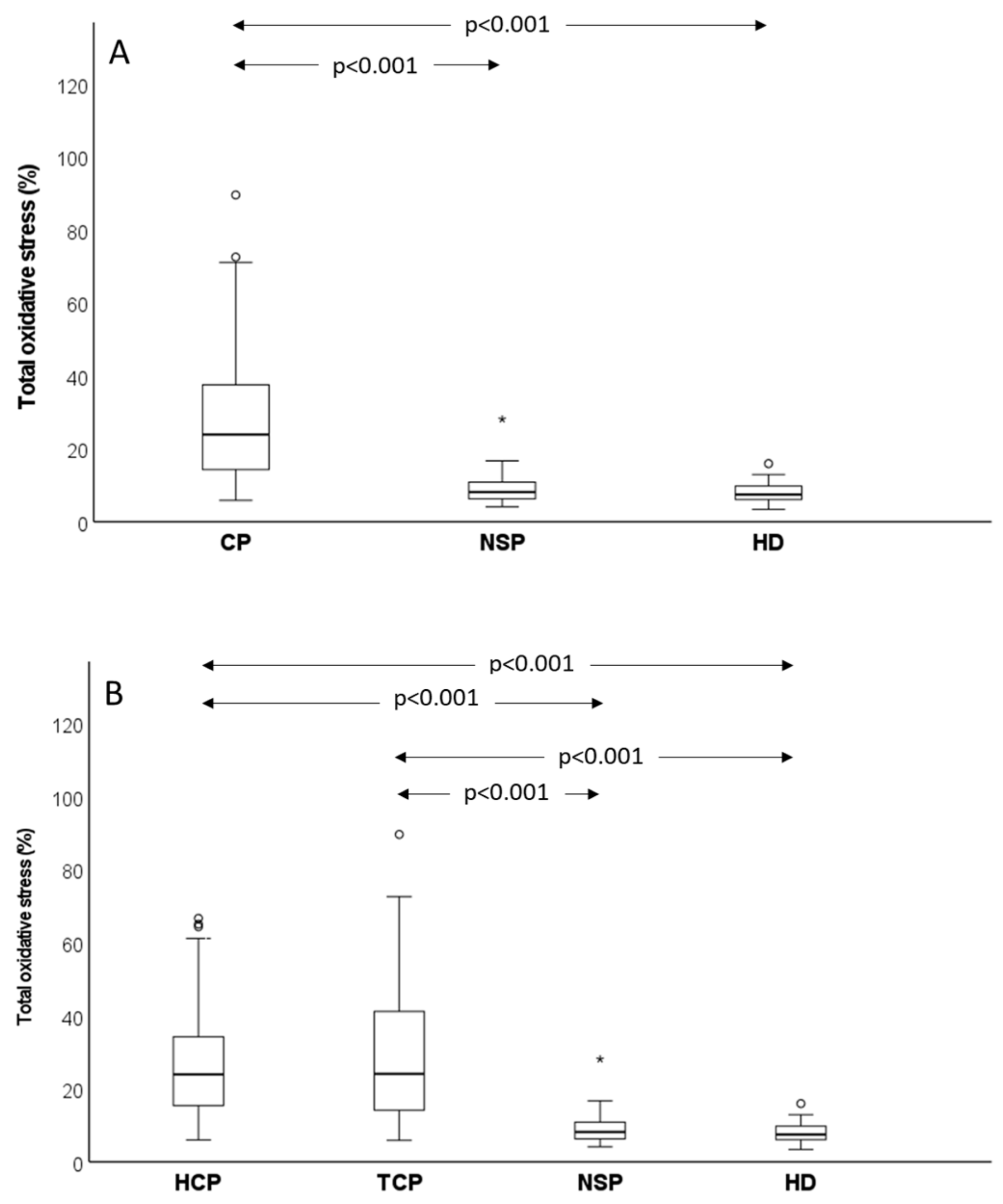
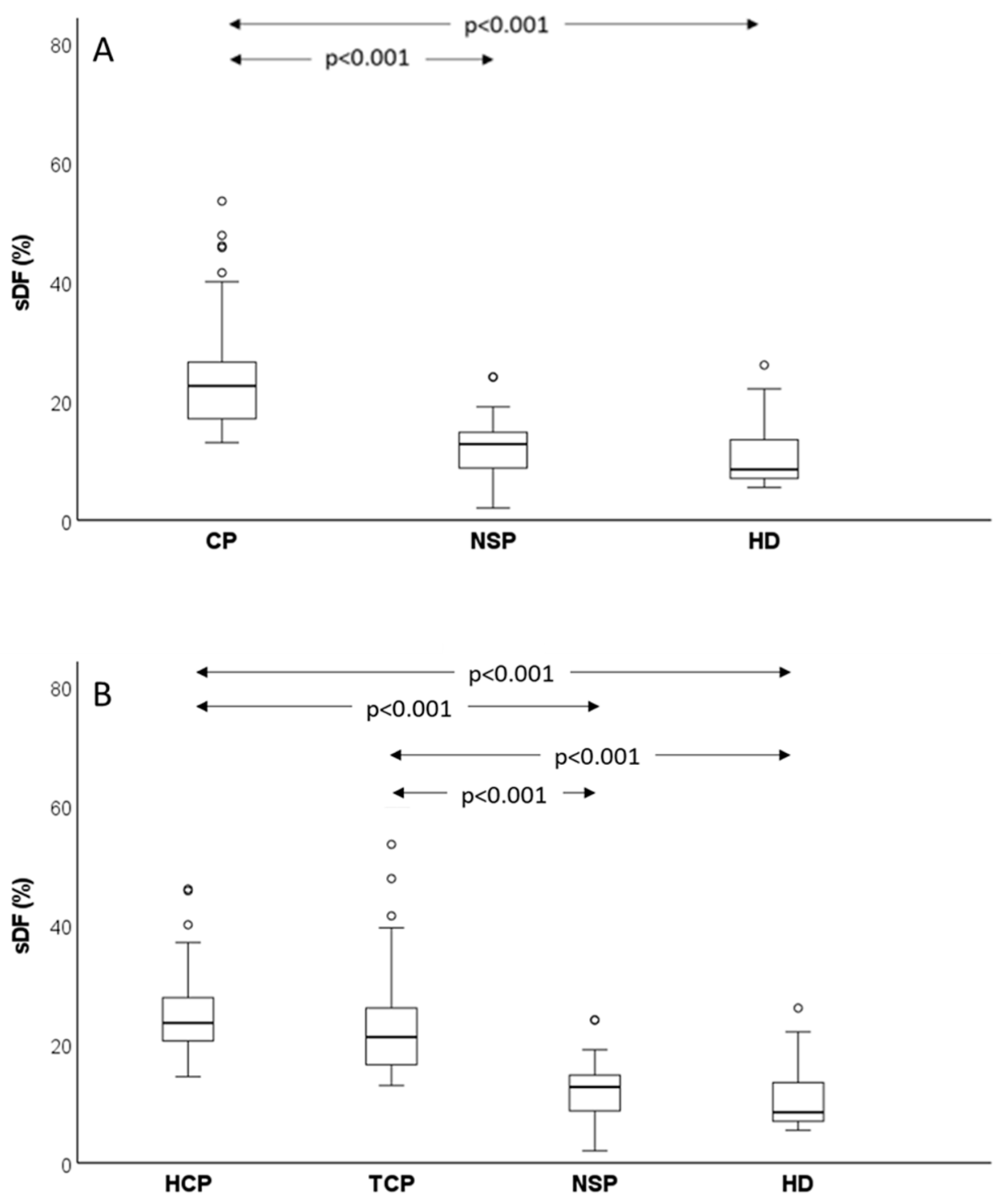
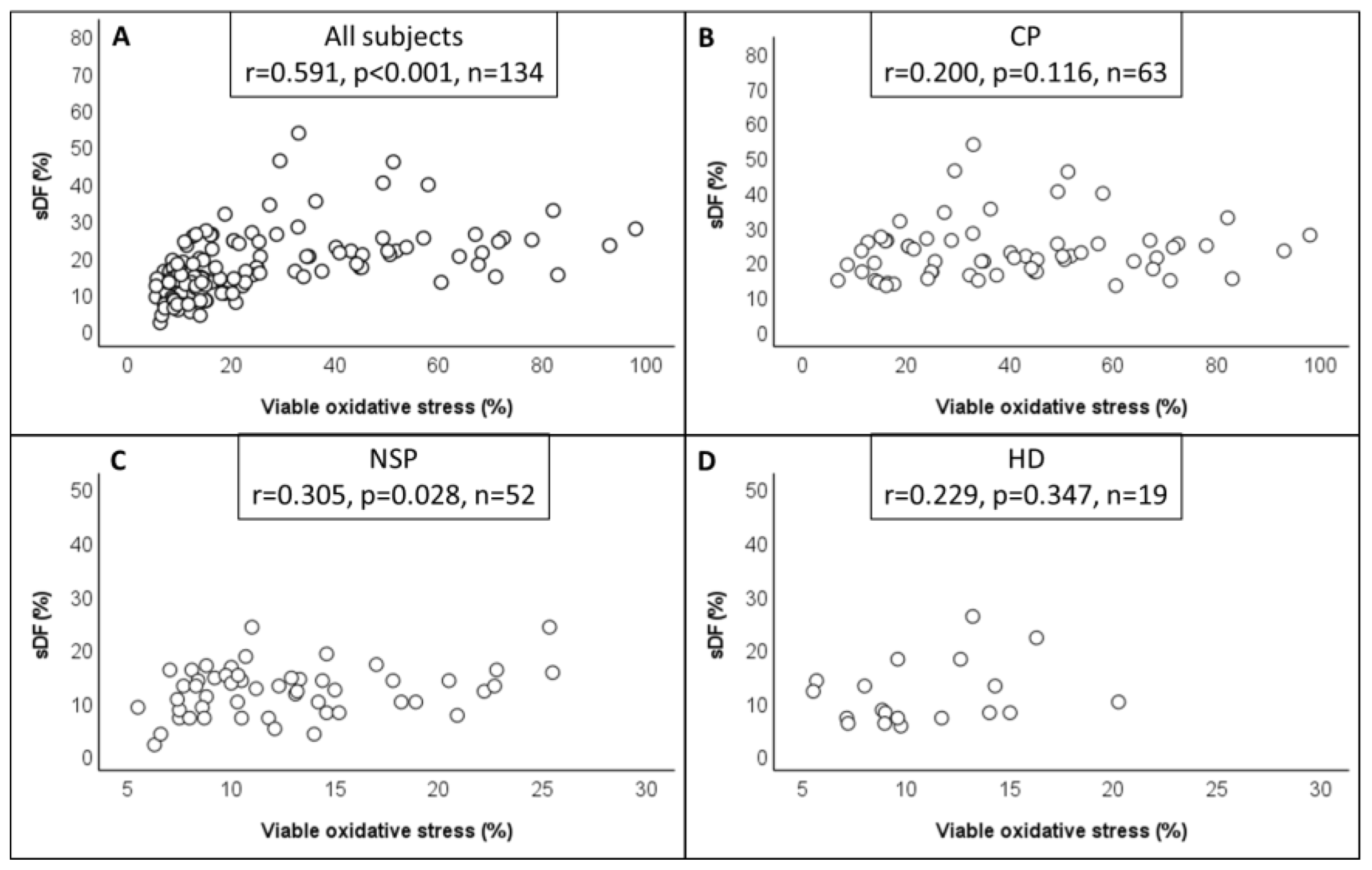
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kocarnik, J.M.; Compton, K.; Dean, F.E.; Fu, W.; Gaw, B.L.; Harvey, J.D.; Henrikson, H.J.; Lu, D.; Pennini, A.; Xu, R.; et al. Cancer Incidence, Mortality, Years of Life Lost, Years Lived With Disability, and Disability-Adjusted Life Years for 29 Cancer Groups From 2010 to 2019: A Systematic Analysis for the Global Burden of Disease Study 2019. JAMA Oncol. 2022, 8, 420–444. [Google Scholar] [PubMed]
- Howlader, N.; Noone, A.M.; Krapcho, M.; Neyman, N.; Aminou, R.; Waldron, W.; Altekruse, S.F.; Kosary, C.L.; Ruhl, J.; Tatalovich, Z.; et al. (Eds.) SEER Cancer Statistics Review, 1975–2008; National Cancer Institute: Bethesda, MD, USA, 2011. Available online: https://seer.cancer.gov/csr/1975_2008 (accessed on 20 January 2023).
- Depalo, R.; Falagario, D.; Masciandaro, P.; Nardelli, C.; Vacca, M.P.; Capuano, P.; Specchia, G.; Battaglia, M. Fertility preservation in males with cancer: 16-year monocentric experience of sperm banking and post-thaw reproductive outcomes. Ther. Adv. Med. Oncol. 2016, 8, 412–420. [Google Scholar] [CrossRef] [PubMed]
- American Cancer Society. Cancer Facts & Figures. 2012. Available online: http://www.cancer.org/research/cancerfactsstatistics/cancerfactsfigures2012/ (accessed on 1 January 2012).
- Meistrich, M.L. Effects of chemotherapy and radiotherapy on spermatogenesis in humans. Fertil. Steril. 2013, 100, 1180–1186. [Google Scholar] [CrossRef]
- Trost, L.W.; Brannigan, R.E. Oncofertility and the male cancer patient. Curr. Treat. Options Oncol. 2012, 13, 146–160. [Google Scholar] [CrossRef]
- Paoli, D.; Pallotti, F.; Lenzi, A.; Lombardo, F. Fatherhood and Sperm DNA Damage in Testicular Cancer Patients. Front. Endocrinol. 2018, 9, 506. [Google Scholar] [CrossRef] [PubMed]
- Farnetani, G.; Fino, M.G.; Cioppi, F.; Riera-Escamilla, A.; Tamburrino, L.; Vannucci, M.; Rosta, V.; Vinci, S.; Casamonti, E.; Turki, L.; et al. Long-term effect of cytotoxic treatments on sperm DNA fragmentation in patients affected by testicular germ cell tumor. Andrology 2023, 17. [Google Scholar] [CrossRef]
- Loren, A.W.; Mangu, P.B.; Beck, L.N.; Brennan, L.; Magdalinski, A.J.; Partridge, A.H.; Quinn, G.; Wallace, W.H.; Oktay, K. American Society of Clinical Oncology. Fertility preservation for patients with cancer: American Society of Clinical Oncology clinical practice guideline update. J. Clin. Oncol. 2013, 19, 2500–2510. [Google Scholar] [CrossRef]
- Ethics Committee of the American Society for Reproductive Medicine. Fertility preservation and reproduction in patients facing gonadotoxic therapies: An Ethics Committee opinion. Fertil Steril. 2018, 110, 380–386. [Google Scholar] [CrossRef] [PubMed]
- Skakkebaek, N.E.; Rajpert-De Meyts, E.; Buck Louis, G.M.; Toppari, J.; Andersson, A.M.; Eisenberg, M.L.; Jensen, T.K.; Jørgensen, N.; Swan, S.H.; Sapra, K.J.; et al. Male Reproductive Disorders and Fertility Trends: Influences of Environment and Genetic Susceptibility. Physiol. Rev. 2016, 96, 55–97. [Google Scholar] [CrossRef]
- Van Casteren, N.J.; Boellaard, W.P.; Romijn, J.C.; Dohle, G.R. Gonadal dysfunction in male cancer patients before cytotoxic treatment. Int. J. Androl. 2010, 1, 73–79. [Google Scholar] [CrossRef]
- Rueffer, U.; Breuer, K.; Josting, A.; Lathan, B.; Sieber, M.; Manzke, O.; Grotenhermen, F.J.; Tesch, H.; Bredenfeld, H.; Koch, P.; et al. Male gonadal dysfunction in patients with Hodgkin’s disease prior to treatment. Ann. Oncol. 2001, 9, 1307–1311. [Google Scholar] [CrossRef]
- O’Donovan, M. An evaluation of chromatin condensation and DNA integrity in the spermatozoa of men with cancer before and after therapy. Andrologia 2005, 37, 83–90. [Google Scholar] [CrossRef]
- Spermon, J.R.; Ramos, L.; Wetzels, A.M.M.; Sweep, C.G.J.; Braat, D.D.M.; Kiemeney, L.A.; Witjes, J.A. Sperm integrity pre- and post-chemotherapy in men with testicular germ cell cancer. Hum. Reprod. 2006, 7, 1781–1786. [Google Scholar] [CrossRef] [PubMed]
- O’Flaherty, C.; Vaisheva, F.; Hales, B.F.; Chan, P.; Robaire, B. Characterization of sperm chromatin quality in testicular cancer and Hodgkin’s lymphoma patients prior to chemotherapy. Hum. Reprod. 2008, 5, 1044–1052. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, T.M.; Bertolla, R.P.; Spaine, D.M.; Fraietta, R.; Ortiz, V.; Cedenho, A.P. Sperm nuclear apoptotic DNA fragmentation in men with testicular cancer. Fertil. Steril. 2008, 90, 1782–1786. [Google Scholar] [CrossRef] [PubMed]
- Smit, M.; van Casteren, N.J.; Wildhagen, M.F.; Romijn, J.C.; Dohle, G.R. Sperm DNA integrity in cancer patients before and after cytotoxic treatment. Hum. Reprod. 2010, 8, 1877–1883. [Google Scholar] [CrossRef] [PubMed]
- WHO World Health Organization Laboratory Manual for the Examination and Processing of Human Semen; WHO Press: Geneve, Switzerland, 2010.
- Riley, L.; Ammar, O.; Mello, T.; Giovannelli, L.; Vignozzi, L.; Muratori, M. Novel methods to detect ROS in viable spermatozoa of native semen samples. Reprod. Toxicol. 2021, 106, 51–60. [Google Scholar] [CrossRef]
- Arciero, V.; Ammar, O.; Maggi, M.; Vignozzi, L.; Muratori, M.; Dabizzi, S. Vapour fast freezing with low semen volumes can highly improve motility and viability or DNA quality of cryopreserved human spermatozoa. Andrology 2022, 6, 1123–1133. [Google Scholar] [CrossRef]
- Marchiani, S.; Tamburrino, L.; Maoggi, A.; Vannelli, G.B.; Forti, G.; Baldi, E.; Muratori, M. Characterization of M540 bodies in human semen: Evidence that they are apoptotic bodies. Mol. Hum. Reprod. 2007, 13, 621–631. [Google Scholar] [CrossRef]
- Fernández, J.L.; Muriel, L.; Rivero, M.T.; Goyanes, V.; Vazquez, R.; Alvarez, J.G. The sperm chromatin dispersion test: A simple method for the determination of sperm DNA fragmentation. J. Androl. 2003, 24, 59–66. [Google Scholar]
- Djaladat, H.; Burner, E.; Parikh, P.M.; Beroukhim Kay, D.; Hays, K. The Association Between Testis Cancer and Semen Abnormalities Before Orchiectomy: A Systematic Review. J. Adolesc. Young Adult Oncol. 2014, 4, 153–159. [Google Scholar] [CrossRef]
- Williams, D.H.; Karpman, E.; Sander, J.C.; Spiess, P.E.; Pisters, L.L.; Lipshultz, L.I. Pretreatment semen parameters in men with cancer. J. Urol. 2009, 181, 736–740. [Google Scholar] [CrossRef] [PubMed]
- O’Flaherty, C.; Hales, B.F.; Chan, P.; Robaire, B. Impact of chemotherapeutics and advanced testicular cancer or Hodgkin lymphoma on sperm deoxyribonucleic acid integrity. Fertil. Steril. 2010, 94, 1374–1379. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, A.; Allamaneni, S.S. Disruption of spermatogenesis by the cancer disease process. J. Natl. Cancer Inst. Monogr. 2005, 34, 9–12. [Google Scholar] [CrossRef] [PubMed]
- Vakalopoulos, I.; Dimou, P.; Anagnostou, I.; Zeginiadou, T. Impact of cancer and cancer treatment on male fertility. Hormones 2015, 14, 579–589. [Google Scholar] [CrossRef] [PubMed]
- Sabanegh, E.S., Jr.; Ragheb, A.M. Male fertility after cancer. Urology 2009, 73, 225–231. [Google Scholar] [CrossRef]
- Michailov, Y.; Lunenfeld, E.; Kapelushnik, J.; Huleihel, M. Leukemia and male infertility: Past, present, and future. Leuk. Lymphoma 2019, 60, 1126–1135. [Google Scholar] [CrossRef]
- van der Kaaij, M.A.; Heutte, N.; van Echten-Arends, J.; Raemaekers, J.M.; Carde, P.; Noordijk, E.M.; Fermé, C.; Thomas, J.; Eghbali, H.; Brice, P.; et al. Sperm quality before treatment in patients with early stage Hodgkin’s lymphoma enrolled in EORTC-GELA Lymphoma Group trials. Haematologica 2009, 94, 1691–1697. [Google Scholar] [CrossRef]
- Paoli, D.; Rizzo, F.; Fiore, G.; Pallotti, F.; Pulsoni, A.; Annechini, G.; Lombardo, F.; Lenzi, A.; Gandini, L. Spermatogenesis in Hodgkin’s lymphoma patients: A retrospective study of semen quality before and after different chemotherapy regimens. Hum. Reprod. 2016, 31, 263–272. [Google Scholar] [CrossRef]
- Pallotti, F.; Pelloni, M.; Faja, F.; Di Chiano, S.; Di Rocco, A.; Lenzi, A.; Lombardo, F.; Paoli, D. Semen quality in non-Hodgkin lymphoma survivors: A monocentric retrospective study. Hum. Reprod. 2021, 36, 16–25. [Google Scholar] [CrossRef]
- Muratori, M.; Marchiani, S.; Tamburrino, L.; Tocci, V.; Failli, P.; Forti, G.; Baldi, E. Nuclear staining identifies two populations of human sperm with different DNA fragmentation extent and relationship with semen parameters. Hum. Reprod. 2008, 23, 1035–1043. [Google Scholar] [CrossRef]
- Lotti, F.; Tamburrino, L.; Marchiani, S.; Maseroli, E.; Vitale, P.; Forti, G.; Muratori, M.; Maggi, M.; Baldi, E. DNA fragmentation in two cytometric sperm populations: Relationship with clinical and ultrasound characteristics of the male genital tract. Asian J. Androl. 2017, 19, 272–279. [Google Scholar] [PubMed]
- Sergerie, M.; Mieusset, R.; Croute, F.; Daudin, M.; Bujan, L. High risk of temporary alteration of semen parameters after recent acute febrile illness. Fertil. Steril. 2007, 88, 970. [Google Scholar] [CrossRef] [PubMed]
- Tesarik, J.; Martinez, F.; Rienzi, L.; Iacobelli, M.; Ubaldi, F.; Mendoza, C.; Greco, E. In-vitro effects of FSH and testosterone withdrawal on caspase activation and DNA fragmentation in different cell types of human seminiferous epithelium. Hum. Reprod. 2002, 17, 1811–1819. [Google Scholar] [CrossRef] [PubMed]
- Muratori, M.; Baldi, E. Effects of FSH on Sperm DNA Fragmentation: Review of Clinical Studies and Possible Mechanisms of Action. Front. Endocrinol 2018, 9, 734. [Google Scholar] [CrossRef] [PubMed]
- Potter, S.J.; DeFalco, T. Role of the testis interstitial compartment in spermatogonial stem cell function. Reproduction 2017, 153, 151–162. [Google Scholar] [CrossRef]
- Loveland, K.L.; Klein, B.; Pueschl, D.; Indumathy, S.; Bergmann, M.; Loveland, B.E.; Hedger, M.P.; Schuppe, H.C. Cytokines in Male Fertility and Reproductive Pathologies: Immunoregulation and Beyond. Front. Endocrinol. 2017, 20, 307. [Google Scholar] [CrossRef]
- Hsu, H.C.; Lee, Y.M.; Tsai, W.H.; Jiang, M.L.; Ho, C.H.; Ho, C.K.; Wang, S.Y. Circulating levels of thrombopoietic and inflammatory cytokines in patients with acute myeloblastic leukemia and myelodysplastic syndrome. Oncology 2002, 63, 64–69. [Google Scholar] [CrossRef]
- Bhushan, S.; Meinhardt, A. The macrophages in testis function. J. Reprod. Immunol. 2017, 119, 107–112. [Google Scholar] [CrossRef]
- Nicolini, F.E.; Alcazer, V.; Huguet, F.; Cony-Makhoul, P.; Heiblig, M.; Fort, M.P.; Morisset, S.; Guerci-Bresler, A.; Soula, V.; Sobh, M.; et al. CML patients show sperm alterations at diagnosis that are not improved with imatinib treatment. Leuk. Res. 2016, 48, 80–83. [Google Scholar] [CrossRef]
- Richie, J.P. Neoplasms of the testis. In Campbell’s Urology, 7th ed.; Walch, P.C., Retik, A.B., Vaughan, E.D., Eds.; Saunders: Philadelphia, PA, USA, 1998; p. 2411. [Google Scholar]
- Muratori, M.; Tamburrino, L.; Marchiani, S.; Cambi, M.; Olivito, B.; Azzari, C.; Forti, G.; Baldi, E. Investigation on the Origin of Sperm DNA Fragmentation: Role of Apoptosis, Immaturity and Oxidative Stress. Mol. Med. 2015, 21, 109–122. [Google Scholar] [CrossRef]
- Hussain, T.; Kandeel, M.; Metwally, E.; Murtaza, G.; Kalhoro, D.H.; Yin, Y.; Tan, B.; Chughtai, M.I.; Yaseen, A.; Afzal, A.; et al. Unraveling the harmful effect of oxidative stress on male fertility: A mechanistic insight. Front. Endocrinol. 2023, 14, 1070692. [Google Scholar] [CrossRef] [PubMed]
- Klein, B.; Haggeney, T.; Fietz, D.; Indumathy, S.; Loveland, K.L.; Hedger, M.; Kliesch, S.; Weidner, W.; Bergmann, M.; Schuppe, H.C. Specific immune cell and cytokine characteristics of human testicular germ cell neoplasia. Hum. Reprod. 2016, 31, 2192–2202. [Google Scholar] [CrossRef] [PubMed]
- Białas, M.; Fiszer, D.; Rozwadowska, N.; Kosicki, W.; Jedrzejczak, P.; Kurpisz, M. The role of IL-6, IL-10, TNF-alpha and its receptors TNFR1 and TNFR2 in the local regulatory system of normal and impaired human spermatogenesis. Am. J. Reprod. Immunol. 2009, 62, 51–59. [Google Scholar] [CrossRef] [PubMed]
- Van Etten, R.A. Aberrant cytokine signaling in leukemia. Oncogene 2007, 26, 6738–6749. [Google Scholar] [CrossRef]
- Karavani, G.; Feigin, N.; Tachover, T.; Bdolah-Abram, T.; Lavie, D.; Ben-Yehuda, D.; Ben-Meir, A. Parameters associated with sperm quality prior to chemotherapy in lymphoma patients. Andrologia 2020, 52, 13794. [Google Scholar] [CrossRef]
- Xavier, R.; de Carvalho, R.C.; Fraietta, R. Semen quality from patients affected by seminomatous and non-seminomatous testicular tumor. Int. Braz. J. Urol. 2021, 47, 495–502. [Google Scholar] [CrossRef]
- Degl’Innocenti, S.; Filimberti, E.; Magini, A.; Krausz, C.; Lombardi, G.; Fino, M.G.; Rastrelli, G.; Maggi, M.; Baldi, E. Semen cryopreservation for men banking for oligospermia, cancers, and other pathologies: Prediction of post-thaw outcome using basal semen quality. Fertil. Steril. 2013, 100, 1555–1563. [Google Scholar] [CrossRef]
- Kumar, A.; Prasad, J.K.; Srivastava, N.; Ghosh, S.K. Strategies to Minimize Various Stress-Related Freeze-Thaw Damages During Conventional Cryopreservation of Mammalian Spermatozoa. Biopreserv. Biobank. 2019, 17, 603–612. [Google Scholar] [CrossRef]
- Tamburrino, L.; Cambi, M.; Marchiani, S.; Manigrasso, I.; Degl’Innocenti, S.; Forti, G.; Maggi, M.; Baldi, E.; Muratori, M. Sperm DNA fragmentation in cryopreserved samples from subjects with different cancers. Reprod. Fertil. Dev. 2017, 29, 637–645. [Google Scholar] [CrossRef]
- Silva, A.M.; Correia, S.; Socorro, S.; Maia, C.J. Endogenous Factors in the Recovery of Reproductive Function After Testicular Injury and Cancer. Curr. Mol. Med. 2016, 16, 631–649. [Google Scholar] [CrossRef] [PubMed]
- Drevet, J.R.; Hallak, J.; Nasr-Esfahani, M.H.; Aitken, R.J. Reactive Oxygen Species and Their Consequences on the Structure and Function of Mammalian Spermatozoa. Antioxid. Redox Signal. 2022, 37, 481–500. [Google Scholar] [CrossRef] [PubMed]
- Chan, D.; Oros Klein, K.; Riera-Escamilla, A.; Krausz, C.; O’Flaherty, C.; Chan, P.; Robaire, B.; Trasler, J.M. Sperm DNA methylome abnormalities occur both pre- and post-treatment in men with Hodgkin disease and testicular cancer. Clin. Epigenetics 2023, 15, 5. [Google Scholar] [CrossRef] [PubMed]
| Parameter | CP n = 123 | NSP n = 52 | HD n = 19 | p-Values | |
|---|---|---|---|---|---|
| Age (y) | 33.00 (27.00–37.00) | 35.00 (32.25–39.75) | 32.00 (26.00–36.00) | 0.019 1 | 0.021 2 1.00 3 0.184 4 |
| Abstinence (d) | 4.00 (3.00–6.00) | 4.00 (3.00–5.38) | 3.00 (2.00–4.00) | 0.015 1 | 1.00 2 0.033 3 0.012 4 |
| Volume (mL) | 3.00 (2.10–4.20) | 3.65 (2.60–4.48) | 3.50 (2.20–4.60) | 0.080 1 | |
| pH | 7.60 (7.40–7.80) | 7.60 (7.40–7.75) | 7.20 (7.20–7.40) | <0.001 1 | 0.765 2 <0.001 3 <0.001 4 |
| Concentration (106/mL) | 39.50 (12.00–74.30) | 112.50 (72.00–159.50) | 94.00 (47.00–102.00) | <0.001 1 | <0.001 2 0.006 3 0.693 4 |
| Number (106/ejaculate) | 97.20 (40.04–224.20) | 395.80 (252.20–620.88) | 226.78 (138.56–398.25) | <0.001 1 | <0.001 2 0.004 3 0.383 4 |
| Progressive Motility (%) | 42.00 (28.00–52.00) | 53.00 (46.00–61.75) | 56.00 (50.00–64.00) | <0.001 1 | <0.001 2 <0.001 3 1.00 4 |
| Immotile (%) | 46.00 (38.00–58.00) | 38.00 (31.50–44.00) | 34.00 (30.00–40.00) | <0.001 1 | <0.001 2 <0.001 3 0.784 4 |
| Normal Morphology (%) | 5.00 (3.00–7.00) | 6.00 (4.25–9.00) | 4.00 (4.00–3.00) | <0.001 1 | 0.004 2 0.395 3 0.002 4 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Calamai, C.; Ammar, O.; Rosta, V.; Farnetani, G.; Zimmitti, S.; Giovannelli, L.; Vignozzi, L.; Krausz, C.; Muratori, M. Testicular and Haematological Cancer Induce Very High Levels of Sperm Oxidative Stress. Antioxidants 2023, 12, 1145. https://doi.org/10.3390/antiox12061145
Calamai C, Ammar O, Rosta V, Farnetani G, Zimmitti S, Giovannelli L, Vignozzi L, Krausz C, Muratori M. Testicular and Haematological Cancer Induce Very High Levels of Sperm Oxidative Stress. Antioxidants. 2023; 12(6):1145. https://doi.org/10.3390/antiox12061145
Chicago/Turabian StyleCalamai, Costanza, Oumaima Ammar, Viktoria Rosta, Ginevra Farnetani, Salvatore Zimmitti, Lisa Giovannelli, Linda Vignozzi, Csilla Krausz, and Monica Muratori. 2023. "Testicular and Haematological Cancer Induce Very High Levels of Sperm Oxidative Stress" Antioxidants 12, no. 6: 1145. https://doi.org/10.3390/antiox12061145
APA StyleCalamai, C., Ammar, O., Rosta, V., Farnetani, G., Zimmitti, S., Giovannelli, L., Vignozzi, L., Krausz, C., & Muratori, M. (2023). Testicular and Haematological Cancer Induce Very High Levels of Sperm Oxidative Stress. Antioxidants, 12(6), 1145. https://doi.org/10.3390/antiox12061145







