Inflammation and Vitamin C in Women with Prenatal Depression and Anxiety: Effect of Multinutrient Supplementation
Abstract
1. Introduction
2. Materials and Methods
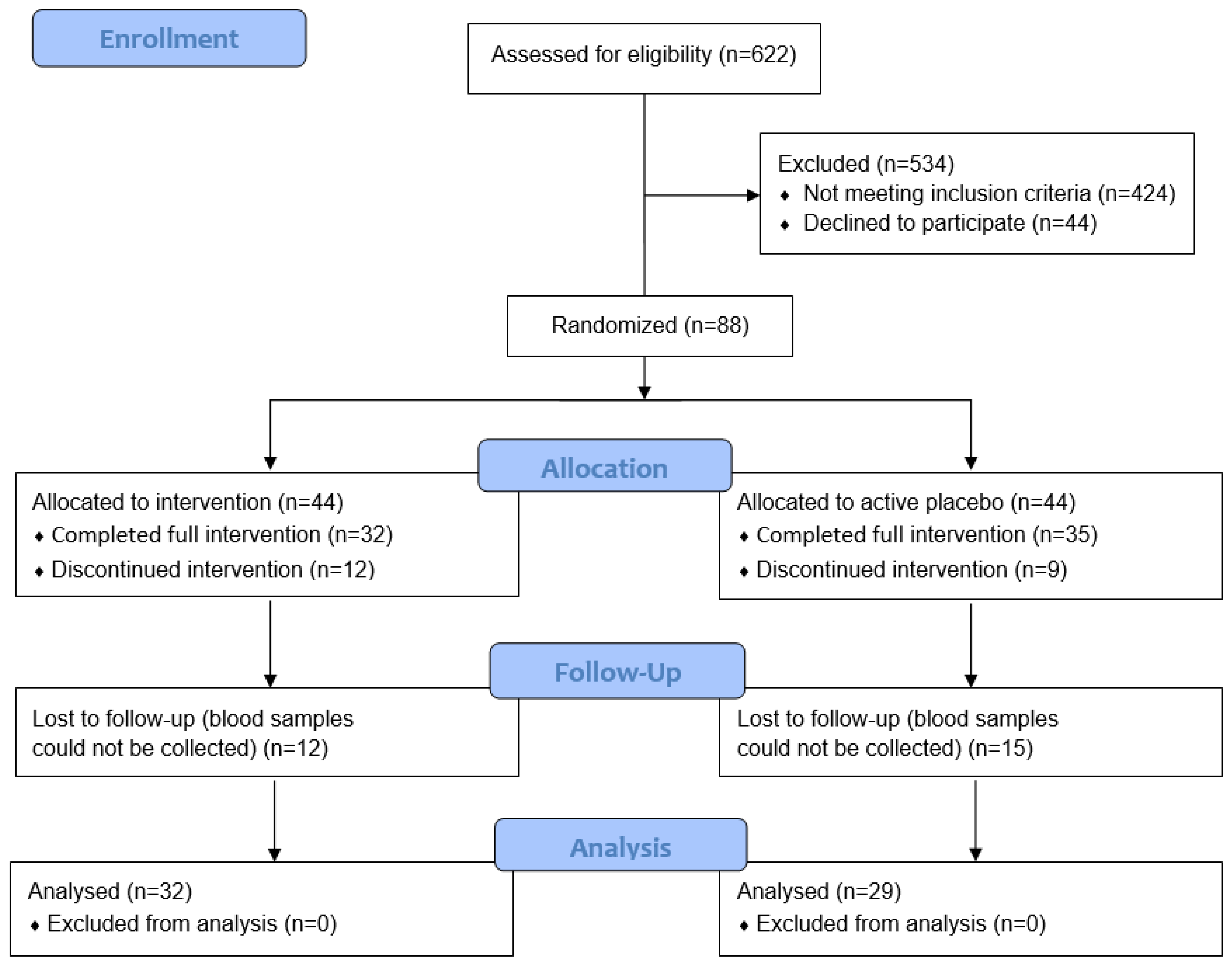
2.1. Study Participants
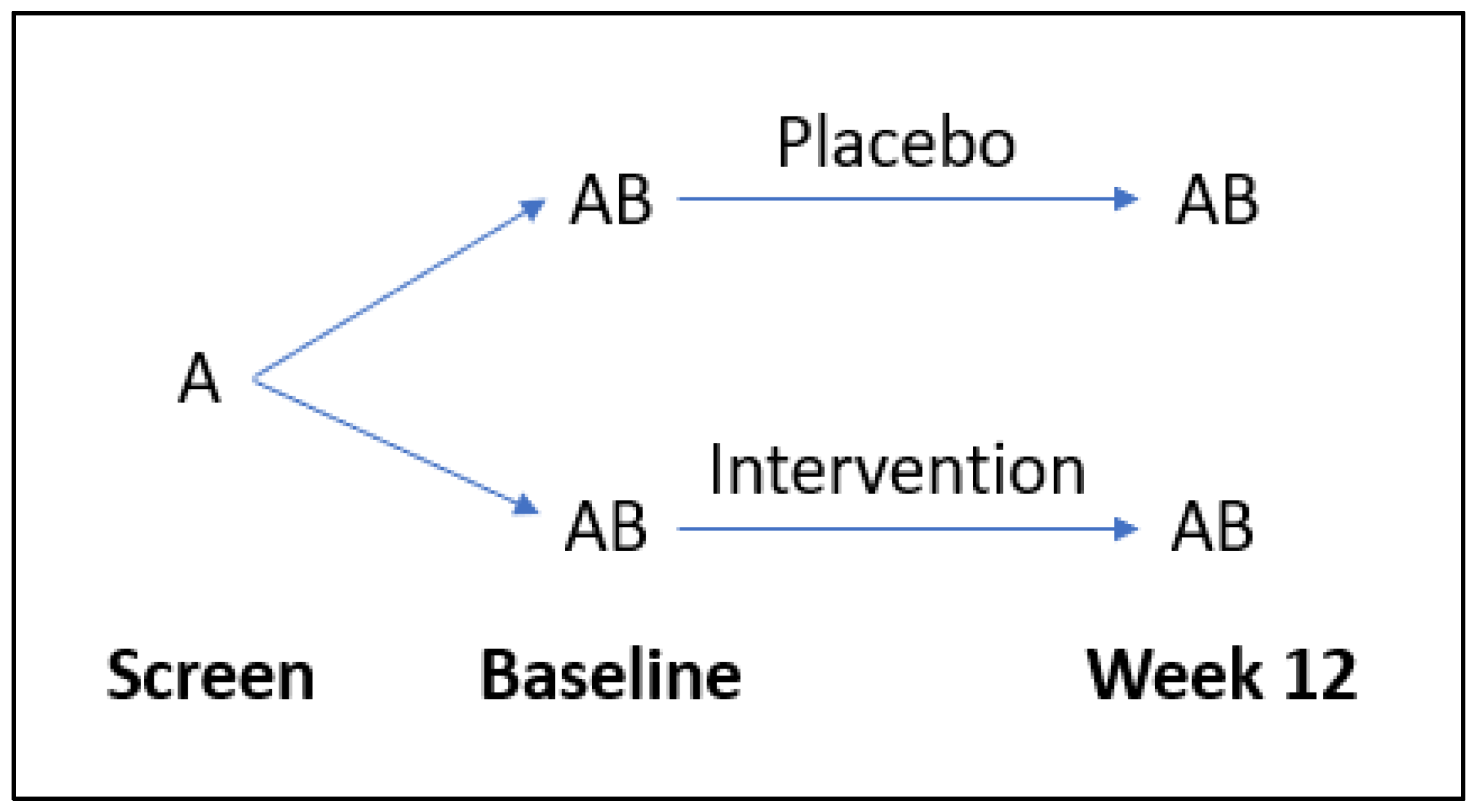
2.2. Intervention
2.3. Data Collection
2.4. Mood Questionnaires
2.5. Sample Collection and Biomarker Analyses
2.6. Statistical Analyses
3. Results
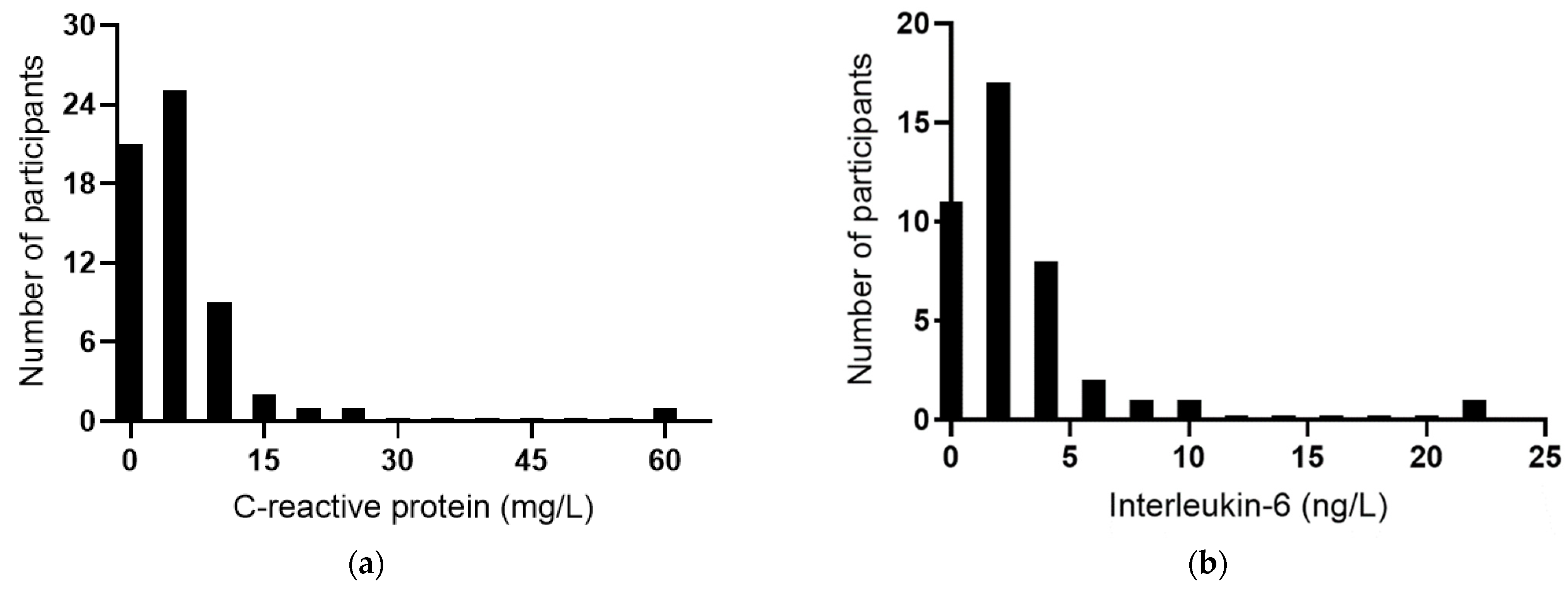
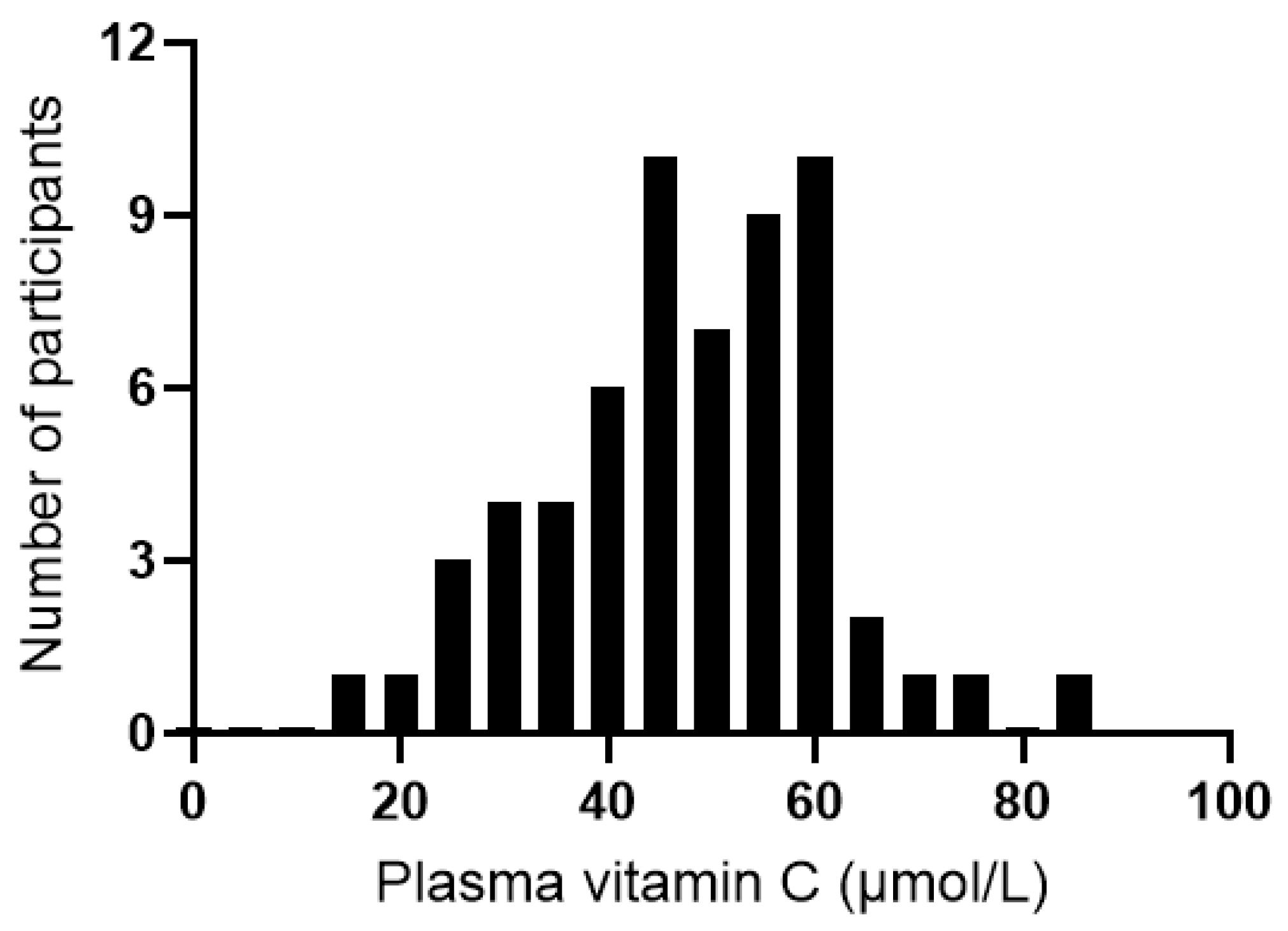
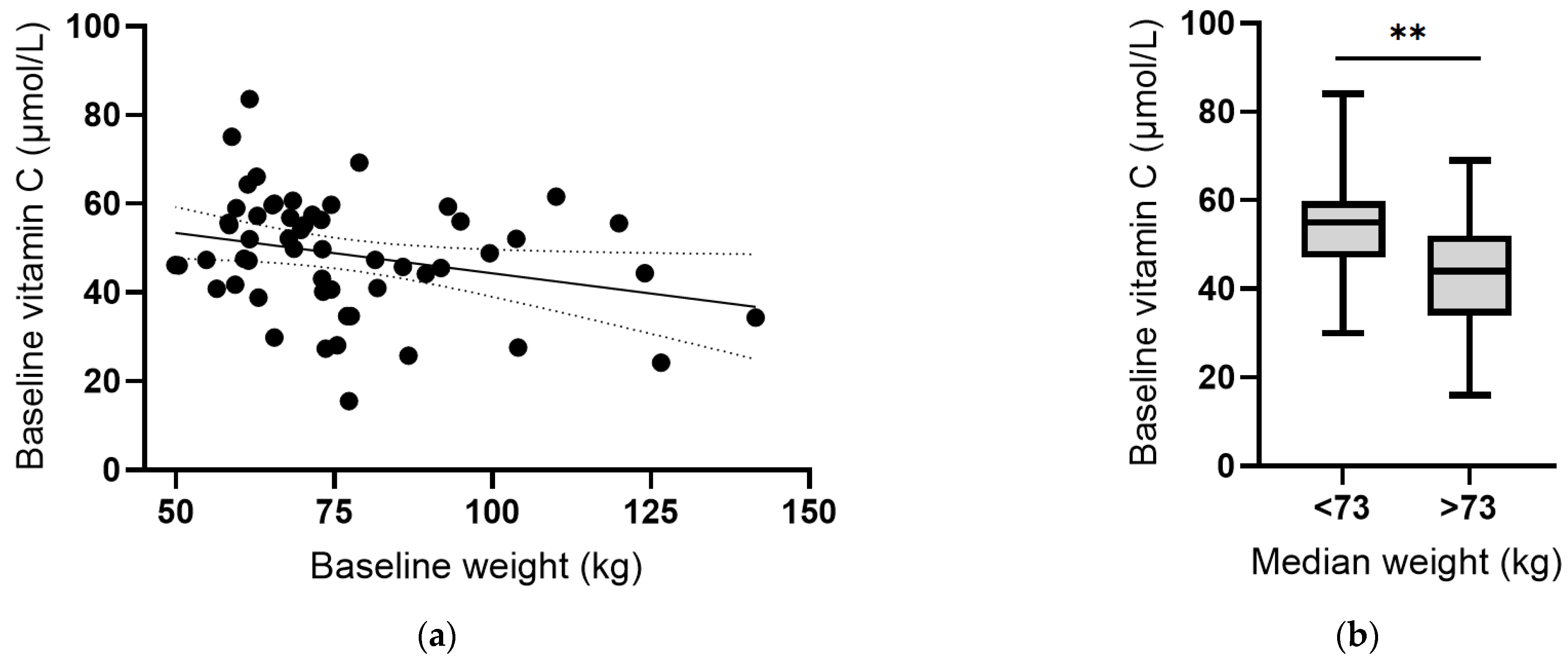
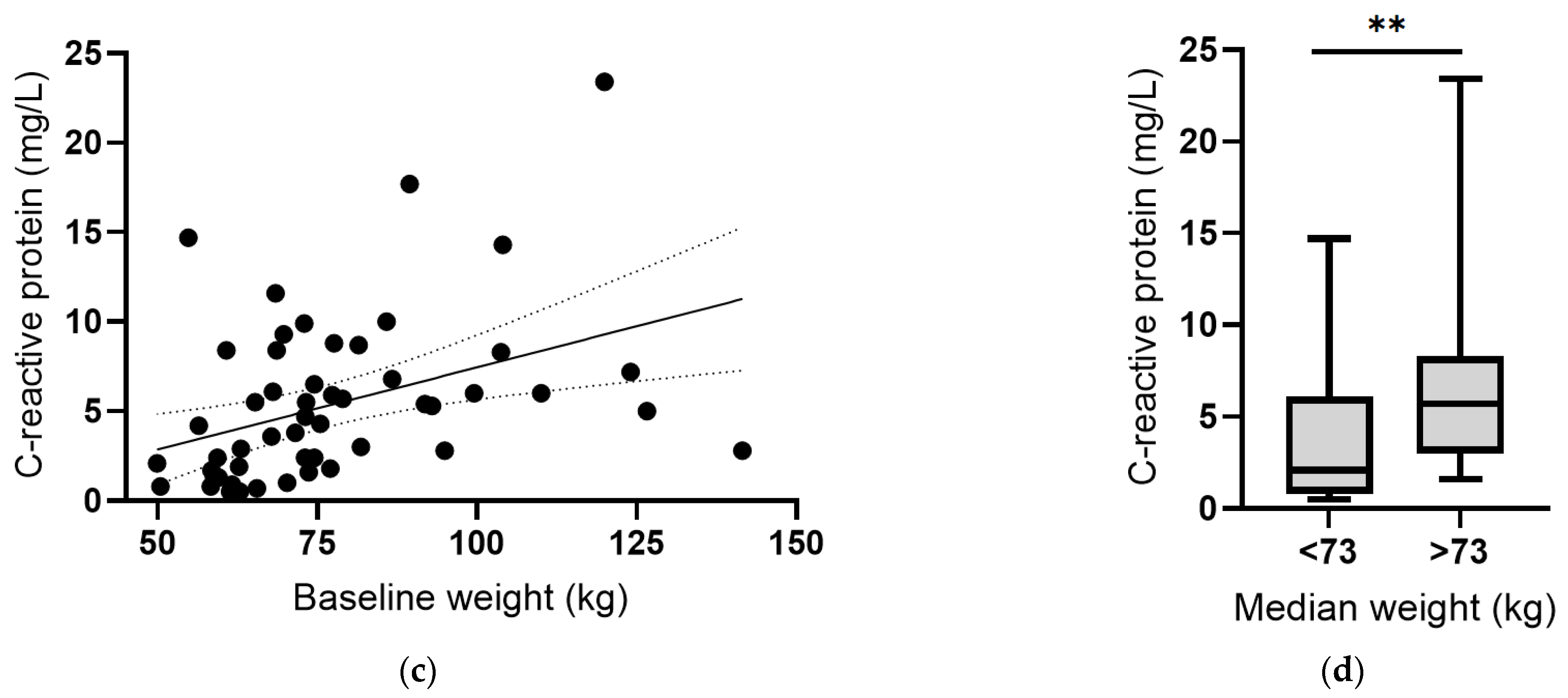
3.1. Participant Characteristics
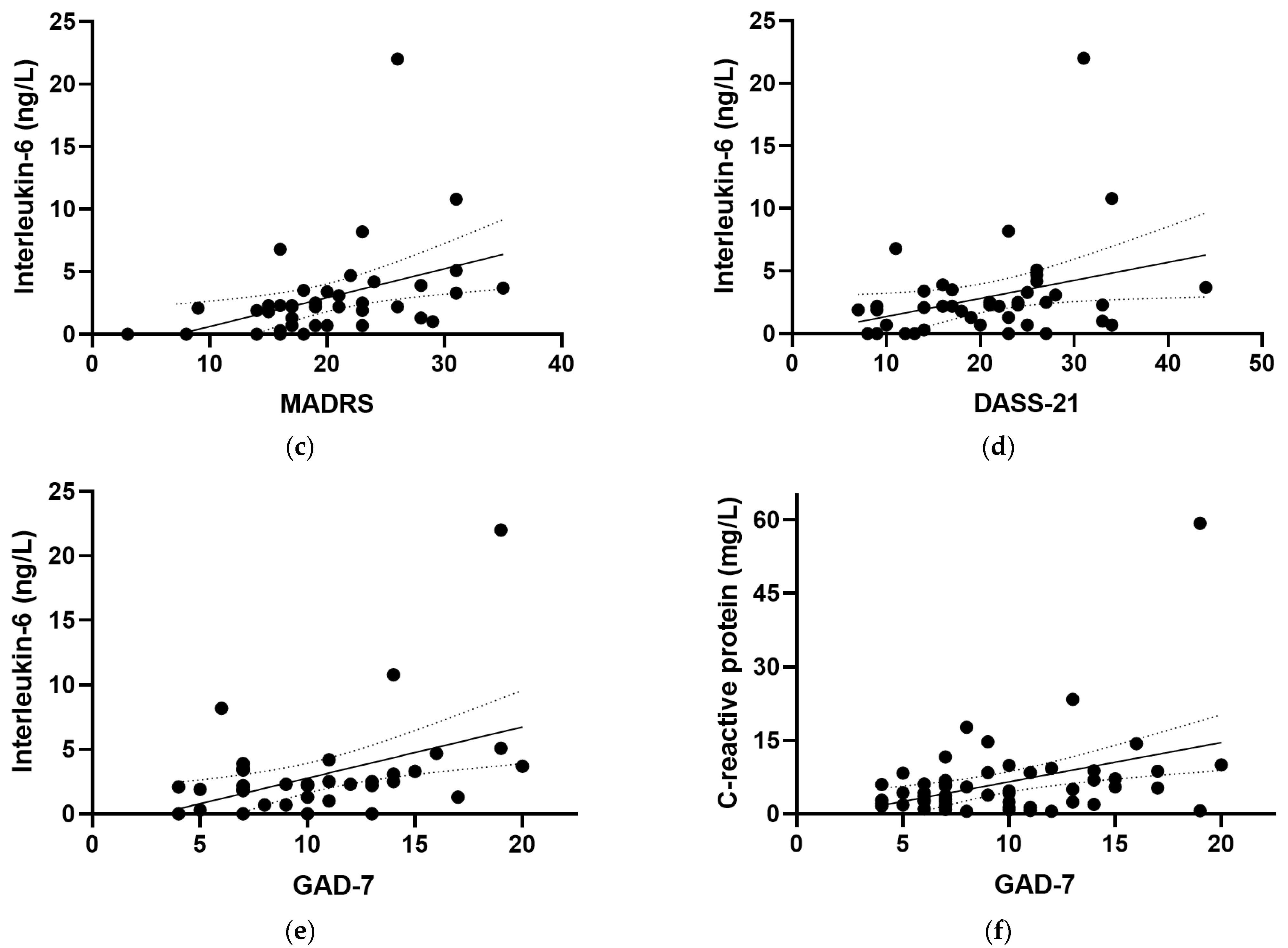
3.2. Relationship of Inflammation with Mood
3.3. Relationship of Inflammation with Vitamin C Status
3.4. Effect of Multinutrient Supplementation on Vitamin C Status and Inflammation
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mathers, C.D.; Loncar, D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006, 3, e442. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; DSM-5; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- Signal, T.L.; Paine, S.J.; Sweeney, B.; Muller, D.; Priston, M.; Lee, K.; Gander, P.; Huthwaite, M. The prevalence of symptoms of depression and anxiety, and the level of life stress and worry in New Zealand Māori and non-Māori women in late pregnancy. Aust. N. Z. J. Psychiatry 2017, 51, 168–176. [Google Scholar] [CrossRef] [PubMed]
- Letourneau, N.L.; Dennis, C.L.; Cosic, N.; Linder, J. The effect of perinatal depression treatment for mothers on parenting and child development: A systematic review. Depress. Anxiety 2017, 34, 928–966. [Google Scholar] [CrossRef]
- Osimo, E.F.; Pillinger, T.; Rodriguez, I.M.; Khandaker, G.M.; Pariante, C.M.; Howes, O.D. Inflammatory markers in depression: A meta-analysis of mean differences and variability in 5,166 patients and 5,083 controls. Brain Behav. Immun. 2020, 87, 901–909. [Google Scholar] [CrossRef] [PubMed]
- Cassidy-Bushrow, A.E.; Peters, R.M.; Johnson, D.A.; Templin, T.N. Association of depressive symptoms with inflammatory biomarkers among pregnant African-American women. J. Reprod. Immunol. 2012, 94, 202–209. [Google Scholar] [CrossRef] [PubMed]
- Christian, L.M.; Franco, A.; Glaser, R.; Iams, J.D. Depressive symptoms are associated with elevated serum proinflammatory cytokines among pregnant women. Brain Behav. Immun. 2009, 23, 750–754. [Google Scholar] [CrossRef]
- Osborne, L.M.; Monk, C. Perinatal depression—The fourth inflammatory morbidity of pregnancy?: Theory and literature review. Psychoneuroendocrinology 2013, 38, 1929–1952. [Google Scholar] [CrossRef] [PubMed]
- Ravi, M.; Bernabe, B.; Michopoulos, V. Stress-related mental health disorders and inflammation in pregnancy: The current landscape and the need for further investigation. Front. Psychiatry 2022, 13, 868936. [Google Scholar] [CrossRef] [PubMed]
- Baskin, R.; Hill, B.; Jacka, F.N.; O’Neil, A.; Skouteris, H. The association between diet quality and mental health during the perinatal period. A systematic review. Appetite 2015, 91, 41–47. [Google Scholar] [CrossRef] [PubMed]
- Singh, A.; Trumpff, C.; Genkinger, J.; Davis, A.; Spann, M.; Werner, E.; Monk, C. Micronutrient dietary intake in Latina pregnant adolescents and its association with level of depression, stress, and social support. Nutrients 2017, 9, 1212. [Google Scholar] [CrossRef] [PubMed]
- Hornig, D. Distribution of ascorbic acid, metabolites and analogues in man and animals. Ann. N. Y. Acad. Sci. 1975, 258, 103–118. [Google Scholar] [CrossRef] [PubMed]
- Englard, S.; Seifter, S. The biochemical functions of ascorbic acid. Annu. Rev. Nutr. 1986, 6, 365–406. [Google Scholar] [CrossRef]
- May, J.M. Vitamin C transport and its role in the central nervous system. Subcell. Biochem. 2012, 56, 85–103. [Google Scholar] [CrossRef] [PubMed]
- Scaife, A.R.; McNeill, G.; Campbell, D.M.; Martindale, S.; Devereux, G.; Seaton, A. Maternal intake of antioxidant vitamins in pregnancy in relation to maternal and fetal plasma levels at delivery. Br. J. Nutr. 2006, 95, 771–778. [Google Scholar] [CrossRef] [PubMed]
- Morse, E.H.; Clarke, R.P.; Keyser, D.E.; Merrow, S.B.; Bee, D.E. Comparison of the nutritional status of pregnant adolescents with adult pregnant women. I. Biochemical findings. Am. J. Clin. Nutr. 1975, 28, 1000–1013. [Google Scholar] [CrossRef] [PubMed]
- Levine, M.; Conry-Cantilena, C.; Wang, Y.; Welch, R.W.; Washko, P.W.; Dhariwal, K.R.; Park, J.B.; Lazarev, A.; Graumlich, J.F.; King, J.; et al. Vitamin C pharmacokinetics in healthy volunteers: Evidence for a recommended dietary allowance. Proc. Natl. Acad. Sci. USA 1996, 93, 3704–3709. [Google Scholar] [CrossRef]
- Kinsman, R.A.; Hood, J. Some behavioral effects of ascorbic acid deficiency. Am. J. Clin. Nutr. 1971, 24, 455–464. [Google Scholar] [CrossRef]
- Moritz, B.; Schmitz, A.E.; Rodrigues, A.L.S.; Dafre, A.L.; Cunha, M.P. The role of vitamin C in stress-related disorders. J. Nutr. Biochem. 2020, 85, 108459. [Google Scholar] [CrossRef] [PubMed]
- Yosaee, S.; Keshtkaran, Z.; Abdollahi, S.; Shidfar, F.; Sarris, J.; Soltani, S. The effect of vitamin C supplementation on mood status in adults: A systematic review and meta-analysis of randomized controlled clinical trials. Gen. Hosp. Psychiatry 2021, 71, 36–42. [Google Scholar] [CrossRef] [PubMed]
- Jafarnejad, S.; Boccardi, V.; Hosseini, B.; Taghizadeh, M.; Hamedifard, Z. A meta-analysis of randomized control trials: The impact of vitamin C supplementation on serum CRP and serum hs-CRP concentrations. Curr. Pharm. Des. 2018, 24, 3520–3528. [Google Scholar] [CrossRef]
- Ellulu, M.S.; Rahmat, A.; Patimah, I.; Khaza’ai, H.; Abed, Y. Effect of vitamin C on inflammation and metabolic markers in hypertensive and/or diabetic obese adults: A randomized controlled trial. Drug. Des. Devel. Ther. 2015, 9, 3405–3412. [Google Scholar] [CrossRef] [PubMed]
- Leonard, B.; Maes, M. Mechanistic explanations how cell-mediated immune activation, inflammation and oxidative and nitrosative stress pathways and their sequels and concomitants play a role in the pathophysiology of unipolar depression. Neurosci. Biobehav. Rev. 2012, 36, 764–785. [Google Scholar] [CrossRef]
- Bradley, H.A.; Campbell, S.A.; Mulder, R.T.; Henderson, J.M.T.; Dixon, L.; Boden, J.M.; Rucklidge, J.J. Can broad-spectrum multinutrients treat symptoms of antenatal depression and anxiety and improve infant development? Study protocol of a double blind, randomized, controlled trial (the ‘NUTRIMUM’ trial). BMC Pregnancy Childbirth 2020, 20, 488. [Google Scholar] [CrossRef]
- Popper, C.W. Single-micronutrient and broad-spectrum micronutrient approaches for treating mood disorders in youth and adults. Child. Adolesc. Psychiatr. Clin. N. Am. 2014, 23, 591–672. [Google Scholar] [CrossRef] [PubMed]
- Bailey, R.L.; Miller, P.E.; Mitchell, D.C.; Hartman, T.J.; Lawrence, F.R.; Sempos, C.T.; Smiciklas-Wright, H. Dietary screening tool identifies nutritional risk in older adults. Am. J. Clin. Nutr. 2009, 90, 177–183. [Google Scholar] [CrossRef]
- Cox, J.L.; Holden, J.M.; Sagovsky, R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br. J. Psychiatry 1987, 150, 782–786. [Google Scholar] [CrossRef]
- Berk, M.; Ng, F.; Dodd, S.; Callaly, T.; Campbell, S.; Bernardo, M.; Trauer, T. The validity of the CGI severity and improvement scales as measures of clinical effectiveness suitable for routine clinical use. J. Eval. Clin. Pract. 2008, 14, 979–983. [Google Scholar] [CrossRef]
- Williams, J.B.; Kobak, K.A. Development and reliability of a structured interview guide for the Montgomery Asberg Depression Rating Scale (SIGMA). Br. J. Psychiatry 2008, 192, 52–58. [Google Scholar] [CrossRef] [PubMed]
- Lovibond, P.F.; Lovibond, S.H. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav. Res. Ther. 1995, 33, 335–343. [Google Scholar] [CrossRef]
- Lovibond, S.H.; Lovibond, P.F. Manual for the Depression Anxiety Stress Scales, 2nd ed.; Psychology Foundation: Sydney, Australia, 1995. [Google Scholar]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.; Löwe, B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef]
- Pullar, J.M.; Bayer, S.; Carr, A.C. Appropriate handling, processing and analysis of blood samples is essential to avoid oxidation of vitamin C to dehydroascorbic acid. Antioxidants 2018, 7, 29. [Google Scholar] [CrossRef] [PubMed]
- Carr, A.C.; Pullar, J.M.; Moran, S.; Vissers, M.C. Bioavailability of vitamin C from kiwifruit in non-smoking males: Determination of ‘healthy’ and ‘optimal’ intakes. J. Nutr. Sci. 2012, 1, e14. [Google Scholar] [CrossRef] [PubMed]
- Zhou, X.; Fragala, M.S.; McElhaney, J.E.; Kuchel, G.A. Conceptual and methodological issues relevant to cytokine and inflammatory marker measurements in clinical research. Curr. Opin. Clin. Nutr. Metab. Care 2010, 13, 541–547. [Google Scholar] [CrossRef] [PubMed]
- Rowe, S.; Carr, A.C. Global vitamin C status and prevalence of deficiency: A cause for concern? Nutrients 2020, 12, 2008. [Google Scholar] [CrossRef]
- Carr, A.C.; Rowe, S. Factors affecting vitamin C status and prevalence of deficiency: A global health perspective. Nutrients 2020, 12, 1963. [Google Scholar] [CrossRef] [PubMed]
- Carr, A.C.; Block, G.; Lykkesfeldt, J. Estimation of vitamin C intake requirements based on body weight: Implications for obesity. Nutrients 2022, 14, 1460. [Google Scholar] [CrossRef]
- Moya-Alvarez, V.; Koyembi, J.J.; Kayé, L.M.; Mbecko, J.R.; Sanke-Waîgana, H.; Djorie, S.G.; Nyasenu, Y.T.; Mad-Bondo, D.; Kongoma, J.B.; Nakib, S.; et al. Vitamin C levels in a Central-African mother-infant cohort: Does hypovitaminosis C increase the risk of enteric infections? Matern. Child. Nutr. 2021, 17, e13215. [Google Scholar] [CrossRef] [PubMed]
- Coker, S.J.; Smith-Díaz, C.C.; Dyson, R.M.; Vissers, M.C.M.; Berry, M.J. The epigenetic role of vitamin C in neurodevelopment. Int. J. Mol. Sci. 2022, 23, 1208. [Google Scholar] [CrossRef]
- Rumbold, A.; Ota, E.; Nagata, C.; Shahrook, S.; Crowther, C.A. Vitamin C supplementation in pregnancy. Cochrane Database Syst. Rev. 2015, 2015, Cd004072. [Google Scholar] [CrossRef]
- Zhang, C.; Williams, M.A.; King, I.B.; Dashow, E.E.; Sorensen, T.K.; Frederick, I.O.; Thompson, M.L.; Luthy, D.A. Vitamin C and the risk of preeclampsia—Results from dietary questionnaire and plasma assay. Epidemiology 2002, 13, 409–416. [Google Scholar] [CrossRef]
- Carr, A.C.; Lykkesfeldt, J. Discrepancies in global vitamin C recommendations: A review of RDA criteria and underlying health perspectives. Crit. Rev. Food Sci. Nutr. 2021, 61, 742–755. [Google Scholar] [CrossRef]
- Smith Fawzi, M.C.; Kaaya, S.F.; Mbwambo, J.; Msamanga, G.I.; Antelman, G.; Wei, R.; Hunter, D.J.; Fawzi, W.W. Multivitamin supplementation in HIV-positive pregnant women: Impact on depression and quality of life in a resource-poor setting. HIV Med. 2007, 8, 203–212. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, K.F.; Cunha, D.F.; Weffort, V.R. Analysis of serum and supplemented vitamin C and oxidative stress in HIV-infected children and adolescents. J. Pediatr. (Rio J.) 2011, 87, 517–522. [Google Scholar] [CrossRef] [PubMed]
- Rucklidge, J.J.; Bradley, H.A.; Campbell, S.; Heaton, J.L.; Mulder, R.T.; Henderson, J.; Dixon, L.; Moltchanova, E. Vitamins and minerals treat antenatal depression and improve birth and infant development: Results of the double-blind NutriMum RCT [Abstract]. J. Am. Acad. Child. Adolesc. Psychiatry 2022, 61, S283. [Google Scholar] [CrossRef]
- Bornstein, S.R.; Yoshida-Hiroi, M.; Sotiriou, S.; Levine, M.; Hartwig, H.G.; Nussbaum, R.L.; Eisenhofer, G. Impaired adrenal catecholamine system function in mice with deficiency of the ascorbic acid transporter (SVCT2). FASEB J. 2003, 17, 1928–1930. [Google Scholar] [CrossRef]
- Padayatty, S.J.; Doppman, J.L.; Chang, R.; Wang, Y.; Gill, J.; Papanicolaou, D.A.; Levine, M. Human adrenal glands secrete vitamin C in response to adrenocorticotrophic hormone. Am. J. Clin. Nutr. 2007, 86, 145–149. [Google Scholar] [CrossRef] [PubMed]
- Hooper, M.H.; Carr, A.; Marik, P.E. The adrenal-vitamin C axis: From fish to guinea pigs and primates. Crit. Care 2019, 23, 29. [Google Scholar] [CrossRef] [PubMed]
- Marik, P.E. Vitamin C: An essential “stress hormone” during sepsis. J. Thorac. Dis. 2020, 12, S84–S88. [Google Scholar] [CrossRef] [PubMed]
- Simon, L.; Gauvin, F.; Amre, D.K.; Saint-Louis, P.; Lacroix, J. Serum procalcitonin and C-reactive protein levels as markers of bacterial infection: A systematic review and meta-analysis. Clin. Infect. Dis. 2004, 39, 206–217. [Google Scholar] [CrossRef] [PubMed]



| Characteristics | Baseline | Week 12 |
|---|---|---|
| Age, years | 32 (27, 35) | |
| Ethnicity: | ||
| NZ European | 48 (79) | |
| Māori/Pasifika | 6 (10) | |
| Asian/Other | 7 (11) | |
| Household income: | ||
| Low (0–40 K) | 11 (18) | |
| Mid (40–80 K) | 20 (33) | |
| High (80+ K) | 30 (49) | |
| Relationship status: | ||
| Single | 7 (11) | |
| Married | 32 (52) | |
| Defacto | 22 (36) | |
| EPDS | 15 (14, 18) | |
| Gestation, weeks | 17 (15, 22) | 30 (27, 33) |
| Weight, kg | 73 (62, 88) | 78 (68, 90) |
| Systolic BP, mmHg | 117 (105, 124) | 116 (108, 126) |
| Diastolic BP, mmHg | 77 (72, 83) | 84 (79, 88) |
| Diet quality 1 | 65 (59, 71) | 68 (60, 71) |
| Placebo (n = 21) | Intervention (n = 20) | |||
|---|---|---|---|---|
| Inflammatory Markers | Baseline | Week 12 | Baseline | Week 12 |
| CRP (mg/L) | 4.2 (1.8, 6.1) | 2.6 (1.2, 5.9) | 5.0 (2.4, 8.7) | 5.1 (1.3, 7.1) |
| IL-6 (ng/L) | 2.3 (0.7, 4.1) | 3.5 (0.5, 5.0) | 2.2. (0.8, 2.5) | 3.5 (0.8, 5.2) |
| TNF-α (ng/L) | 0 (0, 19) | 0.4 (0, 11) | 1.6 (0, 18) | 2.1 (0, 18) |
| IL-10 (ng/L) | 1.5 (0.8, 2.9) | 2.2 (1.2, 2.8) | 1.6 (1.0, 2.5) | 1.6 (1.0, 3.2) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Carr, A.C.; Bradley, H.A.; Vlasiuk, E.; Pierard, H.; Beddow, J.; Rucklidge, J.J. Inflammation and Vitamin C in Women with Prenatal Depression and Anxiety: Effect of Multinutrient Supplementation. Antioxidants 2023, 12, 941. https://doi.org/10.3390/antiox12040941
Carr AC, Bradley HA, Vlasiuk E, Pierard H, Beddow J, Rucklidge JJ. Inflammation and Vitamin C in Women with Prenatal Depression and Anxiety: Effect of Multinutrient Supplementation. Antioxidants. 2023; 12(4):941. https://doi.org/10.3390/antiox12040941
Chicago/Turabian StyleCarr, Anitra C., Hayley A. Bradley, Emma Vlasiuk, Hayley Pierard, Jessica Beddow, and Julia J. Rucklidge. 2023. "Inflammation and Vitamin C in Women with Prenatal Depression and Anxiety: Effect of Multinutrient Supplementation" Antioxidants 12, no. 4: 941. https://doi.org/10.3390/antiox12040941
APA StyleCarr, A. C., Bradley, H. A., Vlasiuk, E., Pierard, H., Beddow, J., & Rucklidge, J. J. (2023). Inflammation and Vitamin C in Women with Prenatal Depression and Anxiety: Effect of Multinutrient Supplementation. Antioxidants, 12(4), 941. https://doi.org/10.3390/antiox12040941








