The Importance of Natural Antioxidants in Female Reproduction
Abstract
1. Introduction: Infertility Nowadays
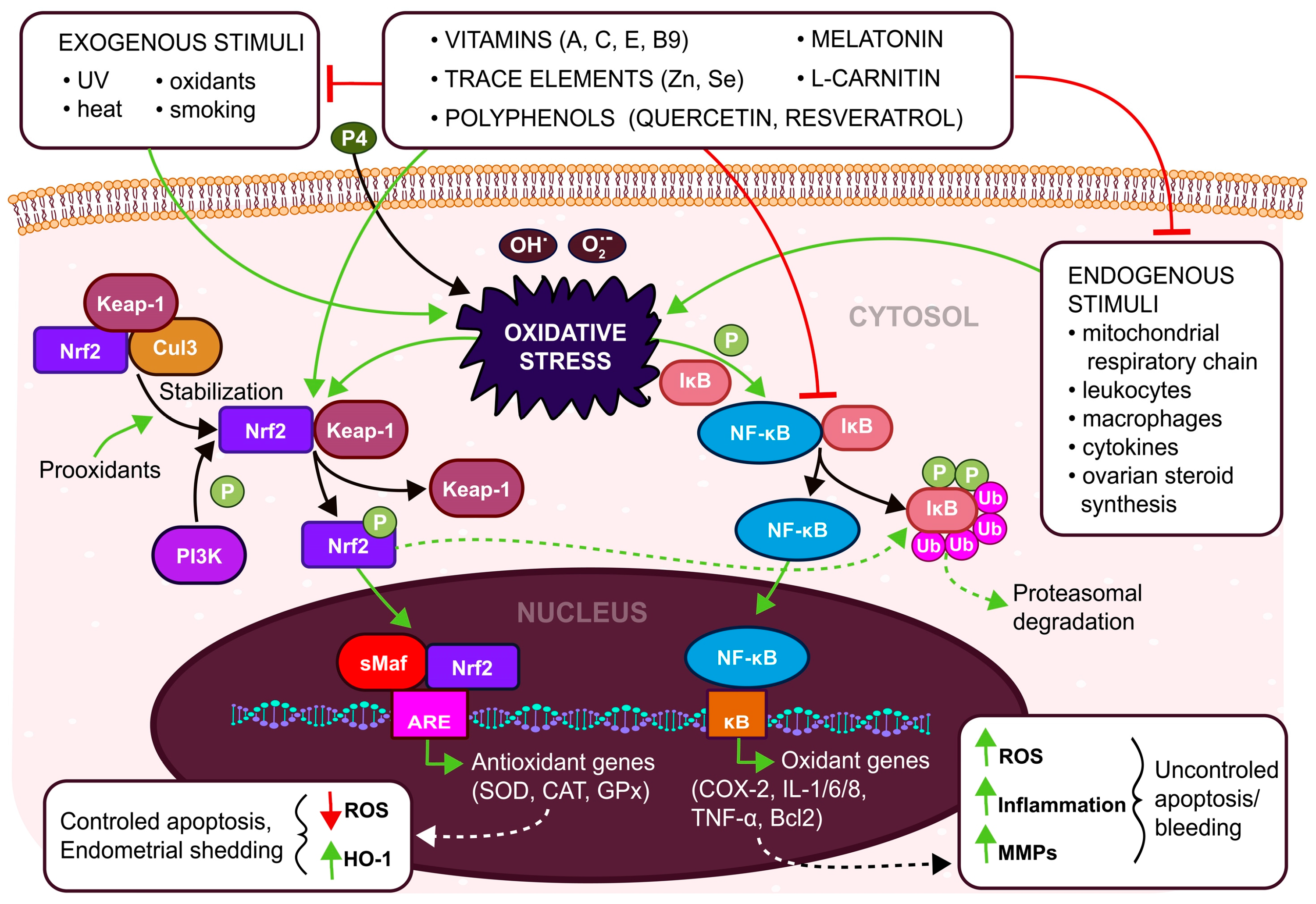
2. Female Reproduction Regulated by Reactive Oxygen and Nitrogen Species
3. Antioxidant Systems in Female Reproduction
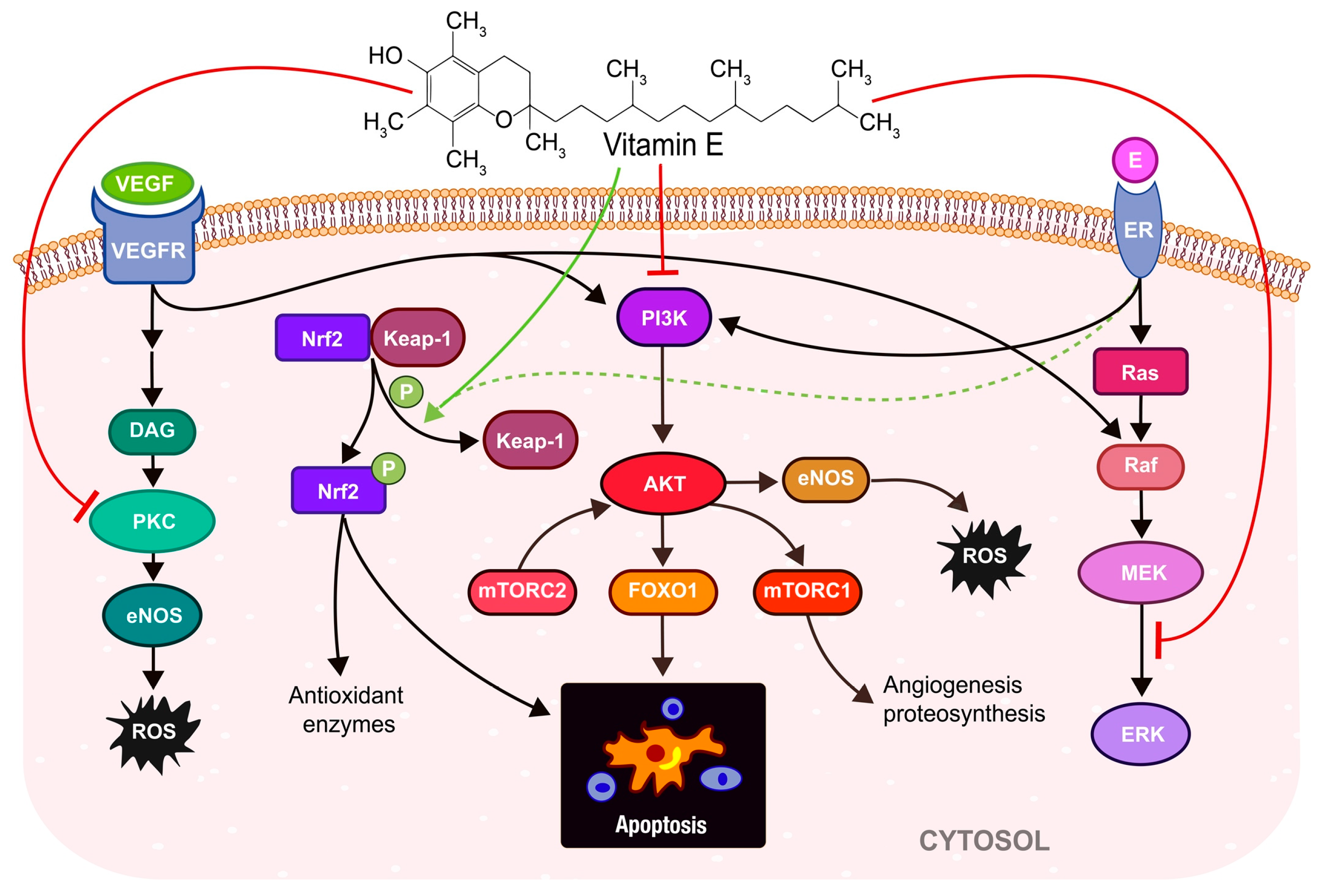
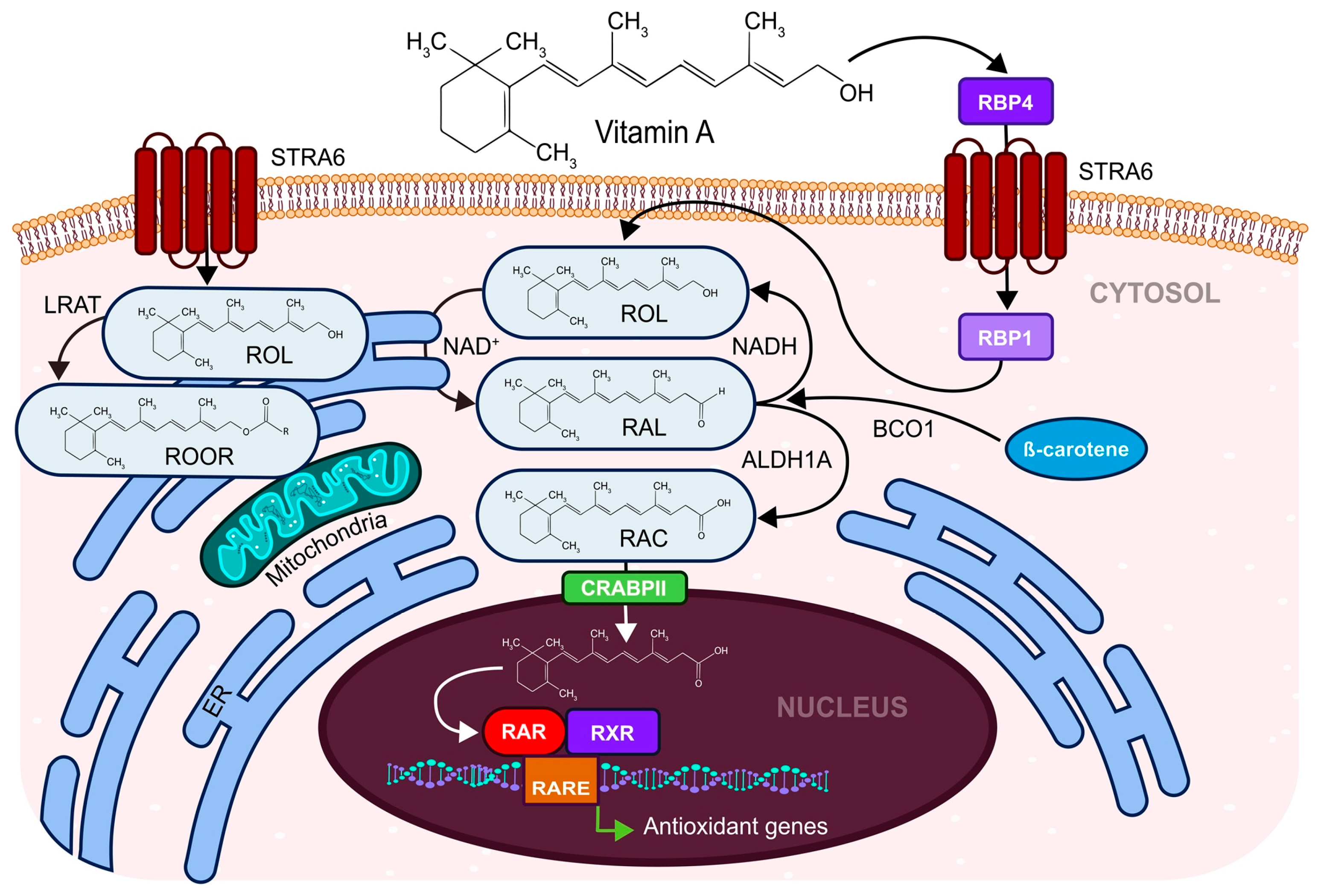
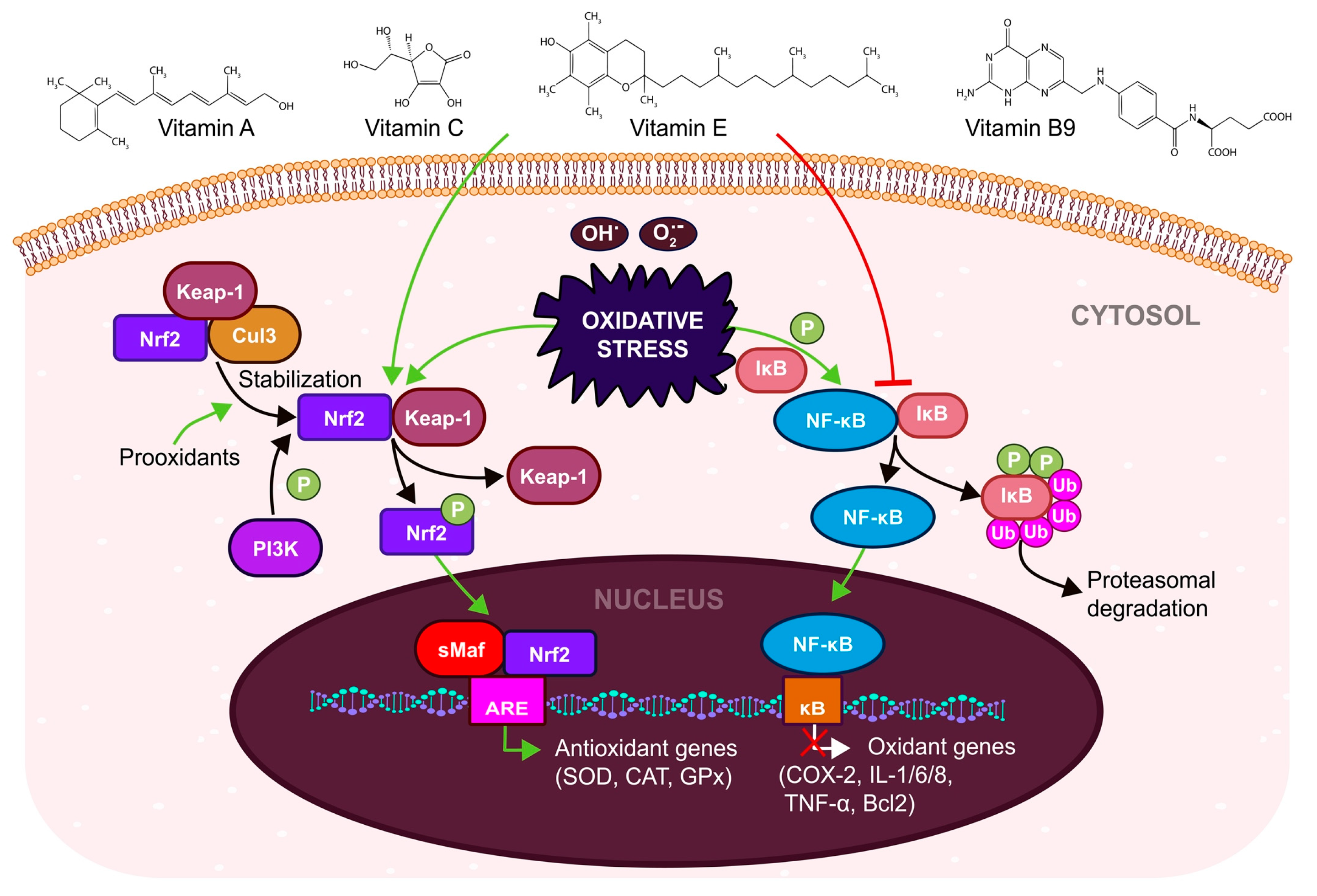
3.1. Carotenoids, Ascorbic Acid, Tocopherol, and Folic Acid Affect the Female Reproductive System
3.2. L-carnitine Ensures the Physiological Need for ATP in Women’s Reproduction Processes
3.3. Melatonin Affects the Normal Hormonal Development and Functioning of the Female Reproductive Organs
3.4. Polyphenols—Quercetin and Resveratrol Have a Dual Function in the OS of the Female Reproductive System
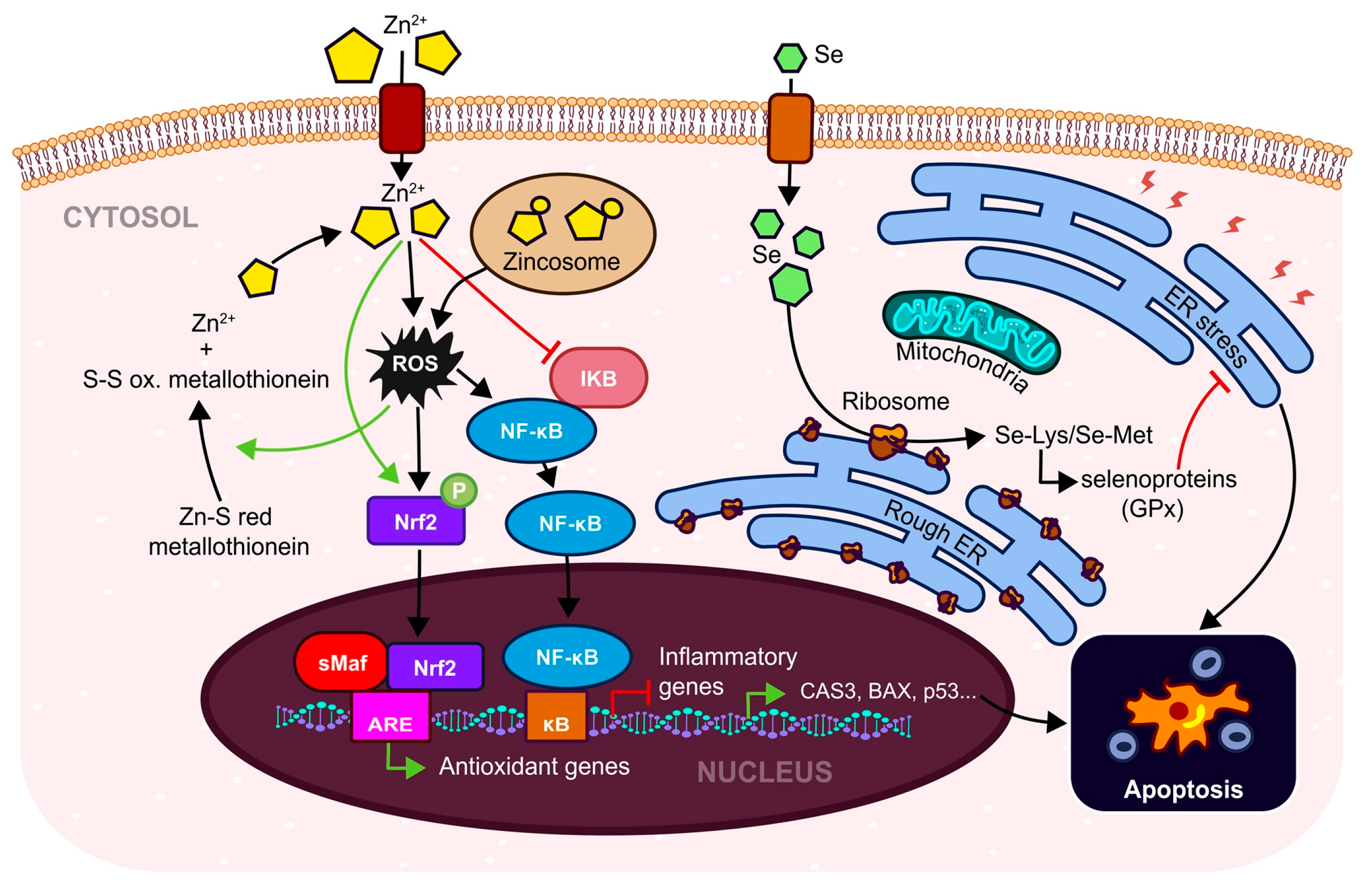
3.5. Trace Elements—Zinc and Selenium and Their Fertility Effects
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sharma, R.; Biedenharn, K.R.; Fedor, J.M.; Agarwal, A. Lifestyle Factors and Reproductive Health: Taking Control of Your Fertility. Reprod. Biol. Endocrinol. 2013, 11, 66. [Google Scholar] [CrossRef]
- Vander Borght, M.; Wyns, C. Fertility and Infertility: Definition and Epidemiology. Clin. Biochem. 2018, 62, 2–10. [Google Scholar] [CrossRef]
- Hsu, L.-C.; Tsui, K.-H.; Wei, J.C.-C.; Yip, H.-T.; Hung, Y.-M.; Chang, R. Female Human Papillomavirus Infection Associated with Increased Risk of Infertility: A Nationwide Population-Based Cohort Study. Int. J. Environ. Res. Public Health 2020, 17, 6505. [Google Scholar] [CrossRef]
- Boivin, J.; Bunting, L.; Collins, J.A.; Nygren, K.G. International Estimates of Infertility Prevalence and Treatment-Seeking: Potential Need and Demand for Infertility Medical Care. Hum. Reprod. 2007, 22, 2800. [Google Scholar] [CrossRef]
- Ombelet, W. WHO fact sheet on infertility gives hope to milions of infertile couples worldwide. Facts Views Vis. Obgyn 2020, 4, 249–251. [Google Scholar]
- Nik Hazlina, N.H.; Norhayati, M.N.; Shaiful Bahari, I.; Nik Muhammad Arif, N.A. Worldwide prevalence, risk factors and psychological impact of infertility among women: A systematic review and meta-analysis. BMJ Open 2022, 12, e057132. [Google Scholar] [CrossRef]
- Cheng, H.; Luo, W.; Si, S.; Xin, X.; Peng, Z.; Zhou, H.; Liu, H.; Yu, Y. Global trends in total fertility rate and its relation to national wealth, life expectancy and female education. BMC Public Health 2022, 22, 1346. [Google Scholar] [CrossRef]
- Beaujouan, E. Latest-Late Fertility? Decline and Resurgence of Late Parenthood Across the Low-Fertility Countries. Popul. Dev. Rev. 2020, 46, 219–247. [Google Scholar] [CrossRef] [PubMed]
- Hodgson, R.M.; Lee, H.L.; Wang, R.; Mol, B.W.; Johnson, N. Interventions for endometriosis-related infertility: A systematic review and network meta-analysis. Fertil. Steril. 2020, 113, 374–382.e2. [Google Scholar] [CrossRef]
- Zaninovic, N.; Rosenwaks, Z. Artificial Intelligence in Human in Vitro Fertilization and Embryology. Fertil. Steril. 2020, 114, 914–920. [Google Scholar] [CrossRef] [PubMed]
- Toporcerová, S.; Špaková, I.; Šoltys, K.; Klepcová, Z.; Kľoc, M.; Bohošová, J.; Trachtová, K.; Peterová, L.; Mičková, H.; Urdzík, P.; et al. Small Non-Coding RNAs as New Biomarkers to Evaluate the Quality of the Embryo in the IVF Process. Biomolecules 2022, 12, 1687. [Google Scholar] [CrossRef] [PubMed]
- Bashiri, A.; Halper, K.I.; Orvieto, R. Recurrent Implantation Failure-update overview on etiology, diagnosis, treatment and future directions. Reprod. Biol. Endocrinol. 2018, 16, 121. [Google Scholar] [CrossRef]
- Okada, H.; Tsuzuki, T.; Murata, H. Decidualization of the Human Endometrium. Reprod. Med. Biol. 2018, 17, 220–227. [Google Scholar] [CrossRef] [PubMed]
- Shankar, K.; Mehendale, H.M. Oxidative Stress. In Encyclopedia of Toxicology; Elsevier: Amsterdam, The Netherlands, 2014; pp. 735–737. ISBN 978-0-12-386455-0. [Google Scholar]
- Immediata, V.; Ronchetti, C.; Spadaro, D.; Cirillo, F.; Levi-Setti, P.E. Oxidative Stress and Human Ovarian Response-From Somatic Ovarian Cells to Oocytes Damage: A Clinical Comprehensive Narrative Review. Antioxidants 2022, 11, 1335. [Google Scholar] [CrossRef]
- Lu, J.; Wang, Z.; Cao, J.; Chen, Y.; Dong, Y. A Novel and Compact Review on the Role of Oxidative Stress in Female Reproduction. Reprod. Biol. Endocrinol. 2018, 16, 80. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, A.; Gupta, S.; Sharma, R.K. Role of Oxidative Stress in Female Reproduction. Reprod. Biol. Endocrinol. 2005, 3, 28. [Google Scholar] [CrossRef]
- Liu, Y.; Wang, J.; Zhang, X. An Update on the Multifaceted Role of NF-KappaB in Endometriosis. Int. J. Biol. Sci. 2022, 18, 4400–4413. [Google Scholar] [CrossRef] [PubMed]
- Hinz, M.; Scheidereit, C. The IκB Kinase Complex in NF-κB Regulation and Beyond. EMBO Rep. 2014, 15, 46–61. [Google Scholar] [CrossRef]
- Forrester, S.J.; Kikuchi, D.S.; Hernandes, M.S.; Xu, Q.; Griendling, K.K. Reactive Oxygen Species in Metabolic and Inflammatory Signaling. Circ. Res. 2018, 122, 877–902. [Google Scholar] [CrossRef]
- Zdrojkowski, Ł.; Jasiński, T.; Ferreira-Dias, G.; Pawliński, B.; Domino, M. The Role of NF-ΚB in Endometrial Diseases in Humans and Animals: A Review. Int. J. Mol. Sci. 2023, 24, 2901. [Google Scholar] [CrossRef] [PubMed]
- Yun, B.H.; Kim, S.; Chon, S.J.; Kim, G.H.; Choi, Y.S.; Cho, S.; Lee, B.S.; Seo, S.K. High Mobility Group Box-1 Promotes Inflammation in Endometriotic Stromal Cells through Toll-like Receptor 4/Nuclear Factor-Kappa B. Am. J. Transl. Res. 2021, 13, 1400–1410. [Google Scholar]
- Wu, B.; Chen, X.; He, B.; Liu, S.; Li, Y.; Wang, Q.; Gao, H.; Wang, S.; Liu, J.; Zhang, S.; et al. ROS Are Critical for Endometrial Breakdown via NF-ΚB–COX-2 Signaling in a Female Mouse Menstrual-Like Model. Endocrinology 2014, 155, 3638–3648. [Google Scholar] [CrossRef]
- Zhang, D.D.; Lo, S.-C.; Cross, J.V.; Templeton, D.J.; Hannink, M. Keap1 Is a Redox-Regulated Substrate Adaptor Protein for a Cul3-Dependent Ubiquitin Ligase Complex. Mol. Cell. Biol. 2004, 24, 10941–10953. [Google Scholar] [CrossRef]
- Vomhof-DeKrey, E.E.; Picklo, M.J. The Nrf2-Antioxidant Response Element Pathway: A Target for Regulating Energy Metabolism. J. Nutr. Biochem. 2012, 23, 1201–1206. [Google Scholar] [CrossRef] [PubMed]
- Ashino, T.; Yamamoto, M.; Numazawa, S. Nrf2/Keap1 System Regulates Vascular Smooth Muscle Cell Apoptosis for Vascular Homeostasis: Role in Neointimal Formation after Vascular Injury. Sci. Rep. 2016, 6, 26291. [Google Scholar] [CrossRef]
- Kasai, S.; Shimizu, S.; Tatara, Y.; Mimura, J.; Itoh, K. Regulation of Nrf2 by Mitochondrial Reactive Oxygen Species in Physiology and Pathology. Biomolecules 2020, 10, 320. [Google Scholar] [CrossRef]
- Vomund, S.; Schäfer, A.; Parnham, M.; Brüne, B.; von Knethen, A. Nrf2, the Master Regulator of Anti-Oxidative Responses. Int. J. Mol. Sci. 2017, 18, 2772. [Google Scholar] [CrossRef] [PubMed]
- Ma, Q. Role of Nrf2 in Oxidative Stress and Toxicity. Annu. Rev. Pharmacol. Toxicol. 2013, 53, 401–426. [Google Scholar] [CrossRef] [PubMed]
- Aouache, R.; Biquard, L.; Vaiman, D.; Miralles, F. Oxidative Stress in Preeclampsia and Placental Diseases. Int. J. Mol. Sci. 2018, 19, 1496. [Google Scholar] [CrossRef]
- Marques, P.; Skorupskaite, K.; Rozario, K.S.; Anderson, R.A.; George, J.T. Physiology of GnRH and Gonadotropin Secretion. In Endotext; Feingold, K.R., Anawalt, B., Blackman, M.R., Boyce, A., Chrousos, G., Corpas, E., de Herder, W.W., Dhatariya, K., Hofland, J., Dungan, K., et al., Eds.; MDText.com, Inc.: South Dartmouth, MA, USA, 2000. [Google Scholar]
- Mazat, J.-P.; Devin, A.; Ransac, S. Modelling Mitochondrial ROS Production by the Respiratory Chain. Cell. Mol. Life Sci. 2020, 77, 455–465. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Nuevo, A.; Torres-Sanchez, A.; Duran, J.M.; De Guirior, C.; Martínez-Zamora, M.A.; Böke, E. Oocytes Maintain ROS-Free Mitochondrial Metabolism by Suppressing Complex I. Nature 2022, 607, 756–761. [Google Scholar] [CrossRef] [PubMed]
- Couto, N.; Wood, J.; Barber, J. The Role of Glutathione Reductase and Related Enzymes on Cellular Redox Homoeostasis Network. Free Radic. Biol. Med. 2016, 95, 27–42. [Google Scholar] [CrossRef]
- Ambrozova, N.; Ulrichova, J.; Galandakova, A. Models for the Study of Skin Wound Healing. The Role of Nrf2 and NF-ΚB. Biomed. Pap. 2017, 161, 1–13. [Google Scholar] [CrossRef]
- Chen, N.; Du, B.; Zhou, H.; Shen, F.; Li, J.; Xie, Z. Abnormal Expression of Nrf2 May Play an Important Role in the Pathogenesis and Development of Adenomyosis. PLoS ONE 2017, 12, e0182773. [Google Scholar] [CrossRef]
- Aguilar, T.A.F.; Navarro, B.C.H.; Pérez, J.A.M. Endogenous Antioxidants: A Review of Their Role in Oxidative Stress. In A Master Regulator of Oxidative Stress—The Transcription Factor Nrf2; Morales-Gonzalez, J.A., Morales-Gonzalez, A., Madrigal-Santillan, E.O., Eds.; InTech: London, UK, 2016; ISBN 978-953-51-2837-3. [Google Scholar]
- Bouayed, J.; Bohn, T. Exogenous Antioxidants—Double-Edged Swords in Cellular Redox State: Health Beneficial Effects at Physiologic Doses versus Deleterious Effects at High Doses. Oxid. Med. Cell Longev. 2010, 3, 228–237. [Google Scholar] [CrossRef] [PubMed]
- Oh, C.; Keats, E.C.; Bhutta, Z.A. Vitamin and Mineral Supplementation During Pregnancy on Maternal, Birth, Child Health and Development Outcomes in Low- and Middle-Income Countries: A Systematic Review and Meta-Analysis. Nutrients 2020, 12, 491. [Google Scholar] [CrossRef]
- Jouanne, M.; Oddoux, S.; Noël, A.; Voisin-Chiret, A.S. Nutrient Requirements during Pregnancy and Lactation. Nutrients 2021, 13, 692. [Google Scholar] [CrossRef]
- Vitagliano, A.; Petre, G.C.; Francini-Pesenti, F.; De Toni, L.; Di Nisio, A.; Grande, G.; Foresta, C.; Garolla, A. Dietary Supplements for Female Infertility: A Critical Review of Their Composition. Nutrients 2021, 13, 3552. [Google Scholar] [CrossRef] [PubMed]
- Adams, J.B.; Kirby, J.K.; Sorensen, J.C.; Pollard, E.L.; Audhya, T. Evidence Based Recommendations for an Optimal Prenatal Supplement for Women in the US: Vitamins and Related Nutrients. Matern. Health Neonatol. Perinatol. 2022, 8, 4. [Google Scholar] [CrossRef] [PubMed]
- British Journal of Midwifery—Micronutrients and the Use of Vitamin and Mineral Supplements during Pregnancy and Lactation. Available online: https://www.britishjournalofmidwifery.com/content/clinical-practice/micronutrients-and-the-use-of-vitamin-and-mineral-supplements-during-pregnancy-and-lactation (accessed on 20 February 2023).
- Kakani, V.; Nguyen, V.H.; Kumar, B.P.; Kim, H.; Pasupuleti, V.R. A Critical Review on Computer Vision and Artificial Intelligence in Food Industry. J. Agric. Food Res. 2020, 2, 100033. [Google Scholar] [CrossRef]
- Tuncalp, Ö.; Rogers, L.M.; Lawrie, T.A.; Barreix, M.; Peña-Rosas, J.P.; Bucagu, M.; Neilson, J.; Oladapo, O.T. WHO Recommendations on Antenatal Nutrition: An Update on Multiple Micronutrient Supplements. BMJ Glob. Health 2020, 5, e003375. [Google Scholar] [CrossRef]
- Lewis, E.D.; Meydani, S.N.; Wu, D. Regulatory Role of Vitamin E in the Immune System and Inflammation. IUBMB Life 2019, 71, 487–494. [Google Scholar] [CrossRef] [PubMed]
- Partearroyo, T.; Samaniego-Vaesken, M.D.L.; Ruiz, E.; Olza, J.; Aranceta-Bartrina, J.; Gil, Á.; González-Gross, M.; Ortega, R.M.; Serra-Majem, L.; Varela-Moreiras, G. Dietary Sources and Intakes of Folates and Vitamin B12 in the Spanish Population: Findings from the ANIBES Study. PLoS ONE 2017, 12, e0189230. [Google Scholar] [CrossRef] [PubMed]
- Shalaby, A. Antioxidant Compounds, Assays of Determination and Mode of Action. Afr. J. Pharm. Pharmacol. 2013, 7, 528–539. [Google Scholar] [CrossRef]
- Grieger, J.A.; Grzeskowiak, L.E.; Wilson, R.L.; Bianco-Miotto, T.; Leemaqz, S.Y.; Jankovic-Karasoulos, T.; Perkins, A.V.; Norman, R.J.; Dekker, G.A.; Roberts, C.T. Maternal Selenium, Copper and Zinc Concentrations in Early Pregnancy, and the Association with Fertility. Nutrients 2019, 11, 1609. [Google Scholar] [CrossRef]
- Hu, W.; Zhao, C.; Hu, H.; Yin, S. Food Sources of Selenium and Its Relationship with Chronic Diseases. Nutrients 2021, 13, 1739. [Google Scholar] [CrossRef]
- Garner, T.B.; Hester, J.M.; Carothers, A.; Diaz, F.J. Role of Zinc in Female Reproduction. Biol. Reprod. 2021, 104, 976–994. [Google Scholar] [CrossRef]
- Keller, U.; van der Wal, C.; Seliger, G.; Scheler, C.; Röpke, F.; Eder, K. Carnitine Status of Pregnant Women: Effect of Carnitine Supplementation and Correlation between Iron Status and Plasma Carnitine Concentration. Eur. J. Clin. Nutr. 2009, 63, 1098–1105. [Google Scholar] [CrossRef][Green Version]
- Carnitine—Health Professional Fact Sheet. Available online: https://ods.od.nih.gov/factsheets/Carnitine-HealthProfessional (accessed on 27 February 2023).
- Budani, M.C.; Tiboni, G.M. Effects of Supplementation with Natural Antioxidants on Oocytes and Preimplantation Embryos. Antioxidants 2020, 9, 612. [Google Scholar] [CrossRef]
- Geier, D.A.; Geier, M.R. L-Carnitine Exposure and Mitochondrial Function in Human Neuronal Cells. Neurochem. Res. 2013, 38, 2336–2341. [Google Scholar] [CrossRef]
- Espino, J.; Macedo, M.; Lozano, G.; Ortiz, Á.; Rodríguez, C.; Rodríguez, A.B.; Bejarano, I. Impact of Melatonin Supplementation in Women with Unexplained Infertility Undergoing Fertility Treatment. Antioxidants 2019, 8, 338. [Google Scholar] [CrossRef] [PubMed]
- Batıoğlu, A.S.; Sahin, U.; Gürlek, B.; Oztürk, N.; Unsal, E. The Efficacy of Melatonin Administration on Oocyte Quality. Gynecol. Endocrinol. Off. J. Int. Soc. Gynecol. Endocrinol. 2012, 28, 91–93. [Google Scholar] [CrossRef] [PubMed]
- Wdowiak, A.; Filip, M. The Effect of Myo-Inositol, Vitamin D3 and Melatonin on the Oocyte Quality and Pregnancy in in Vitro Fertilization: A Randomized Prospective Controlled Trial. Eur. Rev. Med. Pharmacol. Sci. 2020, 24, 8529–8536. [Google Scholar] [CrossRef] [PubMed]
- Fernando, S.; Biggs, S.N.; Horne, R.S.C.; Vollenhoven, B.; Lolatgis, N.; Hope, N.; Wong, M.; Lawrence, M.; Lawrence, A.; Russell, C.; et al. The Impact of Melatonin on the Sleep Patterns of Women Undergoing IVF: A Double Blind RCT. Hum. Reprod. Open 2018, 2017, hox027. [Google Scholar] [CrossRef]
- Kopustinskiene, D.M.; Bernatoniene, J. Molecular Mechanisms of Melatonin-Mediated Cell Protection and Signaling in Health and Disease. Pharmaceutics 2021, 13, 129. [Google Scholar] [CrossRef] [PubMed]
- Targhazeh, N.; Reiter, R.J.; Rahimi, M.; Qujeq, D.; Yousefi, T.; Shahavi, M.H.; Mir, S.M. Oncostatic Activities of Melatonin: Roles in Cell Cycle, Apoptosis, and Autophagy. Biochimie 2022, 202, 34–48. [Google Scholar] [CrossRef]
- Shahzad, H.; Giribabu, N.; Muniandy, S.; Salleh, N. Quercetin Induces Morphological and Proliferative Changes of Rat’s Uteri under Estrogen and Progesterone Influences. Int. J. Clin. Exp. Pathol. 2014, 7, 5484–5494. [Google Scholar]
- Ożarowski, M.; Mikołajczak, P.Ł.; Kujawski, R.; Wielgus, K.; Klejewski, A.; Wolski, H.; Seremak-Mrozikiewicz, A. Pharmacological Effect of Quercetin in Hypertension and Its Potential Application in Pregnancy-Induced Hypertension: Review of In Vitro, In Vivo, and Clinical Studies. Evid. Based Complement Altern. Med. 2018, 2018, 7421489. [Google Scholar] [CrossRef] [PubMed]
- Showell, M.G.; Mackenzie-Proctor, R.; Jordan, V.; Hart, R.J. Antioxidants for Female Subfertility. Cochrane Database Syst. Rev. 2020, 2020. [Google Scholar] [CrossRef]
- Costa, P.C.T.D.; de Souza, E.L.; Lacerda, D.C.; Cruz Neto, J.P.R.; de Sales, L.C.S.; Silva Luis, C.C.; Pontes, P.B.; Cavalcanti Neto, M.P.; de Brito Alves, J.L. Evidence for Quercetin as a Dietary Supplement for the Treatment of Cardio-Metabolic Diseases in Pregnancy: A Review in Rodent Models. Foods 2022, 11, 2772. [Google Scholar] [CrossRef]
- Kim, J.K.; Park, S.U. Quercetin and Its Role in Biological Functions: An Updated Review. EXCLI J. 2018, 17, 856. [Google Scholar] [CrossRef]
- Qiu, D.; Yan, X.; Xiao, X.; Zhang, G.; Wang, Y.; Cao, J.; Ma, R.; Hong, S.; Ma, M. To Explore Immune Synergistic Function of Quercetin in Inhibiting Breast Cancer Cells. Cancer Cell Int. 2021, 21, 632. [Google Scholar] [CrossRef] [PubMed]
- How Does Resveratrol Support Fertility?—Bird&Be. Available online: https://birdandbe.com/blogs/the-nest/how-does-resveratrol-support-fertility (accessed on 27 February 2023).
- Malaguarnera Influence of Resveratrol on the Immune Response. Nutrients 2019, 11, 946. [CrossRef] [PubMed]
- Alesci, A.; Nicosia, N.; Fumia, A.; Giorgianni, F.; Santini, A.; Cicero, N. Resveratrol and Immune Cells: A Link to Improve Human Health. Molecules 2022, 27, 424. [Google Scholar] [CrossRef] [PubMed]
- Flieger, J.; Flieger, W.; Baj, J.; Maciejewski, R. Antioxidants: Classification, Natural Sources, Activity/Capacity Measurements, and Usefulness for the Synthesis of Nanoparticles. Materials 2021, 14, 4135. [Google Scholar] [CrossRef]
- Mumford, S.L.; Browne, R.W.; Schliep, K.C.; Schmelzer, J.; Plowden, T.C.; Michels, K.A.; Sjaarda, L.A.; Zarek, S.M.; Perkins, N.J.; Messer, L.C.; et al. Serum Antioxidants Are Associated with Serum Reproductive Hormones and Ovulation among Healthy Women. J. Nutr. 2016, 146, 98–106. [Google Scholar] [CrossRef]
- Edwards, G.; Olson, C.G.; Euritt, C.P.; Koulen, P. Molecular Mechanisms Underlying the Therapeutic Role of Vitamin E in Age-Related Macular Degeneration. Front. Neurosci. 2022, 16, 890021. [Google Scholar] [CrossRef]
- Niki, E.; Abe, K. CHAPTER 1. Vitamin E: Structure, Properties and Functions. In Food Chemistry, Function and Analysis; Niki, E., Ed.; Royal Society of Chemistry: Cambridge, UK, 2019; pp. 1–11. ISBN 978-1-78801-240-9. [Google Scholar]
- Hashemi, Z.; Sharifi, N.; Khani, B.; Aghadavod, E.; Asemi, Z. The Effects of Vitamin E Supplementation on Endometrial Thickness, and Gene Expression of Vascular Endothelial Growth Factor and Inflammatory Cytokines among Women with Implantation Failure. J. Matern.-Fetal Neonatal Med. 2019, 32, 95–102. [Google Scholar] [CrossRef]
- Asbaghi, O.; Sadeghian, M.; Nazarian, B.; Sarreshtedari, M.; Mozaffari-Khosravi, H.; Maleki, V.; Alizadeh, M.; Shokri, A.; Sadeghi, O. The Effect of Vitamin E Supplementation on Selected Inflammatory Biomarkers in Adults: A Systematic Review and Meta-Analysis of Randomized Clinical Trials. Sci. Rep. 2020, 10, 17234. [Google Scholar] [CrossRef]
- Shirazi, S.; Pourghassem Gargari, B.; Izadi, A.; Taghizadeh, S.; Parizad, M. Effect of Vitamin E on Serum Levels of Vascular Endothelial Growth Factor and Angiopoietin-1 in Women with Polycystic Ovary Syndrome: A Pilot Randomized, Placebo-Controlled Trial. Int. J. Fertil. Steril. 2021, 15, 44. [Google Scholar] [CrossRef]
- Akram, N.A.; Shafiq, F.; Ashraf, M. Ascorbic Acid-A Potential Oxidant Scavenger and Its Role in Plant Development and Abiotic Stress Tolerance. Front. Plant Sci. 2017, 8, 613. [Google Scholar] [CrossRef]
- Abdollahifar, M.-A.; Azad, N.; Sajadi, E.; Shams Mofarahe, Z.; Zare, F.; Moradi, A.; Rezaee, F.; Gholamin, M.; Abdi, S. Vitamin C Restores Ovarian Follicular Reservation in a Mouse Model of Aging. Anat. Cell Biol. 2019, 52, 196. [Google Scholar] [CrossRef] [PubMed]
- Ansary, J.; Cianciosi, D. Natural Antioxidants: Is the Research Going in the Right Direction? Mediterr. J. Nutr. Metab. 2020, 13, 187–191. [Google Scholar] [CrossRef]
- Henmi, H.; Endo, T.; Kitajima, Y.; Manase, K.; Hata, H.; Kudo, R. Effects of Ascorbic Acid Supplementation on Serum Progesterone Levels in Patients with a Luteal Phase Defect. Fertil. Steril. 2003, 80, 459–461. [Google Scholar] [CrossRef] [PubMed]
- Yang, M.; Teng, S.; Ma, C.; Yu, Y.; Wang, P.; Yi, C. Ascorbic Acid Inhibits Senescence in Mesenchymal Stem Cells through ROS and AKT/MTOR Signaling. Cytotechnology 2018, 70, 1301–1313. [Google Scholar] [CrossRef] [PubMed]
- Saygin, M.; Ozmen, O.; Erol, O.; Ellidag, H.Y.; Ilhan, I.; Aslankoc, R. The Impact of Electromagnetic Radiation (2.45 GHz, Wi-Fi) on the Female Reproductive System: The Role of Vitamin C. Toxicol. Ind. Health 2018, 34, 620–630. [Google Scholar] [CrossRef]
- Kaźmierczak-Barańska, J.; Boguszewska, K.; Adamus-Grabicka, A.; Karwowski, B.T. Two Faces of Vitamin C—Antioxidative and Pro-Oxidative Agent. Nutrients 2020, 12, 1501. [Google Scholar] [CrossRef]
- Villar, J.; Merialdi, M.; Gülmezoglu, A.M.; Abalos, E.; Carroli, G.; Kulier, R.; de Onis, M. Nutritional Interventions during Pregnancy for the Prevention or Treatment of Maternal Morbidity and Preterm Delivery: An Overview of Randomized Controlled Trials. J. Nutr. 2003, 133, S1606–S1625. [Google Scholar] [CrossRef]
- Santanam, N.; Kavtaradze, N.; Murphy, A.; Dominguez, C.; Parthasarathy, S. Antioxidant Supplementation Reduces Endometriosis-Related Pelvic Pain in Humans. Transl. Res. 2013, 161, 189–195. [Google Scholar] [CrossRef]
- Amini, L.; Chekini, R.; Nateghi, M.R.; Haghani, H.; Jamialahmadi, T.; Sathyapalan, T.; Sahebkar, A. The Effect of Combined Vitamin C and Vitamin E Supplementation on Oxidative Stress Markers in Women with Endometriosis: A Randomized, Triple-Blind Placebo-Controlled Clinical Trial. Pain Res. Manag. 2021, 2021, 5529741. [Google Scholar] [CrossRef]
- Fiedor, J.; Burda, K. Potential Role of Carotenoids as Antioxidants in Human Health and Disease. Nutrients 2014, 6, 466–488. [Google Scholar] [CrossRef] [PubMed]
- Vašková, J.; Patlevič, P.; Vaško, L.; Kluchová, D. Prenatal Effects of Retinoic Acid on Lumbar Spinal Cord Development and Liver Antioxidants in Rats. Acta Histochem. 2014, 116, 855–862. [Google Scholar] [CrossRef]
- Metzler, M.; Sandell, L. Enzymatic Metabolism of Vitamin A in Developing Vertebrate Embryos. Nutrients 2016, 8, 812. [Google Scholar] [CrossRef]
- Radhika, M.S.; Bhaskaram, P.; Balakrishna, N.; Ramalakshmi, B.A.; Devi, S.; Kumar, B.S. Effects of Vitamin A Deficiency during Pregnancy on Maternal and Child Health. BJOG Int. J. Obstet. Gynaecol. 2002, 109, 689–693. [Google Scholar] [CrossRef] [PubMed]
- Skowrońska, P.; Kunicki, M.; Pastuszek, E.; Konieczna, L.; Bączek, T.; Łukaszuk, K. Follicular Fat-Soluble Vitamins as Markers of Oocyte Competency. Syst. Biol. Reprod. Med. 2020, 66, 112–121. [Google Scholar] [CrossRef]
- Chan, Y.-M.; Bailey, R.; O’Connor, D.L. Folate. Adv. Nutr. 2013, 4, 123–125. [Google Scholar] [CrossRef]
- Abbasi, I.H.R.; Abbasi, F.; Wang, L.; Abd El Hack, M.E.; Swelum, A.A.; Hao, R.; Yao, J.; Cao, Y. Folate Promotes S-Adenosyl Methionine Reactions and the Microbial Methylation Cycle and Boosts Ruminants Production and Reproduction. AMB Express 2018, 8, 65. [Google Scholar] [CrossRef] [PubMed]
- Gliszczynskaswiglo, A. Folates as Antioxidants. Food Chem. 2007, 101, 1480–1483. [Google Scholar] [CrossRef]
- Gaskins, A.J.; Afeiche, M.C.; Wright, D.L.; Toth, T.L.; Williams, P.L.; Gillman, M.W.; Hauser, R.; Chavarro, J.E. Dietary Folate and Reproductive Success among Women Undergoing Assisted Reproduction. Obstet. Gynecol. 2014, 124, 801–809. [Google Scholar] [CrossRef]
- Papaleo, E.; Unfer, V.; Baillargeon, J.-P.; Fusi, F.; Occhi, F.; De Santis, L. Myo-Inositol May Improve Oocyte Quality in Intracytoplasmic Sperm Injection Cycles. A Prospective, Controlled, Randomized Trial. Fertil. Steril. 2009, 91, 1750–1754. [Google Scholar] [CrossRef]
- Boxmeer, J.C.; Macklon, N.S.; Lindemans, J.; Beckers, N.G.M.; Eijkemans, M.J.C.; Laven, J.S.E.; Steegers, E.A.P.; Steegers-Theunissen, R.P.M. IVF Outcomes Are Associated with Biomarkers of the Homocysteine Pathway in Monofollicular Fluid. Hum. Reprod. Oxf. Engl. 2009, 24, 1059–1066. [Google Scholar] [CrossRef]
- Placidi, M.; Di Emidio, G.; Virmani, A.; D’Alfonso, A.; Artini, P.G.; D’Alessandro, A.M.; Tatone, C. Carnitines as Mitochondrial Modulators of Oocyte and Embryo Bioenergetics. Antioxidants 2022, 11, 745. [Google Scholar] [CrossRef] [PubMed]
- Li, J.-L.; Wang, Q.-Y.; Luan, H.-Y.; Kang, Z.-C.; Wang, C.-B. Effects of L-Carnitine against Oxidative Stress in Human Hepatocytes: Involvement of Peroxisome Proliferator-Activated Receptor Alpha. J. Biomed. Sci. 2012, 19, 32. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Liu, L.; Weng, J.; Yin, T.; Yang, J.; Feng, H.L. Biological Roles of l-carnitine in Oocyte and Early Embryo Development. Mol. Reprod. Dev. 2021, 88, 673–685. [Google Scholar] [CrossRef]
- Genazzani, A.D.; Despini, G.; Czyzyk, A.; Podfigurna, A.; Simoncini, T.; Meczekalski, B. Modulatory Effects of l -Carnitine plus l-Acetyl-Carnitine on Neuroendocrine Control of Hypothalamic Functions in Functional Hypothalamic Amenorrhea (FHA). Gynecol. Endocrinol. 2017, 33, 963–967. [Google Scholar] [CrossRef] [PubMed]
- Petrillo, T.; Battipaglia, C.; Virmani, M.A.; Genazzani, A.R.; Genazzani, A.D. Neuroendocrine Effects of Carnitines on Reproductive Impairments. Int. J. Mol. Sci. 2021, 22, 10781. [Google Scholar] [CrossRef] [PubMed]
- Samimi, M.; Pourhanifeh, M.H.; Mehdizadehkashi, A.; Eftekhar, T.; Asemi, Z. The Role of Inflammation, Oxidative Stress, Angiogenesis, and Apoptosis in the Pathophysiology of Endometriosis: Basic Science and New Insights Based on Gene Expression. J. Cell. Physiol. 2019, 234, 19384–19392. [Google Scholar] [CrossRef]
- Dunning, K.R.; Robker, R.L. Promoting Lipid Utilization with L-Carnitine to Improve Oocyte Quality. Anim. Reprod. Sci. 2012, 134, 69–75. [Google Scholar] [CrossRef]
- Várnagy, A.; Bene, J.; Sulyok, E.; Kovács, G.L.; Bódis, J.; Melegh, B. Acylcarnitine Esters Profiling of Serum and Follicular Fluid in Patients Undergoing in Vitro Fertilization. Reprod. Biol. Endocrinol. RBE 2013, 11, 67. [Google Scholar] [CrossRef] [PubMed]
- Mohd Mutalip, S.; Ab-Rahim, S.; Rajikin, M. Vitamin E as an Antioxidant in Female Reproductive Health. Antioxidants 2018, 7, 22. [Google Scholar] [CrossRef]
- Li, Y.; Hung, S.-W.; Zhang, R.; Man, G.C.-W.; Zhang, T.; Chung, J.P.-W.; Fang, L.; Wang, C.-C. Melatonin in Endometriosis: Mechanistic Understanding and Clinical Insight. Nutrients 2022, 14, 4087. [Google Scholar] [CrossRef] [PubMed]
- Grivas, T.B.; Savvidou, O.D. Melatonin the “Light of Night” in Human Biology and Adolescent Idiopathic Scoliosis. Scoliosis 2007, 2, 6. [Google Scholar] [CrossRef] [PubMed]
- Reiter, R.J.; Mayo, J.C.; Tan, D.-X.; Sainz, R.M.; Alatorre-Jimenez, M.; Qin, L. Melatonin as an Antioxidant: Under Promises but over Delivers. J. Pineal Res. 2016, 61, 253–278. [Google Scholar] [CrossRef] [PubMed]
- Tamura, H.; Takasaki, A.; Taketani, T.; Tanabe, M.; Lee, L.; Tamura, I.; Maekawa, R.; Aasada, H.; Yamagata, Y.; Sugino, N. Melatonin and Female Reproduction. J. Obstet. Gynaecol. Res. 2014, 40, 1–11. [Google Scholar] [CrossRef]
- de Almeida Chuffa, L.G.; Lupi, L.A.; Cucielo, M.S.; Silveira, H.S.; Reiter, R.J.; Seiva, F.R.F. Melatonin Promotes Uterine and Placental Health: Potential Molecular Mechanisms. Int. J. Mol. Sci. 2019, 21, 300. [Google Scholar] [CrossRef]
- Zheng, M.; Tong, J.; Li, W.-P.; Chen, Z.-J.; Zhang, C. Melatonin Concentration in Follicular Fluid Is Correlated with Antral Follicle Count (AFC) and in Vitro Fertilization (IVF) Outcomes in Women Undergoing Assisted Reproductive Technology (ART) Procedures. Gynecol. Endocrinol. 2018, 34, 446–450. [Google Scholar] [CrossRef] [PubMed]
- Mojaverrostami, S.; Asghari, N.; Khamisabadi, M.; Heidari Khoei, H. The Role of Melatonin in Polycystic Ovary Syndrome: A Review. Int. J. Reprod. Biomed. IJRM 2019, 17, 865. [Google Scholar] [CrossRef] [PubMed]
- Ding, D.-N.; Xie, L.-Z.; Shen, Y.; Li, J.; Guo, Y.; Fu, Y.; Liu, F.-Y.; Han, F.-J. Insights into the Role of Oxidative Stress in Ovarian Cancer. Oxid. Med. Cell Longev. 2021, 2021, 8388258. [Google Scholar] [CrossRef]
- Carbillon, L. Cell-Free Fetal DNA Fragments and Preeclampsia. Chem. Biol. Interact. 2014, 218, 10–11. [Google Scholar] [CrossRef]
- Wang, L.; Tang, J.; Wang, L.; Tan, F.; Song, H.; Zhou, J.; Li, F. Oxidative Stress in Oocyte Aging and Female Reproduction. J. Cell Physiol. 2021, 236, 7966–7983. [Google Scholar] [CrossRef]
- Kumar, S.; Pandey, A.K. Chemistry and Biological Activities of Flavonoids: An Overview. Sci. World J. 2013, 2013, 162750. [Google Scholar] [CrossRef]
- Guven, H.; Arici, A.; Simsek, O. Flavonoids in Our Foods: A Short Review. J. Basic Clin. Health Sci. 2019, 3, 96–106. [Google Scholar] [CrossRef]
- Jeong, J.-H.; An, J.Y.; Kwon, Y.T.; Rhee, J.G.; Lee, Y.J. Effects of Low Dose Quercetin: Cancer Cell-Specific Inhibition of Cell Cycle Progression. J. Cell Biochem. 2009, 106, 73–82. [Google Scholar] [CrossRef]
- Li, Y.; Yao, J.; Han, C.; Yang, J.; Chaudhry, M.; Wang, S.; Liu, H.; Yin, Y. Quercetin, Inflammation and Immunity. Nutrients 2016, 8, 167. [Google Scholar] [CrossRef] [PubMed]
- Shafabakhsh, R.; Asemi, Z. Quercetin: A Natural Compound for Ovarian Cancer Treatment. J. Ovarian Res. 2019, 12, 55. [Google Scholar] [CrossRef]
- Wang, J.; Zhang, C.; Zhang, J.; Xie, J.; Yang, L.; Xing, Y.; Li, Z. The Effects of Quercetin on Immunity, Antioxidant Indices, and Disease Resistance in Zebrafish (Danio Rerio). Fish Physiol. Biochem. 2020, 46, 759–770. [Google Scholar] [CrossRef] [PubMed]
- Sun, L.; Xu, G.; Dong, Y.; Li, M.; Yang, L.; Lu, W. Quercetin Protects against Lipopolysaccharide-Induced Intestinal Oxidative Stress in Broiler Chickens through Activation of Nrf2 Pathway. Molecules 2020, 25, 1053. [Google Scholar] [CrossRef] [PubMed]
- Zhao, P.; Hu, Z.; Ma, W.; Zang, L.; Tian, Z.; Hou, Q. Quercetin Alleviates Hyperthyroidism-induced Liver Damage via Nrf2 Signaling Pathway. BioFactors 2020, 46, 608–619. [Google Scholar] [CrossRef] [PubMed]
- Ferraz, C.R.; Carvalho, T.T.; Manchope, M.F.; Artero, N.A.; Rasquel-Oliveira, F.S.; Fattori, V.; Casagrande, R.; Verri, W.A. Therapeutic Potential of Flavonoids in Pain and Inflammation: Mechanisms of Action, Pre-Clinical and Clinical Data, and Pharmaceutical Development. Molecules 2020, 25, 762. [Google Scholar] [CrossRef] [PubMed]
- Cao, Y.; Zhao, H.; Wang, Z.; Zhang, C.; Bian, Y.; Liu, X.; Zhang, C.; Zhang, X.; Zhao, Y. Quercetin Promotes in Vitro Maturation of Oocytes from Humans and Aged Mice. Cell Death Dis. 2020, 11, 965. [Google Scholar] [CrossRef]
- Beazley, K.E.; Nurminskaya, M. Effects of Dietary Quercetin on Female Fertility in Mice: Implication of Transglutaminase 2. Reprod. Fertil. Dev. 2016, 28, 974. [Google Scholar] [CrossRef]
- Perrone, D.; Fuggetta, M.P.; Ardito, F.; Cottarelli, A.; De Filippis, A.; Ravagnan, G.; De Maria, S.; Lo Muzio, L. Resveratrol (3,5,4′-Trihydroxystilbene) and Its Properties in Oral Diseases. Exp. Ther. Med. 2017, 14, 3–9. [Google Scholar] [CrossRef]
- Szkudelski, T.; Szkudelska, K. Anti-Diabetic Effects of Resveratrol. Ann. N. Y. Acad. Sci. 2011, 1215, 34–39. [Google Scholar] [CrossRef]
- Vestergaard, M.; Ingmer, H. Antibacterial and Antifungal Properties of Resveratrol. Int. J. Antimicrob. Agents 2019, 53, 716–723. [Google Scholar] [CrossRef] [PubMed]
- Chen, F.-P.; Chien, M.-H. Phytoestrogens Induce Differential Effects on Both Normal and Malignant Human Breast Cells in Vitro. Climacteric J. Int. Menopause Soc. 2014, 17, 682–691. [Google Scholar] [CrossRef] [PubMed]
- Poschner, S.; Maier-Salamon, A.; Thalhammer, T.; Jäger, W. Resveratrol and Other Dietary Polyphenols Are Inhibitors of Estrogen Metabolism in Human Breast Cancer Cells. J. Steroid Biochem. Mol. Biol. 2019, 190, 11–18. [Google Scholar] [CrossRef]
- Dull, A.-M.; Moga, M.A.; Dimienescu, O.G.; Sechel, G.; Burtea, V.; Anastasiu, C.V. Therapeutic Approaches of Resveratrol on Endometriosis via Anti-Inflammatory and Anti-Angiogenic Pathways. Molecules 2019, 24, 667. [Google Scholar] [CrossRef] [PubMed]
- Horgan, X.; Tatum, H.; Brannan, E.; Paull, D.; Rhodes, L. Resveratrol Analogues Surprisingly Effective against Triple-negative Breast Cancer, Independent of ERα. Oncol. Rep. 2019, 41, 3517–3526. [Google Scholar] [CrossRef]
- Nishigaki, A.; Tsubokura, H.; Tsuzuki-Nakao, T.; Okada, H. Hypoxia: Role of SIRT1 and the Protective Effect of Resveratrol in Ovarian Function. Reprod. Med. Biol. 2022, 21, e12428. [Google Scholar] [CrossRef]
- Novakovic, R.; Rajkovic, J.; Gostimirovic, M.; Gojkovic-Bukarica, L.; Radunovic, N. Resveratrol and Reproductive Health. Life 2022, 12, 294. [Google Scholar] [CrossRef]
- Bruner-Tran, K.L.; Osteen, K.G.; Taylor, H.S.; Sokalska, A.; Haines, K.; Duleba, A.J. Resveratrol Inhibits Development of Experimental Endometriosis in Vivo and Reduces Endometrial Stromal Cell Invasiveness In Vitro. Biol. Reprod. 2011, 84, 106–112. [Google Scholar] [CrossRef] [PubMed]
- Ochiai, A.; Kuroda, K. Preconception Resveratrol Intake against Infertility: Friend or Foe? Reprod. Med. Biol. 2020, 19, 107–113. [Google Scholar] [CrossRef]
- Banaszewska, B.; Wrotyńska-Barczyńska, J.; Spaczynski, R.Z.; Pawelczyk, L.; Duleba, A.J. Effects of Resveratrol on Polycystic Ovary Syndrome: A Double-Blind, Randomized, Placebo-Controlled Trial. J. Clin. Endocrinol. Metab. 2016, 101, 4322–4328. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Zhang, M.; Chen, Z.-J.; Du, Y. Resveratrol Promotes the Embryonic Development of Vitrified Mouse Oocytes after in Vitro Fertilization. In Vitro Cell Dev. Biol. Anim. 2018, 54, 430–438. [Google Scholar] [CrossRef] [PubMed]
- Ng, E.; Lind, P.M.; Lindgren, C.; Ingelsson, E.; Mahajan, A.; Morris, A.; Lind, L. Genome-Wide Association Study of Toxic Metals and Trace Elements Reveals Novel Associations. Hum. Mol. Genet. 2015, 24, 4739–4745. [Google Scholar] [CrossRef]
- Nasiadek, M.; Stragierowicz, J.; Klimczak, M.; Kilanowicz, A. The Role of Zinc in Selected Female Reproductive System Disorders. Nutrients 2020, 12, 2464. [Google Scholar] [CrossRef] [PubMed]
- Dring, J.C.; Forma, A.; Chilimoniuk, Z.; Dobosz, M.; Teresiński, G.; Buszewicz, G.; Flieger, J.; Cywka, T.; Januszewski, J.; Baj, J. Essentiality of Trace Elements in Pregnancy, Fertility, and Gynecologic Cancers—A State-of-the-Art Review. Nutrients 2021, 14, 185. [Google Scholar] [CrossRef]
- Ota, E.; Mori, R.; Middleton, P.; Tobe-Gai, R.; Mahomed, K.; Miyazaki, C.; Bhutta, Z.A. Zinc Supplementation for Improving Pregnancy and Infant Outcome. Cochrane Database Syst. Rev. 2015. [Google Scholar] [CrossRef] [PubMed]
- Maret, W. Zinc Biochemistry: From a Single Zinc Enzyme to a Key Element of Life. Adv. Nutr. 2013, 4, 82–91. [Google Scholar] [CrossRef]
- Maret, W.; Krężel, A. Cellular Zinc and Redox Buffering Capacity of Metallothionein/Thionein in Health and Disease. Mol. Med. 2007, 13, 371–375. [Google Scholar] [CrossRef]
- Lee, S.R. Critical Role of Zinc as Either an Antioxidant or a Prooxidant in Cellular Systems. Oxid. Med. Cell Longev. 2018, 2018, 9156285. [Google Scholar] [CrossRef] [PubMed]
- Jarosz, M.; Olbert, M.; Wyszogrodzka, G.; Młyniec, K.; Librowski, T. Antioxidant and Anti-Inflammatory Effects of Zinc. Zinc-Dependent NF-ΚB Signaling. Inflammopharmacology 2017, 25, 11–24. [Google Scholar] [CrossRef] [PubMed]
- Lu, X.; Zhang, Q.; Xu, L.; Lin, X.; Fu, J.; Wang, X.; Liu, Y.; Lin, Y.; Li, B.; Wang, R.; et al. Zinc Is Essential for the Transcription Function of the PGC-1α/Nrf2 Signaling Pathway in Human Primary Endometrial Stromal Cells. Am. J. Physiol.-Cell Physiol. 2020, 318, C640–C648. [Google Scholar] [CrossRef]
- Lewandowski, Ł.; Kepinska, M.; Milnerowicz, H. The Copper-Zinc Superoxide Dismutase Activity in Selected Diseases. Eur. J. Clin. Investig. 2019, 49, e13036. [Google Scholar] [CrossRef]
- Wang, S.; He, G.; Chen, M.; Zuo, T.; Xu, W.; Liu, X. The Role of Antioxidant Enzymes in the Ovaries. Oxid. Med. Cell Longev. 2017, 2017, 4371714. [Google Scholar] [CrossRef]
- Hisamatsu, Y.; Murata, H.; Tsubokura, H.; Hashimoto, Y.; Kitada, M.; Tanaka, S.; Okada, H. Matrix Metalloproteinases in Human Decidualized Endometrial Stromal Cells. Curr. Issues Mol. Biol. 2021, 43, 2111–2123. [Google Scholar] [CrossRef]
- Rabajdová, M.; Špaková, I.; Klepcová, Z.; Smolko, L.; Abrahamovská, M.; Urdzík, P.; Mareková, M. Zinc(II) Niflumato Complex Effects on MMP Activity and Gene Expression in Human Endometrial Cell Lines. Sci. Rep. 2021, 11, 19086. [Google Scholar] [CrossRef]
- Supasai, S.; Aimo, L.; Adamo, A.M.; Mackenzie, G.G.; Oteiza, P.I. Zinc Deficiency Affects the STAT1/3 Signaling Pathways in Part through Redox-Mediated Mechanisms. Redox Biol. 2017, 11, 469–481. [Google Scholar] [CrossRef] [PubMed]
- Willekens, J.; Runnels, L.W. Impact of Zinc Transport Mechanisms on Embryonic and Brain Development. Nutrients 2022, 14, 2526. [Google Scholar] [CrossRef]
- Zong, L.; Wei, X.; Gou, W.; Huang, P.; Lv, Y. Zinc Improves Learning and Memory Abilities of Fetal Growth Restriction Rats and Promotes Trophoblast Cell Invasion and Migration via Enhancing STAT3-MMP-2/9 Axis Activity. Oncotarget 2017, 8, 115190–115201. [Google Scholar] [CrossRef]
- Roman, M.; Jitaru, P.; Barbante, C. Selenium Biochemistry and Its Role for Human Health. Metallomics 2014, 6, 25–54. [Google Scholar] [CrossRef] [PubMed]
- Tapiero, H.; Townsend, D.M.; Tew, K.D. The Antioxidant Role of Selenium and Seleno-Compounds. Biomed. Pharmacother. 2003, 57, 134–144. [Google Scholar] [CrossRef] [PubMed]
- Zoidis, E.; Seremelis, I.; Kontopoulos, N.; Danezis, G. Selenium-Dependent Antioxidant Enzymes: Actions and Properties of Selenoproteins. Antioxidants 2018, 7, 66. [Google Scholar] [CrossRef]
- Maehira, F.; Miyagi, I.; Eguchi, Y. Selenium Regulates Transcription Factor NF-ΚB Activation during the Acute Phase Reaction. Clin. Chim. Acta 2003, 334, 163–171. [Google Scholar] [CrossRef]
- Nguyen-Ngo, C.; Perkins, A.V.; Lappas, M. Selenium Prevents Inflammation in Human Placenta and Adipose Tissue In Vitro: Implications for Metabolic Diseases of Pregnancy Associated with Inflammation. Nutrients 2022, 14, 3286. [Google Scholar] [CrossRef]
- Xue, H.; Cao, H.; Xing, C.; Feng, J.; Zhang, L.; Zhang, C.; Hu, G.; Yang, F. Selenium Triggers Nrf2-AMPK Crosstalk to Alleviate Cadmium-Induced Autophagy in Rabbit Cerebrum. Toxicology 2021, 459, 152855. [Google Scholar] [CrossRef]
- Qazi, I.; Angel, C.; Yang, H.; Pan, B.; Zoidis, E.; Zeng, C.-J.; Han, H.; Zhou, G.-B. Selenium, Selenoproteins, and Female Reproduction: A Review. Molecules 2018, 23, 3053. [Google Scholar] [CrossRef]
- Hosnedlova, B.; Kepinska, M.; Skalickova, S.; Fernandez, C.; Ruttkay-Nedecky, B.; Malevu, T.D.; Sochor, J.; Baron, M.; Melcova, M.; Zidkova, J.; et al. A Summary of New Findings on the Biological Effects of Selenium in Selected Animal Species—A Critical Review. Int. J. Mol. Sci. 2017, 18, 2209. [Google Scholar] [CrossRef] [PubMed]
- Cengiz, B.; Söylemez, F.; Öztürk, E.; Çavdar, A.O. Serum Zinc, Selenium, Copper, and Lead Levels in Women with Second-Trimester Induced Abortion Resulting from Neural Tube Defects: A Preliminary Study. Biol. Trace Elem. Res. 2004, 97, 225–236. [Google Scholar] [CrossRef]
- Mehdi, Y.; Dufrasne, I. Selenium in Cattle: A Review. Molecules 2016, 21, 545. [Google Scholar] [CrossRef] [PubMed]
- Pieczyńska, J.; Grajeta, H. The Role of Selenium in Human Conception and Pregnancy. J. Trace Elem. Med. Biol. 2015, 29, 31–38. [Google Scholar] [CrossRef]
- Edassery, S.L.; Shatavi, S.V.; Kunkel, J.P.; Hauer, C.; Brucker, C.; Penumatsa, K.; Yu, Y.; Dias, J.A.; Luborsky, J.L. Autoantigens in Ovarian Autoimmunity Associated with Unexplained Infertility and Premature Ovarian Failure. Fertil. Steril. 2010, 94, 2636–2641. [Google Scholar] [CrossRef] [PubMed]
- Wu, S.; Wang, M.; Deng, Y.; Qiu, J.; Zhang, X.; Tan, J. Associations of Toxic and Essential Trace Elements in Serum, Follicular Fluid, and Seminal Plasma with In Vitro Fertilization Outcomes. Ecotoxicol. Environ. Saf. 2020, 204, 110965. [Google Scholar] [CrossRef]
- Khera, A.; Dong, L.; Holland, O.; Vanderlelie, J.; Pasdar, E.A.; Neuzil, J.; Perkins, A.V. Selenium Supplementation Induces Mitochondrial Biogenesis in Trophoblasts. Placenta 2015, 36, 863–869. [Google Scholar] [CrossRef] [PubMed]
- Jiménez Tuñón, J.M.; Trilles, P.P.; Molina, M.G.; Duvison, M.H.; Pastor, B.M.; Martín, P.S.; Martín, F.S.; Sánchez-Borrego, R. A Double-Blind, Randomized Prospective Study to Evaluate the Efficacy of Previous Therapy With Melatonin, Myo-Inositol, Folic Acid, and Selenium in Improving the Results of an Assisted Reproductive Treatment. Clin. Med. Insights Ther. 2017, 9, 1179559X1774290. [Google Scholar] [CrossRef]
- Luddi, A.; Capaldo, A.; Focarelli, R.; Gori, M.; Morgante, G.; Piomboni, P.; De Leo, V. Antioxidants Reduce Oxidative Stress in Follicular Fluid of Aged Women Undergoing IVF. Reprod. Biol. Endocrinol. 2016, 14, 57. [Google Scholar] [CrossRef]
| Example | Adult | Pregnant | In ART | Role | Source |
|---|---|---|---|---|---|
Vitamin A | 0.7–0.77 [39,40] | 0.55–0.77 [40] | 0.6–5.8 [41] | cell differentiation, antioxidant [34] | sweet potato, carrot, tuna, pumpkin, kale |
Vitamin C | 75–85 [39,40] | 70–85 [40,42] | 127–167 [41] | cofactor of oxidases, antioxidant, and wound healing process [43] | guavas, bell pepper, kiwifruit, broccoli, papaya, strawberries |
Vitamin E | 15 [39] | 12–15 [40] | 8.5–11 [41] | antioxidant, modulates signal transduction, cell division, and cell membrane integrity [44] | sunflower seeds, olive oil, almonds, avocado, spinach, butternut squash, kiwifruit |
Vitamin B9 | 0.4–0.6 [39] | 0.4 [45] | 0.2–0.4 [41] | coenzyme in single carbon transferase, aids in the production of nucleic acids [43] | liver, yeast, legumes, pulses, fermented foods, and leafy vegetables [46,47] |
| Selenium | 0.055–0.06 [39] | 0.05–0.06 [48] | ≤0.075 [49] | part of glutathione peroxidases, potent intracellular antioxidant enzymes [43] | Meat, fish, milk, eggs, cruciferous vegetables, liliaceus vegetables, legumes, garlic, onion [50] |
| Zinc | 8–11 [39] | 9.5–11 [40] | ≤18.6 [51] | part of regulatory and catabolic enzymes responsible for signal transduction, gene expression structural role in zinc-finger motifs [43] | oysters, beef, chicken, firm tofu, squash and pumpkin seeds, low-fat yogurt, and lentils |
L-carnitine | 500 [52] | 3000 [53] | 1000 [54] | facilitates long-chain fatty acid entry into cellular mitochondria [55] | sheep meat, beef, pork, fish, chicken, cow’s milk |
Melatonin | approx. 0.5–10 [56,57,58] | 0.3–0.6 [41] | 3–6 [54,59] | antioxidant [60], pro/apoptotic, regulates the uptake of growth factors, increases immunosurveillance, anti-angiogenic [61] | cherries, walnuts, mustard seeds, poppy seeds, corn, rice |
Quercetin | 100–500 [62,63] | 1000 [63] | 1200 [64], 30/kg [65] | antioxidant, anti-inflammatory, antibacterial, antiviral [66], and inhibits cell proliferation [67] | fruits, vegetables, seeds, nuts |
Resveratrol | not specified | avoided [33] | 60–120 [68] | antioxidant, modifies cell morphology, gene expression, ligand-receptor interactions, signaling pathways foam-cell formation [69], and modulates innate and adaptive immunity [70] | skins of grapes, red and white wines, apples, blueberries, peanuts |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vašková, J.; Klepcová, Z.; Špaková, I.; Urdzík, P.; Štofilová, J.; Bertková, I.; Kľoc, M.; Rabajdová, M. The Importance of Natural Antioxidants in Female Reproduction. Antioxidants 2023, 12, 907. https://doi.org/10.3390/antiox12040907
Vašková J, Klepcová Z, Špaková I, Urdzík P, Štofilová J, Bertková I, Kľoc M, Rabajdová M. The Importance of Natural Antioxidants in Female Reproduction. Antioxidants. 2023; 12(4):907. https://doi.org/10.3390/antiox12040907
Chicago/Turabian StyleVašková, Janka, Zuzana Klepcová, Ivana Špaková, Peter Urdzík, Jana Štofilová, Izabela Bertková, Marek Kľoc, and Miroslava Rabajdová. 2023. "The Importance of Natural Antioxidants in Female Reproduction" Antioxidants 12, no. 4: 907. https://doi.org/10.3390/antiox12040907
APA StyleVašková, J., Klepcová, Z., Špaková, I., Urdzík, P., Štofilová, J., Bertková, I., Kľoc, M., & Rabajdová, M. (2023). The Importance of Natural Antioxidants in Female Reproduction. Antioxidants, 12(4), 907. https://doi.org/10.3390/antiox12040907







