Association between Paraoxonase/Arylesterase Activity of Serum PON-1 Enzyme and Rheumatoid Arthritis: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy, Eligibility Criteria, and Study Selection
2.2. Statistical Analysis
3. Results
3.1. Systematic Research
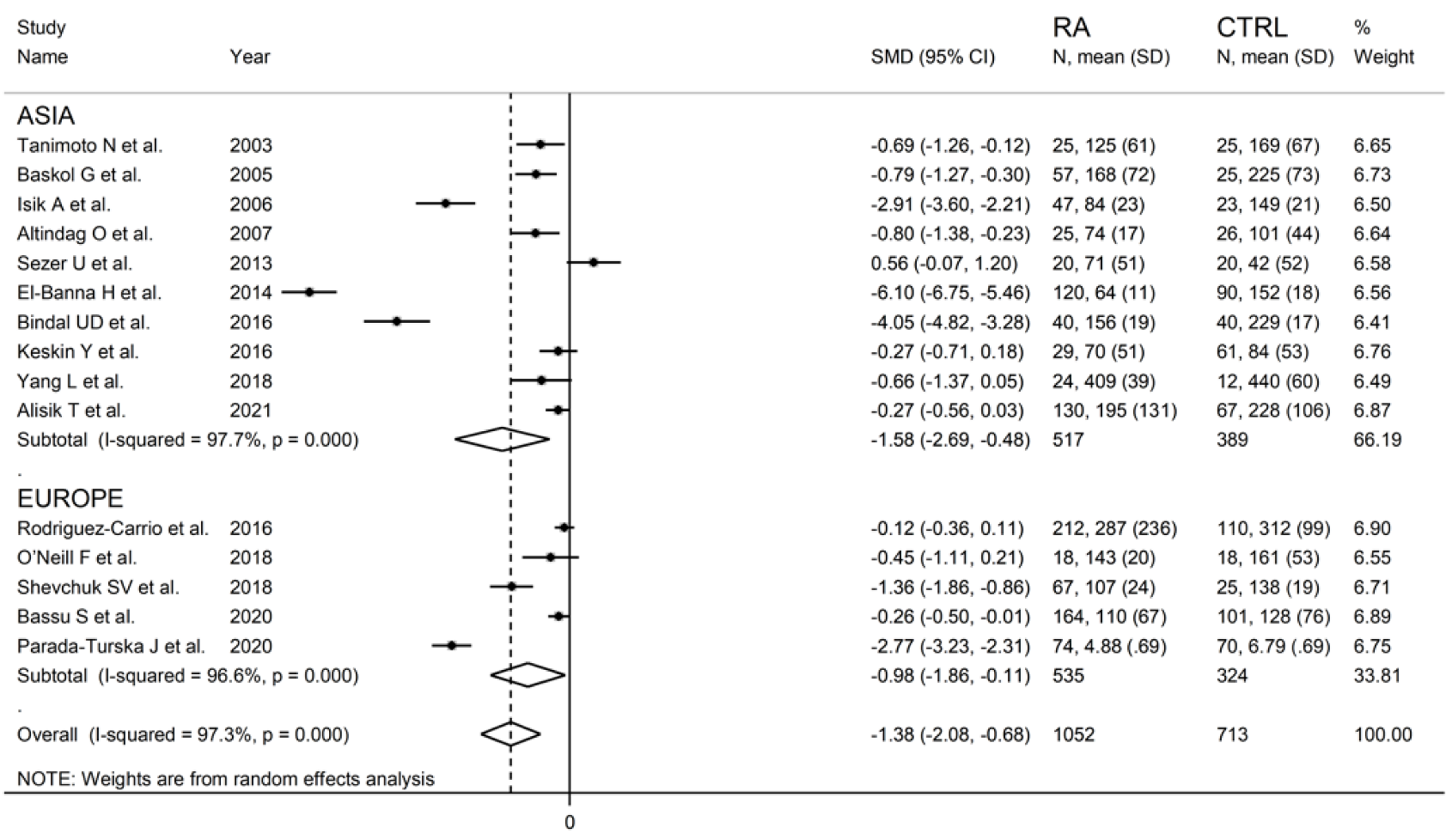
3.2. Meta-Analysis of PON-1 Activity
3.2.1. Study Characteristics
3.2.2. Risk of Bias
3.2.3. Results of Individual Studies and Syntheses
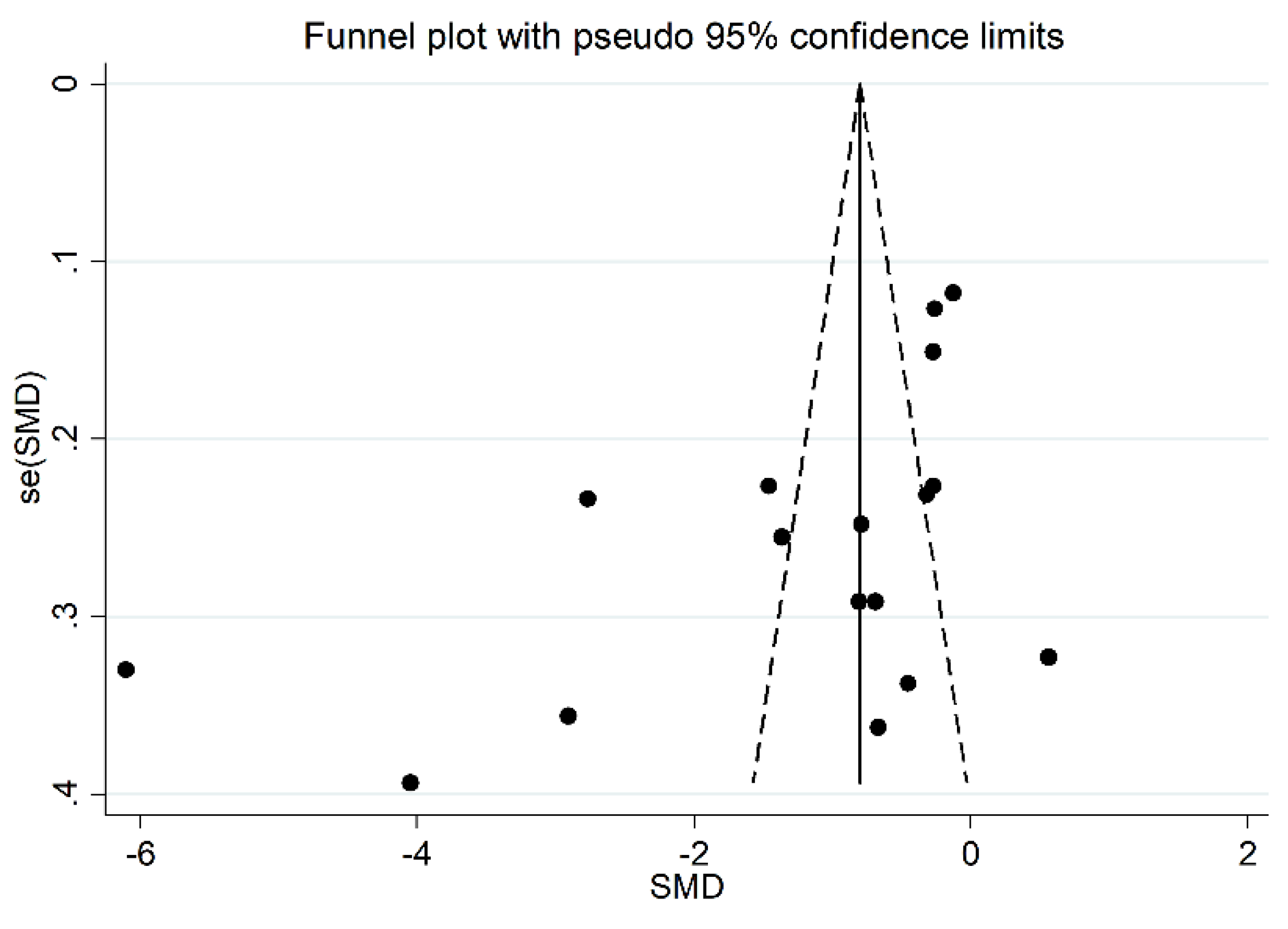
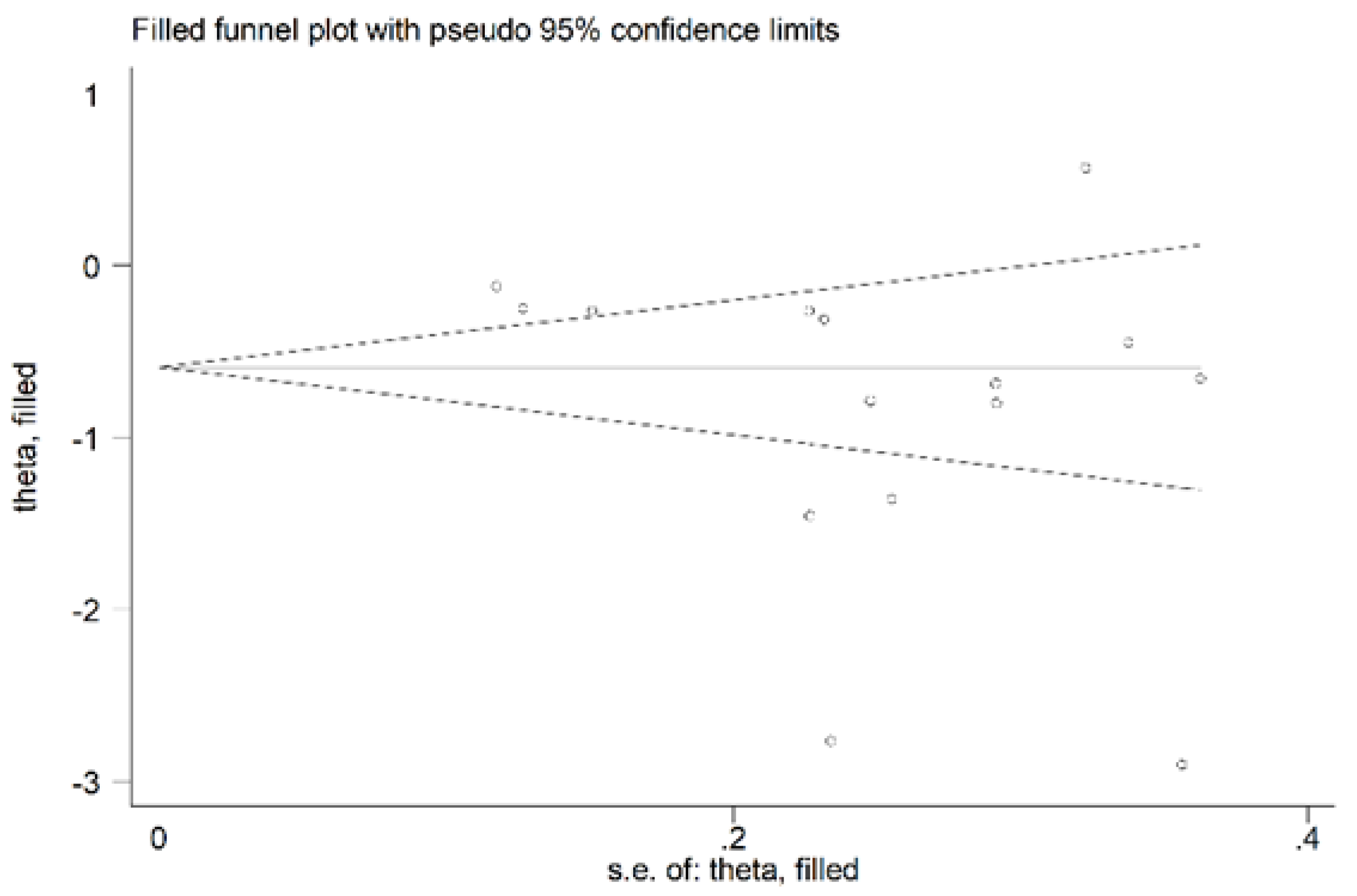
3.2.4. Publication Bias
3.2.5. Meta-Regression and Sub-Group Analysis
3.2.6. Certainty of Evidence
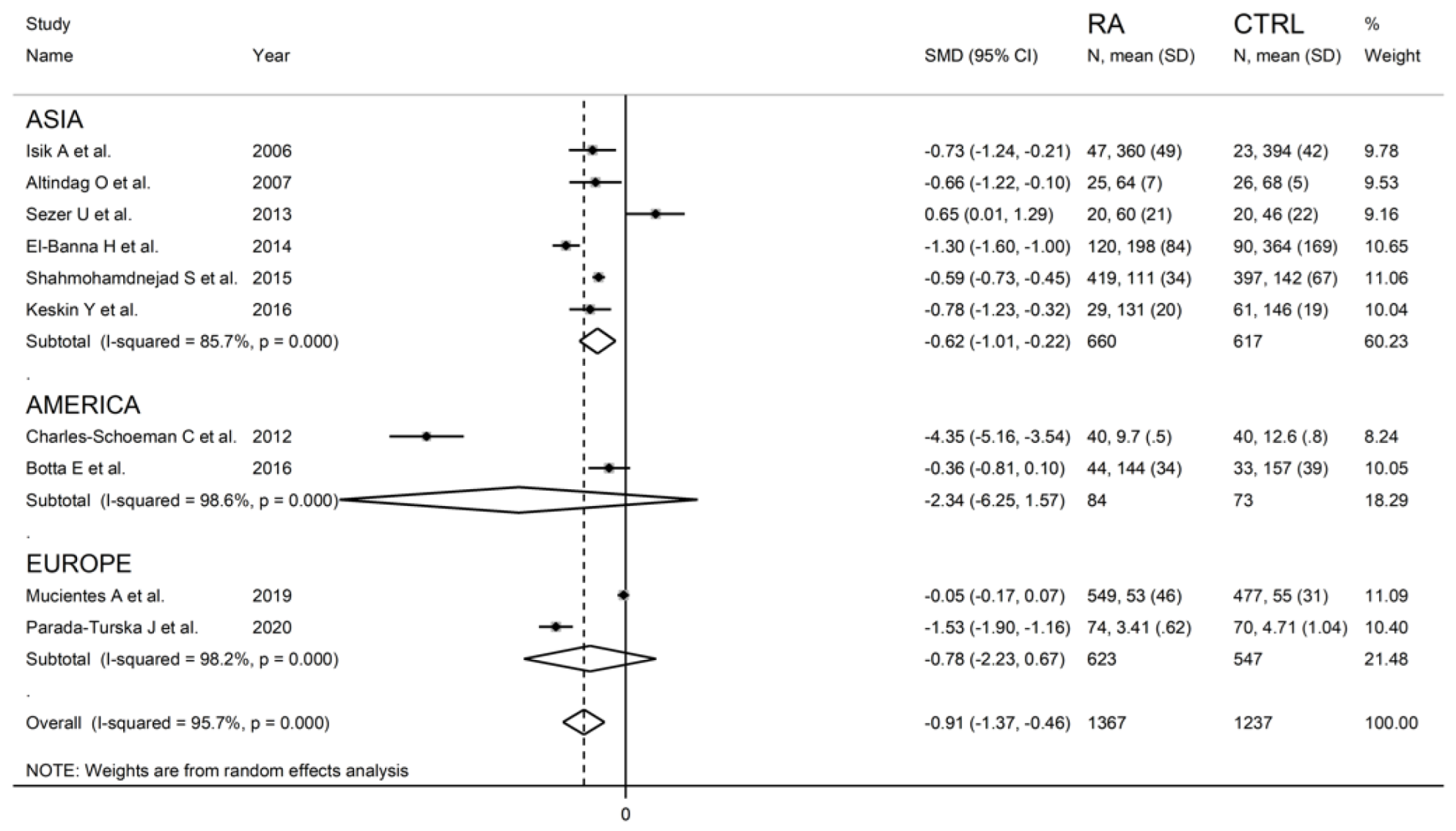
3.3. Meta-Analysis of ARE Activity
3.3.1. Study Characteristics
3.3.2. Risk of Bias
3.3.3. Results of Individual Studies and Syntheses
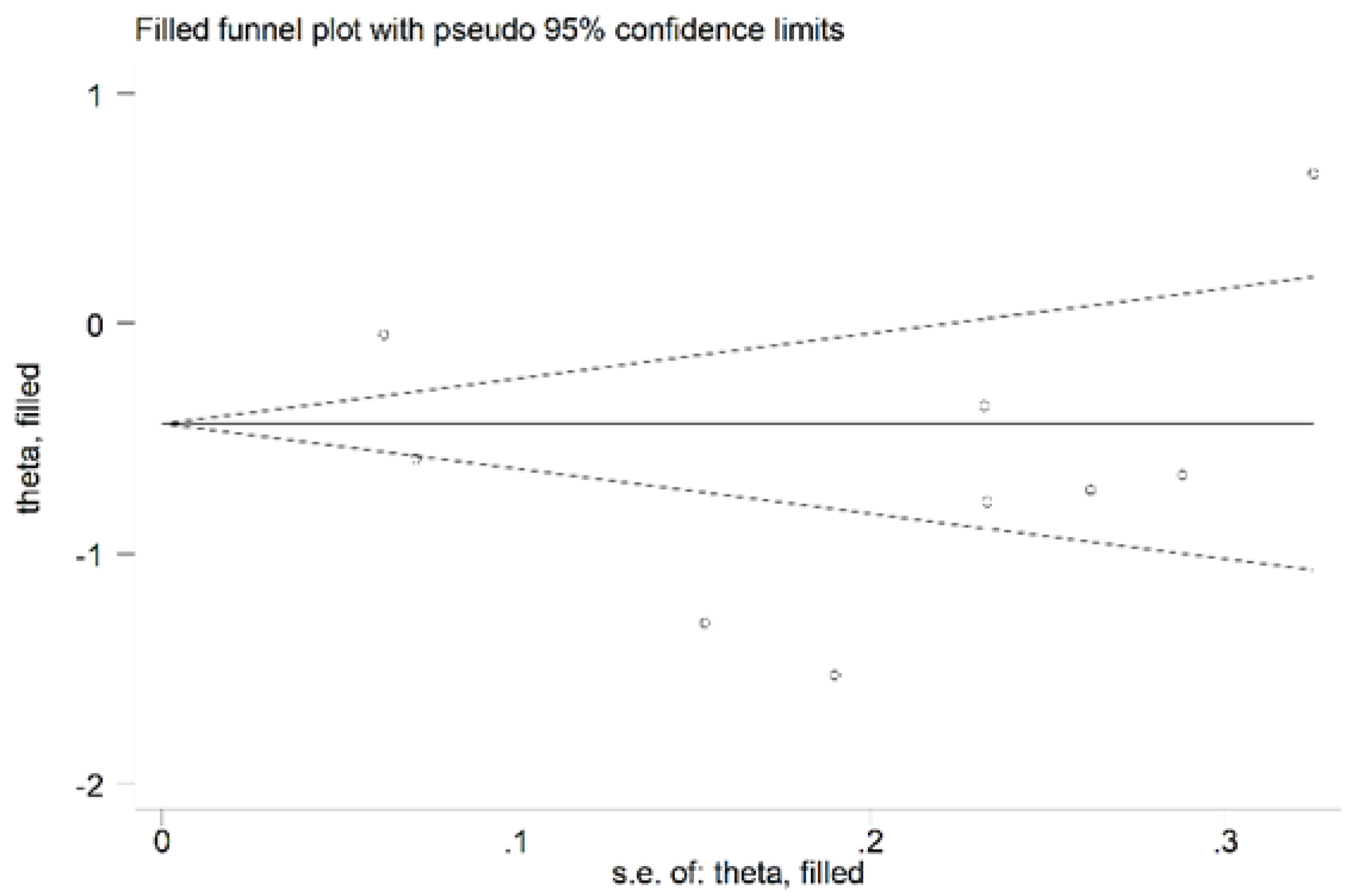
3.3.4. Publication Bias
3.3.5. Meta-Regression and Sub-Group Analysis
3.3.6. Certainty of Evidence
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Smolen, J.S.; Aletaha, D.; Barton, A.; Burmester, G.R.; Emery, P.; Firestein, G.S.; Kavanaugh, A.; McInnes, I.B.; Solomon, D.H.; Strand, V.; et al. Rheumatoid Arthritis. Nat. Rev. Dis. Primer 2018, 4, 18001. [Google Scholar] [CrossRef] [PubMed]
- Cacciapaglia, F.; Spinelli, F.R.; Piga, M.; Erre, G.L.; Sakellariou, G.; Manfredi, A.; Viapiana, O.; Fornaro, M.; Colella, S.; Floris, A.; et al. Estimated 10-Year Cardiovascular Risk in a Large Italian Cohort of Rheumatoid Arthritis Patients: Data from the Cardiovascular Obesity and Rheumatic DISease (CORDIS) Study Group. Eur. J. Intern. Med. 2022, 96, 60–65. [Google Scholar] [CrossRef] [PubMed]
- Erre, G.L.; Cacciapaglia, F.; Sakellariou, G.; Manfredi, A.; Bartoloni, E.; Viapiana, O.; Fornaro, M.; Cauli, A.; Mangoni, A.A.; Woodman, R.J.; et al. C-Reactive Protein and 10-Year Cardiovascular Risk in Rheumatoid Arthritis. Eur. J. Intern. Med. 2022, 104, 49–54. [Google Scholar] [CrossRef] [PubMed]
- Erre, G.L.; Buscetta, G.; Paliogiannis, P.; Mangoni, A.A.; Carru, C.; Passiu, G.; Zinellu, A. Coronary Flow Reserve in Systemic Rheumatic Diseases: A Systematic Review and Meta-Analysis. Rheumatol. Int. 2018, 38, 1179–1190. [Google Scholar] [CrossRef] [PubMed]
- Erre, G.L.; Mangoni, A.A.; Passiu, G.; Bassu, S.; Castagna, F.; Carru, C.; Piga, M.; Zinellu, A.; Sotgia, S. Comprehensive Arginine Metabolomics and Peripheral Vasodilatory Capacity in Rheumatoid Arthritis: A Monocentric Cross-Sectional Study. Microvasc. Res. 2020, 131, 104038. [Google Scholar] [CrossRef] [PubMed]
- Erre, G.L.; Piga, M.; Fedele, A.L.; Mura, S.; Piras, A.; Cadoni, M.L.; Cangemi, I.; Dessi, M.; Di Sante, G.; Tolusso, B.; et al. Prevalence and Determinants of Peripheral Microvascular Endothelial Dysfunction in Rheumatoid Arthritis Patients: A Multicenter Cross-Sectional Study. Mediat. Inflamm. 2018, 2018, 6548715. [Google Scholar] [CrossRef]
- Erre, G.L.; Piras, A.; Mura, S.; Mundula, N.; Piras, M.; Taras, L.; Longu, M.G.; Saba, P.S.; Ganau, A.; Carru, C.; et al. Asymmetric Dimethylarginine and Arterial Stiffness in Patients with Rheumatoid Arthritis: A Case–Control Study. J. Int. Med. Res. 2016, 44, 76–80. [Google Scholar] [CrossRef]
- Erre, G.L.; Piras, A.; Piga, M.; Fedele, A.L.; Mangoni, A.A.; Lazzerini, P.E.; Gremese, E.; Mathieu, A.; Ferraccioli, G.; Passiu, G.; et al. QT and QT Dispersion Intervals in Long-Standing and Moderately Active Rheumatoid Arthritis: Results from a Multicentre Cross-Sectional Study. Clin. Exp. Rheumatol. 2020, 38, 516–522. [Google Scholar]
- Mangoni, A.A.; Woodman, R.J.; Piga, M.; Cauli, A.; Fedele, A.L.; Gremese, E.; Erre, G.L. EDRA Study Group Patterns of Anti-Inflammatory and Immunomodulating Drug Usage and Microvascular Endothelial Function in Rheumatoid Arthritis. Front. Cardiovasc. Med. 2021, 8, 681327. [Google Scholar] [CrossRef]
- Mangoni, A.A.; Tommasi, S.; Sotgia, S.; Zinellu, A.; Paliogiannis, P.; Piga, M.; Cauli, A.; Pintus, G.; Carru, C.; Erre, G.L. Asymmetric Dimethylarginine: A Key Player in the Pathophysiology of Endothelial Dysfunction, Vascular Inflammation and Atherosclerosis in Rheumatoid Arthritis? Curr. Pharm. Des. 2021, 27, 2131–2140. [Google Scholar] [CrossRef]
- Erre, G.L.; Mangoni, A.A.; Castagna, F.; Paliogiannis, P.; Carru, C.; Passiu, G.; Zinellu, A. Meta-Analysis of Asymmetric Dimethylarginine Concentrations in Rheumatic Diseases. Sci. Rep. 2019, 9, 5426. [Google Scholar] [CrossRef]
- Giordo, R.; Thuan, D.T.B.; Posadino, A.M.; Cossu, A.; Zinellu, A.; Erre, G.L.; Pintus, G. Iloprost Attenuates Oxidative Stress-Dependent Activation of Collagen Synthesis Induced by Sera from Scleroderma Patients in Human Pulmonary Microvascular Endothelial Cells. Molecules 2021, 26, 4729. [Google Scholar] [CrossRef]
- Furlong, C.E.; Marsillach, J.; Jarvik, G.P.; Costa, L.G. Paraoxonases-1, -2 and -3: What Are Their Functions? Chem. Biol. Interact. 2016, 259, 51–62. [Google Scholar] [CrossRef]
- Aviram, M.; Rosenblat, M.; Bisgaier, C.L.; Newton, R.S.; Primo-Parmo, S.L.; La Du, B.N. Paraoxonase Inhibits High-Density Lipoprotein Oxidation and Preserves Its Functions: A Possible Peroxidative Role for Paraoxonase. J. Clin. Investig. 1998, 101, 1581–1590. [Google Scholar] [CrossRef]
- Berrougui, H.; Loued, S.; Khalil, A. Purified Human Paraoxonase-1 Interacts with Plasma Membrane Lipid Rafts and Mediates Cholesterol Efflux from Macrophages. Free Radic. Biol. Med. 2012, 52, 1372–1381. [Google Scholar] [CrossRef]
- Kowalska, K.; Socha, E.; Milnerowicz, H. Review: The Role of Paraoxonase in Cardiovascular Diseases. Ann. Clin. Lab. Sci. 2015, 45, 226–233. [Google Scholar]
- Bhattacharyya, T.; Nicholls, S.J.; Topol, E.J.; Zhang, R.; Yang, X.; Schmitt, D.; Fu, X.; Shao, M.; Brennan, D.M.; Ellis, S.G.; et al. Relationship of Paraoxonase 1 (PON1) Gene Polymorphisms and Functional Activity with Systemic Oxidative Stress and Cardiovascular Risk. JAMA-J. Am. Med. Assoc. 2008, 299, 1265–1276. [Google Scholar] [CrossRef]
- Moola, S.; Munn, Z.; Sears, K.; Sfetcu, R.; Currie, M.; Lisy, K.; Tufanaru, C.; Qureshi, R.; Mattis, P.; Mu, P. Conducting Systematic Reviews of Association (Etiology): The Joanna Briggs Institute’s Approach. Int. J. Evid. Based Healthc. 2015, 13, 163–169. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Routledge: London, UK, 2013. [Google Scholar]
- Hultcrantz, M.; Rind, D.; Akl, E.A.; Treweek, S.; Mustafa, R.A.; Iorio, A.; Alper, B.S.; Meerpohl, J.J.; Murad, M.H.; Ansari, M.T. The GRADE Working Group Clarifies the Construct of Certainty of Evidence. J. Clin. Epidemiol. 2017, 87, 4–13. [Google Scholar] [CrossRef]
- Zhang, Y.; Coello, P.A.; Guyatt, G.H.; Yepes-Nuñez, J.J.; Akl, E.A.; Hazlewood, G.; Pardo-Hernandez, H.; Etxeandia-Ikobaltzeta, I.; Qaseem, A.; Williams, J.W.; et al. GRADE Guidelines: 20. Assessing the Certainty of Evidence in the Importance of Outcomes or Values and Preferences-Inconsistency, Imprecision, and Other Domains. J. Clin. Epidemiol. 2019, 111, 83–93. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Hozo, S.P.; Djulbegovic, B.; Hozo, I. Estimating the Mean and Variance from the Median, Range, and the Size of a Sample. BMC Med. Res. Methodol. 2005, 5, 13. [Google Scholar] [CrossRef] [PubMed]
- Deeks, J.J.; Higgins, J.P.; Altman, D.G. Cochrane Statistical Methods Group. Analysing Data and Undertaking Meta-Analyses. Cochrane Handb. Syst. Rev. Interv. 2019, 241–284. [Google Scholar] [CrossRef]
- Tobias, A. Assessing the Influence of a Single Study in the Meta-Anyalysis Estimate. Stata Tech. Bull. 1999, 47, 15–17. [Google Scholar]
- Begg, C.B.; Mazumdar, M. Operating Characteristics of a Rank Correlation Test for Publication Bias. Biometrics 1994, 50, 1088–1101. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.; Egger, M. Funnel Plots for Detecting Bias in Meta-Analysis: Guidelines on Choice of Axis. J. Clin. Epidemiol. 2001, 54, 1046–1055. [Google Scholar] [CrossRef]
- Duval, S.; Tweedie, R. Trim and Fill: A Simple Funnel-Plot-Based Method of Testing and Adjusting for Publication Bias in Meta-Analysis. Biometrics 2000, 56, 455–463. [Google Scholar] [CrossRef]
- Tanimoto, N.; Kumon, Y.; Suehiro, T.; Ohkubo, S.; Ikeda, Y.; Nishiya, K.; Hashimoto, K. Serum Paraoxonase Activity Decreases in Rheumatoid Arthritis. Life Sci. 2003, 72, 2877–2885. [Google Scholar] [CrossRef]
- Baskol, G.; Demir, H.; Baskol, M.; Kilic, E.; Ates, F.; Kocer, D.; Muhtaroglu, S. Assessment of Paraoxonase 1 Activity and Malondialdehyde Levels in Patients with Rheumatoid Arthritis. Clin. Biochem. 2005, 38, 951–955. [Google Scholar] [CrossRef]
- Altindag, Ö.; Karakoç, M.; Soran, N.; Çelik, H.; Çelik, N.; Selek, Ş. Paraoxonase and Arylesterase Activities in Patients with Rheumatoid Arthritis. Rheumatism 2007, 22, 132–136. [Google Scholar]
- Isik, A.; Koca, S.S.; Ustundag, B.; Celik, H.; Yildirim, A. Paraoxonase and Arylesterase Levels in Rheumatoid Arthritis. Clin. Rheumatol. 2007, 26, 342–348. [Google Scholar] [CrossRef]
- Charles-Schoeman, C.; Lee, Y.Y.; Grijalva, V.; Amjadi, S.; FitzGerald, J.; Ranganath, V.K.; Taylor, M.; McMahon, M.; Paulus, H.E.; Reddy, S.T. Cholesterol Efflux by High Density Lipoproteins Is Impaired in Patients with Active Rheumatoid Arthritis. Ann. Rheum. Dis. 2012, 71, 1157–1162. [Google Scholar] [CrossRef]
- Sezer, U.; Erciyas, K.; Üstün, K.; Pehlivan, Y.; Ziya Şenyurt, S.; Aksoy, N.; Tarakçıoğlu, M.; Taysı, S.; Onat, A.M. Effect of Chronic Periodontitis on Oxidative Status in Patients with Rheumatoid Arthritis. J. Periodontol. 2013, 84, 785–792. [Google Scholar] [CrossRef]
- El-Banna, H.; Jiman-Fatani, A. Anti-Cyclic Citrullinated Peptide Antibodies and Paraoxonase-1 Polymorphism in Rheumatoid Arthritis. BMC Musculoskelet. Disord. 2014, 15, 379. [Google Scholar] [CrossRef]
- Shahmohamadnejad, S.; Vaisi-Raygani, A.; Shakiba, Y.; Kiani, A.; Rahimi, Z.; Bahrehmand, F.; Shakiba, E.; Pourmotabbed, T. Association between Butyrylcholinesterase Activity and Phenotypes, Paraoxonase192 Rs662 Gene Polymorphism and Their Enzymatic Activity with Severity of Rheumatoid Arthritis: Correlation with Systemic Inflammatory Markers and Oxidative Stress, Preliminary Report. Clin. Biochem. 2015, 48, 63–69. [Google Scholar] [CrossRef]
- Bindal, U.D.; Saxena, R.; Siddiqui, M.H.; Sharma, D. Correlation of Paraoxonase Status with Disease Activity Score and Systemic Inflammation in Rheumatoid Arthritic Patients. J. Clin. Diagn. Res. 2016, 10, BC01–BC05. [Google Scholar] [CrossRef]
- Keskin, Y.; Aydin, T.; Taspinar, O.; Kepekci, M.; Ozer, O.F.; Selek, S.; Camli, A.; Mutluer, A.S. Assessment of Paroxonase and Aryleserase Antioxidative Parameters in Rheumatic Diseases. Oxid. Commun. 2016, 39, 430–437. [Google Scholar]
- Rodríguez-Carrio, J.; López-Mejías, R.; Alperi-López, M.; López, P.; Ballina-García, F.J.; González-Gay, M.Á.; Suárez, A. Paraoxonase 1 Activity Is Modulated by the Rs662 Polymorphism and IgG Anti-High-Density Lipoprotein Antibodies in Patients with Rheumatoid Arthritis: Potential Implications for Cardiovascular Disease: Modulation of pon-1 activity in Ra. Arthritis Rheumatol. 2016, 68, 1367–1376. [Google Scholar] [CrossRef]
- Botta, E.; Meroño, T.; Saucedo, C.; Martín, M.; Tetzlaff, W.; Sorroche, P.; Boero, L.; Malah, V.; Menafra, M.; Gómez Rosso, L.; et al. Associations between Disease Activity, Markers of HDL Functionality and Arterial Stiffness in Patients with Rheumatoid Arthritis. Atherosclerosis 2016, 251, 438–444. [Google Scholar] [CrossRef]
- O’Neill, F.; Charakida, M.; Topham, E.; McLoughlin, E.; Patel, N.; Sutill, E.; Kay, C.W.M.; D’Aiuto, F.; Landmesser, U.; Taylor, P.C.; et al. Anti-Inflammatory Treatment Improves High-Density Lipoprotein Function in Rheumatoid Arthritis. Heart 2017, 103, 766–773. [Google Scholar] [CrossRef]
- Shevchuk, S.V.; Seheda, Y.S.; Galyutina, O.Y.; Masik, N.P.; Shevchuk, O.V. Serum Paraoxonase Activity in Patients with Rheumatoid Arthritis, Its Relationship with the Clinical Course and Cardiovascular Compications. Regul. Mech. Biosyst. 2018, 9, 90–94. [Google Scholar] [CrossRef]
- Yang, L.; Zou, Q.-H.; Zhang, Y.; Shi, Y.; Hu, C.-R.; Hui, C.-X.; Liu, X.-F.; Fang, Y.-F. Proteomic Analysis of Plasma from Rheumatoid Arthritis Patients with Mild Cognitive Impairment. Clin. Rheumatol. 2018, 37, 1773–1782. [Google Scholar] [CrossRef]
- Mucientes, A.; Fernández-Gutiérrez, B.; Herranz, E.; Rodriguez-Rodriguez, L.; Varadé, J.; Urcelay, E.; Lamas, J.R. Functional Implications of Single Nucleotide Polymorphisms Rs662 and Rs854860 on the Antioxidative Activity of Paraoxonase1 (PON1) in Patients with Rheumatoid Arthritis. Clin. Rheumatol. 2019, 38, 1329–1337. [Google Scholar] [CrossRef] [PubMed]
- Atwa, E.T.; Hussin, A.G.; Mohamed, M.R.; Pasha, H.F.; Hammad, M. Carotid Plaques in Adult Rheumatoid Arthritis Patients; Association with Paroxonase 1 Enzymatic Activity and Q192R Paroxonase 1 Gene Polymorphism. Mol. Biol. Rep. 2020, 47, 4255–4262. [Google Scholar] [CrossRef] [PubMed]
- Bassu, S.; Zinellu, A.; Sotgia, S.; Mangoni, A.A.; Floris, A.; Farina, G.; Passiu, G.; Carru, C.; Erre, G.L. Oxidative Stress Biomarkers and Peripheral Endothelial Dysfunction in Rheumatoid Arthritis: A Monocentric Cross-Sectional Case-Control Study. Molecules 2020, 25, 3855. [Google Scholar] [CrossRef]
- Parada-Turska, J.; Wójcicka, G.; Beltowski, J. Paraoxonase 1 Phenotype and Protein N-Homocysteinylation in Patients with Rheumatoid Arthritis: Implications for Cardiovascular Disease. Antioxidants 2020, 9, 899. [Google Scholar] [CrossRef]
- Alisik, T.; Alisik, M.; Nacir, B.; Ayhan, F.F.; Genc, H.; Erel, O. Evaluation of Dysfunctional High-density Lipoprotein Levels with Myeloperoxidase/Paraoxonase-1 Ratio in Rheumatoid Arthritis. Int. J. Clin. Pract. 2021, 75, e14172. [Google Scholar] [CrossRef]
- Draganov, D.I.; Stetson, P.L.; Watson, C.E.; Billecke, S.S.; La Du, B.N. Rabbit serum paraoxonase 3 PON3 is a high density lipoprotein-associated lactonase and protects low density lipoprotein against oxidation. J. Biol. Chem. 2000, 275, 33435–33442. [Google Scholar] [CrossRef]
- Lu, H.; Zhu, J.; Zang, Y.; Ze, Y.; Qin, J. Cloning, purification, and refolding of human paraoxonase-3 expressed in Escherichia coli and its characterization. Protein Expr. Purif. 2006, 46, 92–99. [Google Scholar] [CrossRef]
- Deakin, S.; Leviev, I.; Gomaraschi, M.; Calabresi, L.; Franceschini, G.; James, R.W. Enzymatically active paraoxonase-1 is located at the external membrane of producing cells and released by a high affinity, saturable, desorption mechanism. J. Biol. Chem. 2002, 277, 4301–4308. [Google Scholar] [CrossRef]
- Marsillach, J.; Mackness, B.; Mackness, M.; Riu, F.; Beltran, R.; Joven, J.; Camps, J. Immunohistochemical analysis of paraoxonases-1, 2, and 3 expression in normal mouse tissues. Free Radic. Biol. Med. 2008, 45, 146–157. [Google Scholar] [CrossRef]
- Navab, M.; Imes, S.S.; Hama, S.Y.; Hough, G.P.; Ross, L.A.; Bork, R.W.; Valente, A.J.; Berliner, J.A.; Drinkwater, D.C.; Laks, H.; et al. Monocyte transmigration induced by modification of low density lipoprotein in cocultures of human aortic wall cells is due to induction of monocyte chemotactic protein 1 synthesis and is abolished by high density lipoprotein. J. Clin. Investig. 1991, 88, 2039–2046. [Google Scholar] [CrossRef]
- Shih, D.M.; Gu, L.; Xia, Y.R.; Navab, M.; Li, W.F.; Hama, S.; Castellani, L.W.; Furlong, C.E.; Costa, L.G.; Fogelman, A.M.; et al. Mice lacking serum paraoxonase are susceptible to organophosphate toxicity and atherosclerosis. Nature 1998, 394, 284–287. [Google Scholar] [CrossRef]
- Bacchetti, T.; Ferretti, G.; Sahebkar, A. The role of paraoxonase in cancer. Semin. Cancer Biol. 2019, 56, 72–86. [Google Scholar] [CrossRef]
- Seshadri, S.; Beiser, A.; Selhub, J.; Jacques, P.F.; Rosenberg, I.H.; D’Agostino, R.B.; Wilson, P.W.; Wolf, P.A. Plasma homocysteine as a risk factor for dementia and Alzheimer’s disease. N. Engl. J. Med. 2002, 346, 476–483. [Google Scholar] [CrossRef]
- Undas, A.; Perla, J.; Lacinski, M.; Trzeciak, W.; Kazmierski, R.; Jakubowski, H. Autoantibodies against N-homocysteinylated proteins in humans: Implications for atherosclerosis. Stroke 2004, 35, 1299–1304. [Google Scholar] [CrossRef]
- Vos, E. Homocysteine levels, paraoxonase 1 (PON1) activity, and cardiovascular risk. JAMA 2008, 300, 168–169. [Google Scholar] [CrossRef]
- Billecke, S.; Draganov, D.; Counsell, R.; Stetson, P.; Watson, C.; Hsu, C.; La Du, B.N. Human serum paraoxonase (PON1) isozymes Q and R hydrolyze lactones and cyclic carbonate esters. Drug Metab. Dispos. Biol. Fate Chem. 2000, 28, 1335–1342. [Google Scholar]
- Taler-Verčič, A.; Goličnik, M.; Bavec, A. The Structure and Function of Paraoxonase-1 and Its Comparison to Paraoxonase-2 and -3. Molecules 2020, 25, 5980. [Google Scholar] [CrossRef]






| Controls | RA | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| First Author, Year Country | n | Age (Years) | Gender (M/F) | PON-1 (Mean ± SD) | ARE (Mean ± SD) | n | Age (Years) | Gender (M/F) | PON-1 (Mean ± SD) | ARE (Mean ± SD) |
| Tanimoto N, 2003 Japan [29] | 25 | 61 | 2/23 | 169 ± 67 | -- | 25 | 61 | 2/23 | 125 ± 61 | -- |
| Baskol G, 2005 Turkey [30] | 25 | 43 | NR | 225 ± 73 | -- | 57 | 46 | NR | 168 ± 72 | -- |
| Altindag O, 2006 Turkey [31] | 26 | 37 | 16/10 | 101 ± 44 | 68 ± 5 | 25 | 38 | 17/8 | 74 ± 17 | 64 ± 7 |
| Isik A, 2006 Turkey [32] | 23 | 50 | 6/17 | 149 ± 21 | 394 ± 42 | 47 | 50 | 7/40 | 84 ± 53 | 360 ± 49 |
| Charles-Schoeman C, 2012 USA [33] | 40 | 52 | 8/32 | -- | 12.6 ± 0.8 | 40 | 56 | 6/34 | -- | 9.7 ± 0.5 |
| Sezer U, 2013, Turkey [34] | 20 | 41 | 6/14 | 42 ± 52 | 46 ± 22 | 20 | 44 | 2/18 | 71 ± 51 | 60 ± 21 |
| El-Banna H, 2014 Saudi Arabia [35] | 90 | 41 | 30/60 | 152 ± 18 | 364 ± 169 | 120 | 41 | 30/90 | 64 ± 11 | 198 ± 84 |
| Shahmohamadnejad S, 2015 Iran [36] | 397 | 49 | 36/361 | -- | 142 ± 67 | 419 | 49 | 42/377 | -- | 111 ± 34 |
| Bindal UD, 2016 India [37] | 40 | 48 | 20/20 | 229 ± 17 | -- | 40 | 49 | 20/20 | 156 ± 19 | -- |
| Botta, 2016 Argentina [38] | 33 | 49 | 7/26 | 128 ± 45 | 157 ± 39 | 44 | 56 | 5/39 | 115 ± 38 | 144 ± 34 |
| Keskin Y, 2016 Turkey [39] | 61 | 41 | 20/41 | 84 ± 53 | 146 ± 19 | 29 | 39 | 9/20 | 70 ± 51 | 131 ± 20 |
| Rodriguez-Carrio J, 2016 Spain [40] | 110 | 54 | 29/81 | 312 ± 99 | -- | 212 | 58 | 37/175 | 287 ± 236 | -- |
| O’Neill F, 2018 UK [41] | 18 | 56 | 8/10 | 161 ± 53 | -- | 18 | 59 | 6/12 | 143 ± 20 | -- |
| Shevchuk SV, 2018 Ukraine [42] | 25 | NR | NR | 138 ± 19 | -- | 67 | NR | 18/49 | 107 ± 24 | -- |
| Yang L, 2018 China [43] | 12 | 43 | 3/9 | 440 ± 60 | -- | 24 | 47 | 6/18 | 409 ± 39 | -- |
| Mucientes A, 2019 Spain [44] | 477 | NR | 234/243 | -- | 55 ± 31 | 549 | NR | 170/379 | -- | 53 ± 46 |
| Atwa ET, 2020 Egypt [45] | 51 | 40 | NR | 20 ± 14 | -- | 48 | 42 | NR | 4.6 ± 4.7 | -- |
| Bassu S, 2020 Italy [46] | 101 | 55 | 50/51 | 128 ± 76 | -- | 164 | 55 | 62/102 | 110 ± 67 | -- |
| Parada-Turska J, 2020 Poland [47] | 70 | 52 | 12/58 | 6.79 ± 0.69 | 55 ± 31 | 74 | 55 | 14/60 | 4.88 ± 0.69 | 53 ± 46 |
| Alisik T, 2021 Turkey [48] | 67 | 52 | 7/60 | 228 ± 106 | -- | 130 | 55 | 23/107 | 195 ± 131 | -- |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Erre, G.L.; Bassu, S.; Giordo, R.; Mangoni, A.A.; Carru, C.; Pintus, G.; Zinellu, A. Association between Paraoxonase/Arylesterase Activity of Serum PON-1 Enzyme and Rheumatoid Arthritis: A Systematic Review and Meta-Analysis. Antioxidants 2022, 11, 2317. https://doi.org/10.3390/antiox11122317
Erre GL, Bassu S, Giordo R, Mangoni AA, Carru C, Pintus G, Zinellu A. Association between Paraoxonase/Arylesterase Activity of Serum PON-1 Enzyme and Rheumatoid Arthritis: A Systematic Review and Meta-Analysis. Antioxidants. 2022; 11(12):2317. https://doi.org/10.3390/antiox11122317
Chicago/Turabian StyleErre, Gian Luca, Stefania Bassu, Roberta Giordo, Arduino A. Mangoni, Ciriaco Carru, Gianfranco Pintus, and Angelo Zinellu. 2022. "Association between Paraoxonase/Arylesterase Activity of Serum PON-1 Enzyme and Rheumatoid Arthritis: A Systematic Review and Meta-Analysis" Antioxidants 11, no. 12: 2317. https://doi.org/10.3390/antiox11122317
APA StyleErre, G. L., Bassu, S., Giordo, R., Mangoni, A. A., Carru, C., Pintus, G., & Zinellu, A. (2022). Association between Paraoxonase/Arylesterase Activity of Serum PON-1 Enzyme and Rheumatoid Arthritis: A Systematic Review and Meta-Analysis. Antioxidants, 11(12), 2317. https://doi.org/10.3390/antiox11122317










