Oxidative Stress Markers and Modified Model for End-Stage Liver Disease Are Associated with Outcomes in Patients with Advanced Heart Failure Receiving Bridged Therapy with Continuous-Flow Left Ventricular Assist Devices
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population and Data Collection
2.2. Pharmacological Treatment
2.3. Laboratory Measurements
2.4. Scales
- −
- OSI = (TOS, μmol/L)/(TAC, mmol/L) [10];
- −
- modMELD = 1.12 × (ln 1) + 0.378 × (ln total bilirubin, in mg/dL) + 0.957 × (ln creatinine, in mg/dL) + 0.643; for an albumin concentration ≥4.1 g/dL;
- −
- modMELD = 1.12 × (ln [1 + 4.1—albumin, g/dL)]) + 0.378 × (ln total bilirubin, in mg/dL) + 0.957 × (ln creatinine, in mg/dL) + 0.643, for an albumin concentration <4.1 g/dL [11].
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hsich, E.M.; Rogers, J.G.; McNamara, D.M.; Taylor, D.O.; Starling, R.C.; Blackstone, E.H.; Schold, J.D. Does survival on the heart transplant waiting list depend on the underlying heart disease? JACC Heart Fail. 2016, 4, 689–697. [Google Scholar] [CrossRef]
- Nguyen, V.P.; Mahr, C.; Mokadam, N.A.; Pal, J.; Smith, J.W.; Dardas, T.F. The benefit of donor-recipient matching for patients undergoing heart transplantation. J. Am. Coll. Cardiol. 2017, 69, 1707–1714. [Google Scholar] [CrossRef] [PubMed]
- Kirklin, J.K.; Cantor, R.; Mohacsi, P.; Gummert, J.; De By, T.; Hannan, M.M.; Kormos, R.L.; Schueler, S.; Lund, L.H.; Nakatani, T.; et al. First Annual IMACS report: A global International Society for Heart and Lung Transplantation Registry for Mechanical Circulatory Support. J. Heart Lung Transpl. 2016, 35, 407–412. [Google Scholar] [CrossRef]
- Kirklin, J.K.; Pagani, F.D.; Kormos, R.L.; Stevenson, L.W.; Blume, E.D.; Myers, S.L.; Miller, M.A.; Baldwin, J.T.; Young, J.B.; Naftel, D.C. Eighth annual INTERMACS report: Special focus on framing the impact of adverse events. J. Heart Lung Transpl. 2017, 36, 1080–1086. [Google Scholar] [CrossRef] [PubMed]
- Kirklin, J.K.; Naftel, D.C.; Pagani, F.D.; Kormos, R.L.; Stevenson, L.W.; Blume, E.D.; Myers, S.L.; Miller, M.A.; Baldwin, J.T.; Young, J.B. Seventh INTERMACS annual report: 15,000 patients and counting. J. Heart Lung Transpl. 2015, 34, 1495–1504. [Google Scholar] [CrossRef]
- Ponikowski, P.; Voors, A.A.; Anker, S.D.; Bueno, H.; Cleland, J.G.; Coats, A.J.; Falk, V.; González-Juanatey, J.R.; Harjola, V.P.; Jankowska, E.A.; et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur. J. Heart Fail. 2016, 18, 891–975. [Google Scholar] [PubMed]
- Ohkawa, H.; Ohishi, N.; Yagi, K. Assay for lipid peroxides in animal tissues by thiobarbituric acid reaction. Anal. Biochem. 1979, 95, 351–358. [Google Scholar] [CrossRef]
- Erel, O. A new automated colorimetric method for measuring total oxidant status. Clin. Biochem. 2005, 38, 1103–1111. [Google Scholar] [CrossRef]
- Erel, O. A novel automated method to measure total antioxidant response against potent free radical reactions. Clin. Biochem. 2004, 37, 112–119. [Google Scholar] [CrossRef]
- Romuk, E.; Wojciechowska, C.; Jacheć, W.; Nowak, J.; Niedziela, J.; Malinowska-Borowska, J.; Głogowska-Gruszka, A.; Birkner, E.; Rozentryt, P. Comparison of Oxidative Stress Parameters in Heart Failure Patients Depending on Ischaemic or Nonischaemic Aetiology. Oxid. Med. Cell. Longev. 2019, 2019, 7156038. [Google Scholar] [CrossRef]
- Szczurek, W.; Gąsior, M.; Romuk, E.; Skrzypek, M.; Szyguła-Jurkiewicz, B. Usefulness of combining prognostic scores to predict survival in patients with advanced heart failure. J. Heart Lung Transpl. 2019, 38, 1224–1227. [Google Scholar] [CrossRef]
- Mandrekar, J.N. Receiver operating characteristic curve in diagnostic test assessment. J. Thorac. Oncol. 2010, 5, 1315–1316. [Google Scholar] [CrossRef] [PubMed]
- Malinchoc, M.; Kamath, P.S.; Gordon, F.D.; Peine, C.J.; Rank, J.; ter Borg, P.C. A model to predict poor survival in patients undergoing transjugular intrahepatic portosystemic shunts. Hepatology 2000, 31, 864871. [Google Scholar] [CrossRef]
- Critsinelis, A.; Kurihara, C.; Volkovicher, N.; Kawabori, M.; Sugiura, T.; Manon, M.; Wang, S.; Civitello, A.B.; Morgan, J.A. Model of End-Stage Liver Disease-eXcluding International Normalized Ratio (MELD-XI) Scoring System to Predict Outcomes in Patients Who Undergo Left Ventricular Assist Device Implantation. Ann. Thorac. Surg. 2018, 106, 513–519. [Google Scholar] [CrossRef] [PubMed]
- Bonde, P.; Ku, N.C.; Genovese, E.A.; Bermudez, C.A.; Bhama, J.K.; Ciarleglio, M.M.; Cong, X.; Teuteberg, J.J.; Kormos, R.L. Model for end-stage liver disease score predicts adverse events related to ventricular assist device therapy. Ann. Thorac. Surg. 2012, 93, 1541–1547. [Google Scholar] [CrossRef] [PubMed]
- Amione-Guerra, J.; Cruz-Solbes, A.S.; Gonzalez Bonilla, H.; Estep, J.D.; Guha, A.; Bhimaraj, A.; Suarez, E.E.; Bruckner, B.A.; Torre-Amione, G.; Park, M.H.; et al. Melding a High-Risk Patient for Continuous Flow Left Ventricular Assist Device into a Low-Risk Patient. ASAIO J. 2017, 63, 704–712. [Google Scholar] [CrossRef]
- Yalcin, Y.C.; Muslem, R.; Veen, K.M.; Soliman, O.I.; Manintveld, O.C.; Darwish Murad, S.; Kilic, A.; Constantinescu, A.A.; Brugts, J.J.; Alkhunaizi, F.; et al. Impact of preoperative liver dysfunction on outcomes in patients with left ventricular assist devices. Eur. J. Cardiothorac. Surg. 2020, 57, 920–928. [Google Scholar] [CrossRef]
- Hasin, T.; Topilsky, Y.; Schirger, J.A.; Li, Z.; Zhao, Y.; Boilson, B.A.; Clavell, A.L.; Rodeheffer, R.J.; Frantz, R.P.; Edwards, B.S.; et al. Changes in renal function after implantation of continuous-flow left ventricular assist devices. J. Am. Coll. Cardiol. 2012, 59, 26–36. [Google Scholar] [CrossRef]
- Sandner, S.E.; Zimpfer, D.; Zrunek, P.; Rajek, A.; Schima, H.; Dunkler, D.; Grimm, M.; Wolner, E.; Wieselthaler, G.M. Renal function and outcome after continuous flow left ventricular assist device implantation. Ann. Thorac. Surg. 2009, 87, 1072–1078. [Google Scholar] [CrossRef]
- Kamdar, F.; Boyle, A.; Liao, K.; Colvin-adams, M.; Joyce, L.; John, R. Effects of centrifugal, axial, and pulsatile left ventricular assist device support on end-organ function in heart failure patients. J. Heart Lung Transpl. 2009, 28, 352–359. [Google Scholar] [CrossRef]
- Yoshioka, D.; Takayama, H.; Colombo, P.C.; Yuzefpolskaya, M.; Garan, A.R.; Topkara, V.K.; Han, J.; Kurlansky, P.; Naka, Y.; Takeda, K. Changes in End-Organ Function in Patients With Prolonged Continuous-Flow Left Ventricular Assist Device Support. Ann. Thorac. Surg. 2017, 103, 717–724. [Google Scholar] [CrossRef] [PubMed]
- Wadia, Y.; Etheridge, W.; Smart, F.; Wood, R.P.; Frazier, O.H. Pathophysiology of hepatic dysfunction and intrahepatic cholestasis in heart failure and after left ventricular assist device suport. J. Heart Lung Transpl. 2005, 24, 361–370. [Google Scholar] [CrossRef]
- Szygula-Jurkiewicz, B.; Szczurek, W.; Skrzypek, M.; Zakliczyński, M.; Siedlecki, Ł.; Przybyłowski, P.; Zembala, M.; Gąsior, M. One-year survival of ambulatory patients with end-stage heart failure: The analysis of prognostic factors. Pol. Arch. Intern. Med. 2017, 127, 254–260. [Google Scholar] [CrossRef][Green Version]
- Jessup, M.; Constanzo, M.R. The cardiorenal syndrome: Do we need a change strategy or a change tactics? J. Am. Coll. Cardiol. 2009, 53, 597–599. [Google Scholar] [CrossRef] [PubMed]
- Coffin, S.T.; Waguespack, D.R.; Haglund, N.A.; Maltais, S.; Dwyer, J.P.; Keebler, M.E. Kidney dysfunction and left ventricular assist device support: A comprehensive perioperative review. Cardiorenal. Med. 2015, 5, 48–60. [Google Scholar] [CrossRef] [PubMed]
- Schieber, M.; Chandel, N.S. ROS function in redox signaling and oxidative stress. Curr. Biol. 2014, 24, R453–R462. [Google Scholar] [CrossRef]
- Takimoto, E.; Kass, D.A. Role of oxidative stress in cardiac hypertrophy and remodeling. Hypertension 2007, 49, 241–248. [Google Scholar] [CrossRef]
- Tsutsui, H.; Kinugawa, S.; Matsushima, S. Oxidative stress and heart failure. Am. J. Physiol-Heart Circ. Physiol. 2011, 301, 2181–2190. [Google Scholar] [CrossRef] [PubMed]
- van der Pol, A.; van Gilst, W.H.; Voors, A.A.; van der Meer, P. Treating oxidative stress in heart failure: Past, present and future. Eur. J. Heart Fail. 2019, 21, 425–435. [Google Scholar] [CrossRef]
- Keith, M.; Geranmayegan, A.; Sole, M.J.; Kurian, R.; Robinson, A.; Omran, A.S.; Jeejeebhoy, K.N. Increased oxidative stress in patients with congestive heart failure. J. Am. Coll. Cardiol. 1998, 31, 1352–1356. [Google Scholar] [CrossRef]
- Caruso, R.; Garatti, A.; Sedda, V.; Milazzo, F.; Campolo, J.; Colombo, T.; Catena, E.; Cighetti, G.; Russo, C.; Frigerio, M.; et al. Pre-operative redox state affects 1-month survival in patients with advanced heart failure undergoing left ventricular assist device implantation. J. Heart Lung Transpl. 2007, 26, 1177–1181. [Google Scholar] [CrossRef] [PubMed]
- Motoyama, T.; Okamoto, K.; Kukita, I.; Hamaguchi, M.; Kinoshita, Y.; Ogawa, H. Possible role of increased oxidant stress in multiple organ failure after systemic inflammatory response syndrome. Crit. Care Med. 2003, 31, 1048–1052. [Google Scholar] [CrossRef] [PubMed]

| Parameters | General Population N = 36 a | Without MACE 1 N = 19 | With MACE N = 17 | p b |
|---|---|---|---|---|
| Baseline data | ||||
| Age, years | 58.0 (50.0–63.0) | 58.0 (39.0–64.0) | 58.0 (52.0–61.0) | 0.8005 |
| Male, n (%) | 33 (86.8) | 18 (94.7) | 15 (88.2) | 0.4811 |
| Follow up, days | 547.00 (522.5–547.0) | 547.0 (547.0–547.0) | 522.0 (515.0–533.0) | <0.0001 b |
| Ischemic etiology, % | 24 (66.7) | 14 (73.7) | 10 (58.8) | 0.034 b |
| BMI, kg/m2 | 27.4 (5.9) | 27.1 (5.8) | 27.6 (6.1) | 0.7982 |
| HR, bpm | 71.31 (7.30) | 70.74 (7.11) | 71.94 (7.68) | 0.628 |
| SBP, mmHg | 96.50 (86.50–100.00) | 97.00 (89.00–100.00) | 96.00 (84.00–100.00) | 1 |
| DBP, mmHg | 66.25 (12.50) | 66.05 (10.72) | 66.47 (14.58) | 0.9219 |
| Comorbidities | ||||
| Hypertension, n (%) | 16 (44.4) | 8 (42.1) | 8 (47.1) | 0.7652 |
| Type 2 diabetes, n (%) | 16 (44.4) | 7 (36.8) | 9 (52.9) | 0.3318 |
| COPD, n (%) | 2 (0.06) | 1 (5.3) | 1 (5.9) | 0.9355 |
| Persistent FA, n (%) | 14 (38.9) | 5 (26.3) | 9 (52.9) | 0.1018 |
| Hypercholesterolemia, n (%) | 17 (47.2) | 8 (42.1) | 9 (52.9) | 0.5156 |
| Pulmonary hypertension, n (%) | 35 (97.2) | 18 (94.7) | 17 (100) | 0.3374 |
| Laboratory parameters | ||||
| WBC, ×109/l | 8.7 (6.7–9.9) | 7.7 (6.7–10.3) | 8.8 (6.7–9.7) | 0.875 |
| Hemoglobin, mmol/L | 7.86 (1.2) | 7.75 (1.2) | 7.98 (1.2) | 0.586 |
| Platelets, ×109/l | 187.0 (134.0–268.5) | 212.0 (164.0–274.0) | 168.0 (125.0–238.0) | 0.1294 |
| Albumin, g/L | 35 (32–39) | 38 (34–41) | 33 (31–38) | 0.0714 |
| Total protein, g/L | 64.6 (7.9) | 65.11 (8.3) | 64.06 (7.8) | 0.7009 |
| ALT, U/I | 33.5 (21.0–64.5) | 34.0 (21.0–44.0) | 33.0 (19.0–408.0) | 0.6598 |
| AST, U/I | 37.0 (25.0–58.5) | 31.0 (23.0–42.0) | 45.0 (37.0–273.0) | 0.0286 b |
| Total bilirubin, µmol/L | 24.8 (17.3–35.3) | 18.5 (12.5–29.8) | 33.5 (24.8–42.8) | 0.0041 b |
| hs-CRP, mg/L | 8.0 (4.5) | 6.9 (3.8) | 9.3 (5.0) | 0.1178 |
| Creatinine, µmol/L | 144.5 (44.4) | 121.5 (31.6) | 170.3 (43.1) | 0.0004 b |
| LDH, U/l | 322. 5 (242.0–458.0) | 289.0 (238.0–420.0) | 430.0 (250.0–521.0) | 0.1412 |
| Urea, µmol/L | 10.9 (7.3–14.6) | 10.3 (6.9–14.1) | 11.0 (9.2–18.0) | 0.4066 |
| NT-proBNP, pg/mL | 9440 (6826–17,466.5) | 7100 (3202–20,555) | (9220–16,531) | 0.0722 |
| Cholesterol, mmol/L | 3.4 (2.9–4.5) | 3.4 (3.1–3.9) | 3.3 (2.3–4.9) | 0.4067 |
| LDL, mmol/L | 1.7 (1.2–2.3) | 1.9 (1.2–2.5) | 1.50 (1.2–2.1) | 0.3807 |
| GGTP, U/I | 141.5 (74.5–186.5) | 140.0 (69.0–184.0) | 154.0 (116.0–189.0) | 0.7532 |
| ALP, U/I | 117.5 (59.0–159.0) | 94.0 (54.0–136.0) | 145.0 (75.0–174.0) | 0.0485 b |
| Glucose, mmol/L | 5.5 (5.2–6.1) | 5.3 (5.1–5.9) | 5.6 (5.4–7.1) | 0.281 |
| Sodium, mmol/L | 136.1 (3.6) | 135.6 (3.1) | 136.5 (4.1) | 0.4612 |
| Uric acid, µmol/L | 466.9 (146.9) | 479.1 (155.4) | 453.4 (140.3) | 0.6075 |
| Fibrinogen, mg/dl | 456.6 (104.2) | 451.9 (95.9) | 461.8 (115.5) | 0.7811 |
| TAC, mmol/L | 1.3 (1.0–1.4) | 1.4 (1.2–1.4) | 1.1 (1.0–1.3) | 0.0331 b |
| TOS, μmol/L | 2.9 (1.1) | 2.3 (0.9) | 3.8 (0.7) | <0.0001 b |
| OSI | 2.5 (1.7–2.8) | 1.7 (1.3–2.2) | 2.7 (2.6–4.5) | <0.0001 b |
| ModMELD | 17.2 (5.4) | 14.01 (4.3) | 20.7 (4.1) | <0.0001 b |
| Echocardiographic parameters | ||||
| RVDD, mm | 42.5 (40.5–45.0) | 42.0 (41.0- 44.0) | 45.0 (40.0–46.0) | 0.2938 |
| RVSP, mmHg | 45.2 (12.4) | 41.4 (10.6) | 49.41 (13.3) | 0.0512 |
| TAPSE, mm | 14.0 (12.0–16.0) | 15.0 (12.0–16.0) | 13.0 (12.0–17.0) | 0.7865 |
| LVEDD, mm | 74.5 (68.0–81.5) | 73.0 (67.0–83.0) | 75.0 (69.0–80.0) | 0.9372 |
| LA, mmol/L | 55.5 (7.5) | 50.1 (9.3) | 52.9 (6.7) | 0.3177 |
| LVEF, % | 15.0 (11.0–15.5) | 15.0 (10.0–18.0) | 14.0 (12.0–15.0) | 0.3978 |
| Pharmacology treatment | ||||
| B-blockers, n (%) | 35 (97.2) | 18 (94.7) | 17 (100) | 0.3374 |
| ACEI/ARB, n (%) | 27 (75) | 13 (68.4) | 14 (82.4) | 0.3352 |
| Loop diuretics, n (%) | 29 (80.6) | 15 (78.9) | 14 (82.4) | 0.7966 |
| MRA, n (%) | 34 (94.4) | 17 (89.5) | 17 (100) | 0.1687 |
| Digoxin, n (%) | 2 (0.06) | 1 (5.3) | 1 (5.9) | 0.9355 |
| Statin, n (%) | 11 (30.6) | 6 (31.6) | 5 (29.4) | 0.8879 |
| Coumarin derivatives, n (%) | 36 (100) | 19 (100) | 17 (100) | |
| Acetylsalicylic acid, n (%) | 16 (44.4) | 9 (47.4) | 7 (41.2) | 0.709 |
| Clopidogrel, n (%) | 20.0 (55.6) | 10 (52.6) | 10 (58.8) | 0.709 |
| Sildenafil, n (%) | 35 (97.2) | 18 (94.7) | 17 (100) | 0.3374 |
| ICD, n (%) | 24 (66.7) | 13 (68.4) | 11 (64.7) | 0.8134 |
| CRT-D, n (%) | 12 (33.3) | 6 (31.6) | 6 (35.3) | 0.8134 |
| Before LVAD Implantation N = 36 a | 6 Months after LVAD Implantation N = 36 | p b | |
|---|---|---|---|
| Albumin, g/L | 35.2 (5.8) | 45.1 (3.7) | <0.0001 b |
| Total protein, g/L | 64.6 (7.9) | 75.4 (4.4) | <0.0001 b |
| ALT, U/I | 33.5 (21.0–64.5) | 17.0 (13.5–24.0) | <0.0001 b |
| AST, U/I | 37.0 (25.0–58.5) | 21.5 (17.0–28.0) | <0.0001 b |
| GGTP, U/I | 141.5 (74.5–186.5) | 47.5 (33.0–109.5) | <0.0001 b |
| ALP, U/I | 117.5 (59.0–159.0) | 95.5 (72.5–118.5) | 0.2193 |
| Total bilirubin, µmol/L | 24.8 (17.4–35.3) | 11.1 (7.3–14.2) | <0.0001 b |
| hs-CRP, mg/L | 7.0 (4.4–11.4) | 3.4 (2.3–7.0) | 0.0008 b |
| Creatinine, µmol/L | 137.5 (109.5–183.5) | 102.5 (95.5–127.5) | <0.0001 b |
| NT-proBNP, pg/mL | 9440.0 (6826.0–17,466.5) | 1347.0 (764.7–3299.5) | <0.0001 b |
| Na, mmol/L | 136.1 (3.6) | 139.5 (2.0) | <0.0001 b |
| Uric acid, µmol/L | 466.9 (146.9) | 456.5 (114.3) | 0.7 |
| Fibrinogen, mg/dl | 449.5 (368.5–522.0) | 389.0 (343.5–441.0) | 0.0191 b |
| TAC, mmol/L | 1.3 (1.0–1.4) | 1.2 (1.1–1.4) | 0.6165 |
| TOS, μmol/L | 3.1 (2.1–3.8) | 2.2 (1.3–4.4) | 0.4776 |
| OSI | 2.5 (1.7–2.8) | 1.9 (1.0–3.9) | 0.7118 |
| modMELD | 16.5 (13.0–21.7) | 7.9 (7.3–0.1) | <0.0001 b |
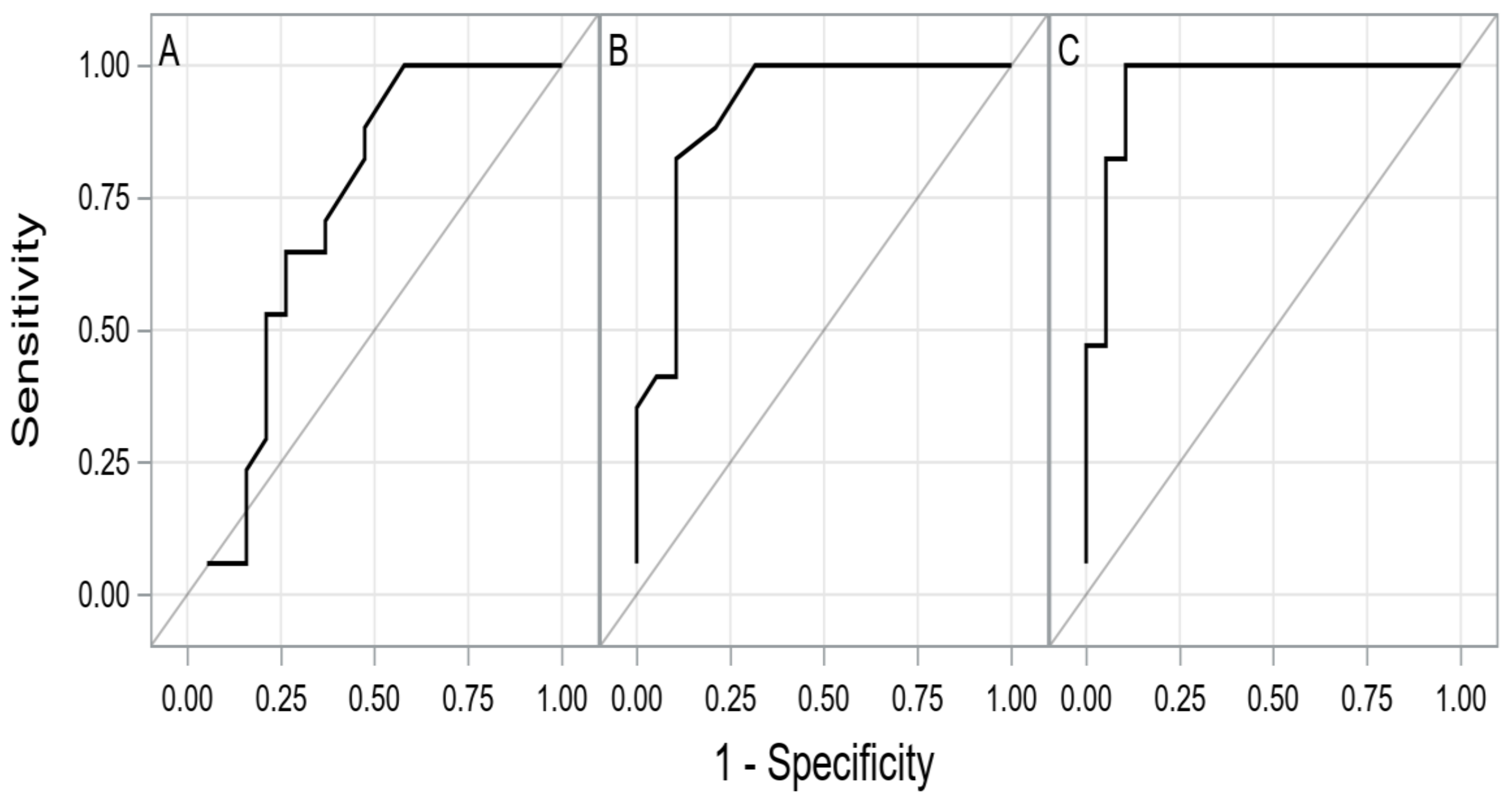
| AUC (±95 CI) | p | Cut-Off | Sens. (±95 CI) | Spec. (±95 CI) | PPV | NPV | Accuracy | |
|---|---|---|---|---|---|---|---|---|
| TAC | 0.7183 (0.5417–0.8948) | <0.01 | <1.37 | 0.99 (0.80–0.99) | 0.42 (0.20–0.67) | 0.61 (0.41–0.79) | 0.99 (0.64–0.99) | 0.69 (0.52–0.84) |
| TOS | 0.9149 (0.8205–0.9900) | <0.01 | >3.28 | 0.82 (0.57–0.96) | 0.89 (0.67–0.99) | 0.88 (0.63–0.98) | 0.85 (0.62–0.97) | 0.86 (0.62–0.97) |
| OSI | 0.9628 (0.9030–0.9878) | <0.01 | >2.48 | 0.99 (0.80–0.99) | 0.89 (0.67–0.99) | 0.89 (0.67–0.99) | 0.99 (0.80–0.99) | 0.94 (0.81–0.99) |
| modMELD | 0.8700 (0.7494–0.9905) | <0.01 | >17.55 | 0.82 (0.57–0.96) | 0.84 (0.60–0.97) | 0.82 (0.57–0.96) | 0.84 (0.60–0.97) | 0.83 (0.60–0.94) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Szyguła-Jurkiewicz, B.; Szczurek-Wasilewicz, W.; Gąsior, M.; Copik, I.; Małyszek-Tumidajewicz, J.; Skrzypek, M.; Romuk, E.; Zembala, M.; Zembala, M.; Przybyłowski, P. Oxidative Stress Markers and Modified Model for End-Stage Liver Disease Are Associated with Outcomes in Patients with Advanced Heart Failure Receiving Bridged Therapy with Continuous-Flow Left Ventricular Assist Devices. Antioxidants 2021, 10, 1813. https://doi.org/10.3390/antiox10111813
Szyguła-Jurkiewicz B, Szczurek-Wasilewicz W, Gąsior M, Copik I, Małyszek-Tumidajewicz J, Skrzypek M, Romuk E, Zembala M, Zembala M, Przybyłowski P. Oxidative Stress Markers and Modified Model for End-Stage Liver Disease Are Associated with Outcomes in Patients with Advanced Heart Failure Receiving Bridged Therapy with Continuous-Flow Left Ventricular Assist Devices. Antioxidants. 2021; 10(11):1813. https://doi.org/10.3390/antiox10111813
Chicago/Turabian StyleSzyguła-Jurkiewicz, Bożena, Wioletta Szczurek-Wasilewicz, Mariusz Gąsior, Izabela Copik, Justyna Małyszek-Tumidajewicz, Michał Skrzypek, Ewa Romuk, Michał Zembala, Marian Zembala, and Piotr Przybyłowski. 2021. "Oxidative Stress Markers and Modified Model for End-Stage Liver Disease Are Associated with Outcomes in Patients with Advanced Heart Failure Receiving Bridged Therapy with Continuous-Flow Left Ventricular Assist Devices" Antioxidants 10, no. 11: 1813. https://doi.org/10.3390/antiox10111813
APA StyleSzyguła-Jurkiewicz, B., Szczurek-Wasilewicz, W., Gąsior, M., Copik, I., Małyszek-Tumidajewicz, J., Skrzypek, M., Romuk, E., Zembala, M., Zembala, M., & Przybyłowski, P. (2021). Oxidative Stress Markers and Modified Model for End-Stage Liver Disease Are Associated with Outcomes in Patients with Advanced Heart Failure Receiving Bridged Therapy with Continuous-Flow Left Ventricular Assist Devices. Antioxidants, 10(11), 1813. https://doi.org/10.3390/antiox10111813






