Dual Diagnosis in Adolescents with Problematic Use of Video Games: Beyond Substances
Abstract
1. Introduction
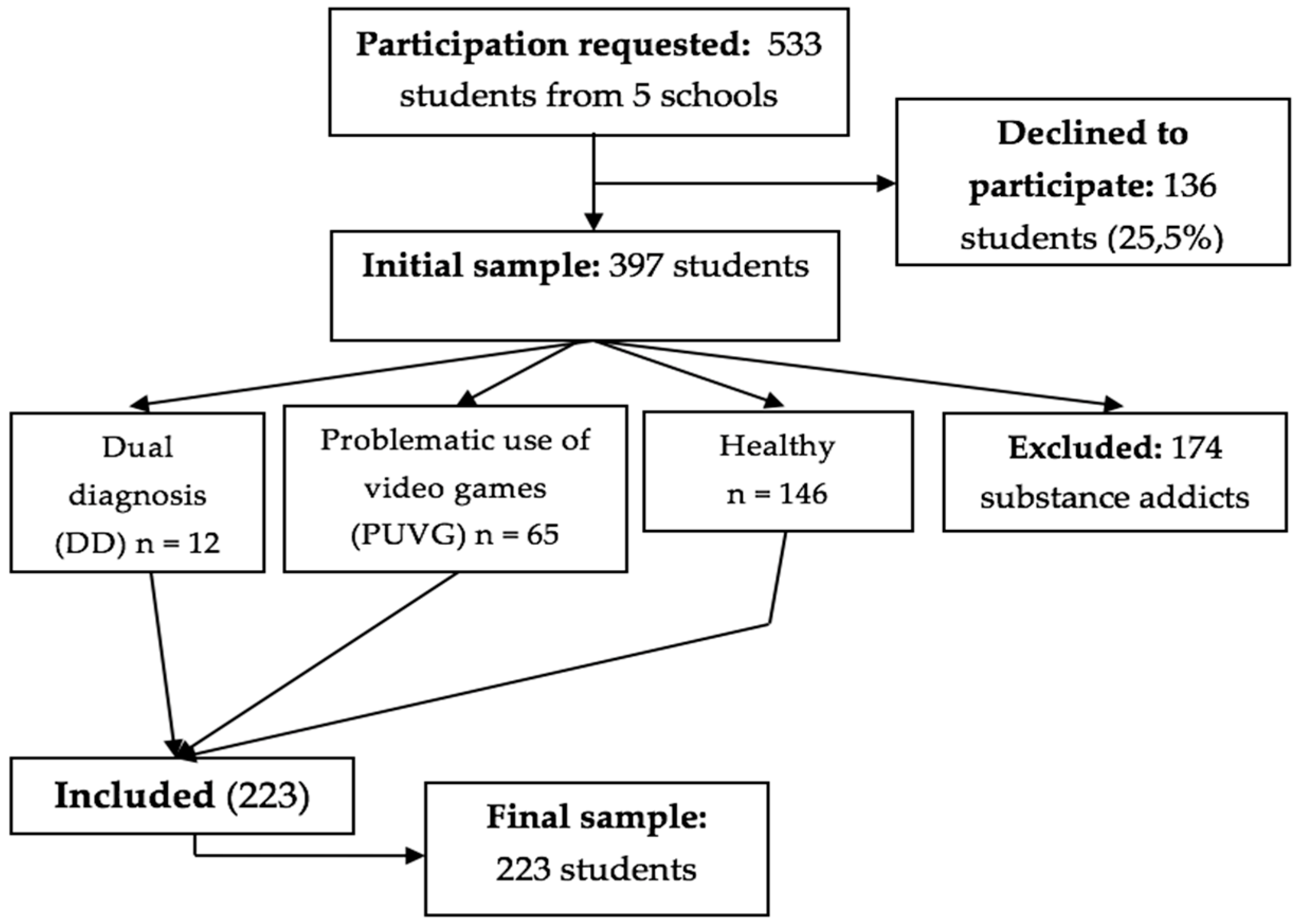
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- López-Caneda, E.; Mota, N.; Crego, A.; Velasquez, T.; Corral, M.; Rodríguez, S.; Cadaveira, F. Neurocognitive anomalies associated with the binge drinking pattern of alcohol consumption in adolescents and young people: A review. Adicciones 2014, 26, 334–359. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. The ICD-11 Classification of Mental and Behavioral Disorders: Diagnostic Criteria for Research; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- Edition, F. Diagnostic and statistical manual of mental disorders. Am. Psychiatric. Assoc. 2013, 21, 591–643. [Google Scholar]
- Pettorruso, M.; Valle, S.; Cavic, E.; Martinotti, G.; di Giannantonio, M.; Grant, J.E. Problematic Internet use (PIU), personality profiles and emotion dysregulation in a cohort of young adults: Trajectories from risky behaviors to addiction. Psychiatry Res. 2020, 289, 113036. [Google Scholar] [CrossRef] [PubMed]
- Oliva Delgado, A.; Hidalgo García, M.V.; Moreno Rodríguez, M.D.C.; Jiménez García, L.; Jiménez Iglesias, A.M.; Antolín Suarez, L.; Ramos Valverde, P. Uso y riesgo de adicciones a las nuevas tecnologías entre adolescentes y jóvenes andaluces. Universidad de Sevilla: Agua Clara SL. 2012. Available online: https://personal.us.es/oliva/libroadicciones.pdf (accessed on 3 January 2022).
- Chacón, C.R.; Zurita, O.F.; Castro, S.M.; Espejo, G.T.; Martínez, A.; Ruiz-Rico, G. The association of Self-concept with Substance Abuse and Problematic Use of Video Games in University Students: A Structural Equation Model. Relación entre autoconcepto, consumo de sustancias y uso problemático de videojuegos en universitarios: Un modelo de ecuaciones estructurales [Relationship between self-concept, substance use and problematic use of video games in university students: A model of structural equations]. Adicciones 2018, 30, 179–188. [Google Scholar] [CrossRef]
- Ricquebourg, M.; Bernède-Bauduin, C.; Mété, D.; Dafreville, C.; Stojcic, I.; Vauthier, M.; Galland, M.C. Internet et jeux vidéo chez les étudiants de La Réunion en 2010: Usages, mésusages, perceptions et facteurs associés. [Internet and video games among students of Reunion Island in 2010: Uses, misuses, perceptions and associated factors]. Rev. Epidemiol Sante Publique. 2013, 61, 503–512. [Google Scholar] [CrossRef] [PubMed]
- Pápay, O.; Urbán, R.; Griffiths, M.D.; Nagygyörgy, K.; Farkas, J.; Kökönyei, G.; Katalin, F.; Attila, O.; Zsuzsanna, E.; Zsolt, D. Psychometric properties of the problematic online gaming questionnaire short-form and prevalence of problematic online gaming in a national sample of adolescents. Cyberpsychol. Behav. Soc. Netw. 2013, 16, 340–348. [Google Scholar] [CrossRef]
- van Rooij, A.J.; Schoenmakers, T.M.; Vermulst, A.A.; van den Eijnden, R.J.; van de Mheen, D. Online video game addiction: Identification of addicted adolescent gamers. Addiction 2011, 106, 205–212. [Google Scholar] [CrossRef]
- de Leeuw, J.R.; de Bruijn, M.; de Weert-van Oene, G.H.; Schrijvers, A.J. Internet and game behaviour at a secondary school and a newly developed health promotion programme: A prospective study. BMC Public Health 2010, 10, 544. [Google Scholar] [CrossRef]
- Wood, R.T.A. Problems with the concept of video game “addiction”: Some case study examples. Int. J. Ment. Health Addict. 2007, 6, 169–178. [Google Scholar] [CrossRef]
- Khurana, A.; Romer, D.; Betancourt, L.M.; Brodsky, N.L.; Giannetta, J.M.; Hurt, H. Working memory ability predicts trajectories of early alcohol use in adolescents: The mediational role of impulsivity. Addiction 2013, 108, 506–515. [Google Scholar] [CrossRef]
- Kuss, D.J.; Griffiths, M.D. Internet and gaming addiction: A systematic literature review of neuroimaging studies. Brain Sci. 2012, 2, 347–374. [Google Scholar] [CrossRef] [PubMed]
- Grant, J.E.; Potenza, M.N.; Weinstein, A.; Gorelick, D.A. Introduction to behavioral addictions. Am. J. Drug Alcohol. Abuse 2010, 36, 233–241. [Google Scholar] [CrossRef] [PubMed]
- Jorgenson, A.G.; Hsiao, R.C.; Yen, C.F. Internet Addiction and Other Behavioral Addictions. Child Adolesc. Psychiatr. Clin. N. Am. 2016, 25, 509–520. [Google Scholar] [CrossRef] [PubMed]
- Gjoneska, B.; Potenza, M.N.; Jones, J.; Corazza, O.; Hall, N.; Sales, C.M.; Grünblatt, E.; Martinotti, G.; Burkauskas, J.; Werling, A.M.; et al. Problematic use of the internet during the COVID-19 pandemic: Good practices and mental health recommendations. Compr. Psychiatry. 2022, 112, 152279. [Google Scholar] [CrossRef] [PubMed]
- Martinotti, G.; Alessi, M.C.; Di Natale, C.; Sociali, A.; Ceci, F.; Lucidi, L.; Picutti, E.; Di Carlo, F.; Corbo, M.; Vellante, F.; et al. Psychopathological Burden and Quality of Life in Substance Users during the COVID-19 Lockdown Period in Italy. Front. Psychiatry 2020, 11, 572245. [Google Scholar] [CrossRef]
- Vismara, M.; Caricasole, V.; Starcevic, V.; Cinosi, E.; Dell’Osso, B.; Martinotti, G.; Fineberg, N.A. Is cyberchondria a new transdiagnostic digital compulsive syndrome? A systematic review of the evidence. Compr. Psychiatry 2020, 99, 152167. [Google Scholar] [CrossRef]
- Jiménez-Murcia, S.; Fernández-Aranda, F.; Granero, R.; Menchón, J.M. Gambling in Spain: Update on experience, research and policy. Addiction 2014, 109, 1595–1601. [Google Scholar] [CrossRef]
- Kim, Y.J.; Lim, J.A.; Lee, J.Y.; Oh, S.; Kim, S.N.; Kim, D.J.; Choi, J.S. Impulsivity and compulsivity in Internet gaming disorder: A comparison with obsessive-compulsive disorder and alcohol use disorder. J. Behav. Addict. 2017, 6, 545–553. [Google Scholar] [CrossRef]
- Suntharalingam, S.; Johnson, D.; Suresh, S.; Thierrault, F.L.; De Sante, S.; Perinpanayagam, P.; Salamatmanesh, M.; Pajer, K. Rates of Dual Diagnosis in Child and Adolescent Psychiatric Inpatients: A Scoping Review. J. Addict. Med. 2022, 16, 101–109. [Google Scholar] [CrossRef]
- Chamarro, A.; Carbonell, X.; Manresa, J.M.; Munoz-Miralles, R.; Ortega-Gonzalez, R.; Lopez-Morron, M.R.; Batalla-Martinez, C.; Toran-Montserrat, P. El Cuestionario de Experiencias Relacionadas con los Videojuegos (CERV): Un instrumento para detectar el uso problemático de videojuegos en adolescentes españoles. [The Questionnaire of Experiences Associated with Video games (CERV): An instrument to detect the problematic use of video games in Spanish adolescents]. Adicciones 2014, 26, 303–311. [Google Scholar]
- Lloret, I.D.; Morell, G.R.; Marzo, C.J.C.; Tirado, G.S. Validación española de la Escala de Adicción a Videojuegos para Adolescentes (GASA). [Spanish validation of Game Addiction Scale for Adolescents (GASA)]. Aten. Primaria 2018, 50, 350–358. [Google Scholar] [CrossRef] [PubMed]
- Rial, A.; Kim-Harris, S.; Knight, J.R.; Araujo, M.; Gómez, P.; Brana, T.; Varela, J.; Golpe, S. Empirical validation of the CRAFFT Abuse Screening Test in a Spanish sample. Validación empírica del CRAFFT Abuse Screening. Test en una muestra de adolescentes españoles. Adicciones 2019, 31, 160–169. [Google Scholar] [CrossRef]
- Araujo, M.; Golpe, S.; Braña, T.; Varela, J.; Rial, A. Validación psicométrica del POSIT para el cribado del consumo de riesgo de alcohol y otras drogas entre adolescentes. [Psychometric validation of the POSIT for screening alcohol and other drugs risk consumption among adolescents]. Adicciones 2018, 30, 130–139. [Google Scholar] [CrossRef] [PubMed]
- Álvarez, S.; Gallego, P.; Latorre, C.; Bermejo, F. Para la detección de consumo excesivo de alcohol en Atención Primaria. [Papel del Test Audit (Alcohol Use Disorders Identification Test)]. MEDIFAM 2001, 11, 553–557. Available online: https://scielo.isciii.es/pdf/medif/v11n9/revisioncri.pdf (accessed on 15 December 2021).
- González, J.; Fernández, S.; Pérez, E.; Santamaría, P. Adaptación Española del Sistema de Evaluación de la Conducta en Niños y Adolescentes: BASC; TEA Ediciones: Madrid, Spain, 2004. [Google Scholar]
- Barbaranelli, C.; Caprara, G.V.; Rabasca, A. BFQ-NA: Cuestionario “Big Five” de Personalidad Para Niños y Adolescentes: Manual, 3rd ed.; TEA Ediciones: Madrid, Spain, 2013. [Google Scholar]
- Benito, A.; Calvo, G.; Real-López, M.; Gallego, M.J.; Francés, S.; Turbi, Á.; Haro, G. Creation of the TXP parenting questionnaire and study of its psychometric properties. Creación y estudio de las propiedades psicométricas del cuestionario de socialización parental TXP. Adicciones 2019, 31, 117–135. [Google Scholar] [CrossRef] [PubMed]
- van Rooij, A.J.; Kuss, D.J.; Griffiths, M.D.; Shorter, G.W.; Schoenmakers, M.T.; van De Mheen, D. The (co-)occurrence of problematic video gaming, substance use, and psychosocial problems in adolescents. J. Behav Addict. 2014, 3, 157–165. [Google Scholar] [CrossRef]
- Coëffec, A.; Romo, L.; Cheze, N.; Riazuelo, H.; Plantey, S.; Kotbagi, G.; Kern, L. Early substance consumption and problematic use of video games in adolescence. Front. Psychol. 2015, 6, 501. [Google Scholar] [CrossRef]
- Oflu, A.; Yalcin, S.S. Uso de videojuegos en alumnos de la escuela secundaria y factores asociados. [Video game use among secondary school students and associated factors]. Arch. Argent. Pediatr. 2019, 117, e584–e591. [Google Scholar] [CrossRef]
- Brandt, M. Video Games Active Reward Regions of Brains in Men More than Women. Stanford study finds; Stanford School of Medicine news release: Stanford, CA, USA, 2008; Available online: https://med.stanford.edu/news/all-news/2008/02/video-games-activate-reward-regions-of-brain-in-men-more-than-women-stanford-study-finds.html (accessed on 7 October 2021).
- Sugaya, N.; Shirasaka, T.; Takahashi, K.; Kanda, H. Bio-psychosocial factors of children and adolescents with internet gaming disorder: A systematic review. Biopsychosoc. Med. 2019, 13, 3. [Google Scholar] [CrossRef]
- González, M.; Landero, R. Diferencias en la percepción de estilos parentales entre jóvenes y adultos de las mismas familias. Summa Psicológica UST 2012, 9, 53–64. [Google Scholar] [CrossRef][Green Version]
- Río-Martínez, L.; Marquez-Arrico, J.E.; Prat, G.; Adan, A. Temperament and Character Profile and Its Clinical Correlates in Male Patients with Dual Schizophrenia. J. Clin. Med. 2020, 9, 1876. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Mondragón, S.; Adan, A. Personality in male patients with substance use disorder and/or severe mental illness. Psychiatry Res. 2015, 228, 488–494. [Google Scholar] [CrossRef] [PubMed]
- Gervasi, A.M.; La Marca, L.; Lombardo, E.; Mannino, G.; Iacolino, C.; Schimmenti, A. Maladaptive personality traits and internet addiction symptoms among young adults: A study based on the alternative DSM-5 model for personality disorders. Clin. Neuropsychiatry 2017, 14, 20–28. [Google Scholar]
- Şalvarlı, Ş.İ.; Griffiths, M.D. Internet gaming disorder and its associated personality traits: A systematic review using PRISMA guidelines. Int. J. Ment. Health Addict. 2021, 19, 1420–1442. [Google Scholar] [CrossRef]
- López-Fernández, F.J.; Mezquita, L.; Griffiths, M.D.; Ortet, G.; Ibáñez, M.I. El papel de la personalidad en el juego problemático y en las preferencias de géneros de videojuegos en adolescentes. [The role of personality on disordered gaming and game genre preferences in adolescence: Gender differences and person-environment transactions]. Adicciones 2021, 33, 263–272. [Google Scholar] [CrossRef] [PubMed]
- Hwang, J.Y.; Choi, J.S.; Gwak, A.R.; Jung, D.; Choi, S.W.; Lee, J.; Kim, D.J. Shared psychological characteristics that are linked to aggression between patients with Internet addiction and those with alcohol dependence. Ann. Gen. Psychiatry 2014, 13, 6. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Llorens, M.; Marí-Sanmillán, M.I.; Benito, A.; Rodríguez-Ruiz, F.; Castellano-García, F.; Almodóvar, I.; Haro, G. Personality traits and psychopathology in adolescents with videogame addiction. Adicciones. 2021, 23, 1629. [Google Scholar] [CrossRef]
- Oreland, L.; Lagravinese, G.; Toffoletto, S.; Nilsson, K.W.; Harro, J.; Robert, C.C.; Comasco, E. Personality as an intermediate phenotype for genetic dissection of alcohol use disorder. J. Neural. Transm. 2018, 125, 107–130. [Google Scholar] [CrossRef]
- Muros, B.; Aragón, Y.; Bustos, A. La ocupación del tiempo libre de jóvenes en el uso de videojuegos y redes. Comunicar 2013, 40, 31–39. [Google Scholar] [CrossRef]
- van Hagen, L.J.; de Waal, M.M.; Christ, C.; Dekker, J.J.M.; Goudriaan, A.E. Patient Characteristics Predicting Abstinence in Substance Use Disorder Patients with Comorbid Mental Disorders. J. Dual Diagn. 2019, 15, 312–323. [Google Scholar] [CrossRef]
- Gonzálvez, M.T.; Espada, J.P.; Tejeiro, R. El uso problemático de videojuegos está relacionado con problemas emocionales en adolescentes. [Problem video game playing is related to emotional distress in adolescents]. Adicciones 2017, 29, 180–185. [Google Scholar] [CrossRef]
- Halbrook, Y.J.; O’Donnell, A.T.; Msetfi, R.M. When and How Video Games Can Be Good: A Review of the Positive Effects of Video Games on Well-Being. Perspect. Psychol. Sci. 2019, 14, 1096–1104. [Google Scholar] [CrossRef] [PubMed]
- Teng, Z.; Pontes, H.M.; Nie, Q.; Griffiths, M.D.; Guo, C. Depression and anxiety symptoms associated with internet gaming disorder before and during the COVID-19 pandemic: A longitudinal study. J. Behav. Addict. 2021, 10, 169–180. [Google Scholar] [CrossRef] [PubMed]
- Viana, R.B.; de Lira, C.A.B. Exergames as Coping Strategies for Anxiety Disorders During the COVID-19 Quarantine Period. Games Health J. 2020, 9, 147–149. [Google Scholar] [CrossRef] [PubMed]
- Király, O.; Potenza, M.N.; Stein, D.J.; King, D.L.; Hodgins, D.C.; Saunders, J.B.; Griffiths, M.D.; Biljana, G.; Joël, B.; Matthias, B.; et al. Preventing problematic internet use during the COVID-19 pandemic: Consensus guidance. Compr. Psychiatry 2020, 100, 152180. [Google Scholar] [CrossRef]
- Button, K.S.; Ioannidis, J.P.; Mokrysz, C.; Nosek, B.A.; Flint, J.; Robinson, E.S.; Munafò, M.R. Power failure: Why small sample size undermines the reliability of neuroscience. Nat. Rev. Neurosci. 2013, 14, 365–376. [Google Scholar] [CrossRef]
- Jo, Y.S.; Bhang, S.Y.; Choi, J.S.; Lee, H.K.; Lee, S.Y.; Kweon, Y.S. Clinical Characteristics of Diagnosis for Internet Gaming Disorder: Comparison of DSM-5 IGD and ICD-11 GD Diagnosis. J. Clin. Med. 2019, 28, 945. [Google Scholar] [CrossRef] [PubMed]
- Kuss, D.J.; Griffiths, M.D. Internet Gaming Addiction: A Systematic Review of Empirical Research. Int. J. Ment. Health Addict. 2011, 10, 278–296. [Google Scholar] [CrossRef]
- Zilberman, N.; Yadid, G.; Efrati, Y.; Rassovsky, Y. Who becomes addicted and to what? Psychosocial predictors of substance and behavioral addictive disorders. Psychiatry Res. 2020, 291, 113221. [Google Scholar] [CrossRef]
- Arias, F.; Szerman, N.; Vega, P.; Mesías, B.; Basurte, I.; Morant, C.; Babín, F. Estudio Madrid sobre prevalencia y características de los pacientes con patología dual en tratamiento en las redes de salud mental y de atención al drogodependiente. Adicciones 2013, 25, 118–127. [Google Scholar] [CrossRef]
- Karapareddy, V. A Review of Integrated Care for Concurrent Disorders: Cost Effectiveness and Clinical Outcomes. J. Dual. Diagn. 2019, 15, 56–66. [Google Scholar] [CrossRef]
- Szerman, N.; Peris, L. Precision Psychiatry and Dual Disorders. J. Dual. Diagn. 2018, 14, 237–246. [Google Scholar] [CrossRef] [PubMed]
- Seo, E.H.; Yang, H.J.; Kim, S.G.; Park, S.C.; Lee, S.K.; Yoon, H.J. A Literature Review on the Efficacy and Related Neural Effects of Pharmacological and Psychosocial Treatments in Individuals with Internet Gaming Disorder. Psychiatry Investig. 2021, 18, 1149–1163. [Google Scholar] [CrossRef] [PubMed]
- Szerman, N.; Ferre, F.; Basurte-Villamor, I.; Arango, C. Gambling Dual Disorder: A Dual Disorder and Clinical Neuroscience Perspective. Front. Psychiatry 2020, 11, 589155. [Google Scholar] [CrossRef] [PubMed]
| Healthy | PUVG | DD | Statistics | |
|---|---|---|---|---|
| Female gender | 75.2% (n = 109) | 27.7% (n = 18) | 33.3% (n = 4) | χ2 45.287 (p < 0.001) V 0.45 CTR H 6.7/CTR DD −6.1. |
| Male gender | 24.8% (n = 36) | 72.3% (n = 47) | 66.7% (n = 8) | X2 45.287 (p < 0.001) V 0.45 CTR H −6.7/CTR DD 6.1. |
| Age in years | M (SD) = 14.67 (0.69) | M (SD) = 14.60 (0.67) | M (SD) = 14.66 (0.70) | F 0.184 (p = 0.832) ES 0.002 |
| Number of siblings | M (SD) = 1.97 (0.84) | M (SD) = 2.17 (1.08) | M (SD) = 2.11 (0.78) | F 0.949 (p = 0.389) ES 0.01 |
| Third year of compulsory secondary education | 48.3% (n = 70) | 52.3% (n = 34) | 58.3% (n = 7) | χ2 0.644 (p = 0.725) V 0.05 |
| Fourth year of compulsory secondary education | 51.7% (n = 75) | 47.7% (n = 31) | 41.7% (n = 5) | χ2 0.644 (p = 0.725) V 0.05 |
| Secular center | 67.8% (n = 99) | 69.2% (n = 45) | 91.7% (n = 11) | χ2 2.981 (p = 0.225) V 0.11 |
| Catholic center | 32.2% (n = 47) | 30.8% (n = 20) | 8.3% (n = 1) | χ2 2.981 (p = 0.225) V 0.11 |
| Private center | 34.2% (n = 50) | 40.0% (n = 26) | 41.7% (n = 5) | χ2 3.397 (p = 0.494) V 0.08 |
| Chartered (state-subsidised) center | 28.8% (n = 42) | 21.5% (n = 14) | 8.3% (n = 1) | χ2 3.397 (p = 0.494) V 0.08 |
| Public center | 37.0% (n = 54) | 38.5% (n = 25) | 50.0% (n = 6) | χ2 3.397 (p = 0.494) V 0.08 |
| Repeated year: no | 87.8% (n = 108) | 91.1% (n = 51) | 90.9% (n = 10) | χ2 0.463 (p = 0.793) V 0.04 |
| Repeated year: yes | 12.2% (n = 15) | 8.9% (n = 5) | 9.1% (n = 1) | χ2 0.463 (p = 0.793) V 0.04 |
| Mean grade: equivalent to a ‘fail’ | 0.8% (n = 1) | 1.8% (n = 1) | 10.0% (n = 1) | χ2 16.106 (p = 0.003) V 0.20 CTR DD 2.2 |
| Mean grade: equivalent to a ‘pass/good’ | 31.1% (n = 38) | 36.4% (n = 20) | 80.0% (n = 8) | χ2 16.106 (p = 0.003) V 0.20 CTR DD 3.0 |
| Mean grade: equivalent to ‘remarkable / outstanding’ | 68% (n = 83) | 61.8% (n = 34) | 10.0% (n = 1) | χ2 16.106 (p = 0.003) V 0.20 CTR DD −3.6 |
| Healthy | PUVG | DD | Statistics: F (p) Tukey’s HSD (p) | |
|---|---|---|---|---|
| M (SD) | M (SD) | M (SD) | ||
| Conscientiousness (BFQ) | 57.19 (8.20) | 52.57 (9.50) | 45.77 (11.76) | F 10.537 (< 0.001) ES 0.10 H > PUVG (0.004) H > DD (0.001) |
| Openness (BFQ) | 58.78 (8.94) | 56.41 (9.65) | 49.66 (10.44) | F 4.704 (0.01) ES 0.05 H > DD (0.014) |
| Extraversion (BFQ) | 51.28 (9.45) | 50.21 (9.81) | 48.55 (14.14) | F 0.475 (0.623) ES 0.005 |
| Agreeableness (BFQ) | 54.24 (8.99) | 50.30 (10.47) | 49.44 (11.69) | F 3.723 (0.026) ES 0.04 H > PUVG (0.034) |
| Emotional stability (BFQ) | 46.42 (11.08) | 48.10 (9.81) | 62.44 (10.19) | F 9.451 (< 0.001) ES 0.09 S < DD (< 0.001) PUVG < DD (0.001) |
| Healthy | PUVG | DD | Statistics | |
|---|---|---|---|---|
| Living with both parents | 76.2% (n = 93) | 83.9% (n = 47) | 63.6% (n = 7) | χ2 12.035 (p = 0.017) V 0.17 |
| Living with one parent alone | 23.8% (n = 29) | 10.7% (n = 6) | 27.3% (n = 3) | χ2 12.035 (p = 0.017) V 0.17 CTR PUVG −2.1 |
| Other cohabitants | 0.0% (n = 0) | 5.4% (n = 3) | 9.1% (n = 1) | χ2 12.035 (p = 0.017) V 0.17 CTR H −2.7/CTR PUVG 2.0 |
| Affection–communication (TXP) | M (SD) = 87.75 (12.18) | M (SD) = 82.67 (12.19) | M (SD) = 73.66 (13.02) | F 7.642 (p = 0.001) ES 0.08 Tukey’s HSD (p) H > PUVG 0.032) H > DD (0.003) |
| Control and structure (TXP) | M (SD) = 35.47 (5.26) | M (SD) = 35.44 (4.95) | M (SD) = 36.77 (4.23) | F 0.281 (p = 0.755) ES 0.003 |
| D | C | Op | Ag | ES | AC | |
|---|---|---|---|---|---|---|
| D | ||||||
| C | r = −0.361 p < 0.001 | |||||
| Op | r = −0.231 p < 0.001 | r = 0.748 p < 0.001 | ||||
| Ag | r = −0.249 p < 0.001 | r = 0.633 p < 0.001 | r = 0.437 p < 0.001 | |||
| ES | r = 0.239 p < 0.001 | r = −0.177 p < 0.001 | r = −0.209 p < 0.001 | r = −0.150 p = 0.003 | ||
| AC | r = −0.290 p < 0.001 | r = 0.314 p < 0.001 | r = 0.265 p < 0.001 | r = 0.261 p < 0.001 | r = −0.322 p < 0.001 |
| D | G | MG | LA | |
|---|---|---|---|---|
| D | ||||
| G | r = −0.442 p < 0.001 | |||
| MG | r = −0.180 p = 0.014 | r = 0.023 p = 0.669 | ||
| LA | r = −0.016 p = 0.830 | r = 0.003 p = 0.956 | r = −0.066 p = 0.230 |
| (a) Adjusted Multinomial Main Effects Regression | ||
|---|---|---|
| Problematic Use of Video Games OR [95% CI], p | Dual Diagnosis OR [95% CI], p | |
| Male gender | 9.854 [4.084–23.779], < 0.001 | 7.119 [1.132–44.785], 0.036 |
| Emotional stability (BFQ) | 1.017 [0.977–1.059], 0.412 | 1.116 [1.030–1.209], 0.008 |
| (b) Unadjusted Individual Multinomial Regressions | ||
| Problematic Use of Video Games OR [95% CI], p | Dual Diagnosis OR [95% CI], p | |
| Mean grade equivalent to a ‘fail’ | 2.441 [0.148–40.160], 0.532 | 83,000 [2.766–2490.921], 0.011 |
| Mean grade equivalent to a ‘pass/good’ | 1.285 [0.656–2.517], 0.465 | 17,474 [2.110–144.705], 0.008 |
| Conscientiousness (BFQ) | 0.936 [0.905–0.969], < 0.001 | 0.843 [0.776–0.916], < 0.001 |
| Openness (BFQ) | 0.968 [0.939–0.999], 0.045 | 0.901 [0.843–0.962], 0.002 |
| Agreeableness (BFQ) | 0.951 [0.921–0.982], 0.002 | 0.920 [0.861–0.983], 0.013 |
| Affection–communication (TXP) | 0.968 [0.945–0.992], 0.009 | 0.927 [0.891–0.965], < 0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Esteve, A.; Jovani, A.; Benito, A.; Baquero, A.; Haro, G.; Rodríguez-Ruiz, F. Dual Diagnosis in Adolescents with Problematic Use of Video Games: Beyond Substances. Brain Sci. 2022, 12, 1110. https://doi.org/10.3390/brainsci12081110
Esteve A, Jovani A, Benito A, Baquero A, Haro G, Rodríguez-Ruiz F. Dual Diagnosis in Adolescents with Problematic Use of Video Games: Beyond Substances. Brain Sciences. 2022; 12(8):1110. https://doi.org/10.3390/brainsci12081110
Chicago/Turabian StyleEsteve, Arturo, Antonio Jovani, Ana Benito, Abel Baquero, Gonzalo Haro, and Francesc Rodríguez-Ruiz. 2022. "Dual Diagnosis in Adolescents with Problematic Use of Video Games: Beyond Substances" Brain Sciences 12, no. 8: 1110. https://doi.org/10.3390/brainsci12081110
APA StyleEsteve, A., Jovani, A., Benito, A., Baquero, A., Haro, G., & Rodríguez-Ruiz, F. (2022). Dual Diagnosis in Adolescents with Problematic Use of Video Games: Beyond Substances. Brain Sciences, 12(8), 1110. https://doi.org/10.3390/brainsci12081110







