Eye Movement Abnormalities in Amyotrophic Lateral Sclerosis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Demographic and Clinical Data
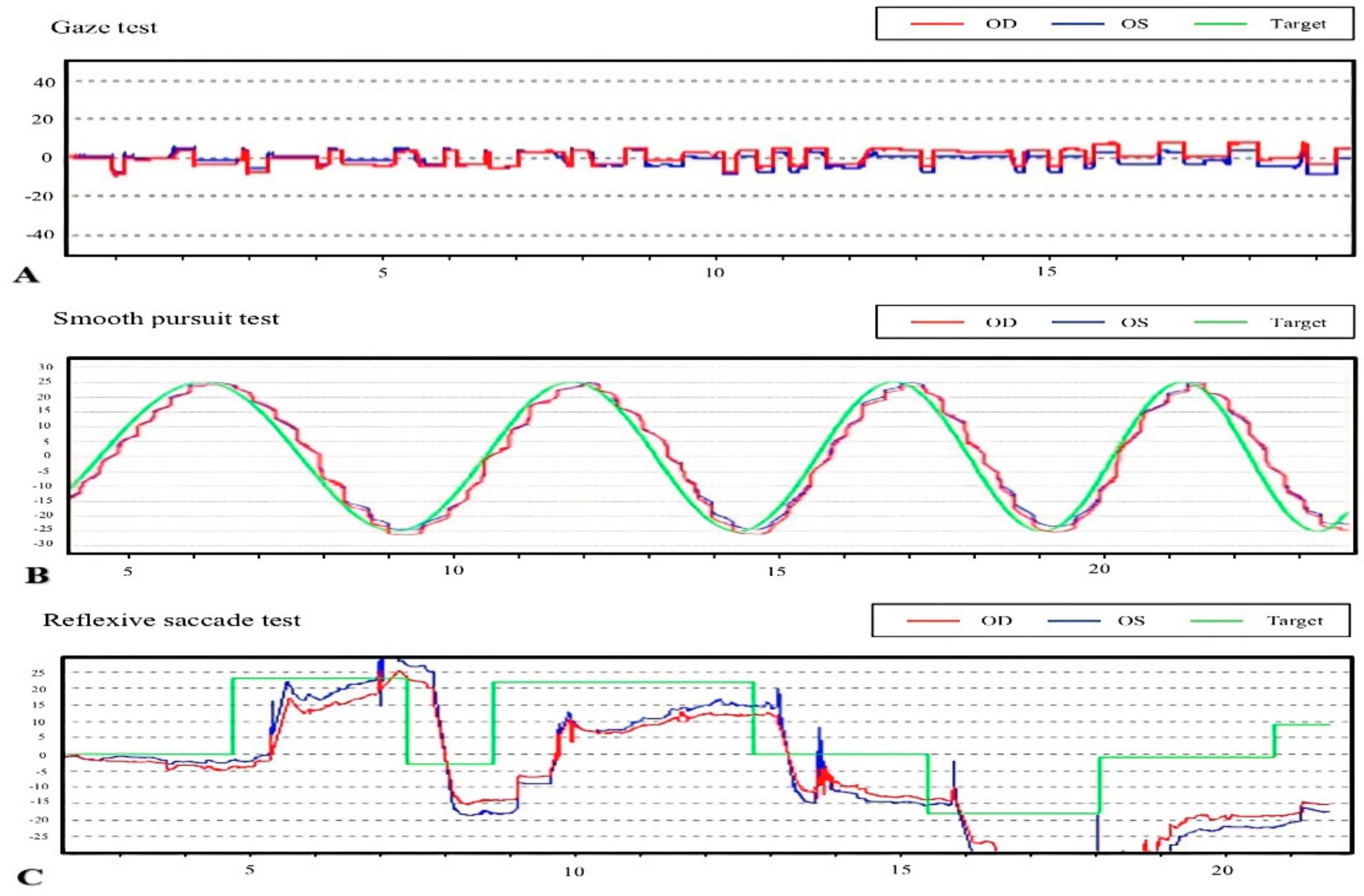
2.3. Oculomotor Evaluations
2.4. Statistical Analysis
3. Results
3.1. Comparison between ALS Patients and Control Subjects
3.2. Clinical Data and Oculomotor Performance of ALS Patients with and without Bulbar Involvement
3.3. Comparison between Bulbar-Onset and Spinal-Onset ALS Patients
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Brooks, B.R.; Miller, R.G.; Swash, M.; Munsat, T.L. El Escorial Revisited: Revised Criteria for the Diagnosis of Amyotrophic Lateral Sclerosis. Amyotroph. Lateral Scler. Other Mot. Neuron Disord. 2000, 1, 293–299. [Google Scholar] [CrossRef]
- Chen, L.; Zhang, B.; Chen, R.; Tang, L.; Liu, R.; Yang, Y.; Yang, Y.; Liu, X.; Ye, S.; Zhan, S.; et al. Natural History and Clinical Features of Sporadic Amyotrophic Lateral Sclerosis in China. J. Neurol. Neurosurg. Psychiatry 2015, 86, 1075–1081. [Google Scholar] [CrossRef] [PubMed]
- Chiò, A.; Logroscino, G.; Hardiman, O.; Swingler, R.; Mitchell, D.; Beghi, E.; Traynor, B.G. Prognostic Factors in Als: A Critical Review. Amyotroph. Lateral. Scler. 2009, 10, 310–323. [Google Scholar] [CrossRef] [Green Version]
- Robberecht, W.; Philips, T. The Changing Scene of Amyotrophic Lateral Sclerosis. Nat. Rev. Neurosci. 2013, 14, 248–264. [Google Scholar] [CrossRef]
- Mandrioli, J.; Faglioni, P.; Nichelli, P.; Sola, P. Amyotrophic Lateral Sclerosis: Prognostic Indicators of Survival. Amyotroph. Lateral. Scler. 2006, 7, 211–220. [Google Scholar] [CrossRef]
- Jacobs, L.; Bozian, D.; Heffner, R.R., Jr.; Barron, S.A. An Eye Movement Disorder in Amyotrophic Lateral Sclerosis. Neurology 1981, 31, 1282–1287. [Google Scholar] [CrossRef]
- Leveille, A.; Kiernan, J.; Goodwin, J.A.; Antel, J. Eye Movements in Amyotrophic Lateral Sclerosis. Arch. Neurol. 1982, 39, 684–686. [Google Scholar] [CrossRef]
- Mizuno, M. Neurotological Findings in Amyotrophic Lateral Sclerosis. Auris Nasus Larynx 1986, 13 (Suppl 2), S139–S146. [Google Scholar] [CrossRef]
- Saito, S.; Yamamoto, H. Analysis of Oculomotor Disorders in Motor Neuron Disease. Rinsho Shinkeigaku. 1989, 29, 969–975. [Google Scholar]
- Gizzi, M.; DiRocco, A.; Sivak, M.; Cohen, B. Ocular Motor Function in Motor Neuron Disease. Neurology 1992, 42, 1037–1046. [Google Scholar] [CrossRef]
- Okuda, B.; Yamamoto, T.; Yamasaki, M.; Maya, K.; Imai, T. Motor Neuron Disease with Slow Eye Movements and Vertical Gaze Palsy. Acta Neurol. Scand. 1992, 85, 71–76. [Google Scholar] [CrossRef] [PubMed]
- Marti-Fàbregas, J.; Roig, C. Oculomotor Abnormalities in Motor Neuron Disease. J. Neurol. 1993, 240, 475–478. [Google Scholar] [CrossRef] [PubMed]
- Ohki, M.; Kanayama, R.; Nakamura, T.; Okuyama, T.; Kimura, Y.; Koike, Y. Ocular Abnormalities in Amyotrophic Lateral Sclerosis. Acta Otolaryngol. Suppl. 1994, 511, 138–142. [Google Scholar] [CrossRef]
- Shaunak, S.; Orrell, R.W.; O’Sullivan, E.; Hawken, M.B.; Lane, R.J.; Henderson, L.; Kennard, C. Oculomotor Function in Amyotrophic Lateral Sclerosis: Evidence for Frontal Impairment. Ann. Neurol. 1995, 38, 38–44. [Google Scholar] [CrossRef] [PubMed]
- Palmowski, A.; Jost, W.H.; Prudlo, J.; Osterhage, J.; Käsmann, B.; Schimrigk, K.; Ruprecht, K.W. Eye Movement in Amyotrophic Lateral Sclerosis: A Longitudinal Study. Ger. J. Ophthalmol. 1995, 4, 355–362. [Google Scholar]
- Donaghy, C.; Pinnock, R.; Abrahams, S.; Cardwell, C.; Hardiman, O.; Patterson, V.; McGivern, R.C.; Gibson, J.M. Ocular Fixation Instabilities in Motor Neurone Disease. A Marker of Frontal Lobe Dysfunction? J. Neurol. 2009, 256, 420–426. [Google Scholar] [CrossRef]
- Donaghy, C.; Pinnock, R.; Abrahams, S.; Cardwell, C.; Hardiman, O.; Patterson, V.; McGivern, R.C.; Gibson, J.M. Slow Saccades in Bulbar-Onset Motor Neurone Disease. J. Neurol. 2010, 257, 1134–1140. [Google Scholar] [CrossRef] [Green Version]
- Moss, H.E.; McCluskey, L.; Elman, L.; Hoskins, K.; Talman, L.; Grossman, M.; Balcer, L.J.; Galetta, S.L.; Liu, G.T. Cross-Sectional Evaluation of Clinical Neuro-Ophthalmic Abnormalities in an Amyotrophic Lateral Sclerosis Population. J. Neurol. Sci. 2012, 314, 97–101. [Google Scholar] [CrossRef] [Green Version]
- Proudfoot, M.; Menke, R.A.; Sharma, R.; Berna, C.M.; Hicks, S.L.; Kennard, C.; Talbot, K.; Turner, M.R. Eye-Tracking in Amyotrophic Lateral Sclerosis: A Longitudinal Study of Saccadic and Cognitive Tasks. Amyotroph Lateral Scler Front. Degener 2015, 17, 101–111. [Google Scholar] [CrossRef] [Green Version]
- Kang, B.H.; Kim, J.I.; Lim, Y.M.; Kim, K.K. Abnormal Oculomotor Functions in Amyotrophic Lateral Sclerosis. J. Clin. Neurol. 2018, 14, 464–471. [Google Scholar] [CrossRef]
- Abel, L.A.; Williams, I.M.; Gibson, K.L.; Levi, L. Effects of Stimulus Velocity and Acceleration on Smooth Pursuit in Motor Neuron Disease. J. Neurol. 1995, 242, 419–424. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Zhang, S.; Huang, X.; Zhang, Y.; Fan, D. Vestibular Evoked Myogenic Potentials and Their Clinical Utility in Patients with Amyotrophic Lateral Sclerosis. Clin. Neurophysiol. 2019, 130, 647–654. [Google Scholar] [CrossRef] [PubMed]
- Neumann, M.; Sampathu, D.M.; Kwong, L.K.; Truax, A.C.; Micsenyi, M.C.; Chou, T.T.; Bruce, J.; Schuck, T.; Grossman, M.; Clark, C.M.; et al. Ubiquitinated Tdp-43 in Frontotemporal Lobar Degeneration and Amyotrophic Lateral Sclerosis. Science 2006, 314, 130–133. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Braak, H.; Brettschneider, J.; Ludolph, A.C.; Lee, V.M.; Trojanowski, J.Q.; Del Tredici, K. Amyotrophic Lateral Sclerosis--a Model of Corticofugal Axonal Spread. Nat. Rev. Neurol. 2013, 9, 708–714. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brettschneider, J.; Del Tredici, K.; Toledo, J.B.; Robinson, J.L.; Irwin, D.J.; Grossman, M.; Suh, E.; Van Deerlin, V.M.; Wood, E.M.; Baek, Y.; et al. Stages of Ptdp-43 Pathology in Amyotrophic Lateral Sclerosis. Ann. Neurol. 2013, 74, 20–38. [Google Scholar] [CrossRef] [PubMed]
- Gorges, M.; Müller, H.P.; Lulé, D.; Del Tredici, K.; Brettschneider, J.; Keller, J.; Pfandl, K.; Ludolph, A.C.; Kassubek, J.; Pinkhardt, E.H. Eye Movement Deficits Are Consistent with a Staging Model of Ptdp-43 Pathology in Amyotrophic Lateral Sclerosis. PLoS ONE 2015, 10, e0142546. [Google Scholar] [CrossRef]
- Leigh, R.J.; Zee, D.S. The Neurology of Eye Movements; Contemporary Neurology: Columbia, MD, USA, 2015. [Google Scholar]
- Swinnen, B.; Robberecht, W. The Phenotypic Variability of Amyotrophic Lateral Sclerosis. Nat. Rev. Neurol. 2014, 10, 661–670. [Google Scholar] [CrossRef] [Green Version]
- Kaufmann, P.; Levy, G.; Thompson, J.L.; Delbene, M.L.; Battista, V.; Gordon, P.H.; Rowland, L.P.; Levin, B.; Mitsumoto, H. The Alsfrsr Predicts Survival Time in an Als Clinic Population. Neurology 2005, 64, 38–43. [Google Scholar] [CrossRef]
- Kimura, F.; Fujimura, C.; Ishida, S.; Nakajima, H.; Furutama, D.; Uehara, H.; Shinoda, K.; Sugino, M.; Hanafusa, T. Progression Rate of Alsfrs-R at Time of Diagnosis Predicts Survival Time in Als. Neurology 2006, 66, 265–267. [Google Scholar] [CrossRef]
- McCaslin, D.L. Electronystagmography and Videonystagmography (Eng/Vng); Plural Publishing: San Diego, CA, USA, 2019. [Google Scholar]
- Herishanu, Y.O.; Sharpe, J.A. Normal Square Wave Jerks. Invest. Ophthalmol. Vis. Sci. 1981, 20, 268–272. [Google Scholar]
- Anagnostou, E.; Karavasilis, E.; Potiri, I.; Constantinides, V.; Efstathopoulos, E.; Kapaki, E.; Potagas, C. A Cortical Substrate for Square-Wave Jerks in Progressive Supranuclear Palsy. J. Clin. Neurol. 2020, 16, 37–45. [Google Scholar] [CrossRef] [PubMed]
- Otero-Millan, J.; Macknik, S.L.; Serra, A.; Leigh, R.J.; Martinez-Conde, S. Triggering Mechanisms in Microsaccade and Saccade Generation: A Novel Proposal. Ann. N. Y. Acad. Sci. 2011, 1233, 107–116. [Google Scholar] [CrossRef] [PubMed]
- Carasig, D.; Paul, K.; Fucito, M.; Ramcharan, E.; Gnadt, J.W. Irrepressible Saccades from a Tectal Lesion in a Rhesus Monkey. Vision Res. 2006, 46, 1161–1169. [Google Scholar] [CrossRef] [Green Version]
- Munoz, D.P.; Wurtz, R.H. Fixation Cells in Monkey Superior Colliculus. Ii. Reversible Activation and Deactivation. J Neurophysiol 1993, 70, 576–589. [Google Scholar] [CrossRef]
- Averbuch-Heller, L.; Helmchen, C.; Horn, A.K.; Leigh, R.J.; Büttner-Ennerver, J.A. Slow Vertical Saccades in Motor Neuron Disease: Correlation of Structure and Function. Ann. Neurol. 1998, 44, 641–648. [Google Scholar] [CrossRef]
| ALS Patients (n = 60) | Control Subjects (n = 30) | p-Value | |
|---|---|---|---|
| Age, y | 54.35 ± 10.87 | 53.13 ± 10.50 | 0.506 |
| Sex, male/female | 30 (50.0%)/30 (50.0%) | 15 (50.0%)/15 (50.0%) | |
| Age of onset, y | 52.82 ± 11.33 | ||
| Disease duration, mo | 17.50 (10.00, 33.75) | ||
| Onset pattern, bulbar/spinal | 12 (20.0%)/48 (80.0%) | ||
| Bulbar involvement, yes/no | 44 (73.3%)/16 (26.7%) | ||
| ALSFRS-R total score | 40.00 (36.00, 43.25) | ||
| ΔALSFRS-R | 0.57 (0.22, 0.88) |
| ALS Patients (n = 60) | Control Subjects (n = 30) | p-Value | ||
|---|---|---|---|---|
| Gaze test | Square-wave jerks | 32 (53.3%) | 2 (6.7%) | <0.001 * |
| Reflexive saccade test | Hypometria | 6 (10.0%) | 0 | 0.173 |
| Latency, ms | 342.23 ± 47.54 | 340.79 ± 23.16 | 0.153 | |
| Velocity, °/s | 603.00 (548.00, 656.50) | 541.00 (477.50, 657.50) a | 0.187 | |
| Smooth pursuit test | Abnormal cogwheeling | 30 (50.0%) | 2 (6.7%) | <0.001 * |
| Velocity gain toward left | 0.85 (0.82,0.88) | 0.87 (0.85,0.89) a | 0.106 | |
| Velocity gain toward right | 0.85 (0.82,0.87) | 0.86 (0.84,0.87) a | 0.097 |
| Square-Wave Jerks | Abnormal Cogwheeling during Smooth Pursuit | |||||||
|---|---|---|---|---|---|---|---|---|
| Univariate Analysis | Multivariable Analysis | Univariate Analysis | Multivariable Analysis | |||||
| OR (95% CI) | p-Value | OR (95% CI) | p-Value | OR (95% CI) | p-Value | OR (95% CI) | p-Value | |
| ALS patient | 16.00 (3.49–73.27) | <0.001 * | 16.20 (3.50–74.95) | <0.001 * | 13.50 (2.94–61.90) | 0.001 * | 14.04 (3.00–65.75) | 0.001 * |
| Age | 1.03 (0.99–1.08) | 0.135 | 1.03 (0.99–1.08) | 0.160 | 1.04 (1.00–1.09) | 0.050 | 1.05 (1.00–1.10) | 0.056 |
| Sex | 0.68 (0.29–1.61) | 0.385 | 0.44 (0.18–1.06) | 0.067 | ||||
| ALS Patients with Bulbar Involvement (n = 44) | ALS Patients without Bulbar Involvement (n = 16) | p-Value | ||
|---|---|---|---|---|
| Age, y | 55.16 ± 11.10 | 52.13 ± 10.22 | 0.343 | |
| Sex, male/female | 22 (50.0%)/22 (50.0%) | 8 (50.0%)/8 (50.0%) | ||
| Age of onset, y | 53.80 ± 11.66 | 50.13 ± 10.24 | 0.271 | |
| Disease duration, mo | 16.00 (9.25, 32.00) | 23.50 (11.25, 41.50) | 0.123 | |
| ALSFRS-R total score | 38.00 (32.00, 41.00) | 42.00 (40.00, 44.25) | 0.015 * | |
| ΔALSFRS-R | 0.71 (0.33, 1.00) a | 0.26 (0.15, 0.49) | 0.009 * | |
| Gaze test | Square-wave jerks | 30 (68.2%) | 2 (12.5%) | <0.001 * |
| Reflexive saccade test | Hypometria | 5 (11.4%) | 1 (6.3%) | |
| Latency, ms | 340.64 ± 50.85 | 346.67 ± 37.95 | 0.677 | |
| Velocity, °/s | 582.00 (548.50, 651.50) | 613.00 (517.00, 679.00) a | 0.443 | |
| Smooth pursuit test | Abnormal cogwheeling | 28 (63.6%) | 2 (12.5%) | 0.001 * |
| Velocity gain toward left | 0.85 (0.82, 0.88) | 0.86 (0.82, 0.90) a | 0.437 | |
| Velocity gain toward right | 0.85 (0.82, 0.87) | 0.85 (0.82, 0.86) a | 0.760 |
| Square-Wave Jerks | Abnormal Cogwheeling during Smooth Pursuit | |||||||
|---|---|---|---|---|---|---|---|---|
| Univariate Analysis | Multivariable Analysis | Univariate Analysis | Multivariable Analysis | |||||
| OR (95% CI) | p-Value | OR (95% CI) | p-Value | OR (95% CI) | p-Value | OR (95% CI) | p-Value | |
| Bulbar involvement | 15.00 (2.99–75.17) | 0.001 * | 26.51 (2.83–248.05) | 0.004 * | 12.25 (2.46–60.91) | 0.002 * | 6.56 (1.19–36.16) | 0.031 * |
| Age | 1.03 (0.98–1.08) | 0.319 | 1.20 (0.95–1.09) | 0.564 | 1.04 (0.99–1.09) | 0.123 | 1.01 (0.95–1.07) | 0.705 |
| Sex | 2.26 (0.80–6.36) | 0.123 | 2.36 (0.72–8.70) | 0.143 | ||||
| Age of onset | 1.03 (0.98–1.07) | 0.294 | 1.04 (0.99–1.09) | 0.126 | ||||
| Disease duration, | 0.98 (0.94–1.02) | 0.316 | 0.98 (0.95–1.02) | 0.399 | ||||
| ALSFRS-R total score | 0.92 (0.83–1.02) | 0.126 | 0.97 (0.84–1.12) | 0.668 | 0.90 (0.81–1.01) | 0.063 | 0.96 (0.84–1.09) | 0.507 |
| ΔALSFRS-R | 2.53 (0.68–9.42) | 0.166 | 0.745 (0.12–4.84) | 0.758 | 3.68 (0.93–14.49) | 0.063 | 1.47 (0.25–8.73) | 0.669 |
| Bulbar Onset (n = 12) | Spinal Onset (n = 48) | p-Value | ||
|---|---|---|---|---|
| Age, y | 58.17 ± 11.58 | 53.40 ± 10.60 | 0.176 | |
| Sex, male/female | 8 (66.7%)/4 (33.3%) | 22 (45.8%)/26 (54.2%) | 0.197 | |
| Age of onset, y | 61.50 (45.00, 66.25) | 51.00 (44.25, 60.50) a | 0.109 | |
| Disease duration, mo | 11.50 (9.00, 30.00) | 20.00 (11.00, 33.75) | 0.242 | |
| ALSFRS-R total score | 40.00 (38.00, 44.50) | 40.00 (35.50, 42.50) | 0.358 | |
| ΔALSFRS-R | 0.33 (0.23, 0.86) | 0.58 (0.21, 0.88) a | 0.746 | |
| Gaze test | Square-wave jerks | 9 (75.0%) | 23 (47.9%) | 0.115 |
| Reflexive saccade test | Hypometria | 1 (8.3%) | 5 (10.4%) | |
| Latency, ms | 322.17 ± 37.18 | 347.58 ± 48.91 | 0.100 | |
| Velocity, °/s | 554.00 ± 133.28 | 587.84 ± 108.60 | 0.365 | |
| Smooth pursuit test | Abnormal cogwheeling | 8 (66.7%) | 22 (45.8%) | 0.333 |
| Velocity gain toward left | 0.85 (0.83, 0.87) a | 0.85 (0.82, 0.88) | 0.844 | |
| Velocity gain toward right | 0.84 (0.82, 0.87) a | 0.85 (0.82, 0.86) | 0.783 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Guo, X.; Liu, X.; Ye, S.; Liu, X.; Yang, X.; Fan, D. Eye Movement Abnormalities in Amyotrophic Lateral Sclerosis. Brain Sci. 2022, 12, 489. https://doi.org/10.3390/brainsci12040489
Guo X, Liu X, Ye S, Liu X, Yang X, Fan D. Eye Movement Abnormalities in Amyotrophic Lateral Sclerosis. Brain Sciences. 2022; 12(4):489. https://doi.org/10.3390/brainsci12040489
Chicago/Turabian StyleGuo, Xintong, Xiaoxuan Liu, Shan Ye, Xiangyi Liu, Xu Yang, and Dongsheng Fan. 2022. "Eye Movement Abnormalities in Amyotrophic Lateral Sclerosis" Brain Sciences 12, no. 4: 489. https://doi.org/10.3390/brainsci12040489
APA StyleGuo, X., Liu, X., Ye, S., Liu, X., Yang, X., & Fan, D. (2022). Eye Movement Abnormalities in Amyotrophic Lateral Sclerosis. Brain Sciences, 12(4), 489. https://doi.org/10.3390/brainsci12040489






