Thalamic and Cerebellar Regional Involvement across the ALS–FTD Spectrum and the Effect of C9orf72
Abstract
1. Introduction
2. Materials and Methods
2.1. Clinical Data
2.2. Image Acquisition
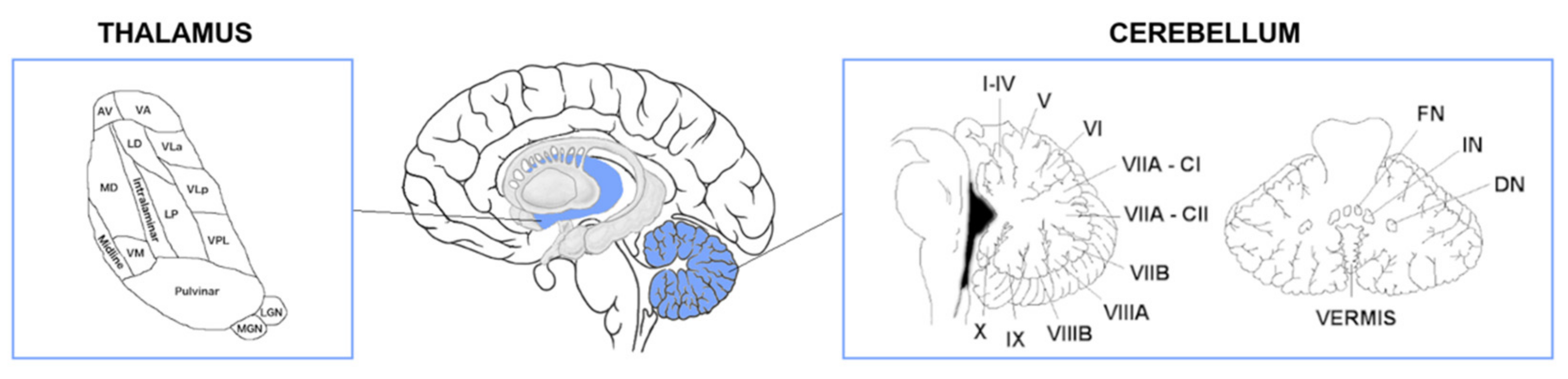
2.3. Thalamic and Cerebellar Subregions
2.4. Statistical Analyses
3. Results
3.1. Characteristics of Study Participants
3.1.1. Demographics
3.1.2. Cognitive Function
3.1.3. Behavioural Changes
3.2. Imaging Findings
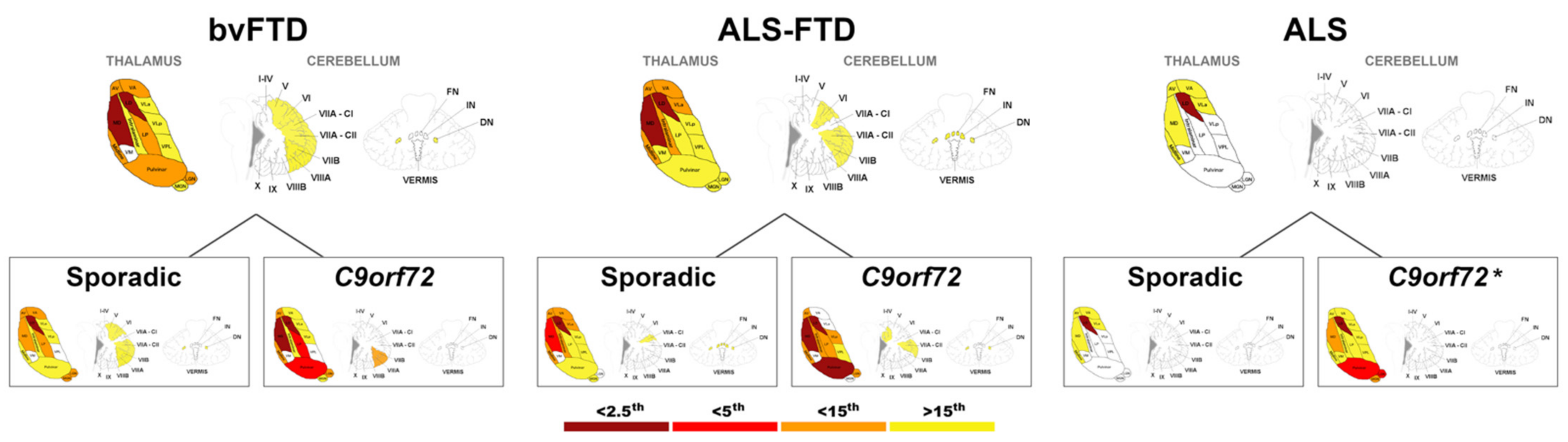
3.2.1. Thalamic and Cerebellar Regional Atrophy Patterns Compared to Controls
3.2.2. Thalamic and Cerebellar Regional Atrophy Patterns across Clinical Diagnosis
3.2.3. Effect of Genetic Status on Thalamic Regional Atrophy
bvFTD
ALS–FTD
ALS
3.2.4. Effect of Genetic Status on Cerebellar Regional Volumes
bvFTD
ALS–FTD
ALS
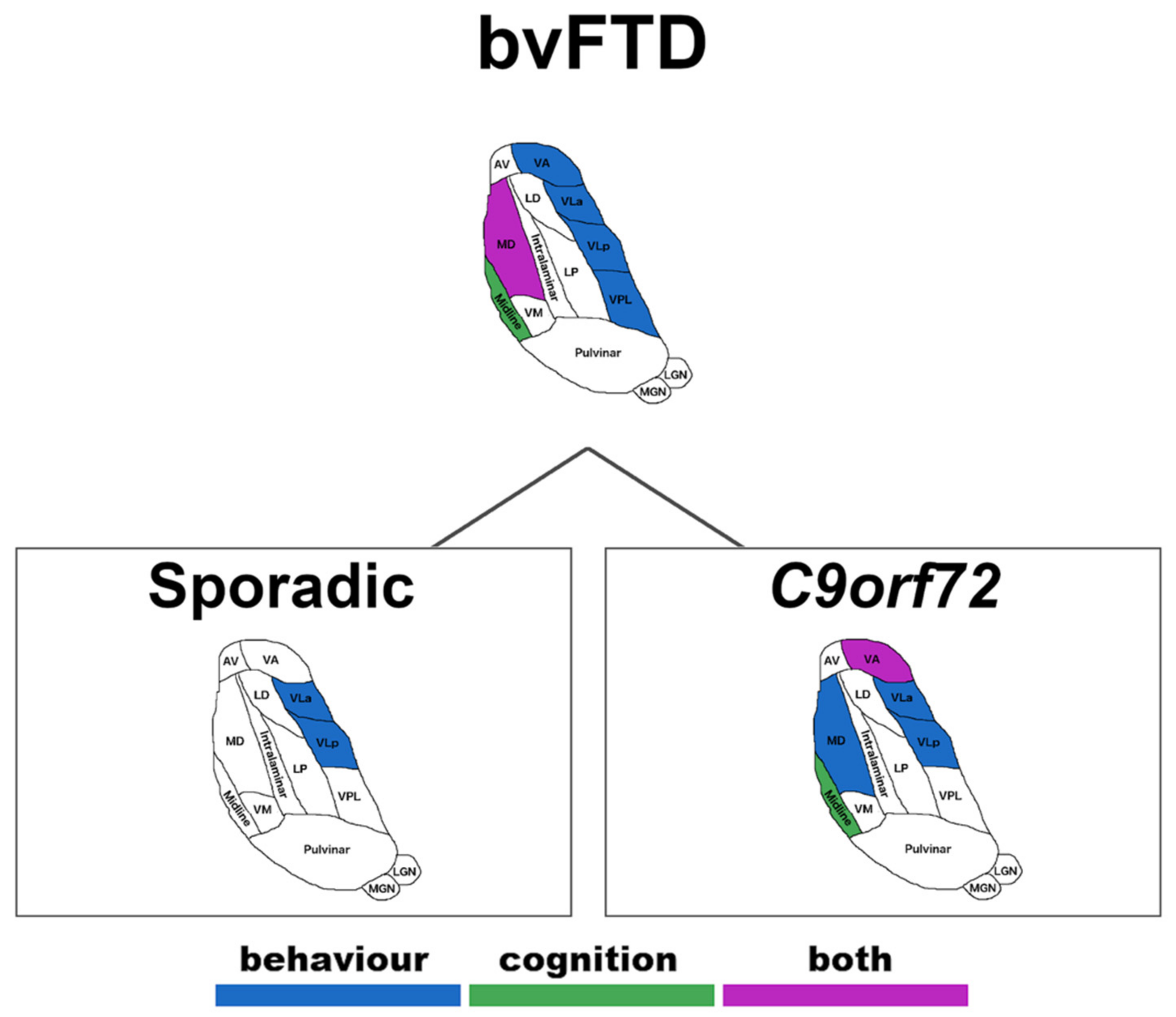
3.3. Correlations between Thalamic Volumes and Behaviour and Cognition
Sporadic versus Genetic Correlations
3.4. Correlations between Cerebellar Volumes and Behaviour and Cognition
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Burrell, J.R.; Halliday, G.M.; Kril, J.J.; Ittner, L.M.; Gotz, J.; Kiernan, M.C.; Hodges, J.R. The frontotemporal dementia-motor neuron disease continuum. Lancet 2016, 388, 919–931. [Google Scholar] [CrossRef]
- Ringholz, G.M.; Appel, S.H.; Bradshaw, M.; Cooke, N.A.; Mosnik, D.M.; Schulz, P.E. Prevalence and patterns of cognitive impairment in sporadic ALS. Neurology 2005, 65, 586–590. [Google Scholar] [CrossRef] [PubMed]
- Clark, C.M.; Forman, M.S. Frontotemporal lobar degeneration with motor neuron disease: A clinical and pathological spectrum. Arch. Neurol. 2006, 63, 489–490. [Google Scholar] [CrossRef] [PubMed]
- Lomen-Hoerth, C.; Anderson, T.; Miller, B. The overlap of amyotrophic lateral sclerosis and frontotemporal dementia. Neurology 2002, 59, 1077–1079. [Google Scholar] [CrossRef] [PubMed]
- Burrell, J.R.; Kiernan, M.C.; Vucic, S.; Hodges, J.R. Motor neuron dysfunction in frontotemporal dementia. Brain 2011, 134 Pt 9, 2582–2594. [Google Scholar] [CrossRef] [PubMed]
- Tan, R.; Kril, J.; Fatima, M.; McGeachie, A.; McCann, H.; Shepherd, C.; Forrest, S.L.; Affleck, A.; Kwok, J.; Hodges, J.R.; et al. TDP-43 proteinopathies: Pathological identification of brain regions differentiating clinical phenotypes. Brain 2015, 138 Pt 10, 3110–3122. [Google Scholar] [CrossRef]
- MacKenzie, I.R.A.; Bigio, E.H.; Ince, P.; Geser, F.; Neumann, M.; Cairns, N.J.; Kwong, L.K.; Forman, M.S.; Ravits, J.; Stewart, H.; et al. Pathological TDP-43 distinguishes sporadic amyotrophic lateral sclerosis from amyotrophic lateral sclerosis with SOD1 mutations. Ann. Neurol. 2007, 61, 427–434. [Google Scholar] [CrossRef]
- Rohrer, J.D.; Geser, F.; Zhou, J.; Gennatas, E.D.; Sidhu, M.; Trojanowski, J.Q.; DeArmond, S.J.; Miller, B.L.; Seeley, W.W. TDP-43 subtypes are associated with distinct atrophy patterns in frontotemporal dementia. Neurology 2010, 75, 2204–2211. [Google Scholar] [CrossRef]
- Hodges, J. Familial frontotemporal dementia and amyotrophic lateral sclerosis associated with the C9ORF72 hexanucleotide repeat. Brain 2012, 135 Pt 3, 652–655. [Google Scholar] [CrossRef]
- Majounie, E.; Renton, A.E.; Mok, K.; Dopper, E.G.; Waite, A.; Rollinson, S.; Chio, A.; Restagno, G.; Nicolaou, N.; Sánchez, J.S.; et al. Frequency of the C9orf72 hexanucleotide repeat expansion in patients with amyotrophic lateral sclerosis and frontotemporal dementia: A cross-sectional study. Lancet Neurol. 2012, 11, 323–330. [Google Scholar] [CrossRef]
- Schludi, M.H.; May, S.; Grasser, F.A.; Rentzsch, K.; Kremmer, E.; Kupper, C.; Klopstock, T.; German Consortium for Frontotemporal Lobar Degeneration; Bavarian Brain Banking Alliance; Arzberger, T.; et al. Distribution of dipeptide repeat proteins in cellular models and C9orf72 mutation cases suggests link to transcriptional silencing. Acta Neuropathol. 2015, 130, 537–555. [Google Scholar] [CrossRef] [PubMed]
- Downey, L.E.; Fletcher, P.D.; Golden, H.L.; Mahoney, C.J.; Agustus, J.L.; Schott, J.M.; Rohrer, J.D.; Beck, J.; Mead, S.; Rossor, M.N.; et al. Altered body schema processing in frontotemporal dementia with C9ORF72 mutations. J. Neurol. Neurosurg. Psychiatry 2014, 85, 1016–1023. [Google Scholar] [CrossRef]
- Ducharme, S.; Bajestan, S.; Dickerson, B.C.; Voon, V. Psychiatric Presentations of C9orf72 Mutation: What Are the Diagnostic Implications for Clinicians? J. Neuropsychiatry Clin. Neurosci. 2017, 29, 195–205. [Google Scholar] [CrossRef] [PubMed]
- Fletcher, P.D.; Downey, L.E.; Golden, H.L.; Clark, C.; Slattery, C.F.; Paterson, R.W.; Rohrer, J.; Schott, J.; Rossor, M.; Warren, J.D. Pain and temperature processing in dementia: A clinical and neuroanatomical analysis. Brain 2015, 138 Pt 11, 3360–3372. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, R.M.; Irish, M.; Henning, E.; Dermody, N.; Bartley, L.; Kiernan, M.C.; Piguet, O.; Farooqi, S.; Hodges, J.R. Assessment of Eating Behavior Disturbance and Associated Neural Networks in Frontotemporal Dementia. JAMA Neurol. 2016, 73, 282–290. [Google Scholar] [CrossRef] [PubMed]
- Bocchetta, M.; Malpetti, M.; Todd, E.G.; Rowe, J.B.; Rohrer, J.D. Looking beneath the surface: The importance of subcortical structures in frontotemporal dementia. Brain Commun. 2021, 3, fcab158. [Google Scholar] [CrossRef] [PubMed]
- Häkkinen, S.; Chu, S.A.; Lee, S.E. Neuroimaging in genetic frontotemporal dementia and amyotrophic lateral sclerosis. Neurobiol. Dis. 2020, 145, 105063. [Google Scholar] [CrossRef] [PubMed]
- Bede, P.; Bokde, A.L.; Byrne, S.; Elamin, M.; McLaughlin, R.L.; Kenna, K.; Fagan, A.J.; Pender, N.; Bradley, D.G.; Hardiman, O. Multiparametric MRI study of ALS stratified for the C9orf72 genotype. Neurology 2013, 81, 361–369. [Google Scholar] [CrossRef]
- Agosta, F.; Ferraro, P.M.; Riva, N.; Spinelli, E.G.; Domi, T.; Carrera, P.; Copetti, M.; Falzone, Y.M.; Ferrari, M.; Lunetta, C.; et al. Structural and functional brain signatures of C9orf72 in motor neuron disease. Neurobiol. Aging 2017, 57, 206–219. [Google Scholar] [CrossRef]
- Westeneng, H.-J.; Walhout, R.; Straathof, M.; Schmidt, R.; Hendrikse, J.; Veldink, J.H.; van den Heuvel, M.P.; van den Berg, L.H. Widespread structural brain involvement in ALS is not limited to theC9orf72repeat expansion. J. Neurol. Neurosurg. Psychiatry 2016, 87, 1354–1360. [Google Scholar] [CrossRef]
- van der Burgh, H.K.; Westeneng, H.J.; Walhout, R.; van Veenhuijzen, K.; Tan, H.H.G.; Meier, J.M.; Bakker, L.A.; Hendrikse, J.; van Es, M.A.; Veldink, J.H.; et al. Multimodal longitudinal study of structural brain involvement in amyotrophic lateral sclerosis. Neurology 2020, 94, e2592–e2604. [Google Scholar] [CrossRef]
- Cedarbaum, J.M.; Stambler, N.; Malta, E.; Fuller, C.; Hilt, D.; Thurmond, B.; Nakanishi, A.; BDNF ALS Study Group (Phase III). The ALSFRS-R: A revised ALS functional rating scale that incorporates assessments of respiratory function. J. Neurol. Sci. 1999, 169, 13–21. [Google Scholar] [CrossRef]
- Kaufmann, P.; Levy, G.; Thompson, J.L.; DelBene, M.L.; Battista, V.; Gordon, P.H.; Rowland, L.P.; Levin, B.; Mitsumoto, H. The ALSFRSr predicts survival time in an ALS clinic population. Neurology 2005, 64, 38–43. [Google Scholar] [CrossRef]
- Rascovsky, K.; Hodges, J.R.; Knopman, D.; Mendez, M.F.; Kramer, J.H.; Neuhaus, J.; Van Swieten, J.C.; Seelaar, H.; Dopper, E.G.P.; Onyike, C.U.; et al. Sensitivity of revised diagnostic criteria for the behavioural variant of frontotemporal dementia. Brain 2011, 134 Pt 9, 2456–2477. [Google Scholar] [CrossRef] [PubMed]
- Strong, M.J.; Abrahams, S.; Goldstein, L.H.; Woolley, S.; Mclaughlin, P.; Snowden, J.; Mioshi, E.; Roberts-South, A.; Benatar, M.; Hortobágyi, T.; et al. Amyotrophic lateral sclerosis-frontotemporal spectrum disorder (ALS-FTSD): Revised diagnostic criteria. Amyotroph. Lateral Scler. Front. Degener. 2017, 18, 153–174. [Google Scholar] [CrossRef]
- Shefner, J.M.; Al-Chalabi, A.; Baker, M.R.; Cui, L.-Y.; de Carvalho, M.; Eisen, A.; Grosskreutz, J.; Hardiman, O.; Henderson, R.; Matamala, J.M.; et al. A proposal for new diagnostic criteria for ALS. Clin. Neurophysiol. 2020, 131, 1975–1978. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, S.; Schubert, S.; Hoon, C.; Mioshi, E.; Hodges, J.R. Validation of the Addenbrooke’s Cognitive Examination III in Frontotemporal Dementia and Alzheimer’s Disease. Dement. Geriatr. Cogn. Disord. 2013, 36, 242–250. [Google Scholar] [CrossRef] [PubMed]
- Scrymgeour-Wedderburn, C.; Wear, H.; Brown, J.; Mason, S.J.; Barker, R.A.; Hodges, J.; Williams-Gray, C. The utility of the Cambridge Behavioural Inventory in neurodegenerative disease. J. Neurol. Neurosurg. Psychiatry 2008, 79, 500–503. [Google Scholar] [CrossRef]
- Cardoso, M.J.; Modat, M.; Wolz, R.; Melbourne, A.; Cash, D.; Rueckert, D.; Ourselin, S. Geodesic Information Flows: Spatially-Variant Graphs and Their Application to Segmentation and Fusion. IEEE Trans. Med. Imaging 2015, 34, 1976–1988. [Google Scholar] [CrossRef]
- Diedrichsen, J.; Balsters, J.; Flavell, J.; Cussans, E.; Ramnani, N. A probabilistic MR atlas of the human cerebellum. NeuroImage 2009, 46, 39–46. [Google Scholar] [CrossRef]
- Diedrichsen, J.; Maderwald, S.; Küper, M.; Thürling, M.; Rabe, K.; Gizewski, E.R.; Ladd, M.; Timmann, D. Imaging the deep cerebellar nuclei: A probabilistic atlas and normalization procedure. NeuroImage 2011, 54, 1786–1794. [Google Scholar] [CrossRef]
- Iglesias, J.E.; Insausti, R.; Lerma-Usabiaga, G.; Bocchetta, M.; Van Leemput, K.; Greve, D.N.; van der Kouwe, A.; Fischl, B.; Caballero-Gaudes, C.; Paz-Alonso, P.M. A probabilistic atlas of the human thalamic nuclei combining ex vivo MRI and histology. NeuroImage 2018, 183, 314–326. [Google Scholar] [CrossRef] [PubMed]
- Malone, I.B.; Leung, K.K.; Clegg, S.; Barnes, J.; Whitwell, J.L.; Ashburner, J.; Fox, N.; Ridgway, G. Accurate automatic estimation of total intracranial volume: A nuisance variable with less nuisance. NeuroImage 2015, 104, 366–372. [Google Scholar] [CrossRef]
- Ahmed, R.M.; Bocchetta, M.; Todd, E.G.; Tse, N.Y.; Devenney, E.M.; Tu, S.; Caga, J.; Hodges, J.R.; Halliday, G.M.; Irish, M.; et al. Tackling clinical heterogeneity across the ALS-FTD spectrum using a transdiagnostic approach. Brain Commun. 2021, 3, fcab257. [Google Scholar] [CrossRef] [PubMed]
- Chipika, R.H.; Finegan, E.; Shing, S.L.H.; McKenna, M.C.; Christidi, F.; Chang, K.M.; Doherty, M.; Hengeveld, J.C.; Vajda, A.; Pender, N.; et al. “Switchboard” malfunction in motor neuron diseases: Selective pathology of thalamic nuclei in amyotrophic lateral sclerosis and primary lateral sclerosis. NeuroImage Clin. 2020, 27, 102300. [Google Scholar] [CrossRef] [PubMed]
- Tu, S.; Menke, R.A.L.; Talbot, K.; Kiernan, M.C.; Turner, M.R. Regional thalamic MRI as a marker of widespread cortical pathology and progressive frontotemporal involvement in amyotrophic lateral sclerosis. J. Neurol. Neurosurg. Psychiatry 2018, 89, 1250–1258. [Google Scholar] [CrossRef] [PubMed]
- Hwang, K.; Bertolero, M.; Liu, W.B.; D’Esposito, M. The Human Thalamus Is an Integrative Hub for Functional Brain Networks. J. Neurosci. 2017, 37, 5594–5607. [Google Scholar] [CrossRef]
- Schmahmann, J.D. Vascular Syndromes of the Thalamus. Stroke 2003, 34, 2264–2278. [Google Scholar] [CrossRef]
- Lee, S.E.; Khazenzon, A.M.; Trujillo, A.J.; Guo, C.; Yokoyama, J.S.; Sha, S.J.; Takada, L.; Karydas, A.M.; Block, N.; Coppola, G.; et al. Altered network connectivity in frontotemporal dementia with C9orf72 hexanucleotide repeat expansion. Brain 2014, 137 Pt 11, 3047–3060. [Google Scholar] [CrossRef]
- Dermody, N.; Hornberger, M.; Piguet, O.; Hodges, J.R.; Irish, M. Prospective Memory Impairments in Alzheimer’s Disease and Behavioral Variant Frontotemporal Dementia: Clinical and Neural Correlates. J. Alzheimer’s Dis. 2016, 50, 425–441. [Google Scholar] [CrossRef]
- Bocchetta, M.; Iglesias, J.E.; Neason, M.; Cash, D.M.; Warren, J.; Rohrer, J. Thalamic nuclei in frontotemporal dementia: Mediodorsal nucleus involvement is universal but pulvinar atrophy is unique to C9orf72. Hum. Brain Mapp. 2020, 41, 1006–1016. [Google Scholar] [CrossRef] [PubMed]
- Radanovic, M.; Rosemberg, S.; Adas, R.; Miranda, S.C.; Caramelli, P.; Caixeta, L.; Nitrini, R. Frontotemporal dementia with severe thalamic involvement: A clinical and neuropathological study. Arq. Neuro-Psiquiatr. 2003, 61, 930–935. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Spinelli, E.G.; Ghirelli, A.; Basaia, S.; Cividini, C.; Riva, N.; Canu, E.; Castelnovo, V.; Domi, T.; Magnani, G.; Caso, F.; et al. Structural MRI Signatures in Genetic Presentations of the Frontotemporal Dementia-Motor Neuron Disease Spectrum. Neurology 2021, 97, e1594–e1607. [Google Scholar] [CrossRef] [PubMed]
- Cykowski, M.D.; Takei, H.; Van Eldik, L.J.; Schmitt, F.A.; Jicha, G.A.; Powell, S.Z.; Nelson, P.T. Hippocampal Sclerosis but Not Normal Aging or Alzheimer Disease Is Associated With TDP-43 Pathology in the Basal Forebrain of Aged Persons. J. Neuropathol. Exp. Neurol. 2016, 75, 397–407. [Google Scholar] [CrossRef] [PubMed]
- Irwin, D.; McMillan, C.; Brettschneider, J.; Libon, D.J.; Powers, J.; Rascovsky, K.; Toledo, J.; Boller, A.; Bekisz, J.; Chandrasekaran, K.; et al. Cognitive decline and reduced survival inC9orf72expansion frontotemporal degeneration and amyotrophic lateral sclerosis. J. Neurol. Neurosurg. Psychiatry 2013, 84, 163–169. [Google Scholar] [CrossRef] [PubMed]
- Vatsavayai, S.C.; Yoon, S.J.; Gardner, R.C.; Gendron, T.F.; Vargas, J.N.S.; Trujillo, A.; Pribadi, M.; Phillips, J.J.; Gaus, S.E.; Hixson, J.D.; et al. Timing and significance of pathological features in C9orf72 expansion-associated frontotemporal dementia. Brain 2016, 139 Pt 12, 3202–3216. [Google Scholar] [CrossRef]
- Yang, Y.; Halliday, G.M.; Hodges, J.R.; Tan, R.H. von Economo Neuron Density and Thalamus Volumes in Behavioral Deficits in Frontotemporal Dementia Cases with and without a C9ORF72 Repeat Expansion. J. Alzheimer’s Dis. 2017, 58, 701–709. [Google Scholar] [CrossRef]
- Devenney, E.M.; Landin-Romero, R.; Irish, M.; Hornberger, M.; Mioshi, E.; Halliday, G.M.; Kiernan, M.C.; Hodges, J.R. The neural correlates and clinical characteristics of psychosis in the frontotemporal dementia continuum and the C9orf72 expansion. NeuroImage Clin. 2017, 13, 439–445. [Google Scholar] [CrossRef]
- Convery, R.S.; Bocchetta, M.; Greaves, C.V.; Moore, K.M.; Cash, D.M.; Van Swieten, J.; Moreno, F.; Sánchez-Valle, R.; Borroni, B.; Laforce, R., Jr.; et al. Abnormal pain perception is associated with thalamo-cortico-striatal atrophy in C9orf72 expansion carriers in the GENFI cohort. J. Neurol. Neurosurg. Psychiatry 2020, 91, 1325–1328. [Google Scholar] [CrossRef]
- Bede, P.; Omer, T.; Finegan, E.; Chipika, R.H.; Iyer, P.M.; Doherty, M.; Vajda, A.; Pender, N.; McLaughlin, R.; Hutchinson, S.; et al. Connectivity-based characterisation of subcortical grey matter pathology in frontotemporal dementia and ALS: A multimodal neuroimaging study. Brain Imaging Behav. 2018, 12, 1696–1707. [Google Scholar] [CrossRef]
- Tan, R.H.; Devenney, E.; Dobson-Stone, C.; Kwok, J.B.; Hodges, J.R.; Kiernan, M.C.; Halliday, G.M.; Hornberger, M. Cerebellar Integrity in the Amyotrophic Lateral Sclerosis-Frontotemporal Dementia Continuum. PLoS ONE 2014, 9, e105632. [Google Scholar] [CrossRef]
- Chen, Y.; Kumfor, F.; Landin-Romero, R.; Irish, M.; Piguet, O. The Cerebellum in Frontotemporal Dementia: A Meta-Analysis of Neuroimaging Studies. Neuropsychol. Rev. 2019, 29, 450–464. [Google Scholar] [CrossRef]
- Palesi, F.; Tournier, J.-D.; Calamante, F.; Muhlert, N.; Castellazzi, G.; Chard, D.; D’Angelo, E.; Wheeler-Kingshott, C.A.M. Contralateral cerebello-thalamo-cortical pathways with prominent involvement of associative areas in humans in vivo. Brain Struct. Funct. 2015, 220, 3369–3384. [Google Scholar] [CrossRef]
- Makris, N.; Hodge, S.M.; Haselgrove, C.; Kennedy, D.N.; Dale, A.; Fischl, B.; Rosen, B.R.; Harris, G.; Caviness, V.S., Jr.; Schmahmann, J.D. Human Cerebellum: Surface-Assisted Cortical Parcellation and Volumetry with Magnetic Resonance Imaging. J. Cogn. Neurosci. 2003, 15, 584–599. [Google Scholar] [CrossRef] [PubMed]
- Whitwell, J.L.; Weigand, S.D.; Boeve, B.F.; Senjem, M.L.; Gunter, J.L.; DeJesus-Hernandez, M.; Rutherford, N.J.; Baker, M.; Knopman, D.S.; Wszolek, Z.K.; et al. Neuroimaging signatures of frontotemporal dementia genetics: C9ORF72, tau, progranulin and sporadics. Brain 2012, 135 Pt 3, 794–806. [Google Scholar] [CrossRef] [PubMed]
- Sha, S.J.; Takada, L.T.; Rankin, K.P.; Yokoyama, J.S.; Rutherford, N.J.; Fong, J.C.; Khan, B.; Karydas, A.; Baker, M.C.; DeJesus-Hernandez, M.; et al. Frontotemporal dementia due to C9ORF72 mutations: Clinical and imaging features. Neurology 2012, 79, 1002–1011. [Google Scholar] [CrossRef]
- Schönecker, S.; Neuhofer, C.M.; Otto, M.; Ludolph, A.; Kassubek, J.; Landwehrmeyer, G.B.; Anderl-Straub, S.; Semler, E.; Diehl-Schmid, J.; Prix, C.; et al. Atrophy in the Thalamus but not Cerebellum Is Specific for C9orf72 FTD and ALS Patients—An Atlas-Based Volumetric MRI Study. Front. Aging Neurosci. 2018, 10, 45. [Google Scholar] [CrossRef]
- Chen, Y.; Kumfor, F.; Landin-Romero, R.; Irish, M.; Hodges, J.R.; Piguet, O. Cerebellar atrophy and its contribution to cognition in frontotemporal dementias. Ann. Neurol. 2018, 84, 98–109. [Google Scholar] [CrossRef]
- Saalmann, Y.B.; Kastner, S. The cognitive thalamus. Front. Syst. Neurosci. 2015, 9, 39. [Google Scholar] [CrossRef]
- Tan, R.H.; Devenney, E.; Kiernan, M.C.; Halliday, G.M.; Hodges, J.R.; Ehornberger, M. Terra incognita—Cerebellar contributions to neuropsychiatric and cognitive dysfunction in behavioral variant frontotemporal dementia. Front. Aging Neurosci. 2015, 7, 121. [Google Scholar] [CrossRef]
- Behrens, T.E.J.; Johansen-Berg, H.; Woolrich, M.W.; Smith, S.M.; Wheeler-Kingshott, C.A.M.; Boulby, P.A.; Barker, G.J.; Sillery, E.L.; Sheehan, K.; Ciccarelli, O.; et al. Non-invasive mapping of connections between human thalamus and cortex using diffusion imaging. Nat. Neurosci. 2003, 6, 750–757. [Google Scholar] [CrossRef] [PubMed]
| Controls (n = 57) | bvFTD (n = 58) | ALS–FTD (n = 41) | ALS (n = 52) | |
|---|---|---|---|---|
| Sex (M/F) | 25/32 | 38/20 | 31/10 | 42/10 |
| Age (years) | 64.2 (10.9) | 61.7 (8.2) | 64.5 (8.3) | 60.3 (10.7) |
| Education (years) | 13.4 (2.6) | 12.4 (3.1) | 12.7 (3.2) | 13.0 (2.6) |
| Disease duration (months) | -- | 61.0 (49.5) | 32.9 (22.6) | 28.0 (27.6) |
| C9orf72 expansion carriers (number) | -- | 17 | 12 | 2 |
| Carriers of mutations in other genes (number) | -- | 3 GRN, 1 MAPT | 0 | 1 SOD1 |
| ALSFRS-R score (/45) | -- | -- | 41 | 42 |
| ACE III total score (/100) | 94.6 (3.4) | 77.1 (15.7) | 72.0 (14.4) | 92.4 (5.5) |
| ACE—Attention (/18) | 17.2 (0.9) | 14.9 (2.9) | 15.3 (2.6) | 17.0 (1.4) |
| ACE—Memory (/26) | 24.7 (1.6) | 190 (5.3) | 19.0 (5.2) | 23.2 (4.3) |
| ACE—Fluency (/14) | 12.1 (1.6) | 6.9 (4.0) | 5.0 (3.7) | 11.3 (1.8) |
| ACE—Language (/26) | 25.1 (0.9) | 22.4 (4.3) | 19.3 (4.6) | 24.5 (2.0) |
| ACE—Visuospatial (/16) | 15.5 (0.9) | 14.0 (2.6) | 13.7 (2.1) | 15.5 (0.9) |
| CBI-R total score (/180) | -- | 65.2 (29.2) | 44.2 (30.9) | 25.5 (20.4) |
| Memory | -- | 43.3 (21.4) | 34.7(23.8) | 12.1 (12.9) |
| Everyday skills | -- | 31.0 (25.9) | 20.9 (20.4) | 18.0 (30.0) |
| Self-care skills | -- | 16.3 (25.7) | 8.5 (16.4) | 22.7 (31.3) |
| Mood changes | -- | 29.6 (22.2) | 21.3 (20.4) | 16.9 (15.7) |
| Odd beliefs | -- | 10.1 (17.2) | 5.41 (12.61) | 0.2 (1.4) |
| Abnormal behaviours | -- | 36.6 (23.4) | 22.9 (22.4) | 8.5 (12.2) |
| Eating habits | -- | 41.6 (30.5) | 23.7(28.0) | 8.6 (12.2) |
| Sleep | -- | 43.8 (25.0) | 27.7(26.0) | 34.1 (27.5) |
| Stereotypic and motor behaviours | -- | 41.5 (28.9) | 34.6(30.7) | 8.6 (12.7) |
| Reduced motivation | -- | 58.9 (30.1) | 34.8(29.0) | 13.6 (17.3) |
| Thalamus | Cerebellum | |||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Clinical Diagnosis | AV | LD | LP | VA | VLa | VLp | VPL | VM | Intralaminar | Midline | MD | LGN | MGN | Pulvinar | Whole | I–IV | V | VI | VIIa-CI | VIIa-CII | VIIb | VIIIa | VIIIb | IX | X | DN | IN | FN | Whole | |
| bvFTD (n = 58) | Mean | −1.14 | −4.61 | −1.53 | −1.13 | −0.85 | −0.73 | −0.29 | −0.05 | −0.72 | −1.12 | −1.96 | −1.13 | −1.03 | −1.15 | −1.42 | −0.29 | −0.34 | −0.41 | −0.38 | −0.52 | −0.73 | −0.82 | −0.09 | −0.18 | 0.18 | −0.32 | −0.10 | 0.02 | −0.60 |
| SD | 1.06 | 0.46 | 1.11 | 1.06 | 0.94 | 1.00 | 1.07 | 1.08 | 0.85 | 1.19 | 1.18 | 1.05 | 0.82 | 0.93 | 0.77 | 1.12 | 1.00 | 1.17 | 1.07 | 1.10 | 1.32 | 1.16 | 1.01 | 0.87 | 0.98 | 1.12 | 1.13 | 1.04 | 1.02 | |
| p-value | 0.001 | 0.001 | 0.001 | 0.001 | 0.001 | 0.001 | 0.044 | 0.716 | 0.001 | 0.001 | 0.001 | 0.001 | 0.001 | 0.001 | 0.001 | 0.062 | 0.016 | 0.008 | 0.008 | 0.001 | 0.001 | 0.001 | 0.500 | 0.149 | 0.191 | 0.043 | 0.510 | 0.913 | 0.001 | |
| ALS–FTD (n = 41) | Mean | −1.36 | −4.74 | −1.03 | −1.41 | −1.14 | −1.02 | −0.59 | −0.34 | −1.08 | −1.54 | −2.00 | −0.58 | −0.94 | −0.91 | −1.49 | −0.19 | −0.17 | −0.41 | −0.29 | −0.57 | −0.63 | −0.48 | −0.16 | −0.17 | 0.18 | −0.81 | −0.47 | −0.30 | −0.53 |
| SD | 0.76 | 0.38 | 0.91 | 1.14 | 1.01 | 0.97 | 1.00 | 0.93 | 0.75 | 0.81 | 1.08 | 1.40 | 1.27 | 1.27 | 1.03 | 1.08 | 0.98 | 0.98 | 0.99 | 1.08 | 1.71 | 1.55 | 0.94 | 0.95 | 1.00 | 1.07 | 0.97 | 0.80 | 1.09 | |
| p-value | 0.001 | 0.001 | 0.001 | 0.001 | 0.001 | 0.001 | 0.001 | 0.040 | 0.001 | 0.001 | 0.001 | 0.015 | 0.001 | 0.001 | 0.001 | 0.272 | 0.297 | 0.005 | 0.058 | 0.003 | 0.028 | 0.063 | 0.316 | 0.253 | 0.281 | 0.001 | 0.003 | 0.027 | 0.007 | |
| ALS (n = 52) | Mean | −0.78 | −4.66 | −0.05 | −0.99 | −0.49 | −0.19 | 0.46 | 0.74 | −0.02 | −0.43 | −0.29 | 1.30 | −0.09 | 0.46 | −0.01 | 0.74 | 1.00 | 0.10 | 0.35 | 0.05 | 1.14 | 1.34 | 0.34 | 0.58 | 0.40 | 0.09 | −0.29 | −0.30 | 0.69 |
| SD | 0.72 | 0.48 | 0.89 | 0.90 | 1.08 | 1.05 | 1.15 | 1.03 | 0.71 | 0.65 | 0.86 | 1.44 | 1.08 | 1.18 | 0.88 | 0.82 | 0.97 | 1.34 | 1.23 | 1.00 | 1.39 | 1.22 | 0.95 | 1.15 | 0.89 | 1.42 | 1.31 | 1.32 | 1.17 | |
| p-value | 0.001 | 0.001 | 0.706 | 0.001 | 0.002 | 0.178 | 0.004 | 0.001 | 0.821 | 0.001 | 0.023 | 0.001 | 0.537 | 0.014 | 0.930 | 0.001 | 0.001 | 0.604 | 0.053 | 0.735 | 0.001 | 0.001 | 0.011 | 0.002 | 0.003 | 0.617 | 0.117 | 0.114 | 0.001 | |
| Genetic subgroups | AV | LD | LP | VA | VLa | VLp | VPL | VM | Intralaminar | Midline | MD | LGN | MGN | Pulvinar | Whole | I–IV | V | VI | VIIa-CI | VIIa-CII | VIIb | VIIIa | VIIIb | IX | X | DN | IN | FN | Whole | |
| bvFTD sporadic (n = 41) | Mean | −1.04 | −4.62 | −1.43 | −1.16 | −0.77 | −0.66 | −0.32 | 0.00 | −0.65 | −0.93 | −1.74 | −1.08 | −1.08 | −0.95 | −1.27 | −0.26 | −0.30 | −0.50 | −0.30 | −0.36 | −0.61 | −0.74 | −0.03 | −0.06 | 0.18 | −0.37 | −0.04 | 0.15 | −0.50 |
| SD | 1.07 | 0.44 | 1.00 | 1.12 | 0.91 | 1.00 | 1.14 | 1.18 | 0.92 | 1.32 | 1.18 | 1.00 | 0.91 | 0.85 | 0.76 | 1.15 | 0.89 | 1.03 | 0.97 | 1.05 | 1.41 | 1.29 | 1.09 | 0.81 | 0.86 | 1.18 | 1.12 | 1.04 | 0.98 | |
| p-value | 0.001 | 0.001 | 0.001 | 0.001 | 0.001 | 0.001 | 0.072 | 0.990 | 0.002 | 0.001 | 0.001 | 0.001 | 0.001 | 0.001 | 0.001 | 0.164 | 0.043 | 0.007 | 0.058 | 0.044 | 0.012 | 0.006 | 0.848 | 0.621 | 0.187 | 0.047 | 0.809 | 0.387 | 0.004 | |
| bvFTD C9orf72 (n = 12) | Mean | −1.49 | −4.62 | −1.93 | −0.79 | −0.93 | −0.88 | −0.17 | −0.09 | −0.94 | −1.54 | −2.42 | −1.28 | −0.82 | −1.74 | −1.74 | −0.23 | −0.55 | −0.36 | −0.59 | −0.99 | −1.15 | −1.15 | −0.17 | −0.51 | 0.05 | −0.20 | −0.29 | −0.44 | −0.92 |
| SD | 0.97 | 0.53 | 1.23 | 0.95 | 1.04 | 1.06 | 0.99 | 0.85 | 0.65 | 0.64 | 1.10 | 1.01 | 0.55 | 0.89 | 0.81 | 1.13 | 1.39 | 1.34 | 1.40 | 1.33 | 1.24 | 0.78 | 0.61 | 1.05 | 1.31 | 1.12 | 1.17 | 1.12 | 1.15 | |
| p-value | 0.003 | 0.001 | 0.001 | 0.015 | 0.012 | 0.014 | 0.549 | 0.703 | 0.003 | 0.001 | 0.002 | 0.006 | 0.004 | 0.001 | 0.001 | 0.491 | 0.189 | 0.335 | 0.145 | 0.056 | 0.011 | 0.002 | 0.352 | 0.118 | 0.914 | 0.541 | 0.396 | 0.174 | 0.012 | |
| ALS–FTD sporadic (n = 29) | Mean | −1.25 | −4.74 | −0.96 | −1.38 | −1.09 | −0.92 | −0.43 | −0.23 | −1.06 | −1.61 | −1.78 | −0.15 | −0.66 | −0.45 | −1.21 | 0.04 | −0.02 | −0.43 | −0.43 | −0.41 | −0.51 | −0.43 | −0.03 | −0.23 | 0.14 | −0.81 | −0.45 | −0.41 | −0.46 |
| SD | 0.77 | 0.41 | 0.99 | 0.89 | 0.78 | 0.80 | 0.91 | 0.85 | 0.74 | 0.88 | 1.07 | 1.06 | 1.02 | 0.99 | 0.80 | 1.12 | 0.98 | 1.09 | 1.00 | 1.09 | 1.79 | 1.42 | 1.00 | 1.03 | 1.05 | 1.16 | 0.90 | 0.78 | 1.14 | |
| p-value | 0.001 | 0.001 | 0.001 | 0.001 | 0.001 | 0.001 | 0.021 | 0.170 | 0.001 | 0.001 | 0.001 | 0.486 | 0.001 | 0.021 | 0.001 | 0.864 | 0.894 | 0.052 | 0.046 | 0.054 | 0.144 | 0.121 | 0.858 | 0.230 | 0.506 | 0.002 | 0.010 | 0.013 | 0.050 | |
| ALS–FTD C9orf72 (n = 12) | Mean | −1.61 | −4.74 | −1.19 | −1.49 | −1.28 | −1.24 | −0.99 | −0.60 | −1.12 | −1.39 | −2.53 | −1.63 | −1.60 | −2.02 | −2.16 | −0.75 | −0.51 | −0.38 | 0.03 | −0.99 | −0.92 | −0.59 | −0.46 | −0.05 | 0.27 | −0.83 | −0.52 | −0.04 | −0.71 |
| SD | 0.69 | 0.31 | 0.68 | 1.64 | 1.45 | 1.32 | 1.13 | 1.11 | 0.81 | 0.62 | 0.95 | 1.59 | 1.60 | 1.22 | 1.23 | 0.74 | 0.95 | 0.67 | 0.92 | 0.99 | 1.53 | 1.91 | 0.74 | 0.72 | 0.91 | 0.85 | 1.15 | 0.81 | 1.01 | |
| p-value | 0.001 | 0.001 | 0.002 | 0.051 | 0.063 | 0.031 | 0.020 | 0.087 | 0.004 | 0.003 | 0.002 | 0.015 | 0.069 | 0.004 | 0.002 | 0.009 | 0.107 | 0.073 | 0.896 | 0.013 | 0.079 | 0.345 | 0.067 | 0.829 | 0.344 | 0.010 | 0.199 | 0.864 | 0.056 | |
| ALS sporadic (n = 49) | Mean | −0.75 | −4.67 | −0.01 | −0.98 | −0.46 | −0.16 | 0.51 | 0.78 | −0.01 | −0.45 | −0.26 | 1.44 | −0.03 | 0.57 | 0.06 | 0.76 | 1.04 | 0.16 | 0.31 | 0.03 | 1.13 | 1.34 | 0.31 | 0.61 | 0.39 | 0.10 | −0.31 | −0.32 | 0.70 |
| SD | 0.72 | 0.49 | 0.91 | 0.92 | 1.07 | 1.05 | 1.15 | 1.02 | 0.72 | 0.67 | 0.82 | 1.33 | 1.05 | 1.09 | 0.82 | 0.83 | 0.97 | 1.36 | 1.25 | 1.03 | 1.41 | 1.25 | 0.94 | 1.17 | 0.91 | 1.45 | 1.34 | 1.36 | 1.20 | |
| p-value | 0.001 | 0.001 | 0.938 | 0.001 | 0.012 | 0.317 | 0.008 | 0.001 | 0.961 | 0.001 | 0.029 | 0.001 | 0.827 | 0.002 | 0.630 | 0.001 | 0.001 | 0.404 | 0.095 | 0.834 | 0.001 | 0.001 | 0.019 | 0.001 | 0.005 | 0.618 | 0.117 | 0.108 | 0.002 | |
| ALS C9orf72 (n = 2) | Mean | −1.01 | −4.42 | −0.57 | −0.84 | −0.71 | −0.58 | −0.76 | −0.24 | −0.28 | −0.27 | −1.42 | −1.67 | −1.57 | −1.69 | −1.43 | 0.38 | 0.56 | −0.70 | 1.37 | 0.38 | 1.72 | 1.16 | 0.27 | −0.10 | 0.38 | −0.07 | 0.25 | 0.05 | 0.83 |
| SD | 0.68 | 0.44 | 0.11 | 0.38 | 1.73 | 1.43 | 1.08 | 1.22 | 0.84 | 0.18 | 1.33 | 1.18 | 1.51 | 1.64 | 1.53 | 1.05 | 0.06 | 0.95 | 0.16 | 0.60 | 1.16 | 0.70 | 1.01 | 0.06 | 0.87 | 1.34 | 0.91 | 0.54 | 0.39 | |
| Thalamus | Cerebellum | |||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Clinical Diagnosis | AV | LD | LP | VA | VLa | VLp | VPL | VM | Intralaminar | Midline | MD | LGN | MGN | Pulvinar | Whole | I–IV | V | VI | VIIa-CI | VIIa-CII | VIIb | VIIIa | VIIIb | IX | X | DN | IN | FN | Whole | |
| bvFTD | ALS–FTD | 0.673 | 0.446 | 0.041 | 0.514 | 0.481 | 0.494 | 0.524 | 0.504 | 0.071 | 0.080 | 1.000 | 0.119 | 1.000 | 0.891 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | 1.000 | 0.611 | 1.000 | 1.000 | 1.000 | 0.141 | 0.361 | 0.467 | 1.000 |
| ALS | 0.099 | 1.000 | <0.0005 | 1.000 | 0.186 | 0.019 | 0.001 | <0.0005 | <0.0005 | 0.001 | <0.0005 | <0.0005 | <0.0005 | <0.0005 | <0.0005 | <0.0005 | <0.0005 | 0.075 | 0.002 | 0.018 | <0.0005 | <0.0005 | 0.069 | <0.0005 | 0.697 | 0.242 | 1.000 | 0.379 | <0.0005 | |
| ALS–FTD | ALS | 0.006 | 1.000 | <0.0005 | 0.150 | 0.007 | <0.0005 | <0.0005 | <0.0005 | <0.0005 | <0.0005 | <0.0005 | <0.0005 | <0.0005 | <0.0005 | <0.0005 | <0.0005 | <0.0005 | 0.118 | 0.020 | 0.017 | <0.0005 | <0.0005 | 0.047 | 0.001 | 0.797 | 0.001 | 1.000 | 1.000 | <0.0005 |
| Genetic vs. sporadic | AV | LD | LP | VA | VLa | VLp | VPL | VM | Intralaminar | Midline | MD | LGN | MGN | Pulvinar | Whole | I–IV | V | VI | VIIa-CI | VIIa-CII | VIIb | VIIIa | VIIIb | IX | X | DN | IN | FN | Whole | |
| bvFTD | p-value | 0.160 | 0.973 | 0.184 | 0.252 | 0.588 | 0.500 | 0.656 | 0.774 | 0.216 | 0.023 | 0.064 | 0.542 | 0.192 | 0.009 | 0.066 | 0.919 | 0.551 | 0.728 | 0.521 | 0.139 | 0.214 | 0.182 | 0.547 | 0.197 | 0.728 | 0.659 | 0.497 | 0.098 | 0.247 |
| ALS–FTD | p-value | 0.157 | 0.968 | 0.427 | 0.838 | 0.696 | 0.469 | 0.136 | 0.303 | 0.830 | 0.368 | 0.029 | 0.005 | 0.070 | 0.002 | 0.017 | 0.014 | 0.130 | 0.879 | 0.154 | 0.103 | 0.451 | 0.806 | 0.141 | 0.533 | 0.645 | 0.947 | 0.860 | 0.194 | 0.478 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bocchetta, M.; Todd, E.G.; Tse, N.Y.; Devenney, E.M.; Tu, S.; Caga, J.; Hodges, J.R.; Halliday, G.M.; Irish, M.; Piguet, O.; et al. Thalamic and Cerebellar Regional Involvement across the ALS–FTD Spectrum and the Effect of C9orf72. Brain Sci. 2022, 12, 336. https://doi.org/10.3390/brainsci12030336
Bocchetta M, Todd EG, Tse NY, Devenney EM, Tu S, Caga J, Hodges JR, Halliday GM, Irish M, Piguet O, et al. Thalamic and Cerebellar Regional Involvement across the ALS–FTD Spectrum and the Effect of C9orf72. Brain Sciences. 2022; 12(3):336. https://doi.org/10.3390/brainsci12030336
Chicago/Turabian StyleBocchetta, Martina, Emily G. Todd, Nga Yan Tse, Emma M. Devenney, Sicong Tu, Jashelle Caga, John R. Hodges, Glenda M. Halliday, Muireann Irish, Olivier Piguet, and et al. 2022. "Thalamic and Cerebellar Regional Involvement across the ALS–FTD Spectrum and the Effect of C9orf72" Brain Sciences 12, no. 3: 336. https://doi.org/10.3390/brainsci12030336
APA StyleBocchetta, M., Todd, E. G., Tse, N. Y., Devenney, E. M., Tu, S., Caga, J., Hodges, J. R., Halliday, G. M., Irish, M., Piguet, O., Kiernan, M. C., Rohrer, J. D., & Ahmed, R. M. (2022). Thalamic and Cerebellar Regional Involvement across the ALS–FTD Spectrum and the Effect of C9orf72. Brain Sciences, 12(3), 336. https://doi.org/10.3390/brainsci12030336







