Association of Severe Retinopathy of Prematurity and Bronchopulmonary Dysplasia with Adverse Neurodevelopmental Outcomes in Preterm Infants without Severe Brain Injury
Abstract
1. Introduction
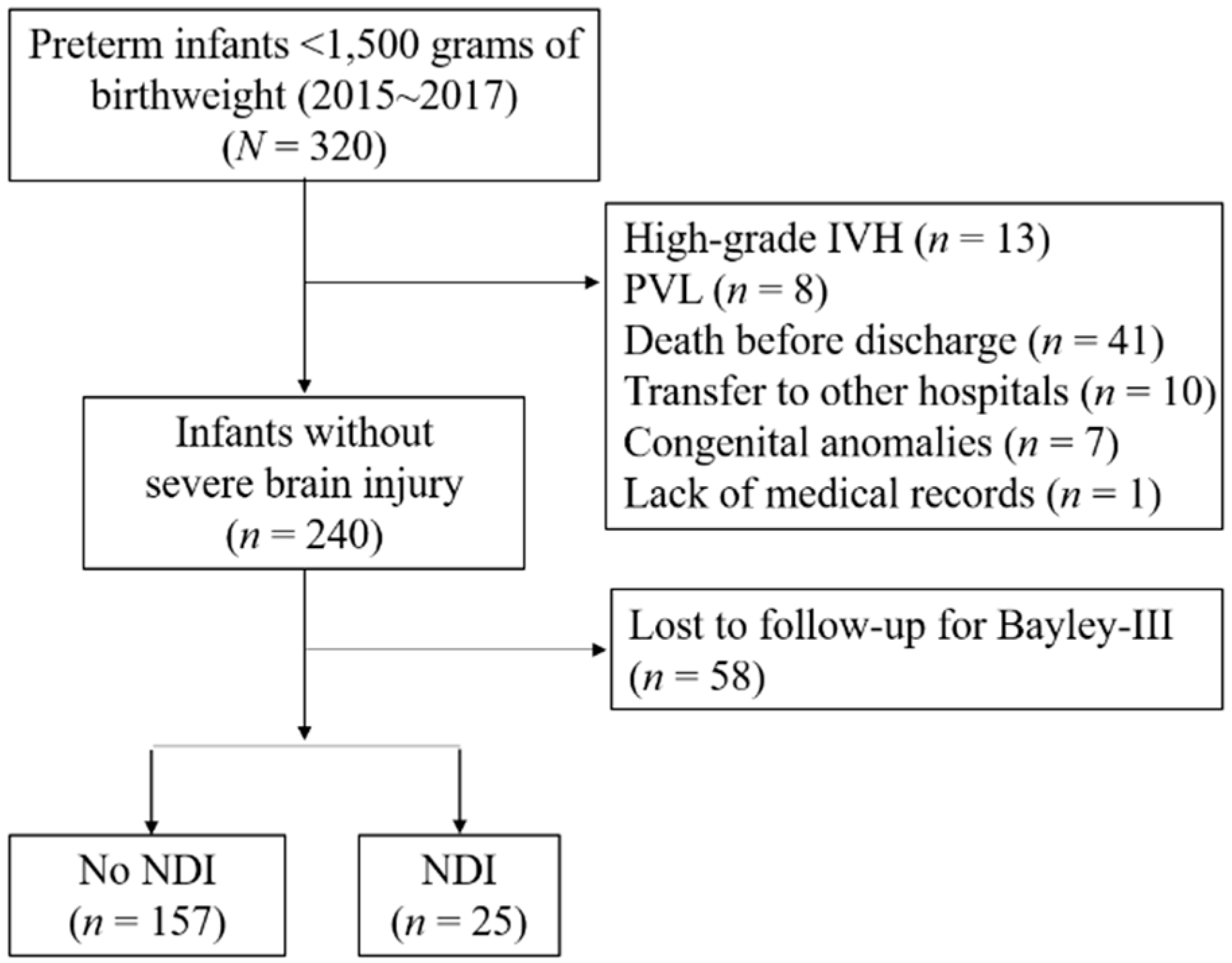
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bolisetty, S.; Dhawan, A.; Abdel-Latif, M.; Bajuk, B.; Stack, J.; Oei, J.-L.; Lui, K.; New South Wales and Australian Capital Territory Neonatal Intensive Care Units Data Collection. Intraventricular hemorrhage and neurodevelopmental outcomes in extreme preterm infants. Pediatrics 2014, 133, 55–62. [Google Scholar] [CrossRef] [PubMed]
- O’Shea, T.M.; Kuban, K.C.K.; Allred, E.N.; Paneth, N.; Pagano, M.; Dammann, O.; Bostic, L.; Brooklier, K.; Butler, S.; Goldstein, D.J.; et al. Neonatal cranial ultrasound lesions and developmental delays at 2 years of age among extremely low gestational age children. Pediatrics 2008, 122, e662–e669. [Google Scholar] [CrossRef] [PubMed]
- Adams-Chapman, I.; Hansen, N.I.; Stoll, B.J.; Higgins, R. For the NICHD research network neurodevelopmental outcome of extremely low birth weight infants with posthemorrhagic hydrocephalus requiring shunt insertion. Pediatrics 2008, 121, e1167–e1177. [Google Scholar] [CrossRef]
- Lee, J.; Hong, M.; Yum, S.K.; Lee, J.H. Perinatal prediction model for severe intraventricular hemorrhage and the effect of early postnatal acidosis. Child’s Nerv. Syst. 2018, 34, 2215–2222. [Google Scholar] [CrossRef] [PubMed]
- Sherlock, R.; Anderson, P.; Doyle, L. Neurodevelopmental sequelae of intraventricular haemorrhage at 8 years of age in a regional cohort of ELBW/very preterm infants. Early Hum. Dev. 2005, 81, 909–916. [Google Scholar] [CrossRef] [PubMed]
- Reubsaet, P.; Brouwer, A.J.; Van Haastert, I.C.; Brouwer, M.J.; Koopman, C.; Groenendaal, F.; De Vries, L.S. The impact of low-grade germinal matrix-intraventricular hemorrhage on neurodevelopmental outcome of very preterm infants. Neonatology 2017, 112, 203–210. [Google Scholar] [CrossRef]
- Klebermass-Schrehof, K.; Czaba, C.; Olischar, M.; Fuiko, R.; Waldhoer, T.; Rona, Z.; Pollak, A.; Weninger, M. Impact of low-grade intraventricular hemorrhage on long-term neurodevelopmental outcome in preterm infants. Child’s Nerv. Syst. 2012, 28, 2085–2092. [Google Scholar] [CrossRef] [PubMed]
- Ancel, P.-Y.; Livinec, F.; Larroque, B.; Marret, S.; Arnaud, C.; Pierrat, V.; Dehan, M.; N′guyen, S.; Escande, B.; Burguet, A.; et al. Cerebral Palsy among very preterm children in relation to gestational age and neonatal ultrasound abnormalities: The EPIPAGE cohort study. Pediatrics 2006, 117, 828–835. [Google Scholar] [CrossRef] [PubMed]
- Patra, K.; Wilson-Costello, D.; Taylor, H.G.; Mercuri-Minich, N.; Hack, M. Grades I-II intraventricular hemorrhage in extremely low birth weight infants: Effects on neurodevelopment. J. Pediatr. 2006, 149, 169–173. [Google Scholar] [CrossRef] [PubMed]
- Bendersky, M.; Lewis, M. Effects of intraventricular hemorrhage and other medical and environmental risks on multiple out-comes at age three years. J. Dev. Behav. Pediatr. 1995, 16, 89–96. [Google Scholar] [CrossRef] [PubMed]
- Pinto-Martin, J.A.; Whitaker, A.H.; Feldman, J.F.; Van Rossem, R.; Paneth, N. Relation of cranial ultrasound abnormalities in low-birthweight infants to motor or cognitive performance at ages 2, 6, and 9 years. Dev. Med. Child Neurol. 1999, 41, 826–833. [Google Scholar] [CrossRef] [PubMed]
- Stoll, B.J.; Hansen, N.I.; Adams-Chapman, I.; Fanaroff, A.A.; Hintz, S.R.; Vohr, B.; Higgins, R.D. For the National Institute of Child Health and human development neonatal research network neurodevelopmental and growth impairment among extremely low-birth-weight infants with neonatal infection. JAMA 2004, 292, 2357–2365. [Google Scholar] [CrossRef]
- Shah, D.K.; Doyle, L.W.; Anderson, P.J.; Bear, M.; Daley, A.J.; Hunt, R.W.; Inder, T.E. Adverse neurodevelopment in preterm infants with postnatal sepsis or necrotizing enterocolitis is mediated by white matter abnormalities on magnetic resonance imaging at term. J. Pediatr. 2008, 153, 170–175.e1. [Google Scholar] [CrossRef]
- DeMauro, S.B. Neurodevelopmental outcomes of infants with bronchopulmonary dysplasia. Pediatr. Pulmonol. 2021. [Google Scholar] [CrossRef] [PubMed]
- Gallini, F.; Coppola, M.; De Rose, D.U.; Maggio, L.; Arena, R.; Romano, V.; Cota, F.; Ricci, D.; Romeo, D.M.; Mercuri, E.M.; et al. Neurodevelopmental outcomes in very preterm infants: The role of severity of Bronchopulmonary Dysplasia. Early Hum. Dev. 2021, 152, 105275. [Google Scholar] [CrossRef] [PubMed]
- Glass, A.; Chau, T.J.; Gardiner, V.; Foong, J.; Vinall, J.; Zwicker, J.; Grunau, J.G.E.; Synnes, R.; Poskitt, A.; Miller, K.J.S. Severe retinopathy of prematurity predicts delayed white matter maturation and poorer neurodevelopment. Arch. Dis. Child. Fetal Neonatal Ed. 2017, 102, F532–F537. [Google Scholar] [CrossRef]
- Schmidt, B.; Davis, P.G.; Asztalos, E.V.; Solimano, A.; Roberts, R.S. Association between severe retinopathy of prematurity and nonvisual disabilities at age 5 years. JAMA 2014, 311, 523–525. [Google Scholar] [CrossRef]
- Villar, J.; Giuliani, F.; Fenton, T.R.O.; Ohuma, E.; Ismail, L.C.; Kennedy, S.H. INTERGROWTH-21st very preterm size at birth reference charts. Lancet 2016, 387, 844–845. [Google Scholar] [CrossRef]
- Jobe, A.H.; Bancalari, E. Bronchopulmonary dysplasia. Am. J. Respir. Crit. Care Med. 2001, 163, 1723–1729. [Google Scholar] [CrossRef] [PubMed]
- Gole, A.; Ells, G.; Katz, A.L.; Holmstrom, X.; Fielder, G.; Capone, A.R.; Flynn, A.; Good, J.T.; Holmes, W.G.J.; McNamara, A.J.; et al. The International Classification of Retinopathy of Prematurity Revisited. Arch. Ophthalmol. 2005, 123, 991–999. [Google Scholar] [CrossRef]
- Bell, M.J.; Ternberg, J.L.; Feigin, R.D.; Keating, J.P.; Marshall, R.; Barton, L.; Brotherton, T. Neonatal necrotizing enterocolitis. Therapeutic decisions based upon clinical staging. Ann. Surg. 1978, 187, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Papile, L.-A.; Burstein, J.; Burstein, R.; Koffler, H. Incidence and evolution of subependymal and intraventricular hemorrhage: A study of infants with birth weights less than 1500 gm. J. Pediatr. 1978, 92, 529–534. [Google Scholar] [CrossRef]
- Johnson, S.; Moore, T.; Marlow, N. Using the Bayley-III to assess neurodevelopmental delay: Which cut-off should be used? Pediatr. Res. 2014, 75, 670–674. [Google Scholar] [CrossRef] [PubMed]
- Kilbride, H.W.; Aylward, G.P.; Doyle, L.W.; Singer, L.T.; Lantos, J. Prognostic neurodevelopmental testing of preterm infants: Do we need to change the paradigm? J. Perinatol. 2017, 37, 475–479. [Google Scholar] [CrossRef] [PubMed]
- Payne, A.H.; Hintz, S.R.; Hibbs, A.M.; Walsh, M.C.; Vohr, B.R.; Bann, C.M.; Wilson-Costello, D.E. For the Eunice Kennedy Shriver National Institute of Child Health and Human Development neonatal research network neurodevelopmental outcomes of extremely low-gestational-age neonates with low-grade periventricular-intraventricular hemorrhage. JAMA Pediatr. 2013, 167, 451–459. [Google Scholar] [CrossRef] [PubMed]
- Graz, M.B.; Tolsa, J.-F.; Fumeaux, C.J.F. Being Small for Gestational Age: Does it Matter for the Neurodevelopment of Premature Infants? A Cohort Study. PLoS ONE 2015, 10, e0125769. [Google Scholar] [CrossRef]
- Jelliffe-Pawlowski, L.L.; Hansen, R.L. Neurodevelopmental outcome at 8 months and 4 years among infants born full-term small-for-gestational-age. J. Perinatol. 2004, 24, 505–514. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Lodygensky, A.; Seghier, G.; Warfield, M.L.; Tolsa, S.K.; Sizonenko, C.B.; Lazeyras, S.; Hüppi, F.P.S. Intrauterine growth restriction affects the preterm infant’s hippocampus. Pediatr. Res. 2008, 63, 438–443. [Google Scholar] [CrossRef]
- Beaino, G.; Khoshnood, B.; Kaminski, M.; Marret, S.; Pierrat, V.; Vieux, R.; Thiriez, G.; Matis, J.; Picaud, J.-C.; Rozé, J.-C.; et al. Predictors of the risk of cognitive deficiency in very preterm infants: The EPIPAGE prospective cohort. Acta Paediatr. 2011, 100, 370–378. [Google Scholar] [CrossRef] [PubMed]
- DeMauro, S.B. The impact of bronchopulmonary dysplasia on childhood outcomes. Clin. Perinatol. 2018, 45, 439–452. [Google Scholar] [CrossRef]
- Cheong, J.L.; Doyle, L.W. An update on pulmonary and neurodevelopmental outcomes of bronchopulmonary dysplasia. Semin. Perinatol. 2018, 42, 478–484. [Google Scholar] [CrossRef]
- Anderson, P.J.; Doyle, L.W. Neurodevelopmental outcome of bronchopulmonary dysplasia. Semin. Perinatol. 2006, 30, 227–232. [Google Scholar] [CrossRef]
- Schmidt, B.; Roberts, R.S.; Davis, P.G.; Doyle, L.W.; Asztalos, E.V.; Opie, G.; Bairam, A.; Solimano, A.; Arnon, S.; Sauve, R.S.; et al. Prediction of late death or disability at age 5 years using a count of 3 neonatal morbidities in very low birth weight infants. J. Pediatr. 2015, 167, 982–986.e2. [Google Scholar] [CrossRef] [PubMed]
- DePaz, E.J.; Aghai, Z.; Konduri, G.G. Severe intraventricular hemorrhage, a marker of severe retinopathy of prematurity. Pediatr. Res. 1999, 45, 194. [Google Scholar] [CrossRef][Green Version]
- Watts, P.; Adams, G.G.W.; Thomas, R.M.; Bunce, C. Intraventricular haemorrhage and stage 3 retinopathy of prematurity. Br. J. Ophthalmol. 2000, 84, 596–599. [Google Scholar] [CrossRef]
- Foos, R.Y. Retinopathy of prematurity. Retina 1987, 7, 260–276. [Google Scholar] [CrossRef]
- Ng, Y.K.; Fielder, A.R.; Levene, M.I.; Trounce, J.Q.; McLellan, N. Are severe acute retinopathy of prematurity and severe periventricular leucomalacia both ischaemic insults? Br. J. Ophthalmol. 1989, 73, 111–114. [Google Scholar] [CrossRef] [PubMed]
- Leversen, K.T.; Sommerfelt, K.; Rønnestad, A.; Kaaresen, P.I.; Farstad, T.; Skranes, J.; Støen, R.; Elgen, I.B.; Rettedal, S.; Eide, G.E.; et al. Prediction of neurodevelopmental and sensory outcome at 5 years in norwegian children born extremely preterm. Pediatrics 2011, 127, e630–e638. [Google Scholar] [CrossRef]
- Ricci, D.; Lucibello, S.; Orazi, L.; Gallini, F.; Staccioli, S.; Serrao, F.; Olivieri, G.; Quintiliani, M.; Sivo, S.; Rossi, V.; et al. Early visual and neuro-development in preterm infants with and without retinopathy. Early Hum. Dev. 2020, 148, 105134. [Google Scholar] [CrossRef]
- Drost, F.J.; Keunen, K.; Moeskops, P.; Claessens, N.H.P.; Van Kalken, F.; Išgum, I.; Voskuil-Kerkhof, E.S.M.; Groenendaal, F.; De Vries, L.S.; Benders, M.J.N.L.; et al. Severe retinopathy of prematurity is associated with reduced cerebellar and brainstem volumes at term and neurodevelopmental deficits at 2 years. Pediatr. Res. 2018, 83, 818–824. [Google Scholar] [CrossRef] [PubMed]
- Sveinsdóttir, K.; Ley, D.; Hövel, H.; Fellman, V.; Huppi, P.S.; Smith, L.E.; Hellström, A.; Pupp, I.H. Relation of retinopathy of prematurity to brain volumes at term equivalent age and developmental outcome at 2 years of corrected age in very preterm infants. Neonatology 2018, 114, 46–52. [Google Scholar] [CrossRef] [PubMed]
- Morrone, M.C. Brain development: Critical periods for cross-sensory plasticity. Curr. Biol. 2010, 20, R934–R936. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Lickliter, R. The integrated development of sensory organization. Clin. Perinatol. 2011, 38, 591–603. [Google Scholar] [CrossRef]
| No IVH (n = 195) | Low-Grade IVH (n = 45) | p-Value | |
|---|---|---|---|
| GA (week) | 30.3 (28.3–32) | 28.4 (26.4–30.4) | <0.001 |
| Birth weight (g) | 1230 (980–1340) | 920 (680–1210) | <0.001 |
| SGA | 49 (25.4) | 12 (27.3) | 0.849 |
| IVF | 95 (48.7) | 21 (46.7) | 0.869 |
| Male | 98 (50.3) | 26 (57.8) | 0.410 |
| C/S | 120 (61.5) | 30 (66.7) | 0.609 |
| hCAM | 68 (36) | 22 (51.2) | 0.083 |
| PPROM >18 h | 52 (27.8) | 19 (43.2) | 0.068 |
| Oligohydramnios | 36 (20.2) | 13 (31) | 0.150 |
| PIH | 26 (13.6) | 9 (20.9) | 0.239 |
| No ACS | 34 (17.7) | 6 (13.6) | 0.516 |
| No IVH (n = 195) | Low-Grade IVH (n = 45) | p-Value | |
|---|---|---|---|
| RDS | 80 (41) | 32 (71.1) | <0.001 |
| Treated PDA | 52 (26.7) | 20 (44.4) | 0.029 |
| Moderate to severe BPD | 51 (26.6) | 18 (40) | 0.074 |
| Any stage ROP | 40 (20.7) | 17 (37.8) | 0.016 |
| Severe ROP | 10 (5.1) | 6 (13.3) | 0.088 |
| NEC | 7 (3.6) | 3 (6.7) | 0.403 |
| Sepsis | 9 (4.6) | 4 (8.9) | 0.273 |
| Hospital stay (days) | 53 (32–79) | 73 (55–95.5) | <0.001 |
| No IVH (n = 195) | Low-Grade IVH (n = 45) | p-Value | |
|---|---|---|---|
| Neurodevelopmental impairment | 19 (9.7) | 6 (13.3) | 0.430 |
| Cerebral palsy | 1 (0.5) | 0 (0) | 1.000 |
| Hearing loss | - | - | - |
| Blindness | - | - | - |
| Bayley-III | (n = 146) | (n = 36) | |
| Cognitive domain | 100 (90–105) | 90 (87.5–110) | 0.484 |
| Language domain | 97 (86–106) | 90 (79–100) | 0.025 |
| Motor domain | 97 (88–103) | 97 (88–100) | 0.617 |
| Cognitive and language <85 | 11 (7.5) | 3 (8.3) | 1.000 |
| Motor <85 | 15 (10.3) | 6 (16.7) | 0.380 |
| Univariate Analysis | Multivariate Analysis | ||||||
|---|---|---|---|---|---|---|---|
| OR | 95% CI | p-Value | Adjusted OR | 95% CI | p-Value | VIF | |
| GA (week) | 0.90 | (0.77–1.04) | 0.141 | 1.00 | (0.75–1.33) | 0.986 | 2.830 |
| SGA | 3.07 | (1.32–7.16) | 0.009 | 6.82 | (1.77–26.31) | 0.005 | 2.670 |
| RDS | 1.82 | (0.78–4.24) | 0.163 | 2.44 | (0.57–10.44) | 0.228 | 1.810 |
| Treated PDA | 1.65 | (0.70–3.86) | 0.253 | 0.87 | (0.29–2.67) | 0.814 | 1.810 |
| Moderate to severe BPD | 5.33 | (2.23–12.78) | 0.000 | 3.21 | (1.03–10.0) | 0.044 | 1.680 |
| NEC | 4.05 | (0.98–16.80) | 0.054 | 1.94 | (0.34–11.08) | 0.457 | 1.330 |
| Severe ROP | 8.90 | (2.97–26.71) | 0.000 | 5.67 | (1.13–28.40) | 0.035 | 1.230 |
| Sepsis | 4.36 | (1.24–15.38) | 0.022 | 3.71 | (0.72–19.03) | 0.116 | 1.120 |
| Low-grade IVH | 1.43 | (0.53–3.80) | 0.479 | 0.71 | (0.21–2.46) | 0.594 | 1.080 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bae, S.P.; Shin, S.H.; Yoon, Y.M.; Kim, E.-K.; Kim, H.-S. Association of Severe Retinopathy of Prematurity and Bronchopulmonary Dysplasia with Adverse Neurodevelopmental Outcomes in Preterm Infants without Severe Brain Injury. Brain Sci. 2021, 11, 699. https://doi.org/10.3390/brainsci11060699
Bae SP, Shin SH, Yoon YM, Kim E-K, Kim H-S. Association of Severe Retinopathy of Prematurity and Bronchopulmonary Dysplasia with Adverse Neurodevelopmental Outcomes in Preterm Infants without Severe Brain Injury. Brain Sciences. 2021; 11(6):699. https://doi.org/10.3390/brainsci11060699
Chicago/Turabian StyleBae, Seong Phil, Seung Han Shin, Young Mi Yoon, Ee-Kyung Kim, and Han-Suk Kim. 2021. "Association of Severe Retinopathy of Prematurity and Bronchopulmonary Dysplasia with Adverse Neurodevelopmental Outcomes in Preterm Infants without Severe Brain Injury" Brain Sciences 11, no. 6: 699. https://doi.org/10.3390/brainsci11060699
APA StyleBae, S. P., Shin, S. H., Yoon, Y. M., Kim, E.-K., & Kim, H.-S. (2021). Association of Severe Retinopathy of Prematurity and Bronchopulmonary Dysplasia with Adverse Neurodevelopmental Outcomes in Preterm Infants without Severe Brain Injury. Brain Sciences, 11(6), 699. https://doi.org/10.3390/brainsci11060699






