The Association between Executive Functions and Body Weight/BMI in Children and Adolescents with ADHD
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Group
2.2. Anthropometric Measurements
2.3. Calendar Age
2.4. Cognitive Tests
2.4.1. Sustained Attention to Response Test
2.4.2. Attention Network Test
2.5. Statistical Methods
3. Results
3.1. The Values of Height, Body Weight, and BMI
3.2. Results of the Cognitive Tasks
3.3. The Association between Mean Norm-Referenced Standardized Height, Body Weight, and BMI and the Results of Cognitive Tasks
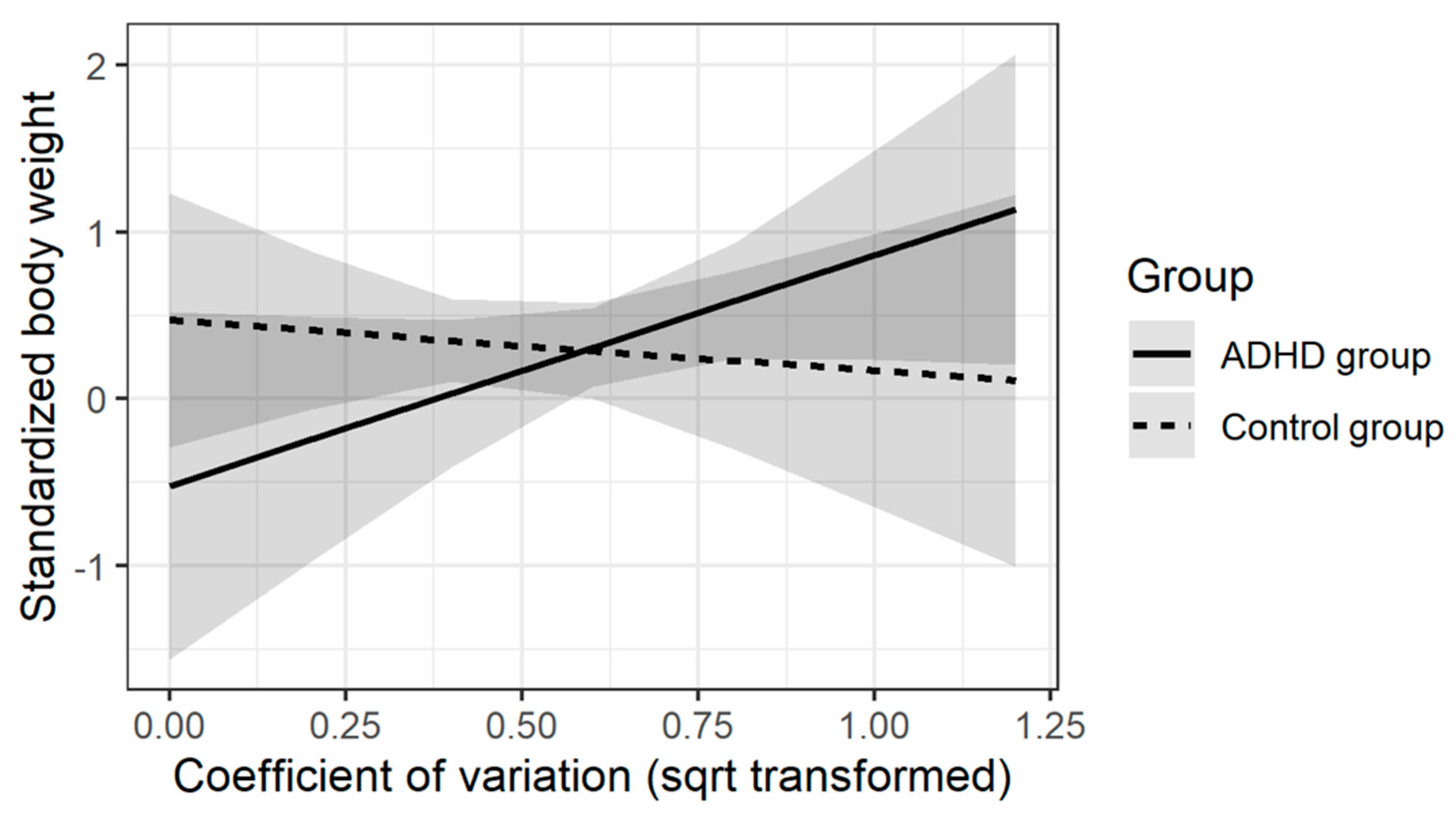
3.4. ADHD Diagnosis and Executive Functioning as Predictors of Body Weight
4. Discussion
4.1. The Results of Cognitive Tests
- (1)
- Participants with ADHD made significantly more errors in both ‘go’ trials, which showed their less effective sustained attention, as well as in ‘no-go’ trials, which demonstrated less effective response inhibition and greater impulsivity. These results are consistent with the observations of Johnson et al. [32], O’Connell et al. [33], Shallice et al. [34], and Wodka [35], which in turn is in line with the hypothesis that deficit in response inhibition is a primary mechanism causing ADHD symptoms (Barkley [36]);
- (2)
- Participants with ADHD had significantly higher values of the Coefficient of Variation, which means lower stability of reaction times, thus less stability of attention processes (Coefficient of Variation is a measure of intra-subject variability, which is characteristic of ADHD (Castellanos and Tannock [37]). These results are consistent with the results of other studies (Bellgrove et al. [38]; Castellanos et al. [39]; Epstein et al. [40]; Gómez-Guerrero et al. [41]; Hervey et al. [42]; Hynd et al. [43]; Klein et al. [44]; Leth-Steensen et al. [45]). It is believed that the Coefficient of Variation better characterizes people with ADHD than the accuracy of performing tasks or the mean reaction time (Klein et al. [44]). Furthermore, intra-subject variability has been shown to be hereditary, both for people with ADHD and people from the control group (Andreou et al. [46]; Kuntsi et al. [47]; Kuntsi and Stevenson [48]);
- (1)
- Participants with ADHD had significantly longer time in response to incongruent stimulus presentation, which indicated less effective inhibition of the attention orienting and greater distractibility. This is consistent with the results of studies of Konrad et al. [49], Johnson et al. [50], and Mullane et al. [51].
- (2)
- Participants with ADHD had significantly longer total reaction time in the task, which meant less effective attention processes during the whole task. This result is consistent with the results of studies of Johnson et al. [50] and Kratz et al. [52]. On the other hand, in the study of Adolfsdottir et al. [53], there were no significant differences in reaction time in the group of ADHD patients and the control group.
- (3)
- Participants with ADHD achieved a lower accuracy in congruent trials, which indicated worse stability of attention processes and lower accuracy in incongruent trials, which indicated greater sensitivity to distractors.
- (4)
- Participants with ADHD did not differ from the control group in terms of Alerting and Orienting, which indicated a similar level of attention span and similar time to redirect attention to the stimulus (similar to the study of Adolfsdottir et al. [53]). These results are in line with the assumptions in which executive control is a superior function related to prefrontal and frontal areas (dopaminergic and noradrenergic pathways), which explains the lack of evident deficits in alertness and orienting of attention ADHD (Fan et al. [23]). Different results were obtained by Mullane et al. [51] and Johnson et al. [50], who showed the presence of significant differences in the alertness of attention in children with ADHD compared with control groups.
4.2. The Association between Mean Standardized Height, Body Weight, and BMI and the Results of Cognitive Tasks
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Albayrak, Ö.; Pütter, C.; Volckmar, A.L.; Cichon, S.; Hoffmann, P.; Nöthen, M.M.; Jöckel, K.H.; Schreiber, S.; Wichmann, H.E.; Faraone, S.V.; et al. Common Obesity Risk Alleles in Childhood Attention-Deficit/Hyperactivity Disorder. Am. J. Med. Genet. Part B Neuropsychiatr. Genet. 2013, 162, 295–305. [Google Scholar] [CrossRef]
- Choudhry, Z.; Sengupta, S.M.; Grizenko, N.; Thakur, G.A.; Fortier, M.E.; Schmitz, N.; Joober, R. Association between Obesity-Related Gene FTO and ADHD. Obesity 2013. [Google Scholar] [CrossRef] [PubMed]
- Hanć, T.; Dmitrzak-Węglarz, M.; Borkowska, A.; Wolańczyk, T.; Pytlińska, N.; Rybakowski, F.; Słopień, R.; Słopień, A. Overweight in Boys With ADHD Is Related to Candidate Genes and Not to Deficits in Cognitive Functions. J. Atten. Disord. 2018, 22, 1158–1172. [Google Scholar] [CrossRef] [PubMed]
- Patte, K.A.; Davis, C.A.; Levitan, R.D.; Kaplan, A.S.; Carter-Major, J.; Kennedy, J.L. A Behavioral Genetic Model of the Mechanisms Underlying the Link between Obesity and Symptoms of ADHD. J. Atten. Disord. 2016. [Google Scholar] [CrossRef] [PubMed]
- Pauli-Pott, U.; Becker, K.; Albayrak, Ö.; Hebebrand, J.; Pott, W. Links between psychopathological symptoms and disordered eating behaviors in overweight/obese youths. Int. J. Eat. Disord. 2013, 46, 156–163. [Google Scholar] [CrossRef] [PubMed]
- Ptacek, R.; Kuzelova, H.; Stefano, G.B.; Raboch, J.; Sadkova, T.; Goetz, M.; Kream, R.M. Disruptive Patterns of Eating Behaviors and Associated Lifestyles in Males with ADHD. Med. Sci. Monit. 2014, 20, 608–613. [Google Scholar] [CrossRef]
- Korczak, D.J.; Lipman, E.; Morrison, K.; Duku, E.; Szatmari, P. Child and Adolescent Psychopathology Predicts Increased Adult Body Mass Index. J. Dev. Behav. Pediatr. 2014, 35, 108–117. [Google Scholar] [CrossRef]
- Kummer, A.; Barbosa, I.G.; Rodrigues, D.H.; Rocha, N.P.; Da Silva Rafael, M.; Pfeilsticker, L.; Simõese Silva, A.C.; Teixeira, A.L. Frequency of Overweight and Obesity in Children and Adolescents with Autism and Attention Deficit/Hyperactivity Disorder. Rev. Paul. Pediatr. 2016, 34, 71–77. [Google Scholar] [CrossRef]
- Pauli-Pott, U.; Neidhard, J.; Heinzel-Gutenbrunner, M.; Becker, K. On the link between attention deficit/hyperactivity disorder and obesity: Do comorbid oppositional defiant and conduct disorder matter? Eur. Child Adolesc. Psychiatry 2014, 23, 531–537. [Google Scholar] [CrossRef]
- Racicka, E.; Hanć, T.; Giertuga, K.; Bryńska, A.; Wolańczyk, T. Prevalence of Overweight and Obesity in Children and Adolescents with ADHD: The Significance of Comorbidities and Pharmacotherapy. J. Atten. Disord. 2018, 22, 1095–1108. [Google Scholar] [CrossRef]
- White, B.; Nicholls, D.; Christie, D.; Cole, T.J.; Viner, R.M. Childhood Psychological Function and Obesity Risk across the Lifecourse: Findings from the 1970 British Cohort Study. Int. J. Obes. 2012, 36, 511–516. [Google Scholar] [CrossRef] [PubMed]
- Vogel, S.W.N.; Bijlenga, D.; Tanke, M.; Bron, T.I.; van der Heijden, K.B.; Swaab, H.; Beekman, A.T.F.; Sandra Kooij, J.J. Circadian Rhythm Disruption as a Link between Attention-Deficit/Hyperactivity Disorder and Obesity? J. Psychosom. Res. 2015, 79, 443–450. [Google Scholar] [CrossRef] [PubMed]
- Anderson, S.E.; Cohen, P.; Naumova, E.N.; Must, A. Relationship of Childhood Behavior Disorders to Weight Gain from Childhood into Adulthood. Ambul. Pediatr. 2006, 6, 297–301. [Google Scholar] [CrossRef]
- Cook, B.G.; Li, D.; Heinrich, K.M. Obesity, Physical Activity, and Sedentary Behavior of Youth with Learning Disabilities and ADHD. J. Learn. Disabil. 2015, 48, 563–576. [Google Scholar] [CrossRef] [PubMed]
- Ebenegger, V.; Munsch, S. Relationship of Hyperactivity/Inattention with Adiposity and Lifestyle Characteristics in Preschool Children. J. Child Neurol. 2012. [Google Scholar] [CrossRef]
- Khalife, N.; Kantomaa, M.; Glover, V.; Tammelin, T.; Laitinen, J.; Ebeling, H.; Hurtig, T.; Jarvelin, M.R.; Rodriguez, A. Childhood Attention-Deficit/Hyperactivity Disorder Symptoms Are Risk Factors for Obesity and Physical Inactivity in Adolescence. J. Am. Acad. Child Adolesc. Psychiatry 2014, 53, 425–436. [Google Scholar] [CrossRef]
- Kim, C.H.; Hahn, M.K.; Joung, Y.; Anderson, S.L.; Steele, A.H.; Mazei-Robinson, M.S.; Gizer, I.; Teicher, M.H.; Cohen, B.M.; Robertson, D.; et al. A Polymorphism in the Norepinephrine Transporter Gene Alters Promoter Activity and Is Associated with Attention-Deficit Hyperactivity Disorder. Proc. Natl. Acad. Sci. USA 2006, 103, 19164–19169. [Google Scholar] [CrossRef]
- Lingineni, R.K.; Biswas, S.; Ahmad, N.; Jackson, B.E.; Bae, S.; Singh, K.P. Factors associated with attention deficit/hyper activity disorder among US children: Results from a national survey. BMC Pediatr. 2012, 12, 50. [Google Scholar] [CrossRef]
- McWilliams, L.; Sayal, K.; Glazebrook, C. Inattention and Hyperactivity in Children at Risk of Obesity: A Community Cross-Sectional Study. BMJ Open 2013, 3, e002871. [Google Scholar] [CrossRef]
- Graziano, P.A.; Bagner, D.M.; Waxmonsky, J.G.; Reid, A.; Mcnamara, J.P.; Geffken, G.R. Co-Occurring Weight Problems among Children with Attention Deficit/Hyperactivity Disorder: The Role of Executive Functioning. Int. J. Obes. 2012, 36, 567–572. [Google Scholar] [CrossRef]
- Van der Oord, S.; Braet, C.; Cortese, S.; Claes, L. Testing the Dual Pathway Model of ADHD in Obesity: A Pilot Study. Eat. Weight Disord. 2018, 23, 507–512. [Google Scholar] [CrossRef] [PubMed]
- Robertson, I.H.; Manly, T.; Andrade, J.; Baddeley, B.T.; Yiend, J. “Oops!”: Performance Correlates of Everyday Attentional Failures in Traumatic Brain Injured and Normal Subjects. Neuropsychologia 1997, 35, 747–758. [Google Scholar] [CrossRef]
- Fan, J.; McCandliss, B.D.; Sommer, T.; Raz, A.; Posner, M.I. Testing the Efficiency and Independence of Attentional Networks. J. Cogn. Neurosci. 2002, 14, 340–347. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. In DSM-IV-TR; American Psychiatric Association: Philadelphia, PA, USA, 2000. [Google Scholar]
- Kaufman, J.; Birmaher, B.; Brent, D.; Rao, U.; Flynn, C.; Moreci, P.; Williamson, D.; Ryan, N. Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): Initial Reliability and Validity Data. J. Am. Acad. Child Adolesc. Psychiatry 1997, 36, 980–988. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. International Classification of Diseases (ICD), 10th ed.; World Health Organization: Geneva, Switzerland, 1994. [Google Scholar]
- Chumlea, W.C.; Shumei, S.G.; Cameron, N. The assessment of human growth. In Human Growth and Development; Academic Press: Cambridge, MA, USA, 2002; pp. 349–361. [Google Scholar]
- De Onis, M.; Garza, C.; Victora, C.G.; Onyango, A.W.; Frongillo, E.A.; Martines, J. The WHO Multicentre Growth Reference Study: Planning, Study Design, and Methodology. Food Nutr. Bull. 2004, 25 (Suppl. 1), 15–26. [Google Scholar] [CrossRef]
- Kułaga, Z.; Litwin, M.; Tkaczyk, M.; Palczewska, I.; Zaja̧czkowska, M.; Zwolińska, D.; Krynicki, T.; Wasilewska, A.; Moczulska, A.; Morawiec-Knysak, A.; et al. Polish 2010 Growth References for School-Aged Children and Adolescents. Eur. J. Pediatr. 2011, 170, 599–609. [Google Scholar] [CrossRef]
- Posner, M.I. Orienting of attention. Q. J. Exp. Psychol. 1980, 32, 3–25. [Google Scholar] [CrossRef]
- R Core Team. R: A language and environment for statistical computing (3.5.3). R Foundation for Statistical Computing. Available online: https://www.r-project.org/ (accessed on 20 October 2020).
- Johnson, K.A.; Robertson, I.H.; Kelly, S.P.; Silk, T.J.; Barry, E.; Dáibhis, A.; Watchorn, A.; Keavey, M.; Fitzgerald, M.; Gallagher, L.; et al. Dissociation in Performance of Children with ADHD and High-Functioning Autism on a Task of Sustained Attention. Neuropsychologia 2007, 45, 2234–2245. [Google Scholar] [CrossRef]
- O’Connell, R.G.; Bellgrove, M.A.; Dockree, P.M.; Robertson, I.H. Cognitive remediation in ADHD: Effects of periodic non-contingent alerts on sustained attention to response. Neuropsychol. Rehabil. 2006, 16, 653–665. [Google Scholar] [CrossRef]
- Shallice, T.; Marco Marzocchi, G.; Coser, S.; Del Savio, M.; Meuter, R.F.; Rumiati, R.I. Executive Function Profile of Children with Attention Deficit Hyperactivity Disorder. Dev. Neuropsychol. 2002, 21, 43–71. [Google Scholar] [CrossRef]
- Wodka, E.L.; Mahone, E.M.; Blankner, J.G.; Larson, J.C.G.; Fotedar, S.; Denckla, M.B.; Mostofsky, S.H. Evidence That Response Inhibition Is a Primary Deficit in ADHD. J. Clin. Exp. Neuropsychol. 2007, 29, 345–356. [Google Scholar] [CrossRef] [PubMed]
- Barkley, R.A. Behavioral inhibition, sustained attention, and executive functions: Constructing a unifying theory of ADHD. Psychol. Bull. 1997, 121, 65–94. [Google Scholar] [CrossRef] [PubMed]
- Castellanos, F.X.; Tannock, R. Neuroscience of Attention-Deficit/Hyperactivity Disorder: The Search for Endophenotypes. Nat. Rev. Neurosci. 2002, 3, 617–628. [Google Scholar] [CrossRef] [PubMed]
- Bellgrove, M.A.; Hawi, Z.; Kirley, A.; Gill, M.; Robertson, I.H. Dissecting the Attention Deficit Hyperactivity Disorder (ADHD) Phenotype: Sustained Attention, Response Variability and Spatial Attentional Asymmetries in Relation to Dopamine Transporter (DAT1) Genotype. Neuropsychologia 2005, 43, 1847–1857. [Google Scholar] [CrossRef]
- Castellanos, F.X.; Sonuga-Barke, E.J.S.; Scheres, A.; Di Martino, A.; Hyde, C.; Walters, J.R. Varieties of Attention-Deficit/Hyperactivity Disorder-Related Intra-Individual Variability. Biol. Psychiatry 2005, 57, 1416–1423. [Google Scholar] [CrossRef]
- Epstein, J.N.; Langberg, J.M.; Rosen, P.J.; Graham, A.; Narad, M.E.; Antonini, T.N.; Brinkman, W.B.; Froehlich, T.; Simon, J.O. Evidence for higher reaction time variability for children with ADHD on a range of cognitive tasks including reward and event rate manipulations. Neuropsychology 2011, 25, 427–441. [Google Scholar] [CrossRef]
- Gómez-guerrero, L.; Domínguez-martín, C.; Mairena, M.A.; Psy, C.; Martino, A.D.; Wang, J.; Mendelsohn, A.; Dreyer, B.; Isquith, P.K.; Gioia, G.; et al. Response-Time Variability Is Related to Parent Ratings of Inattention, Hyperactivity, and Executive Function. J. Atten. Disord. 2013, 15, 572–582. [Google Scholar] [CrossRef]
- Hervey, A.S.; Epstein, J.N.; Curry, J.F.; Tonev, S.; Eugene Arnold, L.; Keith Conners, C.; Hinshaw, S.P.; Swanson, J.M.; Hechtman, L. Reaction Time Distribution Analysis of Neuropsychological Performance in an ADHD Sample. Child Neuropsychol. 2006, 12, 125–140. [Google Scholar] [CrossRef]
- Hynd, G.W.; Nieves, N.; Connor, R.T.; Stone, P.; Town, P.; Becker, M.G.; Lahey, B.B.; Lorys, A.R. Attention Deficit Disorder with and without Hyperactivity: Reaction Time and Speed of Cognitive Processing. J. Learn. Disabil. 1989, 22, 573–580. [Google Scholar] [CrossRef]
- Klein, C.; Wendling, K.; Huettner, P.; Ruder, H.; Peper, M. Intra-Subject Variability in Attention-Deficit Hyperactivity Disorder. Biol. Psychiatry 2006, 60, 1088–1097. [Google Scholar] [CrossRef]
- Leth-Steensen, C.; King Elbaz, Z.; Douglas, V.I. Mean Response Times, Variability, and Skew in the Responding of ADHD Children: A Response Time Distributional Approach. Acta Psychol. 2000, 104, 167–190. [Google Scholar] [CrossRef]
- Andreou, P.; Neale, B.E.N.M.; Chen, W.A.I.; Christiansen, H.; Heise, A.; Meidad, S.; Muller, U.C. Europe PMC Funders Group Reaction Time Performance in ADHD: Improvement under Fast-Incentive Condition and Familial Effects. Psychol. Med. 2013, 37, 1703–1715. [Google Scholar] [CrossRef] [PubMed]
- Kuntsi, J.; Rogers, H.; Swinard, G.; Börger, N.; Meere, J.; Rijsdijk, F.; Asherson, P. Reaction time, inhibition, working memory and ‘delay aversion’ performance: Genetic influences and their interpretation. Psychol. Med. 2006, 36, 1613–1624. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kuntsi, J.; Stevenson, J. Psychological Mechanisms in Hyperactivity: II The Role of Genetic Factors. J. Child Psychol. Psychiatry 2001, 42, 211–219. [Google Scholar] [CrossRef] [PubMed]
- Konrad, K.; Neufang, S.; Hanisch, C.; Fink, G.R.; Herpertz-Dahlmann, B. Dysfunctional Attentional Networks in Children with Attention Deficit/Hyperactivity Disorder: Evidence from an Event-Related Functional Magnetic Resonance Imaging Study. Biol. Psychiatry 2006, 59, 643–651. [Google Scholar] [CrossRef] [PubMed]
- Johnson, K.A.; Robertson, I.H.; Barry, E.; Mulligan, A.; Dáibhis, A.; Daly, M.; Watchorn, A.; Gill, M.; Bellgrove, M.A. Impaired Conflict Resolution and Alerting in Children with ADHD: Evidence from the Attention Network Task (ANT). J. Child Psychol. Psychiatry 2008, 49, 1339–1347. [Google Scholar] [CrossRef]
- Mullane, J.C.; Corkum, P.V.; Klein, R.M.; McLaughlin, E.N.; Lawrence, M.A. Alerting, Orienting, and Executive Attention in Children with ADHD. J. Atten. Disord. 2011, 15, 310–320. [Google Scholar] [CrossRef]
- Kratz, O.; Studer, P.; Malcherek, S.; Erbe, K.; Moll, G.H.; Heinrich, H. Attentional Processes in Children with ADHD: An Event-Related Potential Study Using the Attention Network Test. Int. J. Psychophysiol. 2011, 2, 82–90. [Google Scholar] [CrossRef]
- Adólfsdóttir, S.; Sørensen, L.; Lundervold, A.J. The Attention Network Test: A Characteristic Pattern of Deficits in Children with ADHD. Behav. Brain Funct. 2008, 4–9. [Google Scholar] [CrossRef]
- Macleod, J.W.; Lawrence, M.A.; McConnell, M.M.; Eskes, G.A.; Klein, R.M.; Shore, D.I. Appraising the ANT: Psychometric and theoretical considerations of the Attention Network Test. Neuropsychology. 2010, 5, 637–651. [Google Scholar] [CrossRef]
- Jauregi, A.; Kessler, K.; Hassel, S. Linking Cognitive Measures of Response Inhibition and Reward Sensitivity to Trait Impulsivity. Front. Psychol. 2018, 9, 2306. [Google Scholar] [CrossRef] [PubMed]

| n | M | Min | Max | SD | |
|---|---|---|---|---|---|
| Adjusted treatment duration (days) | 43 | 1096.9 | 73 | 2777 | 584 |
| Methylphenidate OROS dose (mg) | 43 | 36.8 | 18 | 54 | 12.4 |
| Adjusted treatment duration (days) | 10 | 1188 | 583 | 2139 | 575.6 |
| Methylphenidate SR dose (mg) | 10 | 27 | 10 | 50 | 12.5 |
| Control M | ADHD M | t | df | p | Control n | ADHD n | Control SD | ADHD SD | |
|---|---|---|---|---|---|---|---|---|---|
| zBV (♂ + ♀) | 0.43 | 0.22 | 1.16 | 118 | 0.25 | 62 | 58 | 0.97 | 1.03 |
| zBW (♂ + ♀) | 0.43 | 0.34 | 0.53 | 118 | 0.60 | 62 | 58 | 0.86 | 1.07 |
| zBMI (♂ + ♀) | 0.33 | 0.34 | −0.04 | 118 | 0.97 | 62 | 58 | 0.84 | 1.18 |
| BMI (♂ + ♀) | 20.8 | 20.5 | 0.39 | 118 | 0.70 | 62 | 58 | 2.92 | 4.21 |
| Control (n = 61) | ADHD (n = 57) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Min | Med | Max | IQR | Min | Med | Max | IQR | p | |
| Mean Reaction time in go trials | 203 | 375 | 618 | 147 | 157 | 376 | 571 | 139 | 0.477 |
| SD of RTs in go trials | 46 | 131 | 359 | 61 | 77 | 182 | 416 | 100 | <0.001 |
| Coefficient of variation | 0.10 | 0.33 | 0.93 | 0.15 | 0.23 | 0.49 | 1.17 | 0.24 | <0.001 |
| Accuracy in go trials | 0.75 | 0.99 | 1.00 | 0.03 | 0.63 | 0.93 | 1.00 | 0.10 | <0.001 |
| Accuracy in no go trials | 0.08 | 0.64 | 1.00 | 0.32 | 0.00 | 0.44 | 0.92 | 0.32 | <0.001 |
| Control (n = 62) | ADHD (n = 57) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Min | Med | Max | IQR | Min | Med | Max | IQR | p | |
| Total Reaction time | 444 | 596 | 891 | 150 | 485 | 662 | 889 | 134 | 0.001 |
| Accuracy in congruent trials | 0.96 | 1.00 | 1.00 | 0.01 | 0.81 | 0.99 | 1.00 | 0.02 | 0.004 |
| Accuracy in incongruent trials | 0.73 | 0.96 | 1.00 | 0.04 | 0.24 | 0.94 | 1.00 | 0.06 | 0.006 |
| Alerting | −52.75 | 25.84 | 129.40 | 37.51 | −66.38 | 38.68 | 142.00 | 43.71 | 0.092 |
| Orienting | −26.31 | 58.17 | 115.90 | 46.33 | −24.12 | 55.18 | 127.80 | 38.76 | 0.411 |
| Executive | 29.81 | 98.55 | 242.50 | 43.74 | −32.61 | 130.0 | 307.20 | 56.20 | <0.001 |
| ADHD Group | Control Group | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| zBW | zBMI | zBW | zBMI | ||||||||
| Task Performance Indices | n | rho | p | Rho | p | n | Rho | p | Rho | p | |
| ANT | Total Reaction time | 57 | 0.00 | 0.976 | 0.04 | 0.756 | 62 | −0.02 | 0.896 | 0.07 | 0.579 |
| Accuracy in congruent trials | 0.16 | 0.248 | 0.24 | 0.073 | 0.14 | 0.295 | 0.21 | 0.107 | |||
| Accuracy in incongruent trials | 0.05 | 0.710 | 0.11 | 0.433 | 0.00 | 0.990 | −0.05 | 0.681 | |||
| Alerting | 0.10 | 0.440 | 0.05 | 0.713 | −0.13 | 0.328 | −0.06 | 0.657 | |||
| Orienting | 0.05 | 0.722 | 0.10 | 0.477 | 0.05 | 0.723 | 0.06 | 0.655 | |||
| Executive | 0.07 | 0.583 | 0.12 | 0.389 | −0.04 | 0.778 | 0.10 | 0.427 | |||
| SART | Mean Reaction time in go trials | 57 | −0.06 | 0.634 | −0.03 | 0.837 | 61 | 0.11 | 0.380 | 0.08 | 0.542 |
| Coefficient of variation | 0.17 | 0.196 | 0.09 | 0.483 | −0.24 | 0.060 | −0.13 | 0.334 | |||
| Accuracy in go trials | −0.20 | 0.137 | −0.12 | 0.383 | 0.22 | 0.088 | 0.01 | 0.933 | |||
| Accuracy in no−go trials | −0.27 | 0.042 | −0.21 | 0.119 | 0.24 | 0.063 | 0.20 | 0.129 | |||
| Beta | SE | t | p | |
|---|---|---|---|---|
| Intercept | 0.33 | 0.32 | ||
| Transformed CoV | −0.55 | 0.23 | −0.24 | 0.81 |
| Group (ADHD = −1, Control = 1) | 0.65 | 0.33 | 1.98 | 0.050 |
| Height (centered) | 0.02 | 0.01 | 3.85 | <0.001 |
| Transformed CoV × Group | −0.51 | 0.24 | −2.17 | 0.032 |
| Model statistics | F(4, 113) = 7.12, p < 0.001, R2 = 0.15 Adjusted R2 = 0.12, interactionΔ R2 = 0.03 | |||
| Beta | SE | t | p | |
|---|---|---|---|---|
| Intercept | 0.26 | 0.08 | ||
| Accuracy in no-go trials | −0.04 | 0.09 | −0.43 | 0.66 |
| Group | 0.01 | 0.08 | 0.06 | 0.950 |
| Height (centered) | 0.02 | 0.01 | 3.57 | 0.001 |
| Accuracy in no-go trials× Group | 0.22 | 0.09 | 2.42 | 0.017 |
| Model statistics | F(4, 113) = 6.54, p < 0.001, R2 = 0.17 Adjusted R2 = 0.14, interaction ΔR2 = 0.05 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Racicka-Pawlukiewicz, E.; Kuć, K.; Bielecki, M.; Hanć, T.; Cybulska-Klosowicz, A.; Bryńska, A. The Association between Executive Functions and Body Weight/BMI in Children and Adolescents with ADHD. Brain Sci. 2021, 11, 178. https://doi.org/10.3390/brainsci11020178
Racicka-Pawlukiewicz E, Kuć K, Bielecki M, Hanć T, Cybulska-Klosowicz A, Bryńska A. The Association between Executive Functions and Body Weight/BMI in Children and Adolescents with ADHD. Brain Sciences. 2021; 11(2):178. https://doi.org/10.3390/brainsci11020178
Chicago/Turabian StyleRacicka-Pawlukiewicz, Ewa, Katarzyna Kuć, Maksymilian Bielecki, Tomasz Hanć, Anita Cybulska-Klosowicz, and Anita Bryńska. 2021. "The Association between Executive Functions and Body Weight/BMI in Children and Adolescents with ADHD" Brain Sciences 11, no. 2: 178. https://doi.org/10.3390/brainsci11020178
APA StyleRacicka-Pawlukiewicz, E., Kuć, K., Bielecki, M., Hanć, T., Cybulska-Klosowicz, A., & Bryńska, A. (2021). The Association between Executive Functions and Body Weight/BMI in Children and Adolescents with ADHD. Brain Sciences, 11(2), 178. https://doi.org/10.3390/brainsci11020178






