Impact of Alternate Gait Training Using Knee–Ankle–Foot Orthoses with Oil Damper Ankle Hinge in Patients with Subacute Severe Hemiplegia
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Subjects
2.2.1. Prospective Unified AGT Subjects
2.2.2. HC Subjects
2.2.3. Group Interventions
2.2.4. Intervention of Unified AGT Subjects
2.3. Clinical Measurements
2.4. Statistical Analyses
3. Results
3.1. Comparison of Demographics Data
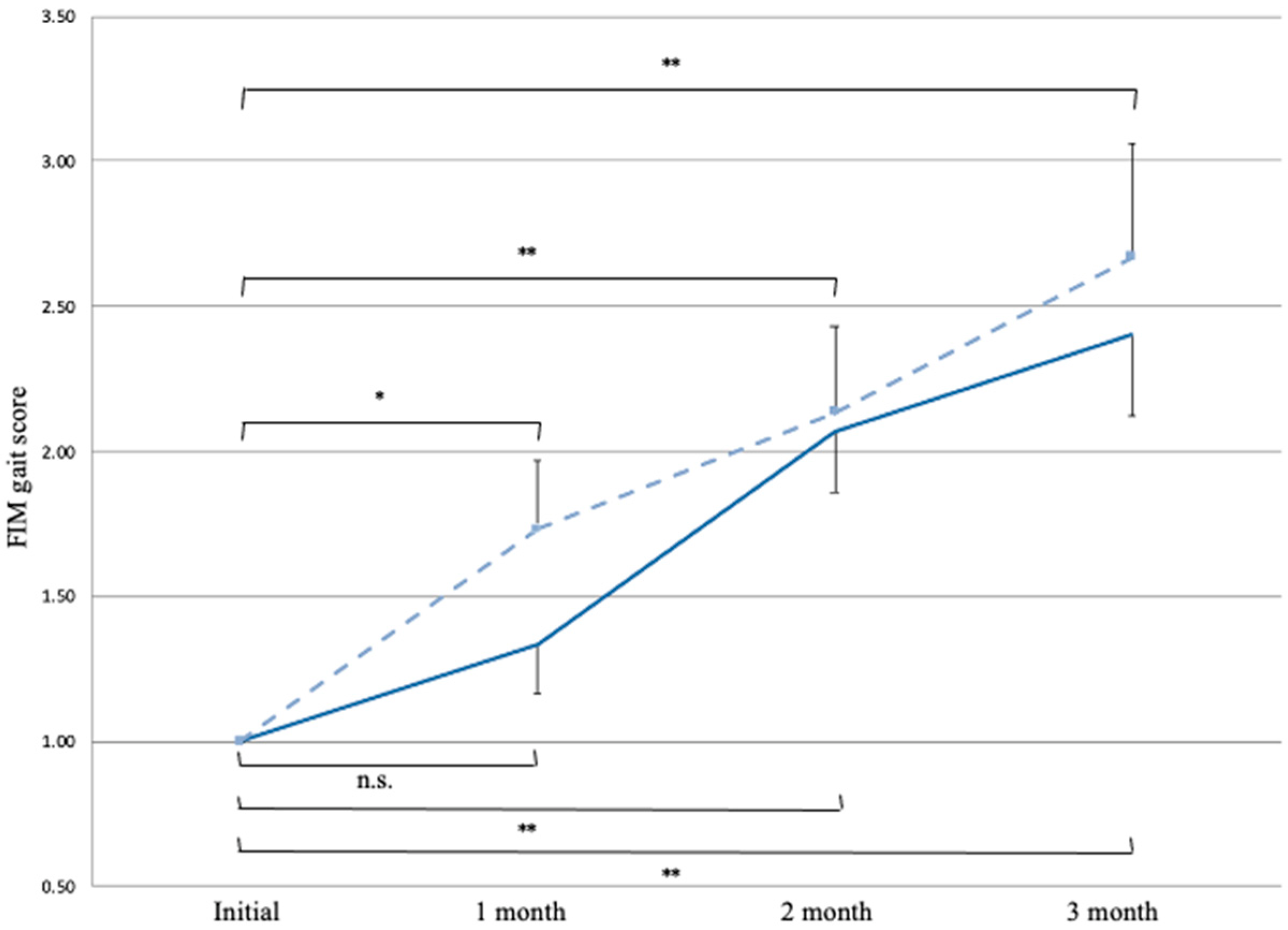
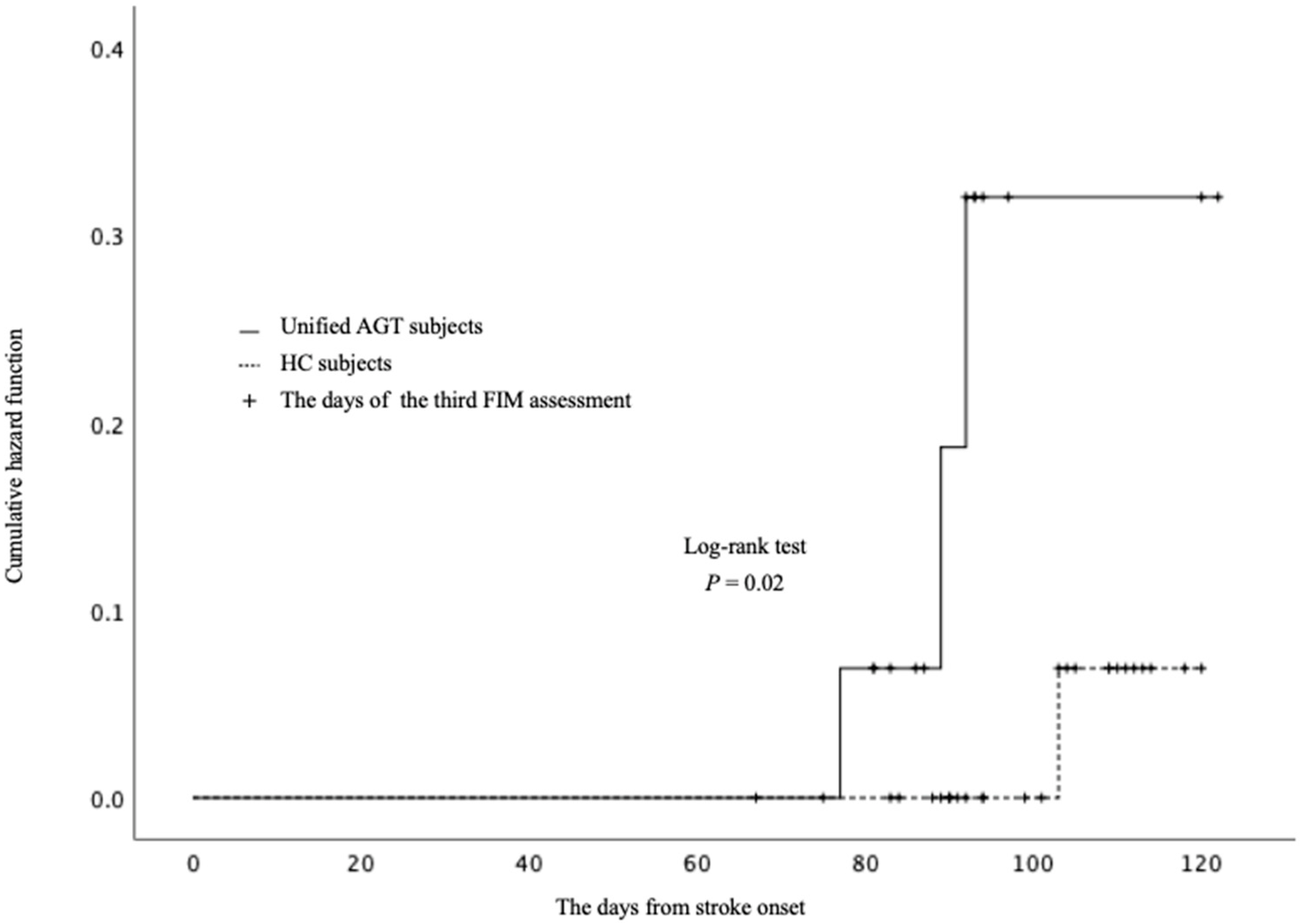
3.2. Effects of AGT on FIM Gait Scores
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hsiao, H.; Knarr, B.A.; Higginson, J.S.; Binder-Macleod, S.A. The relative contribution of ankle moment and trailing limb angle to propulsive force during gait. Hum. Mov. Sci. 2015, 39, 212–221. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jørgensen, H.S.; Nakayama, H.; Raaschou, H.O.; Olsen, T.S. Recovery of walking function in stroke patients: The Copenhagen Stroke Study. Arch. Phys. Med. Rehabil. 1995, 76, 27–32. [Google Scholar] [CrossRef]
- Ahn, Y.H.; Ahn, S.H.; Kim, H.; Hong, J.H.; Jang, S.H. Can stroke patients walk after complete lateral corticospinal tract injury of the affected hemisphere? Neuroreport 2006, 17, 987–990. [Google Scholar] [CrossRef] [PubMed]
- Nishio, D.; Hirano, Y.; Ito, S.; Kurata, M.; Kigawa, H.; Osawa, A.; Maeshima, S. A study on the outcome and clinical features of stroke patients with severe disability in a convalescent rehabilitation ward. Jpn. J. Stroke 2010, 32, 86–90. [Google Scholar] [CrossRef] [Green Version]
- Maeshima, S.; Okazaki, H.; Okamoto, S.; Mizuno, S.; Asano, N.; Maeda, H.; Masaki, M.; Matsuo, H.; Tsunoda, T.; Sonoda, S. A comparison of knee-ankle-foot orthoses with either metal struts or an adjustable posterior strut in hemiplegic stroke patients. J. Stroke Cerebrovasc. Dis. 2015, 24, 1312–1316. [Google Scholar] [CrossRef] [PubMed]
- Kakurai, S.; Akai, M. Clinical experiences with a convertible thermoplastic knee-ankle-foot orthosis for post-stroke hemiplegic patients. Prosthet. Orthot. Int. 1996, 20, 191–194. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Boudarham, J.; Zory, R.; Genet, F.; Vigné, G.; Bensmail, D.; Roche, N.; Pradon, D. Effects of a knee-ankle-foot orthosis on gait biomechanical characteristics of paretic and non-paretic limbs in hemiplegic patients with genu recurvatum. Clin. Biomech. 2013, 28, 73–78. [Google Scholar] [CrossRef] [PubMed]
- Takakusaki, K.; Kohyama, J.; Matsuyama, K.; Mori, S. Medullary reticulospinal tract mediating the generalized motor inhibition in cats: Parallel inhibitory mechanisms acting on motoneurons and on interneuronal transmission in reflex pathways. Neuroscience 2001, 103, 511–527. [Google Scholar] [CrossRef] [Green Version]
- Ballermann, M.; Fouad, K. Spontaneous locomotor recovery in spinal cord injured rats is accompanied by anatomical plasticity of reticulospinal fibers. Eur. J. Neurosci. 2006, 23, 1988–1996. [Google Scholar] [CrossRef] [PubMed]
- Matsuyama, K.; Mori, F.; Nakajima, K.; Drew, T.; Aoki, M.; Mori, S. Locomotor role of the corticoreticular-reticulospinal-spinal interneuronal system. Prog. Brain Res. 2004, 143, 239–249. [Google Scholar] [PubMed]
- Dietz, V.; Müller, R.; Colombo, G. Locomotor activity in spinal man: Significance of afferent input from joint and load receptors. Brain 2002, 125, 2626–2634. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kawashima, N.; Nozaki, D.; Abe, M.O.; Akai, M.; Nakazawa, K. Alternate leg movement amplifies locomotor-like muscle activity in spinal cord injured persons. J. Neurophysiol. 2005, 93, 777–785. [Google Scholar] [CrossRef] [PubMed]
- Data management service of the uniform data system for medical rehabilitation and the center for functional assessment research. In Guide for Use of the Uniform Data Set for Medical Rehabilitation Service, version 3.1; State University of New York at Buffalo: Buffalo, NY, USA, 1990.
- Miki, E.; Yamane, S.; Yamaoka, M.; Fujii, H.; Ueno, H.; Kawahara, T.; Tanaka, K.; Tamashiro, H.; Inoue, E.; Okamoto, T.; et al. Validity and reliability of the Japanese version of the FIM + FAM in patients with cerebrovascular accident. Scand J. Occup. Ther. 2016, 23, 398–404. [Google Scholar] [CrossRef] [PubMed]
- Liu, M.; Chino, N.; Tuji, T.; Masakado, Y.; Hase, K.; Kimura, A. Psychometric properties of the Stroke Impairment Assessment Set (SIAS). Neurorehabil. Neural. Repair 2002, 16, 339–351. [Google Scholar] [CrossRef] [PubMed]
- Chino, N.; Sonoda, S.; Domen, K.; Saitoh, E.; Kimura, A. Stroke impairment assessment set (SIAS): A new evaluation instrument for stroke patients. Jpn. J. Rehabil. Med. 1996, 31, 1199125. [Google Scholar] [CrossRef]
- Toba, K.; Nakai, R.; Akishika, M.; Iijima, S.; Nishinaga, M.; Mizoguchi, T.; Yamada, S.; Yumita, K.; Ouchi, Y. Vitality Index as a useful tool to assess elderly with dementia. Geriatr. Gerontol. Int. 2002, 2, 23–29. [Google Scholar] [CrossRef]
- Yamamoto, S.; Ibayashi, S.; Fuchi, M.; Yasui, T. Immediate-term effects of use of an ankle-foot orthosis with an oil damper on the gait of stroke patients when walking without the device. Prosthet. Orthot. Int. 2015, 39, 140–149. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, S.; Tomokiyo, N.; Yasui, T.; Kawaguchi, T. Effects of plantar flexion resistive moment generated by an ankle-foot orthosis with an oil damper on the gait of stroke patients: A pilot study. Prosthet. Orthot. Int. 2013, 37, 212–221. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ohata, K.; Yasui, T.; Tsuboyama, T.; Ichihashi, N. Effects of an ankle-foot orthosis with oil damper on muscle activity in adults after stroke. Gait Posture 2011, 33, 102–107. [Google Scholar] [CrossRef] [PubMed]


| Unified AGT Subjects | Historical Control Subjects | ||||||
|---|---|---|---|---|---|---|---|
| Mean ± SD or Number | Median, Interquartile Range | 95% CI | Mean ± SD or Number | Median, Interquartile Range | 95% CI | p-Value | |
| Number of subjects | 15 | 30 | |||||
| Age† | 77.1 ± 9.3 | 77.0, 14 | 71.9–82.2 | 77.9 ± 5.2 | 78.5, 7 | 75.9–79.8 | 0.76 |
| Sex (male/female) ‡ | 5/10 | 14/16 | 0.39 | ||||
| Etiology (SAH/INF/ICH/INF and ICH) ‡ | 0/9/6/0 | 2/17/10/1 | 0.65 | ||||
| Paretic side (Right/Left) ‡ | 9/6 | 12/18 | 0.21 | ||||
| Stroke recurrence (yes/no) ‡ | 3/12 | 7/23 | 0.8 | ||||
| Time from stroke to admission (days) * | 28.8 ± 11.2 | 27.0, 11 | 22.6–35.0 | 36.6 ± 14.6 | 37.0, 28 | 31.1–42.0 | 0.18 |
| Length of hospital stay (days) † | 120.5 ± 32.4 | 139.0, 46 | 102.5–138.4 | 120.5 ± 22.7 | 116.0, 35 | 112.1–129.0 | 0.99 |
| Duration of the use of Gait Innovation (days) | 41.8 ± 18.3 | 43.0, 28 | none | ||||
| Duration of physical therapy (minutes) † | 7980.0 ± 2388.0 | 6940.0, 4340 | 6658.0–9302.0 | 8330.0 ± 2642.0 | 8260.0, 3840 | 7343.8–9317.4 | 0.67 |
| Duration of occupational therapy (minutes) † | 6073.4 ± 2109.3 | 5240.0, 5640 | 4905.2–7241.4 | 6526.0 ± 1815.9 | 6700.0, 2000 | 5848.0–7204.0 | 0.61 |
| Initial ADL (FIM total) * | 36.9 ± 11.7 | 36.0, 19 | 30.4–43.3 | 33.9 ± 11.6 | 33.5, 17 | 29.6–38.4 | 0.43 |
| Initial gait ability (FIM gait) † | 1.0 ± 0.0 | 1, 0 | 1.0–1.0 | 1.0 ± 0.0 | 1, 0 | 1.0–1.0 | All patients score is 1 |
| Vitality index (E) motivation * | 1.2 ± 0.4 | 1.0, 1 | 0.97–1.43 | 1.1 ± 0.4 | 1.0, 1 | 1.0–1.26 | 0.57 |
| Vitality index total † | 5.8 ± 1.8 | 5.0, 3 | 4.8–6.8 | 6.1 ± 1.9 | 6.0, 2 | 5.4 -6.8 | 0.71 |
| SIAS motor hip * | 1.2 ± 1.4 | 0.0, 3 | 0.4–2.0 | 1.3 ± 1.3 | 1.0, 2 | 0.8–1.8 | 0.84 |
| SIAS motor knee * | 1.2 ± 1.5 | 0.0, 3 | 0.4–2.0 | 1.1 ± 1.2 | 1.0, 2 | 0.7–1.5 | 0.88 |
| SIAS motor ankle * | 0.8 ± 1.3 | 0.0, 2 | 0.1–1.5 | 0.9 ± 1.4 | 0.0, 2 | 0.4–1.5 | 0.83 |
| SIAS knee extension strength of the unaffected side * | 2.0 ± 0.8 | 2.0, 2 | 1.6–2.4 | 1.8 ± 1.0 | 1.5, 2 | 1.37–2.2 | 0.48 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abe, H.; Nishiyama, K.; Yamamoto, Y.; Okanuka, T.; Yonezawa, Y.; Matsumoto, K. Impact of Alternate Gait Training Using Knee–Ankle–Foot Orthoses with Oil Damper Ankle Hinge in Patients with Subacute Severe Hemiplegia. Brain Sci. 2021, 11, 1430. https://doi.org/10.3390/brainsci11111430
Abe H, Nishiyama K, Yamamoto Y, Okanuka T, Yonezawa Y, Matsumoto K. Impact of Alternate Gait Training Using Knee–Ankle–Foot Orthoses with Oil Damper Ankle Hinge in Patients with Subacute Severe Hemiplegia. Brain Sciences. 2021; 11(11):1430. https://doi.org/10.3390/brainsci11111430
Chicago/Turabian StyleAbe, Hiroaki, Kazutaka Nishiyama, Yuichi Yamamoto, Toru Okanuka, Yasuhito Yonezawa, and Koji Matsumoto. 2021. "Impact of Alternate Gait Training Using Knee–Ankle–Foot Orthoses with Oil Damper Ankle Hinge in Patients with Subacute Severe Hemiplegia" Brain Sciences 11, no. 11: 1430. https://doi.org/10.3390/brainsci11111430
APA StyleAbe, H., Nishiyama, K., Yamamoto, Y., Okanuka, T., Yonezawa, Y., & Matsumoto, K. (2021). Impact of Alternate Gait Training Using Knee–Ankle–Foot Orthoses with Oil Damper Ankle Hinge in Patients with Subacute Severe Hemiplegia. Brain Sciences, 11(11), 1430. https://doi.org/10.3390/brainsci11111430






