Considering Preventative Care in a Native vs. Non-native Language: A Foreign Language Effect
Abstract
1. Introduction
1.1. Evaluating Outcomes: How Bad Would It Be If Things Went Wrong?
1.2. Estimating Risks: What Is the Likelihood That Things Will Go Wrong?
1.3. Weighing Costs and Benefits: Will You Rely on Intuition or Data?
1.4. The Present Study
2. Materials and Methods
2.1. Participants
2.2. Design
2.3. Stimuli and Procedure
2.3.1. Structure of Scenarios
- One sentence describing a potential medical problem: You find out that millions of people are likely to get sick from the flu this year.
- Two sentences describing adverse effects associated with declining preventative treatment (i.e., disease symptoms): If you get the flu, you may experience a number of unpleasant symptoms such as a sore throat and fever. It could even turn into pneumonia, which can cause severe body aches and difficulty breathing.
- One sentence describing a benefit of accepting preventative treatment: You will greatly reduce your chance of catching the flu if you get a flu shot…
- Three sentences describing adverse effects associated with accepting preventative treatment (i.e., treatment complications): … but there are risks involved in getting the injection. Specifically, there may be soreness at the injection site. You may also experience weakness in your arms, making it difficult to perform normal tasks. You may also have allergic reactions to the shot, and experience negative symptoms such as difficulty breathing.
- Within each language condition, half of the participants were provided with the population risk associated with declining preventative care (i.e., disease symptoms). These participants read the following information after the description of the medical condition: According to estimates, approximately x% of people will experience one or more of the aforementioned negative effects if they do not receive the flu shot as preventative care.
- The remaining participants were provided with the population risk associated with accepting preventative care (i.e., treatment complications). These participants read the following information after the description of the preventative treatment: According to estimates, approximately x% of people will experience one or more of the aforementioned negative effects if they receive the flu shot as preventative care.
- Each of the 10 scenarios was randomly paired with a “low population risk” (2%, 9%, 16%, 23%, or 30%) or a “high population risk” (70%, 77%, 84%, 91%, or 98%). Assignment of risks to scenarios, as well as the order of scenarios was randomized for each participant.
2.3.2. Measures
- Willingness to accept preventative treatment: How willing would you be to get the flu shot as preventative care? (0 = Not willing at all; 100 = Extremely willing)
- Perceived (1) negativity and (2) risk of experiencing adverse effects associated with declining preventative care: As mentioned above, choosing NOT TO get the flu shot as preventative care can cause some negative effects (sore throat, fever, pneumonia, severe body aches, and death).
- ▪
- How bad do you think these negative effects are? (0 = Not bad at all; 100 = Extremely bad)
- ▪
- How likely do you think it is that you would experience these negative effects? (0 = Not likely at all; 100 = Extremely likely)
- Perceived (1) negativity and (2) risk of experiencing adverse effects associated with accepting preventative care: As mentioned above, choosing TO get the flu shot as preventative care can also cause some negative effects (soreness, weakness, difficulty performing tasks, allergic reaction, difficulty breathing).
- ▪
- How bad do you think these negative effects are? (0 = Not bad at all; 100 = Extremely bad)
- ▪
- How likely do you think it is that you would experience these negative effects? (0 = Not likely at all; 100 = Extremely likely)
3. Predictions and Analyses
- Hypothesis 1 (H1). Using a foreign language will attenuate the perceived negativity of potential adverse effects (i.e., disease symptoms and treatment complications).
- Hypothesis 2 (H2). Using a foreign language will reduce the perceived risk of potential adverse effects.
- Hypothesis 3 (H3). Using a foreign language will increase sensitivity to known population risks—that is, the effect of population risk on perceived personal risk should be greater in the foreign language than in the native language, particularly when population risks are directly relevant to the judgement (e.g., perceived personal risk of treatment complications based on known population risk of treatment complications).
- Hypothesis 4 (H4). Using a foreign language will increase sensitivity to the relative expected utility of accepting vs. declining preventative treatment—that is, the degree to which the expected harm of disease symptoms exceeds that of treatment complications.
- Language. Native (Chinese): −0.52 vs. Foreign (English): +0.48;
- Medical Event (i.e., the outcome being evaluated). Disease Symptoms: −0.50 vs. Treatment Complications: +0.50;
- Relevance (of population risk to judgment). Irrelevant (e.g., evaluating the disease with knowledge of population treatment risks): −0.50 vs. Relevant (e.g., evaluating the disease with knowledge of population disease risks): +0.50;
- Population Risk (continuous measure of population risk).
- Language. Native (Chinese): −0.52 vs. Foreign (English): +0.48;
- Risk Condition. Knowledge of population risks for the disease: −0.47 vs. Treatment: +0.53;
- Relative Treatment Utility (continuous measure of expected harm of declining treatment—expected harm of accepting treatment).
4. Results
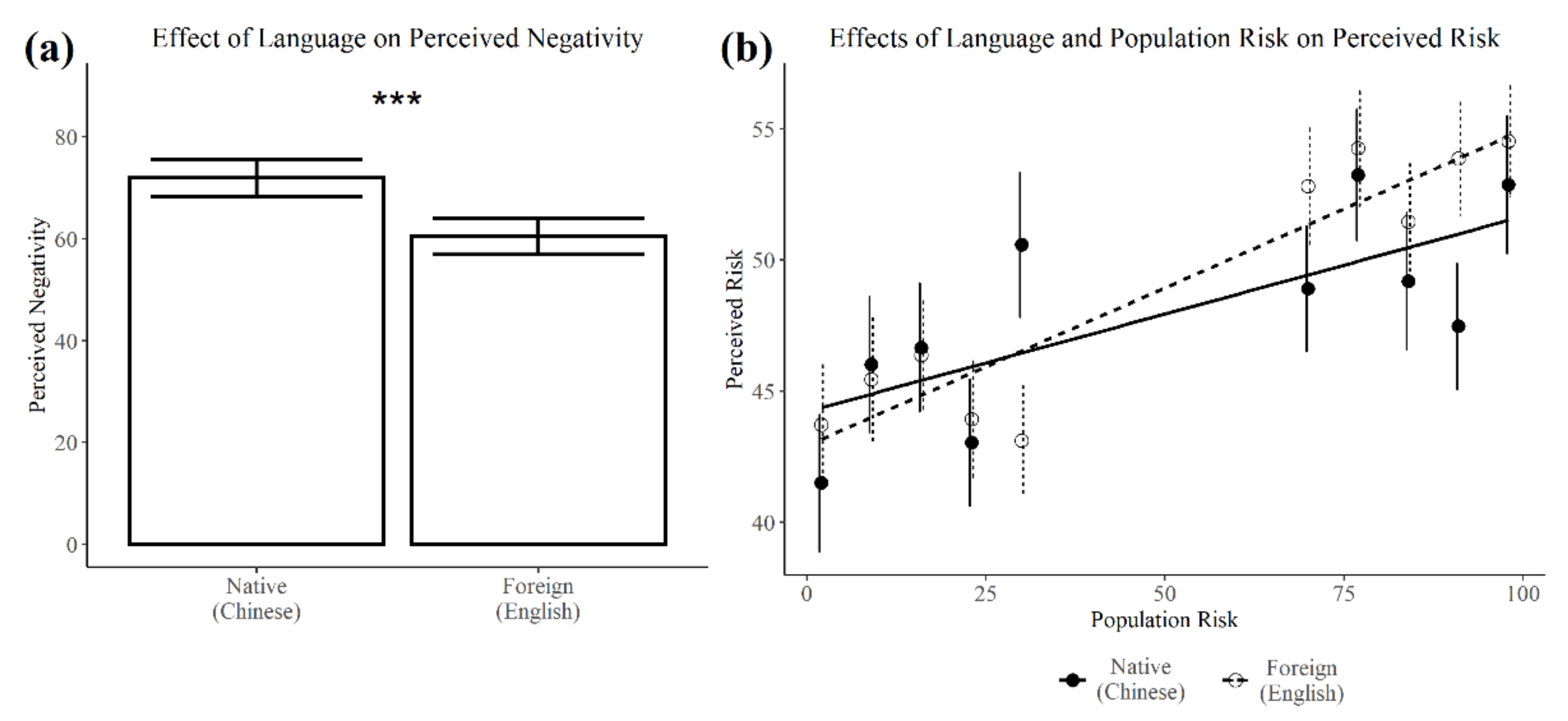
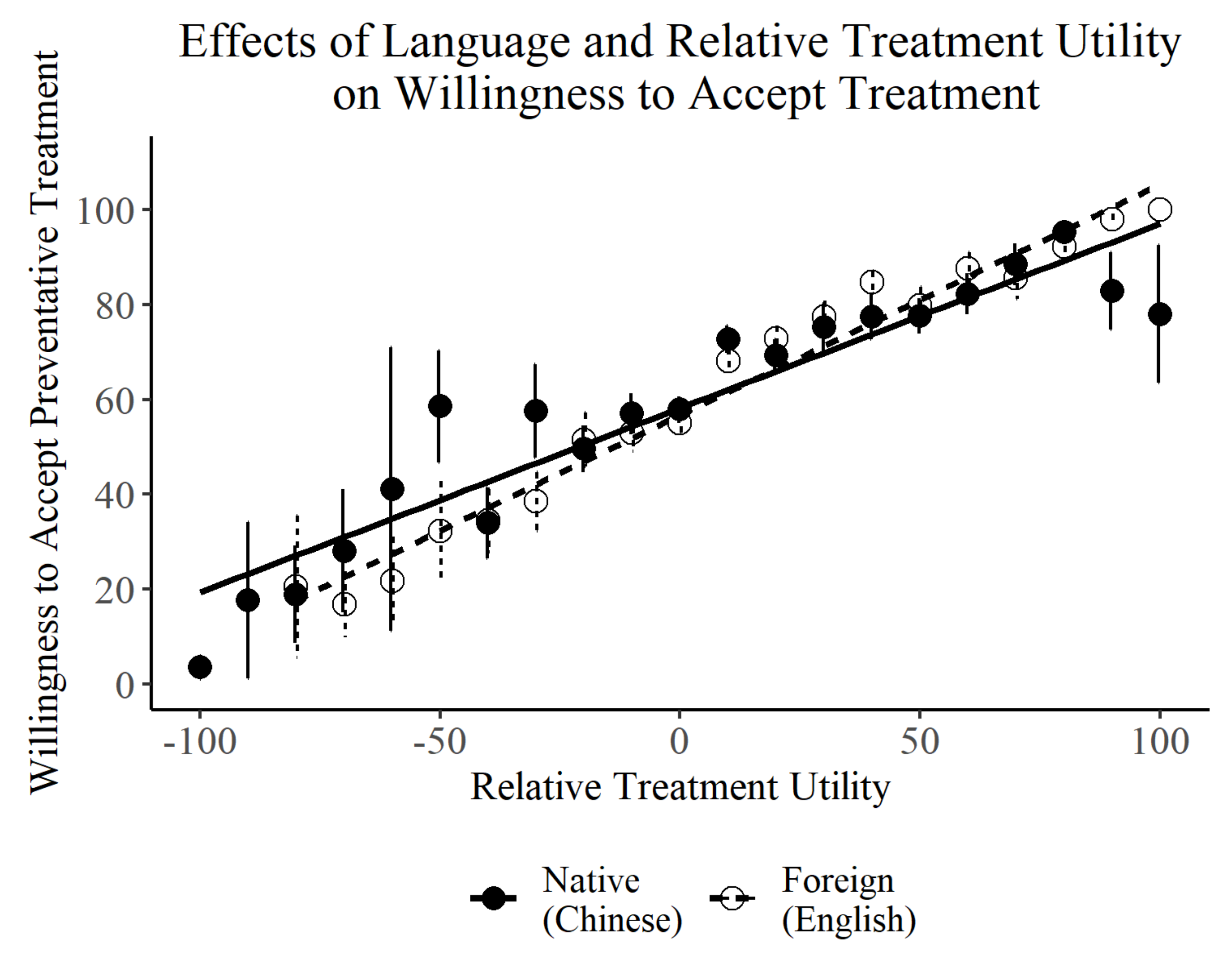
Effects of Language on Perceived Negativity, Perceived Risk, and Willingness to Accept Preventative Treatment
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
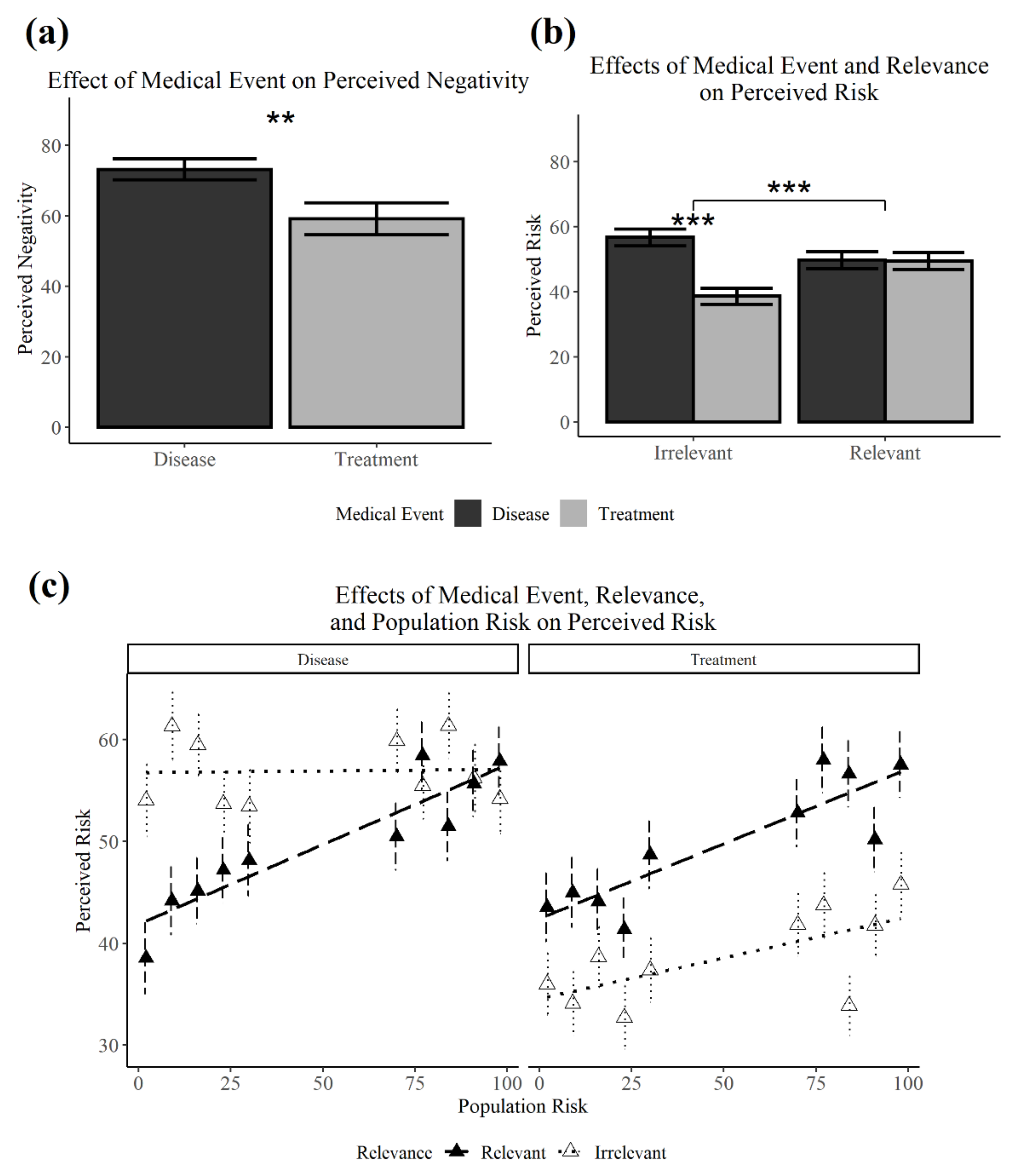
Appendix A. Effects of Medical Event on Perceived Negativity, Perceived Risk, and Willingness to Accept Preventative Treatment
| Estimate | SE | df | t | p | |
|---|---|---|---|---|---|
| Perceived Negativity | |||||
| Medical_Event | −13.79 | 3.21 | 14.13 | −4.29 | 0.001 ** |
| Medical_Event:Language | −3.05 | 3.28 | 484.83 | −0.93 | 0.354 |
| Medical_Event:Relevance | 6.40 | 4.42 | 270.62 | 1.45 | 0.149 |
| Medical_Event:Population_Risk | −0.01 | 0.02 | 2819.26 | −0.33 | 0.738 |
| Med:Lang:Rel | 11.24 | 8.86 | 270.53 | 1.27 | 0.206 |
| Med:Lang:PopRisk | −0.02 | 0.04 | 2824.13 | −0.57 | 0.568 |
| Med:Rel:PopRisk | 0.01 | 0.04 | 2819.59 | 0.12 | 0.906 |
| Med:Lang:Rel:PopRisk | −0.09 | 0.09 | 2819.49 | −1.02 | 0.309 |
| Perceived Risk | |||||
| Medical_Event | −10.48 | 2.75 | 23.1 | −3.81 | 0.001 ** |
| Medical_Event:Language | 1.7 | 3.82 | 454.25 | 0.45 | 0.656 |
| Medical_Event:Relevance | 23.76 | 5.1 | 266.58 | 4.66 | <0.001 *** |
| Medical_Event:Population_Risk | 0.03 | 0.02 | 2818.09 | 1.08 | 0.28 |
| Med:Lang:Rel | 11.72 | 10.22 | 266.5 | 1.15 | 0.252 |
| Med:Lang:PopRisk | 0.01 | 0.05 | 2823.25 | 0.26 | 0.791 |
| Med:Rel:PopRisk | −0.11 | 0.05 | 2821.69 | −2.22 | 0.026 * |
| Med:Lang:Rel:PopRisk | 0.09 | 0.1 | 2821.55 | 0.91 | 0.365 |
Appendix B. Full Output for Analyses of Perceived Negativity and Perceived Risk
| Estimate | SE | df | t | p | |
|---|---|---|---|---|---|
| (Intercept) | 64.48 | 3.55 | 10.76 | 18.17 | <0.001 *** |
| Language | −10.43 | 2.22 | 270.36 | −4.70 | <0.001 *** |
| Medical_Event | −13.79 | 3.21 | 14.13 | −4.29 | 0.001 ** |
| Relevance | −1.95 | 1.64 | 438.79 | −1.18 | 0.237 |
| Population_Risk | 0.03 | 0.01 | 2818.91 | 2.56 | 0.010 * |
| Lang:MedEvent | −3.05 | 3.28 | 484.83 | −0.93 | 0.354 |
| Lang:Rel | −3.87 | 3.28 | 484.31 | −1.18 | 0.239 |
| MedEvent:Rel | 6.40 | 4.42 | 270.62 | 1.45 | 0.149 |
| Lang:PopRisk | −0.02 | 0.02 | 2819.19 | −0.93 | 0.354 |
| MedEvent:PopRisk | −0.01 | 0.02 | 2819.26 | −0.33 | 0.738 |
| Rel:PopRisk | 0.03 | 0.02 | 2821.90 | 1.37 | 0.172 |
| Lang:MedEvent:Rel | 11.24 | 8.86 | 270.53 | 1.27 | 0.206 |
| Lang:MedEvent:PopRisk | −0.02 | 0.04 | 2824.13 | −0.57 | 0.568 |
| Lang:Rel:PopRisk | 0.07 | 0.04 | 2824.02 | 1.52 | 0.128 |
| MedEvent:Rel:PopRisk | 0.01 | 0.04 | 2819.59 | 0.12 | 0.906 |
| Lang:MedEvent:Rel:PopRisk | −0.09 | 0.09 | 2819.49 | −1.02 | 0.309 |
| Estimate | SE | df | t | p | |
|---|---|---|---|---|---|
| (Intercept) | 44.11 | 1.87 | 25.38 | 23.62 | <0.001 *** |
| Language | −2.14 | 2.55 | 266.66 | −0.84 | 0.403 |
| Medical_Event | −10.48 | 2.75 | 23.1 | −3.81 | 0.001 ** |
| Relevance | −3.29 | 1.93 | 311.8 | −1.71 | 0.089 |
| Population_Risk | 0.09 | 0.01 | 2819.64 | 7.23 | <0.001 *** |
| Lang:MedEvent | 1.7 | 3.82 | 454.25 | 0.45 | 0.656 |
| Lang:Rel | −2.74 | 3.82 | 453.83 | −0.72 | 0.474 |
| MedEvent:Rel | 23.76 | 5.1 | 266.58 | 4.66 | <0.001 *** |
| Lang:PopRisk | 0.05 | 0.02 | 2821.71 | 2.14 | 0.032 * |
| MedEvent:PopRisk | 0.03 | 0.02 | 2818.09 | 1.08 | 0.28 |
| Rel:PopRisk | 0.11 | 0.02 | 2817.71 | 4.25 | <0.001 *** |
| Lang:MedEvent:Rel | 11.72 | 10.22 | 266.5 | 1.15 | 0.252 |
| Lang:MedEvent:PopRisk | 0.01 | 0.05 | 2823.25 | 0.26 | 0.791 |
| Lang:Rel:PopRisk | 0.06 | 0.05 | 2823.38 | 1.13 | 0.257 |
| MedEvent:Rel:PopRisk | −0.11 | 0.05 | 2821.69 | −2.22 | 0.026 * |
| Lang:MedEvent:Rel:PopRisk | 0.09 | 0.1 | 2821.55 | 0.91 | 0.365 |
References
- Patel, Y.M.; Ly, D.P.; Hicks, T.; Jena, A.B. Proportion of non-US-born and noncitizen health care professionals in the United States in 2016. JAMA 2018, 320, 2265–2267. [Google Scholar] [CrossRef]
- Zeigler, K.; Camarota, S.A. 67.3 Million in the United States Spoke a Foreign Language at Home in 2018. Center for Immigration Studies. 2019. Available online: https://cis.org/Report/673-Million-United-States-Spoke-Foreign-Language-Home-2018 (accessed on 24 September 2020).
- Flores, G.; Abreu, M.; Schwartz, I.; Hill, M. The importance of language and culture in pediatric care: Case studies from the Latino community. J. Pediatr. 2000, 137, 842–848. [Google Scholar] [CrossRef] [PubMed]
- Showstack, R.E.; Guzman, K.; Chesser, A.K.; Woods, N.K. Improving Latino health equity through spanish language interpreter advocacy in Kansas. Hisp. Health Care Int. 2019, 17, 18–22. [Google Scholar] [CrossRef] [PubMed]
- Tang, A.S.; Kruger, J.F.; Quan, J.; Fernandez, A. From admission to discharge: Patterns of interpreter use among resident physicians caring for hospitalized patients with limited English proficiency. J. Health Care Poor Underserved 2014, 25, 1784–1798. [Google Scholar] [CrossRef] [PubMed]
- Hsueh, L.; Hirsh, A.T.; Maupomé, G.; Stewart, J.C. Patient–provider language concordance and health outcomes: A systematic review, evidence map, and research agenda. Med. Care Res. Rev. 2019, 78, 3–23. [Google Scholar] [CrossRef]
- Baquiran, C.L.C.; Nicoladis, E. A doctor’s foreign accent affects perceptions of competence. Health Commun. 2020, 35, 726–730. [Google Scholar] [CrossRef] [PubMed]
- Martínez, G. Language and power in healthcare: Towards a theory of language barriers among linguistic minorities in the United States. Read. Lang. Stud. Lang. Power 2010, 2, 59–74. [Google Scholar]
- Steinberg, E.M.; Valenzuela-Araujo, D.; Zickafoose, J.S.; Kieffer, E.; DeCamp, L.R. The “battle” of managing language barriers in health care. Clin. Pediatrics 2016, 55, 1318–1327. [Google Scholar] [CrossRef]
- Gu, Y.; Shah, A.P. A systematic review of interventions to address accent-related communication problems in healthcare. Ochsner J. 2019, 19, 378–396. [Google Scholar] [CrossRef]
- Bereby-Meyer, Y.; Hayakawa, S.; Shalvi, S.; Corey, J.D.; Costa, A.; Keysar, B. Honesty speaks a second language. Top. Cogn. Sci. 2019, 12, 632–643. [Google Scholar] [CrossRef]
- Corey, J.D.; Hayakawa, S.; Foucart, A.; Aparici, M.; Botella, J.; Costa, A.; Keysar, B. Our moral choices are foreign to us. J. Exp. Psychol. Learn. Mem. Cogn. 2017, 43, 1109–1128. [Google Scholar] [CrossRef]
- Costa, A.; Foucart, A.; Hayakawa, S.; Aparici, M.; Apesteguia, J.; Heafner, J.; Keysar, B. Your morals depend on language. PLoS ONE 2014, 9, e94842. [Google Scholar] [CrossRef] [PubMed]
- Costa, A.; Corey, J.D.; Hayakawa, S.; Aparici, M.; Vives, M.-L.; Keysar, B. The role of intentions and outcomes in the foreign language effect on moral judgements. Q. J. Exp. Psychol. 2018, 72, 8–17. [Google Scholar] [CrossRef]
- Geipel, J.; Hadjichristidis, C.; Surian, L. How foreign language shapes moral judgment. J. Exp. Soc. Psychol. 2015, 59, 8–17. [Google Scholar] [CrossRef]
- Hayakawa, S.; Tannenbaum, D.; Costa, A.; Corey, J.D.; Keysar, B. Thinking more or feeling less? Explaining the foreign-language effect on moral judgment. Psychol. Sci. 2017, 28, 1387–1397. [Google Scholar] [CrossRef] [PubMed]
- Hayakawa, S.; Keysar, B. Using a foreign language reduces mental imagery. Cognition 2018, 173, 8–15. [Google Scholar] [CrossRef]
- Costa, A.; Foucart, A.; Arnon, I.; Aparici, M.; Apesteguia, J. “Piensa” twice: On the foreign language effect in decision making. Cognition 2014, 130, 236–254. [Google Scholar] [CrossRef]
- Hayakawa, S.; Lau, B.K.Y.; Holtzmann, S.; Costa, A.; Keysar, B. On the reliability of the foreign language effect on risk-taking. Q. J. Exp. Psychol. 2019, 72, 29–40. [Google Scholar] [CrossRef]
- Keysar, B.; Hayakawa, S.L.; An, S.G. The foreign-language effect: Thinking in a foreign tongue reduces decision biases. Psychol. Sci. 2012, 23, 661–668. [Google Scholar] [CrossRef]
- Antón, E.; Soleto, N.B.; Duñabeitia, J.A. Recycling in Babel: The impact of foreign languages in rule learning. Int. J. Environ. Res. Public Health 2020, 17, 3784. [Google Scholar] [CrossRef]
- Geipel, J.; Hadjichristidis, C.; Klesse, A.-K. Barriers to sustainable consumption attenuated by foreign language use. Nat. Sustain. 2018, 1, 31–33. [Google Scholar] [CrossRef]
- Karataş, M. Making decisions in foreign languages: Weaker senses of ownership attenuate the endowment effect. J. Consum. Psychol. 2020, 30, 296–303. [Google Scholar] [CrossRef]
- Krishna, A.; Ahluwalia, R. Language choice in advertising to bilinguals: Asymmetric effects for multinationals versus local firms. J. Consum. Res. 2008, 35, 692–705. [Google Scholar] [CrossRef]
- Puntoni, S.; De Langhe, B.; Van Osselaer, S.M.J. Bilingualism and the emotional intensity of advertising language. J. Consum. Res. 2009, 35, 1012–1025. [Google Scholar] [CrossRef]
- Schervish, M.J.; Pratt, J.W.; Raiffa, H.; Schlaifer, R. Introduction to Statistical Decision Theory; MIT Press: Cambridge, MA, USA, 1996. [Google Scholar]
- Pham, M.T. Emotion and rationality: A critical review and interpretation of empirical evidence. Rev. Gen. Psychol. 2007, 11, 155–178. [Google Scholar] [CrossRef]
- Power, T.E.; Swartzman, L.C.; Robinson, J.W. Cognitive-emotional decision making (CEDM): A framework of patient medical decision making. Patient Educ. Couns. 2011, 83, 163–169. [Google Scholar] [CrossRef]
- Slovic, P.; Finucane, M.; Peters, E.; MacGregor, D.G. Rational actors or rational fools: Implications of the affect heuristic for behavioral economics. J. Socio-Econ. 2002, 31, 329–342. [Google Scholar] [CrossRef]
- Schwartz, M.D.; Peshkin, B.N.; Tercyak, K.P.; Taylor, K.L.; Valdimarsdottir, H. Decision making and decision support for hereditary breast-ovarian cancer susceptibility. Health Psychol. 2005, 24, S78–S84. [Google Scholar] [CrossRef]
- Gerend, M.A.; Maner, J.K. Fear, anger, fruits, and veggies: Interactive effects of emotion and message framing on health behavior. Health Psychol. 2011, 30, 420–423. [Google Scholar] [CrossRef]
- Gutnik, L.; Hakimzada, A.F.; Yoskowitz, N.A.; Patel, V.L. The role of emotion in decision-making: A cognitive neuroeconomic approach towards understanding sexual risk behavior. J. Biomed. Informatics 2006, 39, 720–736. [Google Scholar] [CrossRef]
- Ellis, E.M.; Klein, W.M.P.; Orehek, E.; Ferrer, R.A. Effects of emotion on medical decisions involving tradeoffs. Med. Decis. Mak. 2018, 38, 1027–1039. [Google Scholar] [CrossRef] [PubMed]
- Waters, E.A.; Weinstein, N.D.; Colditz, G.A.; Emmons, K.M. Aversion to side effects in preventive medical treatment decisions. Br. J. Health Psychol. 2007, 12, 383–401. [Google Scholar] [CrossRef] [PubMed]
- Waters, E.A.; Weinstein, N.D.; Colditz, G.A.; Emmons, K.M. Reducing aversion to side effects in preventive medical treatment decisions. J. Exp. Psychol. Appl. 2007, 13, 11–21. [Google Scholar] [CrossRef]
- Waters, E.A.; Weinstein, N.D.; Colditz, G.A.; Emmons, K. Explanations for side effect aversion in preventive medical treatment decisions. Health Psychol. 2009, 28, 201–209. [Google Scholar] [CrossRef]
- Waters, E.A.; Pachur, T.; Colditz, G.A. Side effect perceptions and their impact on treatment decisions in women. Med. Decis. Mak. 2017, 37, 193–203. [Google Scholar] [CrossRef] [PubMed]
- Ritov, I.; Baron, J. Reluctance to vaccinate: Omission bias and ambiguity. J. Behav. Decis. Mak. 1990, 3, 263–277. [Google Scholar] [CrossRef]
- Spranca, M.; Minsk, E.; Baron, J. Omission and commission in judgment and choice. J. Exp. Soc. Psychol. 1991, 27, 76–105. [Google Scholar] [CrossRef]
- Dewaele, J.-M. The emotional weight of I love you in multilinguals’ languages. J. Pragmat. 2008, 40, 1753–1780. [Google Scholar] [CrossRef]
- Pavlenko, A. Affective processing in bilingual speakers: Disembodied cognition? Int. J. Psychol. 2012, 47, 405–428. [Google Scholar] [CrossRef]
- Caldwell-Harris, C.L.; Ayçiçeği-Dinn, A. Emotion and lying in a non-native language. Int. J. Psychophysiol. 2009, 71, 193–204. [Google Scholar] [CrossRef]
- Iacozza, S.; Costa, A.; Duñabeitia, J.A. What do your eyes reveal about your foreign language? Reading emotional sentences in a native and foreign language. PLoS ONE 2017, 12, e0186027. [Google Scholar] [CrossRef]
- Hsu, C.-T.; Jacobs, A.M.; Conrad, M. Can Harry Potter still put a spell on us in a second language? An fMRI study on reading emotion-laden literature in late bilinguals. Cortex 2015, 63, 282–295. [Google Scholar] [CrossRef]
- Jankowiak, K.; Korpal, P. On modality effects in bilingual emotional language processing: Evidence from galvanic skin response. J. Psycholinguist. Res. 2018, 47, 663–677. [Google Scholar] [CrossRef]
- Jończyk, R.; Boutonnet, B.; Musiał, K.; Hoemann, K.; Thierry, G. The bilingual brain turns a blind eye to negative statements in the second language. Cogn. Affect. Behav. Neurosci. 2016, 16, 527–540. [Google Scholar] [CrossRef] [PubMed]
- Dewaele, J.-M.; Costa, B. Multilingual clients’ experience of psychotherapy. Lang. Psychoanal. 2013, 2, 31–50. [Google Scholar] [CrossRef]
- García-Palacios, A.; Costa, A.; Castilla, D.; Del Río, E.; Casaponsa, A.; Duñabeitia, J.A. The effect of foreign language in fear acquisition. Sci. Rep. 2018, 8, 1157. [Google Scholar] [CrossRef] [PubMed]
- Marian, V.; Fausey, C.M. Language-dependent memory in bilingual learning. Appl. Cogn. Psychol. 2006, 20, 1025–1047. [Google Scholar] [CrossRef]
- Marian, V.; Kaushanskaya, M. Self-construal and emotion in bicultural bilinguals. J. Mem. Lang. 2004, 51, 190–201. [Google Scholar] [CrossRef]
- Marian, V.; Kaushanskaya, M. Language context guides memory content. Psychon. Bull. Rev. 2007, 14, 925–933. [Google Scholar] [CrossRef] [PubMed]
- Marian, V.; Neisser, U. Language-dependent recall of autobiographical memories. J. Exp. Psychol. Gen. 2000, 129, 361–368. [Google Scholar] [CrossRef]
- Marian, V.; Kaushanskaya, M. Language-dependent memory: Insights from bilingualism. In Relations Between Language and Memory; Zelinsky-Wibbelt, C., Ed.; Peter Lang: Bern, Switzerland, 2011. [Google Scholar]
- Freeman, M.R.; Shook, A.; Marian, V. Cognitive and emotional effects of bilingualism in adulthood. In Bilingualism Across the Lifespan: Factors Moderating Language Proficiency; Nicoladis, E., Montanari, S., Eds.; American Psychological Association: Washington, DC, USA, 2016. [Google Scholar]
- Białek, M.; Muda, R.; Stewart, K.; Niszczota, P.; Pieńkosz, D. Thinking in a foreign language distorts allocation of cognitive effort: Evidence from reasoning. Cognition 2020, 205, 104420. [Google Scholar] [CrossRef] [PubMed]
- Polonioli, A. A Blind spot in research on foreign language effects in judgment and decision-making. Front. Psychol. 2018, 9, 227. [Google Scholar] [CrossRef]
- Caldwell-Harris, C.L.; Ayçiçeği-Dinn, A. When using the native language leads to more ethical choices: Integrating ratings and electrodermal monitoring. Lang. Cogn. Neurosci. 2020, 36, 885–901. [Google Scholar] [CrossRef]
- Damasio, A.R.; Tranel, D.; Damasio, H.C. Somatic markers and the guidance of behaviour: Theory and preliminary testing. In Frontal Lobe Function and Dysfunction; Levin, H.S., Eisenberg, H.M., Benton, A.L., Eds.; Oxford University Press: Oxford, UK, 1991; pp. 217–229. [Google Scholar]
- Youssef, F.F.; Dookeeram, K.; Basdeo, V.; Francis, E.; Doman, M.; Mamed, D.; Maloo, S.; Degannes, J.; Dobo, L.; Ditshotlo, P.; et al. Stress alters personal moral decision making. Psychoneuroendocrinology 2012, 37, 491–498. [Google Scholar] [CrossRef] [PubMed]
- Greene, J.D.; Morelli, S.; Lowenberg, K.; Nystrom, L.E.; Cohen, J.D. Cognitive load selectively interferes with utilitarian moral judgment. Cognition 2008, 107, 1144–1154. [Google Scholar] [CrossRef] [PubMed]
- Kahneman, D. Maps of bounded rationality: Psychology for behavioral economics. Am. Econ. Rev. 2003, 93, 1449–1475. [Google Scholar] [CrossRef]
- Hayakawa, S.; Costa, A.; Foucart, A.; Keysar, B. Using a foreign language changes our choices. Trends Cogn. Sci. 2016, 20, 791–793. [Google Scholar] [CrossRef] [PubMed]
- Alter, A.L.; Oppenheimer, D.M.; Epley, N.; Eyre, R.N. Overcoming intuition: Metacognitive difficulty activates analytic reasoning. J. Exp. Psychol. Gen. 2007, 136, 569–576. [Google Scholar] [CrossRef]
- Frederick, S. Cognitive Reflection and Decision Making. J. Econ. Perspect. 2005, 19, 25–42. [Google Scholar] [CrossRef]
- Oganian, Y.; Korn, C.W.; Heekeren, H.R. Language switching—But not foreign language use per se—reduces the framing effect. J. Exp. Psychol. 2016, 42, 140–148. [Google Scholar] [CrossRef]
- Wu, Y.J.; Thierry, G. Fast modulation of executive function by language context in bilinguals. J. Neurosci. 2013, 33, 13533–13537. [Google Scholar] [CrossRef] [PubMed]
- Luk, G.; Green, D.W.; Abutalebi, J.; Grady, C. Cognitive control for language switching in bilinguals: A quantitative meta-analysis of functional neuroimaging studies. Lang. Cogn. Process. 2012, 27, 1479–1488. [Google Scholar] [CrossRef] [PubMed]
- Harris, A.J.; Corner, A.; Hahn, U. Estimating the probability of negative events. Cognition 2009, 110, 51–64. [Google Scholar] [CrossRef]
- Colomé, À.; Rodríguez-Ferreiro, J.; Tubau, E. Too worried to judge: On the role of perceived severity in medical decision-making. Front. Psychol. 2018, 9, 1906. [Google Scholar] [CrossRef] [PubMed]
- Haase, N.; Renkewitz, F.; Betsch, C. The measurement of subjective probability: Evaluating the sensitivity and accuracy of various scales. Risk Anal. 2013, 33, 1812–1828. [Google Scholar] [CrossRef]
- Slovic, P. Perception of risk. Science 1987, 236, 280–285. [Google Scholar] [CrossRef]
- Leventhal, H.; Kelly, K.; Leventhal, E.A. Population risk, actual risk, perceived risk, and cancer control: A discussion. J. Natl. Cancer Inst. Monogr. 1999, 1999, 81–85. [Google Scholar] [CrossRef] [PubMed]
- Hadjichristidis, C.; Geipel, J.; Savadori, L. The effect of foreign language in judgments of risk and benefit: The role of affect. J. Exp. Psychol. Appl. 2015, 21, 117–129. [Google Scholar] [CrossRef]
- Ascher, D.; Polowczyk, J.; Wielicka-Regulska, A.; da Silva, W.V.; Souza, A. The foreign language effect in risk decision-making: A cross-country review of Brazilians and Poles behavior in a loss aversion experiment. In Proceedings of the 8th International Conference on E-business, Management and Economics, Birmingham, UK, 27–29 October 2017; pp. 42–45. [Google Scholar]
- He, Y.; Margoni, F.; Wu, Y.; Liu, H. fMRI evidence reveals emotional biases in bilingual decision making. Brain Struct. Funct. 2021, 226, 1405–1421. [Google Scholar] [CrossRef] [PubMed]
- Zheng, L.; Mobbs, D.; Yu, R. The behavioral and neural basis of foreign language effect on risk-taking. Neuropsychologia 2019, 136, 107290. [Google Scholar] [CrossRef]
- Eichenbaum, H. Comparative cognition, hippocampal function, and recollection. Comp. Cogn. Behav. Rev. 2007, 2, 47–66. [Google Scholar] [CrossRef][Green Version]
- Ramirez, S.; Tonegawa, S.; Liu, X. Identification and optogenetic manipulation of memory engrams in the hippocampus. Front. Behav. Neurosci. 2014, 7, 226. [Google Scholar] [CrossRef] [PubMed]
- Zhang, T.R.; Larosa, A.; Di Raddo, M.E.; Wong, V.; Wong, A.S.; Wong, T.P. Negative memory engrams in the hippocampus enhance the susceptibility to chronic social defeat stress. J. Neurosci. 2019, 39, 7576–7590. [Google Scholar] [CrossRef]
- Zhu, Y.; Gao, H.; Tong, L.; Li, Z.; Wang, L.; Zhang, C.; Yang, Q.; Yan, B. Emotion regulation of hippocampus using real-time fMRI neurofeedback in healthy human. Front. Hum. Neurosci. 2019, 13, 242. [Google Scholar] [CrossRef]
- Abutalebi, J.; Della Rosa, P.A.; Ding, G.; Weekes, B.; Costa, A.; Green, D.W. Language proficiency modulates the engagement of cognitive control areas in multilinguals. Cortex 2013, 49, 905–911. [Google Scholar] [CrossRef]
- Branzi, F.M.; Della Rosa, P.A.; Canini, M.; Costa, A.; Abutalebi, J. Language control in bilinguals: Monitoring and response selection. Cereb. Cortex 2015, 26, 2367–2380. [Google Scholar] [CrossRef]
- Trémolière, B.; Maheux-Caron, V.; Lepage, J.-F.; Blanchette, I. tDCS stimulation of the dlPFC selectively moderates the detrimental impact of emotion on analytical reasoning. Front. Psychol. 2018, 9, 5688. [Google Scholar] [CrossRef]
- Chang, H.H.; Pham, M.T. Affective boundaries of scope insensitivity. J. Consum. Res. 2018, 45, 403–428. [Google Scholar] [CrossRef]
- Hsee, C.K.; Rottenstreich, Y. Music, pandas, and muggers: On the affective psychology of value. J. Exp. Psychol. Gen. 2004, 133, 23–30. [Google Scholar] [CrossRef] [PubMed]
- Rottenstreich, Y.; Hsee, C.K. Money, kisses, and electric shocks: On the affective psychology of risk. Psychol. Sci. 2001, 12, 185–190. [Google Scholar] [CrossRef]
- Pachur, T.; Hertwig, R.; Wolkewitz, R. The affect gap in risky choice: Affect-rich outcomes attenuate attention to probability information. Decision 2014, 1, 64–78. [Google Scholar] [CrossRef]
- Goldberg, I.; Roosen, J. Scope insensitivity in health risk reduction studies: A comparison of choice experiments and the contingent valuation method for valuing safer food. J. Risk Uncertain. 2007, 34, 123–144. [Google Scholar] [CrossRef]
- Qualtrics. Computer Software. Available online: http://www.qualtrics.com (accessed on 19 November 2020).
- Marian, V.; Blumenfeld, H.K.; Kaushanskaya, M. The language experience and proficiency questionnaire (LEAP-Q): Assessing language profiles in bilinguals and multilinguals. J. Speech Lang. Hear. Res. 2007, 50, 940–967. [Google Scholar] [CrossRef]
- Hayakawa, S.; Pan, Y.; Marian, V. Language changes medical judgments and beliefs. Int. J. Biling. 2021. [CrossRef]
- Brislin, R.W. Back-Translation for Cross-Cultural Research. J. Cross-Cult. Psychol. 1970, 1, 185–216. [Google Scholar] [CrossRef]
- Flesch, R. A new readability yardstick. J. Appl. Psychol. 1948, 32, 221–233. [Google Scholar] [CrossRef]
- Barr, D.J.; Levy, R.; Scheepers, C.; Tily, H.J. Random effects structure for confirmatory hypothesis testing: Keep it maximal. J. Mem. Lang. 2013, 68, 255–278. [Google Scholar] [CrossRef]
- Sharot, T.; Garrett, N. Forming beliefs: Why valence matters. Trends Cogn. Sci. 2016, 20, 25–33. [Google Scholar] [CrossRef]
- Oganian, Y.; Heekeren, H.R.; Korn, C.W. Low foreign language proficiency reduces optimism about the personal future. Q. J. Exp. Psychol. 2018, 72, 60–75. [Google Scholar] [CrossRef]
- Trémolière, B.; De Neys, W. Methodological concerns in moral judgement research: Severity of harm shapes moral decisions. J. Cogn. Psychol. 2013, 25, 989–993. [Google Scholar] [CrossRef]
- Cipolletti, H.; McFarlane, S.; Weissglass, C. The moral foreign-language effect. Philos. Psychol. 2014, 29, 23–40. [Google Scholar] [CrossRef]
- Thomson, J. The trolley problem. Yale Law J. 1985, 94, 1395–1415. [Google Scholar] [CrossRef]
- Foot, P. The problem of abortion and the doctrine of double effect. In Virtues and Vices; Blackwell: Oxford, UK, 1978; pp. 19–32. [Google Scholar]
- Białek, M.; Paruzel-Czachura, M.; Gawronski, B. Foreign language effects on moral dilemma judgments: An analysis using the CNI model. J. Exp. Soc. Psychol. 2019, 85, 103855. [Google Scholar] [CrossRef]
- Mækelæ, J.M.; Pfuhl, G. Deliberate reasoning is not affected by language. PLoS ONE 2019, 14, e0211428. [Google Scholar] [CrossRef]
- Vives, M.-L.; Aparici, M.; Costa, A. The limits of the foreign language effect on decision-making: The case of the outcome bias and the representativeness heuristic. PLoS ONE 2018, 13, e0203528. [Google Scholar] [CrossRef]
- Muda, R.; Niszczota, P.; Białek, M.; Conway, P. Reading dilemmas in a foreign language reduces both deontological and utilitarian response tendencies. J. Exp. Psychol. Learn. Mem. Cogn. 2018, 44, 321–326. [Google Scholar] [CrossRef]
- Akkermans, A.P.D.; Harzing, A.-W.; van Witteloostuijn, A. Cultural accommodation and language priming. Manag. Int. Rev. 2010, 50, 559–583. [Google Scholar] [CrossRef]
- Ralston, D.A.; Cunniff, M.K.; Gustafson, D.J. Cultural accommodation: The effect of language on the response of bilingual Hong Kong Chinese managers. J. Cross-Cult. Psychol. 1995, 26, 714–727. [Google Scholar] [CrossRef]
- Ramírez-Esparza, N.; Gosling, S.; Benet-Martinez, V.; Potter, J.P.; Pennebaker, J.W. Do bilinguals have two personalities? A special case of cultural frame switching. J. Res. Pers. 2006, 40, 99–120. [Google Scholar] [CrossRef]
- Ross, M.; Xun, W.E.; Wilson, A.E. Language and the bicultural self. Personal. Soc. Psychol. Bull. 2002, 28, 1040–1050. [Google Scholar] [CrossRef]
- Verkuyten, M.; Pouliasi, K. Biculturalism among older children: Cultural frame switching, attributions, self-identification, and attitudes. J. Cross-Cult. Psychol. 2002, 33, 596–609. [Google Scholar] [CrossRef]
- Matsumoto, D. Cultural similarities and differences in display rules. Motiv. Emot. 1990, 14, 195–214. [Google Scholar] [CrossRef]
- Panayiotou, A. Switching codes, switching code: Bilinguals’ emotional responses in English and Greek. J. Multiling. Multicult. Dev. 2004, 25, 124–139. [Google Scholar] [CrossRef]
- Arkes, H.R.; Blumer, C. The psychology of sunk cost. Organ. Behav. Hum. Decis. Process. 1985, 35, 124–140. [Google Scholar] [CrossRef]
- Meyers, E.A.; Białek, M.; Fugelsang, J.A.; Koehler, D.J.; Friedman, O. Wronging past rights: The sunk cost bias distorts moral judgment. Judgm. Decis. Mak. 2019, 14, 721–727. [Google Scholar]
| Native Mandarin | Non-Native English | p | |
|---|---|---|---|
| Age | 25.93 (4.29) | 25.63 (3.55) | 0.63 |
| Gender | 53% Female | 56% Female | 0.79 |
| Mandarin AoA | 0.77 (1.81) | 0.88 (1.87) | 0.72 |
| English AoA | 6.24 (3.65) | 6.00 (3.31) | 0.67 |
| Mandarin AoR | 3.19 (2.83) | 3.07 (2.80) | 0.80 |
| English AoR | 7.38 (3.64) | 7.23 (3.28) | 0.78 |
| Mandarin Speaking | 9.67 (0.99) | 9.49 (1.41) | 0.31 |
| English Speaking | 7.84 (1.41) | 7.26 (1.42) | 0.01 * |
| Mandarin Understanding | 9.72 (0.80) | 9.63 (0.91) | 0.49 |
| English Understanding | 8.16 (1.39) | 7.86 (1.29) | 0.16 |
| Mandarin Reading | 9.79 (0.47) | 9.61 (0.99) | 0.16 |
| English Reading | 8.62 (1.08) | 8.25 (1.50) | 0.08 |
| Estimate | SE | df | t | p | |
|---|---|---|---|---|---|
| Perceived Negativity | |||||
| Language | −10.43 | 2.22 | 270.36 | −4.70 | <0.001 *** |
| Language:Medical_Event | −3.05 | 3.28 | 484.83 | −0.93 | 0.354 |
| Language:Relevance | −3.87 | 3.28 | 484.31 | −1.18 | 0.239 |
| Language:Population_Risk | −0.02 | 0.02 | 2819.19 | −0.93 | 0.354 |
| Lang:Med:Rel | 11.24 | 8.86 | 270.53 | 1.27 | 0.206 |
| Lang:Med:PopRisk | −0.02 | 0.04 | 2824.13 | −0.57 | 0.568 |
| Lang:Rel:PopRisk | 0.07 | 0.04 | 2824.02 | 1.52 | 0.128 |
| Lang:Med:Rel:PopRisk | −0.09 | 0.09 | 2819.49 | −1.02 | 0.309 |
| Perceived Risk | |||||
| Language | −2.14 | 2.55 | 266.66 | −0.84 | 0.403 |
| Language:Medical_Event | 1.7 | 3.82 | 454.25 | 0.45 | 0.656 |
| Language:Relevance | −2.74 | 3.82 | 453.83 | −0.72 | 0.474 |
| Language:Population_Risk | 0.05 | 0.02 | 2821.71 | 2.14 | 0.032 * |
| Lang:Med:Rel | 11.72 | 10.22 | 266.5 | 1.15 | 0.252 |
| Lang:Med:PopRisk | 0.01 | 0.05 | 2823.25 | 0.26 | 0.791 |
| Lang:Rel:PopRisk | 0.06 | 0.05 | 2823.38 | 1.13 | 0.257 |
| Lang:Med:Rel:PopRisk | 0.09 | 0.1 | 2821.55 | 0.91 | 0.365 |
| Estimate | SE | df | t | p | |
|---|---|---|---|---|---|
| Relative Negativity | |||||
| Intercept | 61.19 | 3.97 | 13.02 | 15.40 | <0.001 *** |
| Language | −2.73 | 2.99 | 44.47 | −0.91 | 0.366 |
| Relative Negativity | 0.35 | 0.03 | 1504.85 | 11.09 | <0.001 *** |
| Lang:Relative Negativity | 0.05 | 0.04 | 1277.62 | 1.16 | 0.248 |
| Relative Risk | |||||
| Intercept | 62.76 | 3.97 | 13.36 | 15.80 | <0.001 *** |
| Language | −0.59 | 3.02 | 46.11 | −0.20 | 0.846 |
| Relative Risk | 0.25 | 0.03 | 1558.80 | 9.04 | <0.001 *** |
| Lang:Relative Risk | 0.10 | 0.04 | 1524.98 | 2.46 | 0.014 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hayakawa, S.; Pan, Y.; Marian, V. Considering Preventative Care in a Native vs. Non-native Language: A Foreign Language Effect. Brain Sci. 2021, 11, 1309. https://doi.org/10.3390/brainsci11101309
Hayakawa S, Pan Y, Marian V. Considering Preventative Care in a Native vs. Non-native Language: A Foreign Language Effect. Brain Sciences. 2021; 11(10):1309. https://doi.org/10.3390/brainsci11101309
Chicago/Turabian StyleHayakawa, Sayuri, Yue Pan, and Viorica Marian. 2021. "Considering Preventative Care in a Native vs. Non-native Language: A Foreign Language Effect" Brain Sciences 11, no. 10: 1309. https://doi.org/10.3390/brainsci11101309
APA StyleHayakawa, S., Pan, Y., & Marian, V. (2021). Considering Preventative Care in a Native vs. Non-native Language: A Foreign Language Effect. Brain Sciences, 11(10), 1309. https://doi.org/10.3390/brainsci11101309






