Abstract
In 2015, the Belgian Health Ministers launched a plan intended to evolve towards an integrated care system for chronic patients. This plan is implemented through pilot projects involving local actors. Therefore, the researcher raised the following research question: how does the use of pilot projects as implementation instruments structure the collaboration between parties involved in a pilot project? The term “pilot project” refers to a collaborative work method coupled with an experimentation purpose. This is further developed in the paper via a literature study. This qualitative research draws on interviews, focus groups, direct observation, and a documentary analysis. During the two first phases of the process, field workers had to create multidisciplinary local consortia and write an application file describing the project they would implement during the third phase, which raised challenging collaboration issues. Many people learned to work together over time, progressively overcoming the traditional fragmentation of care. They met regularly, understood their respective roles, and dealt with controversies through negotiation to reach an agreement on a common project. In conclusion, the researcher shows that, thanks to its characteristics, the pilot project instrument supports the development of collaborative care networks; in this example of community-based integrated care networks.
1. Introduction
1.1. Background
For the last ten years, numerous pilot projects have been launched in the Belgian health sector, including “therapeutic projects” and “psy 107” projects in the mental health sector, multidisciplinary local networks for diabetics (type 2) and for patients with renal insufficiency, “protocol 3” projects for frail old people, and also, more recently, integrated care pilot projects for chronic patients. The latter were initiated as part of the “Integrated Care for Better Health” plan targeting chronic patients, which was approved on October 19, 2015. This plan was launched in reaction to the current fragmentation of care, which impedes the delivery of quality care to chronic patients, puts the health care system under budgetary pressure, and as a result, reduces the health care system’s efficiency [1,2].
The prevalence of chronic diseases is one of the major public health challenges worldwide [3]. In Belgium, 27.2% of the population are suffering from chronic disease(s) [4]. These are also the leading cause of mortality, being responsible for about 86% of deaths [5]. As in other European countries, from a financial perspective, their ever increasing prevalence [4,6] has resulted in a constant and important increase in Belgian health care expenditure [7] over the last 15 years [8], and the latter are expected to continue to rise if no action is taken.
Chronic patients often combine several diseases, which can make things even more complicated. In Belgium, more than one in three people over 65 suffer from at least two chronic diseases [9]. This coexistence of several chronic affections (two or more) is referred to as “multi-morbidity” [6]. Managing multi-morbidity over the long term requires the intervention of multiple care professionals and organisations (from first and second lines of care) and also of non-medical stakeholders [1]. It is now also a major challenge given that the “single disease approach”, leading to a high level of specialisation, has dominated medicine for centuries [6]. Chronic patients have indeed very specific and complex needs in terms of care [10,11], which require strong and effective coordination, cooperation and collaboration between practitioners [1].
The Belgian health care system is, nonetheless, characterised by a high degree of fragmentation and does not meet the needs of chronic patients. Admittedly, this fragmentation can be explained by the predominance of the single disease approach, but it is also a legacy of the historical ‘pillarisation’, which has characterised Belgium since its creation [12]. Actually, this country can be seen as a consociational democracy emanating from a society characterised by a sharp segmentation related to denominational communities, namely Catholics and non-Catholics [13], the latter encompassing liberals and socialists [12]. Historically, each of the three communities created “a wide range of organisations dealing with almost every aspect of daily life, i.e., a pillar” [13]. Among these organisations, one can find schools and universities, political parties, trade unions, youth organisations, and in the health sector, health care services, health insurance, and hospitals. The three pillars have each had their own path and have evolved independently in a context of parallel “segmental autonomy” [13]. They have avoided building bridges between each other, which explains the resulting societal fragmentation. “As consociations are composed of societies-in-a-society and systems-in-a-system, creating an integrated system is a major challenge” [13]. In Belgium, the ideological boundaries and tensions existing between the three pillars have underlined the functioning of the Belgian institutional edifice for decades [14]. Even if their influence is less important than before, they still have an influence on the way care is organised in Belgium and at the different levels of the Belgian health care system.
According to international scientific literature [1,4], an integrated care system would seem more appropriate to deal with the challenges posed by the current chronic disease epidemic [3,15]. Care integration can be defined as “the management and delivery of health services so that clients receive a continuum of preventive and curative services, according to their needs over time and across different levels of the health system” [16]. Accordingly, through their plan, the Belgian health ministers—Belgium is a federal state, which explains why there are several health ministers—advocated a transition towards such a collaborative system, drawing on the Triple Aim model principles, which have guided health system reforms in many countries [1]. The Triple Aim model combines these interdependent goals: “improving the individual experience of care, improving the health of populations, and reducing the per capita costs of care for populations” [17]. In other words, the purpose is to simultaneously improve quality, equity, and efficiency by moving from a competitive to a collaborative health care system [18].
Nevertheless, if there was an agreement on the general aim, i.e., achieving integrated care, the question of how it could concretely be done in the Belgian-specific context was more uncertain. This explains why the Belgian authorities decided to use pilot projects as implementation instruments. It was a way to involve field actors in an iterative and incremental co-creation process, giving them the opportunity to build their own project at a local level and to make propositions on the strength of their field experience, which should be more adapted to patients’ needs. Indeed, hands-on professionals have an experience-based knowledge of the Belgian health care system, anchored in their day-to-day practice, which the authorities do not have.
These new integrated care pilot projects are particular in the sense that they simultaneously target several diseases, encompass larger target groups than the previous pilot projects in health care (thousands of people per project), do not overlap geographically, and cover larger geographic areas. Above all, they involve many more different actors from the different pillars, from the different care lines, and from the different levels of the care production chain (macro, meso-, and micro levels) in a phased co-creation process, i.e., policy-makers, civil servants, patients’ representatives, first-line and second-line care actors (hospitals, medical health centres, general practitioners, nurses, etc.), together with non-medical actors (e.g., social and cultural actors). These actors, who would probably not have met otherwise (or, if so, not under the same terms), have different and often diverging interests, which raises major inter-pillar, inter-sectorial, inter-organisational, and inter-professional collaboration issues.
This expected major transformation of the Belgian health care system denotes the authorities “wish to achieve a paradigm shift [2,19], as they state it in the plan ‘Integrated Care for Better Health’”. A paradigm shift can be defined as a change “in the framework of ideas and standards” [19] shared and used by policymakers to define policy goals, instruments, and the problems to be addressed, as well as regulatory mechanisms [19]. In this paper, the researcher focuses on the change of instruments, i.e., the use of pilot projects, instead of passing a law as the authorities did before. In an original manner, she focuses on the instrument “pilot project” as an action mode [20]. She addresses it as an object for research and raises the following research question: how does the use of pilot projects as implementation instruments structure the collaboration between parties involved in a pilot project? To answer this question, she has focused on two pilot projects launched as part of the Belgian plan “Integrated Care for Better Health”. In this paper, the researcher intends to understand how the pilot project approach structures the interactions and the relationships between the numerous pilot project stakeholders who have to learn how to work together, cooperate, and collaborate to achieve integrated care in Belgium. In other words, the analysis deals not only with the need to re-invent health care, but also with the evolution in the means selected to re-invent health care systems.
Her contribution also resides in the fact that she analysed her data by combining elements from three theoretical frameworks:
- -
- The framework of project management stated by Segrestin pertaining to the sociology of organisations;
- -
- The framework of public policy instruments of Lascoumes and Le Galès belonging to the sociology of public action—this framework has already been used to analyse the specific case of an urban project, but not yet to analyse pilot projects in the health sector;
- -
- The framework of sociology of translation by mobilising the work of several authors—Callon, Latour, Akrich, Monaghan, and Freeman.
The next section consists of a literature review regarding the “pilot project” as an object for research.
1.2. Pilot Project: Two Words for One Single Public Policy Instrument
The project-based approach is a work method used in many different sectors. Vreugdenhil and Ker Rault [21] see pilot projects as a “means to establish communication between actors that usually do not cooperate”. In this way, due to their dynamic nature, they help trigger collaboration [22].
The project approach “applies to complex and tailor-made actions” [23] and is supposed to help go beyond traditional solutions when innovation is needed to meet singular and specific needs [23,24]. Based on the idea of “creative cooperation” [23], “the project logic is the one which consists of mandating a team, the project team, to complete successfully the conception of the adequate solution to a mission” [23]. Breaking down the traditional hierarchies, this team often gathers professionals of various origins who have to cooperate in an uncertain context of continual negotiation and imperative exchange of ideas, which can be the source of important new uncertainties [20]. Indeed, “exchanging points of view not only entails admitting once and for all that no one owns the good solution, but also that a collective task cannot come down to the addition of individual or local contributions—it is the exchange by itself which is the source of knowledge, contributing to making creation unpredictable” [23]. The pilot project constitutes, therefore, a social mobilisation instrument characterised by an interactionist and processual rationale, taking what already exists as a starting point for reflection and action [20].
Another characteristic trait of the project approach is that the aims it sets out to achieve are strictly defined, while the participants are free to achieve them in the way they choose, often with limited resources. As a result, a project group always has to handle the challenge of combining and finding a balance between exploration of new possibilities and exploitation of old certainties [25]. This means that “whatever its mission, it will have to create, invent, and also deal with constraints of efficiency” [23], sometimes forcing them to avoid risks linked to the exploration of new possibilities and leading them to resort to more familiar and predictable solutions.
In addition, behind the word ‘pilot’ hides the idea of experimentation, of being (one of) the first trying to achieve a particular task. In a variety of sectors, pilot projects, viewed as collective experiments [22], are often used in innovative contexts to develop and test new solutions, methods, concepts or practices [26,27]. They constitute “common means by which innovations (…) are applied and adapted (or even translated, one might say [28,29]), to real-world situations” [26]. As such, the innovative actions undertaken at the pilot project level are reversible. Indeed, pilot projects “configure a space to introduce and test innovations with smaller risks, either on smaller geographical scales or in short times” [22]. In this way, they “perform as platforms for learning” [26], which leads to knowledge development [21,22]. Consequently, they are also used by policy-makers to produce evidence for policy-making [21].
Eventually, this instrument is often used collectively to initiate and pilot innovation by putting into perspective, on the one hand, the existing local resources on a specific territory, and on the other hand, the public action objective(s). It is expected to induce a better understanding of local issues and a better appropriation of the policy objectives by the mobilised actors [20].
In conclusion, the pilot project is an instrument that has the potential to gather people with very different backgrounds and make them collaborate, even if it is unusual for them. Beyond the fact that it can trigger collaboration, the pilot project also brings about new challenges and structures collaboration in a certain way. This is precisely what the researcher analyses in the case of integrated care pilot projects in light of the literature regarding pilot projects.
2. Materials and Methods
This sociological qualitative and inductive [30] research began in December 2016 during the conceptualisation phase (see below) and it draws on several data collection methods. The data were collected during the 14-month conceptualisation phase, i.e., the application writing period, as well as at the beginning of the execution phase, which started in January 2018 (see below). Inspired by the triangulation approach [31], the three types of information sources listed below were combined:
- Written documents through a literature study (scientific literature) and a documentary analysis (political, legal, and operational documents);
- Actions and interactions through direct observation (attendance at 67 meetings—148 h in total): 100 h were spent attending and observing meetings (preparatory meetings during the conceptualisation phase, follow up meetings during the execution phase, etc.) of two pilot projects (35 h for the first project and 70 h for the second one). The researcher also attended plenary sessions and intervisions organised by the public authorities (43 h) to observe what was happening through interactions and to observe innovation in action;
- Discourses: the researcher conducted 24 semi-structured interviews, lasting between 33 and 98 min, with different categories of actors—policy-advisers and public officials involved in devising and implementing the new policy, pilot project coordinators, and pilot project stakeholders. Furthermore, this research relies on data collected via seven focus groups (n = 7–16, 5 h) on the topic of governance, the purpose of which was to determine the governance modalities of three projects (the two mentioned above and a third additional project).
3. Results
3.1. Launching Integrated Care Pilot Projects: A Phased Process
In January 2016, the publication of the guidance leaflet for future integrated care pilot projects by the Belgian authorities marked the beginning of the implementation of the plan, “Integrated care for better health”. This leaflet contained the specific modalities and guidelines pertaining to the process. As already explained above, it has been divided into four main phases [2]:
- The preparation phase and the conceptualisation phase, which are the two phases of the selection procedure, during which field actors designed their projects together;
- The execution phase, which began in January 2018, which should last for four years, and during which the twelve out of the fourteen selected pilot projects (two pilot projects gave up) are expected to implement their “loco-regional action plan” (see below);
- The expansion phase, which will occur after the four-year execution phase, during which the successful pilot projects will have to evolve to cover the entire Belgian population.
In this paper, the researcher focuses mainly on the two first phases, the preparation and the conceptualisation phase:
- The preparation phase (first phase of the selection procedure): in February 2016, the authorities launched a call for expressions of interest, which marked the beginning of the four-month preparation phase. Field actors who were interested in creating a pilot project had to constitute multidisciplinary local consortia. By doing so, the political will was to gather a variety of people working with chronic patients so that each consortium properly reflected the care offer of the geographical zone covered by its project. Stakeholders had to submit a joint expression of interest approximately defining their target groups, as well as the geographic area covered by their projects, by May 31, 2016. This expression of interest had to be signed by all of the partners who had joined the pilot project consortium.
- The conceptualisation phase (second phase of the selection procedure): between July 2016 and September 2017, each of the twenty selected pilot project consortia had to write a more detailed application file containing a loco-regional action plan. In this plan, pilot project stakeholders had to describe their common vision, their strategic and operational objectives, as well as the actions they would implement to achieve their objectives if they were selected for the four-year execution stage. These had to be based on an analysis of local needs, of available and missing resources in the pilot zone, as well as a risk stratification pertaining to their respective populations.
The application file also had to include:
- a financial plan;
- a communication plan;
- a time line taking the form of a Gantt Chart;
- the description of their future governance structure and legal personality;
- a description of how responsibilities would be distributed among partners during the execution phase [2].
From this phase, each consortium had to appoint a local coordinator, working at least part-time for the project and whose role is described below. In order to achieve these tasks, the coordinators and their consortia members were assisted by external coaches hired by the authorities. The coaches had, inter alia, the mission to provide the coordinators with methodological assistance regarding the analysis of the existing situation in their pilot zones and the conception of the loco-regional action plan [2]. Therefore, at the beginning of the conceptualisation phase, the coaches suggested a non-mandatory governance structure for the pilot projects specific to this phase, which is represented in the organisation chart below (Figure 1):
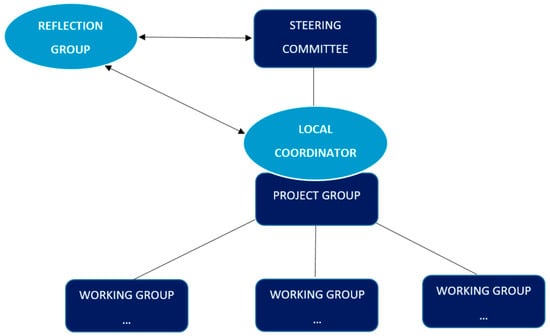
Figure 1.
Pilot projects’ governance structure.
Each type of group gathered specific partners and had its own meeting frequency. The reflection group referred to the entire consortium and gathered all the pilot project partners. This group had to meet at least once during the conceptualisation phase on the initiative of the local coordinator. It had a reflective role on the basis of the proposals received from the project group. The latter was a smaller group, gathering between four and seven key partners, who were expected to meet at least eight times during this phase (around once a month). Its role was to make proposals and to detect problems, among other tasks. The steering committee was larger than the project group and gathered the most concerned people of the consortium. They were supposed to meet four times. Their role was to validate the proposals and documents. Working groups were small groups that gathered experts in their respective fields. Set up to meet specific needs, these ad hoc groups had to develop some ideas further by mobilising their expertise. Finally, the local coordinator was the contact person between all of these stakeholders. They were also the single point of contact for the coach and the authorities, and in charge of organising the meetings for each group (invitation, chairmanship, writing meeting minutes, follow-up, etc.) and of writing the application file. Eventually, the local coordinator was responsible for practical aspects, such as managing the budget, distributing attendance fees, among other tasks.
The structure set out in Figure 1 and the meeting frequencies related to each group were no mere coincidence, as illustrated in this interview extract: “We created a kind of reverse planning model that we gave to the coordinators saying ‘according to us, from this day, here are the steps to perform and the chronology that we have imagined’. So we suggested an entire governance structure including a reflection group and a project group” (Interview with a coach, 2017). The rationale behind this was that according to the coaches, a certain number of meetings were required for each group to be able to submit the application file on time. Interestingly, it appeared that this was not enough, and that pilot project members set up additional meetings.
3.2. Financial Aspects
During the conceptualisation phase, a lump sum funding of 40,000 euros, payable in two instalments, was provided to pay the part-time coordinator’s salary. This was the only funding that the consortia received during this phase. Since the beginning of the execution phase, each consortium has had to appoint a full-time coordinator to lead the execution process (not mandatorily the same person who coordinated the project during the conceptualisation phase).
Another question of importance is how these pilot projects are expected to be financed during the execution phase. It was planned that each year, pilot project consortia would be paid a lump sum fund of exactly 150,000 euros. It is explicitly written in the guidance leaflet that this amount of money is intended to finance the coordinator’s salary, as well as the management costs (administrative expenses, attendance fees, etc.), and to hire additional staff, if needed. In other words, this budget is not supposed to finance the pilot projects’ actions in the domain of health care provision for the patient.
Through the joint plan, the authorities are following the Triple Aim principles, which specifically entail reallocating the available financial means more effectively, while preserving or even enhancing equity and quality of care. To that end, pilot projects, due to their actions, would have to reduce health care expenditure in their pilot zone, which would affect the Belgian health care budget by generating savings at the national level. In return, in addition to the lump sum funding of 150,000 euros, each pilot project will receive, at the end of each year, a budgetary envelope corresponding to the savings they will have helped to generate in their pilot zone. This sum, called the “budgetary guarantee”, would be redistributed to them each year so that they could implement new actions, generate new savings, and so forth. As a result, given the scarcity of financial resources, the stakeholders took part in meetings voluntarily, without being paid.
3.3. Building Integrated Care Pilot Projects
When co-designing integrated care pilot projects at the local level, coordination, cooperation and multidisciplinary collaboration are some of the key components of integrated care [32,33]. Triggering a collaborative culture between the different actors of the care production chain has been precisely one of the major innovations at stake in the plan, given the level of fragmentation in the Belgian health care system. As a result, in a context in which health care professionals do not collaborate spontaneously, the first step was to make them meet, communicate, and be aware of the existence of each other, as well as of their respective roles in the care production chain. This process was initiated during the preparation and conceptualisation phases.
The authorities’ guidelines were listed in the guidance leaflet published in January 2016, in which they set up the framework for action in a top-down manner. In this document, the authorities describe the integrated care framework and determine the general and inescapable objective they want to attain—achieving integrated care in Belgium with limited resources, given the current context of budgetary pressures. On the basis of these guidelines, pilot project stakeholders were invited to think outside of the box and collectively imagine new ways of working, while mobilising what already exists in terms of resources. As proof of this, here is what a public official said to pilot project members during an intervision: “We do not ask you to do better with less, but to do better with what already exists” (Field notes of observation, 2017). In this context, pilot project members were given the freedom to make bottom-up innovative and creative proposals anchored in the reality of their day-to-day experience of care (as professionals, patients, etc.), as illustrated by this interview extract: “In my opinion, and we often repeat it: we do not have all the answers. […] Consequently, it is important for us to have a co-creation process as we often repeat it, that field actors involve themselves, create and make propositions” (Interview with a high-ranking official, 2017).
During the preparation phase, the interested people had to gather in multidisciplinary local consortia, or in other words, to constitute their project teams and design together the first elements of a common project. They were put in a situation in which they had to identify the other relevant actors present in their territory, and with whom they would collaborate to imagine new ways of organising and delivering care for chronic patients at the local level on a delimited territory.
According to one pilot project stakeholder, “It is the first time that we have had so many different actors around the table” (A pilot project stakeholder, Field notes of observation, 2018). Indeed, pilot project consortia are very heterogeneous. Interestingly, their composition blurs the explicit or implicit routine hierarchical reports, which sometimes initiates a redistribution of the roles between the participants. They actually gather, on a voluntarily basis, a variety of stakeholders who do not usually collaborate directly, but who each have a role to play in the care trajectories of the types of chronic patients included in the target population. One can mention general practitioners, nurses, pharmacists, physiotherapists, occupational therapists, specialist doctors, hospitals (directors and managers of specific departments who function within the pilot project target population), social workers, home help- and care partners, home care coordination centres, patients’ associations, as well as associations of their relatives, health care insurance companies, called health care mutuals in Belgium, social aid and social welfare actors, such as public centres for social help, day care centres, and rest homes, along with other non-medical partners, such as the cultural, employment, agricultural, and environmental sector representatives.
Another very unusual thing is that institutions historically related to the three different pillars are simultaneously represented in several consortia, as stated in this interview extract:
“The divisions are different [in the integrated care projects]. In x [name of the project], you can find public and private providers, you have everything. Why would it be this federation instead of this one that would [take the lead]? The conflict resides [in] this pillar logic, i.e., this logic of ideological and confessional division, which has structured the Belgian society since the outset. We would try to evolve towards something more rational in the 21st century, which is not only based on political convictions or beliefs. […] We would try to evolve towards something more rational”(Interview with a pilot project member, 2018).
Actually, one might have imagined that having intra-pillar pilot projects, i.e., different pilot projects, each gathering professionals from one specific pillar, would have possibly facilitated the implementation process, leading to the development of intra-pillar collaborations and intra-pillar care integration. It would also have contributed to reproducing the societal segmentation characterizing the Belgian consociational democracy [13], but it would probably have led to new redundancies in terms of offers of care. Instead, following the authorities’ instructions, consortia are expected to develop territorialised actions and involve the most relevant partners possible, whatever the pillar they are related to. By operating in this way, one of the purposes is notably to reduce, or even eliminate, useless duplications in the care system, which lead to a lack of efficiency.
During the conceptualisation phase, getting to know each other was admittedly a time-consuming, but also an essential, step for all the aforementioned local people who participated voluntarily to build a multidisciplinary pilot project. “If the project is not selected, we will at least have got to know each other. It is not wasted—things have already changed [in terms of collaboration and integration]” (A pilot project stakeholder, Field notes of observation, 2018). This aspect is clearly stated as a positive consequence of being involved in the project given that, so far, a lot of stakeholders used to work in silos.
Drawing on the governance structure mentioned above, the people involved in the selected pre-projects met regularly to brainstorm, discuss, and articulate objectives in order to write collaboratively their loco-regional action plan, as well as the other elements of their application file. They had to reach an agreement on their common vision and goals, and their strategic and operational objectives, as well as the future actions they would implement. This was a challenging task given the diversity of the assembled stakeholders’ profiles. Numerous points of view were indeed represented, which made things even more complex, e.g., a hospital director will not have the same vison of care as a general practitioner or a home care worker. Each partner had their own practice-based knowledge, their own personal interests, and their own opinions to express, which sometimes created important controversies [28] and led to hard and long negotiations. These controversies concerned various matters, e.g., the name chosen for the project, the way financing resources would be allocated, the governance modalities and the project’s potential legal structure, patients’ data protection, the concrete actions that should be launched to achieve integrated care, the selection of priority targets and actions, etc. (this list is far from exhaustive). Pilot project members even felt the need to organise additional meetings with respect to what was planned in the beginning of the process to deal with all the matters aforementioned. As a result, the conceptualisation phase lasted thirteen months instead of seven.
3.4. Empirical Example: Choosing a Governance Structure and Legal Personality for the Future Execution Phase
As a reminder, during the conceptualisation phase, pilot project consortia had to decide which governance structure they would adopt. Each pilot project had also to identify a structure with a legal personality to receive their funding—an existing one (e.g., a partner organisation), or a new one to be created specifically for the project. After having decided this point, the partners had to either decide which organisation would be mandated to receive the funding (in the first case) or to choose the legal personality they would adopt during the execution phase (in the second case). Several scenarios could be considered. Regarding the governance structure, they could create (or not) a new independent structure and choose between several configurations, e.g., a de facto association, a non-profit making organisation, called an ASBL in Belgium (Association Sans But Lucratif in French, which means not-for profit association in English), which is an often-used specific kind of legal personality, or even innovate and imagine new configurations. In this regard, three coordinators wished to consult their stakeholders and organise focus groups to discuss that matter. Concretely, two sessions of focus groups were organised:
- -
- A session for a first project, during which the participants were divided into three focus groups gathering ten to fifteen people and lasting three hours each;
- -
- A joint session for two projects, during which the participants were divided into four focus groups gathering ten to fifteen people and lasting two and a half hours each: these two projects had common stakeholders and considered the possibility of pooling resources, which explains why it was decided to organise a joint session.
In each focus group, every participant had the opportunity to express their opinion regarding the matter at stake. Again, in each focus group, a specific and similar controversy emerged—some participants wanted to create a new “ASBL” for the project and others did not, preferring to keep the governance structure used during the conceptualisation phase. The participants talked about the pros and cons pertaining to each scenario. “We should not put the structure before the horse”, said a participant (Focus group extract, 2017). This illustrates the vision of some partners, according to whom building an ASBL without knowing if the project could be fruitful would be too premature and cumbersome. Indeed, creating an ASBL involves a lot of time-consuming administrative procedures. Others claimed there was a need to create a new and autonomous structure, such as an ASBL, considering that this would be a guarantee of transparency and neutrality regarding the management of the project. Also, many participants stressed that they did not have the proper legal expertise to select the adequate legal structure. “There are probably other solutions that we do not know” (Focus group extract, 2017). Accordingly, it was difficult for them to explore new possibilities and select innovative solutions, which brought them back to exploiting old certainties. In almost each focus group, the majority opted for creating an ASBL, the legal structure they knew best. Surprisingly, the first project members, after having discussed and negotiated the matter again during additional meetings, opted for a de facto association. They designated an organisation member of the project to be the legal mandated person to receive and manage the funding. As for the two other projects, they also set up additional meetings for further discussions and negotiations to agree finally on creating two independent ASBLs.
4. Discussion
4.1. The Case of Integrated Care Pilot Projects: Emerging Collaborative Networks
During the numerous meetings the researcher attended, the diversity of the participants’ profiles often resulted in a melting pot of opinions [23]. In an uncertain and sometimes uncomfortable [23] climate of perpetual negotiation, the partners dealt with controversies [28] by exchanging ideas. Progressively, the stakeholders overcame their personal interests through successive mutual adjustments [20,23] and inter-professional mutual learning [1,25]. They interacted face-to-face with each other on a regular basis [23] and took the time to grasp their respective roles, “to tame each other” (A pilot project stakeholder, Field notes of observation, 2018). They identified the assets already present in their consortia and in their geographical area. Step by step, the stakeholders collectively built their project, articulated the reason for its existence, as well as their common philosophy, and defined or adjusted their own individual role in this complex system [34]. By doing so, the stakeholders stabilised a common identity [20] and a “common language”, which crystallised the compromise achieved through successive iterations [35]. In this way, they made their relationship intelligible, and they united “universes (that) were separate and had no means of communication with one another” [28]. It is in this sense that the pilot project is a social mobilisation instrument—using it as an implementation instrument leads to “the implication of the actors of the concerned territory and the valorisation of the resources harboured on this territory” [20].
This way of working led progressively to the emergence of the early stages of a new culture of horizontal collaboration between pilot project members. Indeed, during the preparation and the conceptualisation phases, numerous different people, who might not have otherwise met, came to work together and learned from each other [25]. They made different worlds communicate [23] and began to alleviate the traditional fragmentation between first- and second-lines of care. The project approach ignores frontiers [23] between professions, hierarchic levels, or sometimes even between structures. By also including non-medical stakeholders, the pilot project consortia even extended to the community, the involvement of which is crucial for the development of integrated care according to the scientific literature [1]. In this way, they began the development of what could become (and what the researcher would call) collaborative community health networks or collaborative community health microcosms in the future. As proof of this, the elements shown in Figure 2 below characterise both integrated care pilot projects and community health care [36].
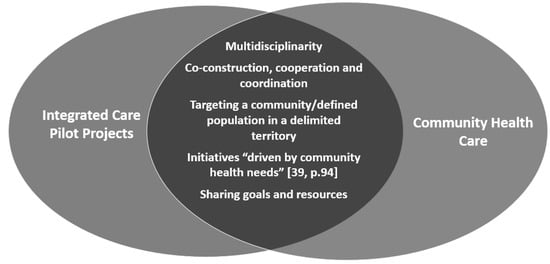
Figure 2.
Community health characteristics.
Accordingly, as an answer to her guiding question, the researcher argues that the pilot project appears to be an instrument of the interactionist and processual rationales that support the development of a specific form of organisation, i.e., collaborative networks [34,37], in this specific case of community-based integrated care networks [38]. As a result, “the project has not only the purpose of designing and implementing [political] objectives (…), it has also the vocation of asserting action identities, stabilising groups of actors united by the sharing of the same objectives” [20]. In this way, it creates conditions over the interactions that are conducive to the emergence of a system, i.e., an autonomous collective actor fitted with a collective and cohesive action capacity [20]. In the three projects which the researcher has focused on, these collective actors, i.e., the nascent networks, take the form of a de facto association in one case and of two independent “ASBLs” in the other case. Each of these three entities has a real autonomous existence, a name, and specific governance modalities decided by the project members themselves.
4.2. Collaboration as a Means, Collaboration as an End to Integrating Care
In this endeavour of implementing integrated care in Belgium, collaboration appears to be both a means and an end—a means to exchange ideas, learn from each other, and imagine collectively how to implement integrated care in Belgium, and an end as a major component of integrated care. More specifically, the researcher argues that the transition into practice during the execution phase does not involve the same collaboration modalities as during the preparation and the conceptualisation phases. Indeed, as Segrestin puts it, “a project is divided into distinct phases, and each phase requires different forms of action, cooperation, and technical formalisation” [23].
During these two first phases, the researcher argues that the partners entered a process of creative “cogitating collaboration”, resulting in the production of discourses that pertained to “what should be done” on the ground during the next phase. It took the form of face-to-face deliberative interactions during meetings; stakeholders brainstormed on the basis of their respective knowledge of the field, explored hypotheses, and finally made decisions after having reached consensus regarding their common purposes [23,34]. They formalised the results of their discussions in their loco-regional action plan, which can be viewed as an artefact of their collegial appropriation of the integrated care policy initiated by the authorities. Cogitating collaboration (see empirical example at point 3.4), inherent in the project approach, was necessary to the network emergence. It was the way through which the partners built their common project, crystallising the network’s reason for existence, and planned the innovative actions they intended to achieve in real-world situations during the execution phase.
The collaboration, viewed as an end in itself, refers to the “operational collaboration” on the ground to deliver quality care, which is one of the core elements of integrated care, and as a result, one of the aims pursued. It requires moving from discourse to practice, from the collective designing process to the collective experiment on the ground, and from the “what are we going to do?” to the “let’s try it”. Even if the cogitating collaboration seems to be a prerequisite to develop operational collaboration on the ground, the latter is not necessarily its corollary. As a result, translating the “loco-regional action plan” into practice constitutes a central issue at this stage of the process and should not be taken for granted. Nevertheless, a lesson that can be learned from this case study is that “the process and the elaboration method are as important as the plan (…) to which they lead” [20]. In other words, the modus operandi is as important as the desired outcome [20].
5. Conclusions
In this paper, the researcher has focused on the use of pilot projects and analysed how they specifically structure collaborative work in the Belgian health sector. Thanks to this case study, she has shown that “the project serves both to constitute sustainable systems of actors, as well as to build and implement decisions” [20]. The researcher has stressed that pilot projects are instruments that create the conditions enabling the emergence of care networks, and more specifically, of what she calls community-based integrated care networks. In this way, she links a specific type of instrument, i.e., the pilot project, to a specific form of organisation, i.e., the network. One should be careful, though, not to consider this link as a systematic cause and effect relationship. Using pilot projects will probably not always lead to the emergence of networks; this depends on the context in which they are used and on the way they are used.
This study has also shown that becoming a group, a cohesive community, or a network that is aware of its existence, is a task in itself, a time-consuming one not to be neglected, and a first step before collaborating on the ground. Indeed, enhancing quality of care is more than collaboratively achieving a task in the field. It requires, first of all, taming each other in order to develop inter-professional mutual learning, so as to define and agree on what has to be done together, and on the role of each other in this endeavour [34]. The preparation and conceptualisation phases were dedicated to this process of defining the pilot projects’ essence and designing what should be done in the field, which took more time than expected.
The partners of the selected pilot project were able to work together in their respective consortium to build a project and plan actions to meet the objectives they jointly defined during the preparation and the conceptualisation phases. At this stage, two important questions can be raised. First, will they be able to move into practice and concretely implement their loco-regional action plans during the execution phase? In other words, will they be able to entrench their nascent integrated care networks and collaborate on the ground in a therapeutic context to experiment collectively with the innovative actions they imagined together? This translation into practice will surely raise unexpected questions of practical feasibility, which the partners did not anticipate before, and which will probably require adjustments [23] or possibly new explorations [29]. Second, will the pilot project members be able to elicit the interest and the involvement of the field actors who did not participate in the preparation and conceptualisation phases? Behind this question hides the issue of enrolling hands-on professionals who work in the pilot zone and whose role is relevant to, or even sometimes crucial for, the implementation and the survival of the project during its operationalisation.
Funding
This research was funded by the IKARE foundation and the University of Liège.
Conflicts of Interest
The author declares no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
References
- Amelung, V.; Stein, V.; Goodwin, N.; Balicer, R.; Nolte, E.; Suter, E. (Eds.) Handbook Integrated Care; Springer International Publishing: Cham, Switzerland, 2017; Available online: http://link.springer.com/10.1007/978-3-319-56103-5 (accessed on 19 September 2018).
- Belgian Ministry of Social Affairs and Public Health. Plan Conjoint en Faveur des Malades Chroniques: «Des Soins Intégrés Pour Une Meilleure Santé». 2015. Available online: http://www.integreo.be/sites/default/files/public/content/plan_fr.pdf (accessed on 4 December 2018).
- Riley, L.; Gouda, H.; Cowan, M. Noncommunicable Diseases Progress Monitor; World Health Organization: Geneva, Switzerland, 2017; Available online: http://apps.who.int/iris/bitstream/10665/258940/1/9789241513029-eng.pdf (accessed on 12 September 2018).
- Paulus, D.; Van den heede, K.; Mertens, R. Organisation Des Soins Pour Les Malades Chroniques en Belgique: Développement d’un Position Paper (Report No. 190B); Centre Fédéral d’Expertise des Soins de Santé (KCE)-Health Services Research (HSR): Bruxelles, Belgium, 2012; Available online: https://kce.fgov.be/sites/default/files/page_documents/KCE_190B_organisation_soin_malades_chroniques_0.pdf (accessed on 16 January 2017).
- World Health Organization. Noncommunicable Diseases (NCD) Country Profiles—Belgium; World Health Organization: Geneva, Switzerland, 2018; Available online: http://www.who.int/nmh/countries/2018/bel_en.pdf?ua=1 (accessed on 4 February 2019).
- Ording, A.; Sørensen, H. Concepts of comorbidities, multiple morbidities, complications, and their clinical epidemiologic analogs. Clin. Epidemiol. 2013, 5, 199–203. [Google Scholar] [CrossRef] [PubMed]
- Schokkaert, E.; Van de Voorde, C. Belgium’s Healthcare System. Should the Communities/Regions Take It Over? Or the Sickness Funds? 2011. Available online: http://www.rethinkingbelgium.eu/rebel-initiative-ebooks/ebook-10-belgium-healthcare-system-communities-regions-take-over-sickness-funds (accessed on 6 February 2017).
- OECD.stat. Health Expenditure and Financing. 2017. Available online: https://stats.oecd.org/viewhtml.aspx?datasetcode=SHA&lang=en (accessed on 14 August 2018).
- Van der Heyden, J.; Charafeddine, R. Enquête de Santé 2013. Rapport 1: Santé et Bien- Être. Résumé Des Principaux Résultats D/2014/2505/53—Référence Interne: PHS Report 2014-031. 2014. Available online: https://his.wiv-isp.be/fr/Documents%20partages/summ_HS_FR_2013.pdf (accessed on 20 August 2018).
- Baszanger, I. Les maladies chroniques et leur ordre négocié. Revue Française de Sociologie 1986, 27, 3–27. [Google Scholar] [CrossRef]
- Czernichow, P. Un système de santé plus intégré pour mieux prendre en charge les maladies chroniques. Santé Publique 2015, 1, 7–8. [Google Scholar] [CrossRef] [PubMed]
- Thunus, S. The system for addressing personal problems. In From Medicalisation to Socialisation: Shifts in Belgian Mental Health and Psychiatric Institutions; Université de Liège: Liège, Belgium, 2015. [Google Scholar]
- Mangez, E. Global Knowledge-based Policy in Fragmented Societies: The case of curriculum reform in French-speaking Belgium: European Journal of Education, Part, I. Eur. J. Educ. 2010, 45, 60–73. [Google Scholar] [CrossRef]
- De Troyer, M.; Krzeslo, E. Assurance maladie, soins de santé et sécurité sociale: Trois éléments indissociables. Chronique Internationale de l’IRES 2004, 91, 113–122. [Google Scholar]
- WHO. Global Status Report on Noncommunicable Diseases 2014: Attaining the Nine Global Noncommunicable Diseases Targets; a Shared Responsibility; World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- WHO. Integrated Health Services—What and Why? Technical Brief No.1.2008; World Health Organization: Geneva, Switzerland, 2008; Available online: http://www.who.int/healthsystems/service_delivery_techbrief1.pdf (accessed on 23 January 2017).
- Berwick, D.M.; Nolan, T.W.; Whittington, J. The Triple Aim: Care, Health, and Cost. Health Aff. 2008, 27, 759–769. [Google Scholar] [CrossRef]
- Buttard, A.; Santos, C.D.; Tizio, S. Networking Healthcare. From a competitive call to a medical cooperation as a guarantee of a found confidence. Recherches en Sciences de Gestion 2012, 6, 21–43. [Google Scholar] [CrossRef]
- Hall, P.A. Policy Paradigms, Social Learning, and the State: The Case of Economic Policymaking in Britain. Comp. Polit. 1993, 25, 275–296. [Google Scholar] [CrossRef]
- Lascoumes, P.; Le Galès, P. (Eds.) Gouverner par les Instruments; Presses de la Fondation Nationale des Sciences Politiques: Paris, France, 2004; 370p. [Google Scholar]
- Vreugdenhil, H.; Ker Rault, P. Pilot Projects for Evidence-Based Policy-Making: Three Pilot Projects in the Rhine Basin. In German Policy Studies; EBSCO Industries, Inc.: Birmingham, AL, USA, 2010; pp. 115–151. [Google Scholar]
- Zurlo, F.; dos Nunes, V.G.A. Designing Pilot Projects as Boundary Objects; Springer International Publishing: Cham, Switzerland, 2016; Available online: http://link.springer.com/10.1007/978-3-319-23141-9 (accessed on 14 December 2017).
- Segrestin, D. Les Chantiers du Manager; Colin: Paris, France, 2004; 343p. [Google Scholar]
- Dumoulin, P.; Dumont, R.; Bross, N.; Masclet, G. Travailler en Réseau: Méthodes et Pratiques en Intervention Sociale; Dunod: Paris, France, 2015. [Google Scholar]
- March, J.G. Exploration and Exploitation in Organizational Learning. Organ. Sci. 1991, 2, 71–87. [Google Scholar] [CrossRef]
- Engström, S.; Lidelöw, S. From the Pilot Project to the Mainstream Practice—Learning Explored in Planning and Design of a Low-Energy Quarter. Procedia Econ. Financ. 2015, 21, 288–296. [Google Scholar] [CrossRef]
- Vreugdenhil, H.; Taljaard, S.; Slinger, J.H. Pilot projects and their diffusion: A case study of integrated coastal management in South Africa. Int. J. Sustain. Dev. 2012, 15, 148–172. [Google Scholar] [CrossRef]
- Callon, M. Some Elements of a Sociology of Translation: Domestication of the Scallops and the Fishermen of St Brieuc Bay. Sociol. Rev. 1984, 32 (Suppl. 1), 196–233. [Google Scholar] [CrossRef]
- Freeman, R. What is ‘translation’? Evid. Policy 2009, 5, 429–447. [Google Scholar] [CrossRef]
- Musselin, C. Sociologie de l’action organisée et analyse des politiques publiques: Deux approches pour un même objet? Revue Française de Science Politique 2005, 55, 51. [Google Scholar] [CrossRef]
- Jick, T.D. Mixing Qualitative and Quantitative Methods: Triangulation in Action. Adm. Sci. Q. 1979, 24, 602–611. [Google Scholar] [CrossRef]
- Contandriopoulos, A.-P.; Denis, J.-L.; Touati, N.; Rodriguez, R. Intégration de soins: Dimensions et mise en oeuvre. Ruptures Revue Transdisciplinaire en Santé 2001, 8, 38–52. [Google Scholar]
- WHO. Integrated Care Models: An Overview. 2016. Available online: http://www.euro.who.int/__data/assets/pdf_file/0005/322475/Integrated-care-models-overview.pdf (accessed on 13 March 2017).
- Schweyer, F.-X.; Levasseur, G.; Pawlikowska, T. Créer et Piloter un Réseau de Santé: Un Outil de Travail Pour Les Équipes; de L’ecole Nationale de la Santé Publique: Rennes, France, 2002.
- Akrich, M.; Callon, M.; Latour, B.; Monaghan, A. The key to success in innovation part II: The art of choosing good spokespersons. Int. J. Innov. Manag. 2002, 6, 207–225. [Google Scholar] [CrossRef]
- Prévot, M. L’approche Communautaire: Un Liant Interdisciplinaire? Santé Conjuguée. 2016. Available online: File:///C:/Users/M%C3%A9lanie/Downloads/sc74_def_prevost_approche_com.pdf (accessed on 12 September 2017).
- Powell, W. Neither Market nor Hierarchy; Network Forms of Organization. In Research in Organizational Behavior; Staw, B.M., Cummings, L.L., Eds.; JAI Press: Greenwich, UK, 1990; pp. 295–336. [Google Scholar]
- Plochg, T.; Klazinga, N.S. Community-based integrated care: Myth or must? Int. J. Qual. Health Care 2002, 14, 91–101. [Google Scholar] [CrossRef] [PubMed]
© 2019 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).