Addressing Adverse Childhood Experiences: It’s All about Relationships
Abstract
1. Introduction
2. Adversity through a Global Population Health Lens
3. Adversity through the Lens of Global Hunger and Poverty
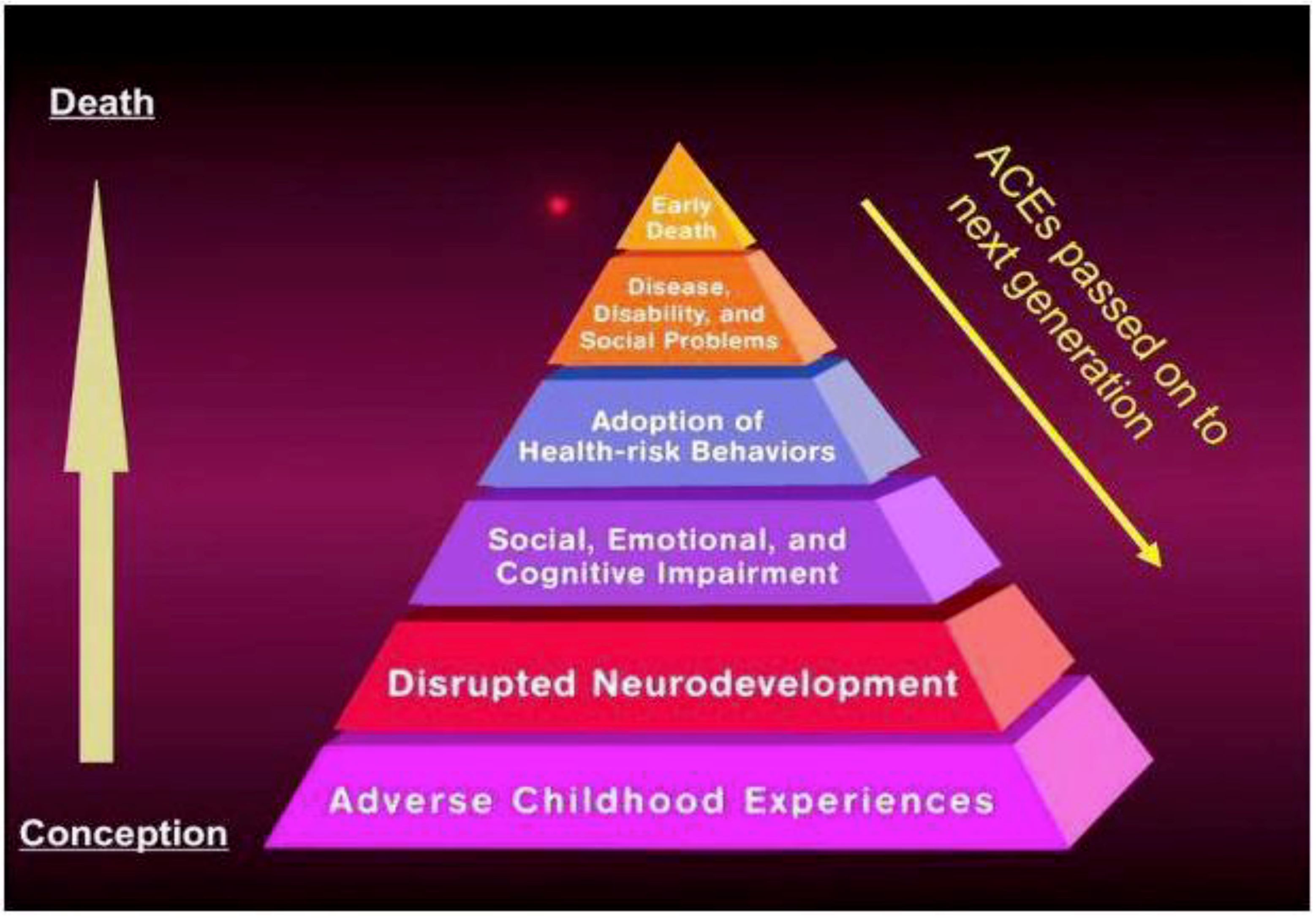
4. What Are Adverse Childhood Experiences (ACEs) and Why Do They Matter?
5. How Does Adversity Affect Short and Long-Term Health?
5.1. Early Brain Development
5.2. Stress Response System
5.3. Gene x Environment Experiences
6. Mitigating the Short and Long-Term Impacts of Psychosocial Trauma: Resilience and Relationships
The Role of Relationships in Community Resilience
7. Asset-Based Assessment and Community-Based Participatory Research (CBPR)
8. Summary and Implications
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- World Health Organization (WHO). Health in 2015: From the MDG’s, Millennium Developmental Goals to SDGs, Sustainable Developmental Goals; WHO: Geneva, Switzerland, 2015; Available online: http://apps.who.int/iris/bitstream/handle/10665/200009/9789241?sequence-1 (accessed on 19 July 2018).
- World Health Organization (WHO). Commission on Social Determinants of Health. 2008. Available online: http://apps.who.int/iris/bitstream/handle/10665/43943/9789241563703_eng.pdf;jsessionid=C7C01BD2CF8CF0CEB5CC301EDA7D1287?sequence=1 (accessed on 18 July 2018).
- United Nations (UN). Transforming Our World: The 2030 Agenda for Sustainable Development; UN: New York, NY, USA, 2015; Available online: https://sustainabledevelopment.un.org/post2015/transformingourworld/publication (accessed on 18 July 2018).
- World Health Organization (WHO). World Conference on the Social Determinants of Health. 2011. Available online: http://www.who.int/sdhconference/declaration/Rio_political_declaration.pdf (accessed on 17 July 2018).
- United Nations (UN). Toward a World Free from Violence: Global Survey on Violence against Children; United Nations: New York, NY, USA, 2016. [Google Scholar] [CrossRef]
- Amnesty International UK. Violence against Women. Available online: https://www.amnesty.org.uk/violence-against-women (accessed on 19 August 2018).
- United Nations (UN). Declaration on the Elimination of Violence against Women 48/104. 1993. Available online: http://www.un-documents.net/a48r104.html (accessed on 19 August 2018).
- MacKinnon, C.A. Rape, genocide, and women’s human rights. In Genocide and Human Rights; Latimer, M., Ed.; Routledge: London, UK, 2017; pp. 133–144. ISBN 9781351157551. [Google Scholar]
- United Nations (UN). Women’s Rights are Human Rights. 2014. Available online: https://www.ohchr.org/Documents/Publications/HR-PUB-14-2.pdf (accessed on 19 August 2018).
- Chetail, V. The human rights of migrants in general international law: From minimum standards to fundamental rights. In Migrants and Rights; Routledge: London, UK, 2017; pp. 3–34. [Google Scholar]
- Bustamante, L.H.U.; Cerqueira, R.O.; Leclerc, E.; Brietzke, E. Stress, trauma, and posttraumatic stress disorder in migrants: A comprehensive review. Braz. J. Psychiatry 2018, 40, 220–225. [Google Scholar] [CrossRef] [PubMed]
- FAO; IFAD; UNICEF; WFP; WHO. The State of Food Security and Nutrition in the World 2017: Building Resilience for Peace and Food Security; FAO: Rome, Italy, 2017. [Google Scholar]
- Bread for the World. 2016 Hunger Report: The Nourishing Effect: Ending Hunger, Improving Health, Reducing Inequality; Bread for the World Institute. Available online: http://hungerreport.org/2016/wp-content/uploads/2015/11/HR2016-Full-Report-Web.pdf (accessed on 14 July 2018).
- UNICEF; World Health Organization; The World Bank. Levels and Trends in Child Malnutrition. UNICEF/WHO/World Bank Group Joint Child Malnutrition Estimates Key Findings of the 2018 Edition. Available online: http://data.unicef.org/wp-content/uploads/2018/05/JME-2018-brochure-.pdf (accessed on 24 August 2018).
- Black, R.E.; Victora, C.G.; Walker, S.P.; Bhutta, Z.A.; Christian, P.; De Onis, M.; Ezzati, M.; Grantham-McGregor, S.; Katz, J.; Martorell, R.; et al. Maternal and child undernutrition and overweight in low income and middle-income countries. Lancet 2013, 382, 427–451. [Google Scholar] [CrossRef]
- Bryce, J.; Boschi-Pinto, C.; Shibuya, K.; Black, R.E. WHO estimates the causes of death in children. Lancet 2005, 365, 1147–1152. [Google Scholar] [CrossRef]
- Food Research and Action Center. Food Insecurity among Immigrants, Refugees, and Asylees. Children’s Health Watch, 2016. Available online: http://org2.salsalabs.com/o/5118/p/salsa/web/common/public/content?content_item_KEY=13089 (accessed on 14 July 2018).
- Hendrix, C.; Brinkman, H.-J. Food Insecurity and Conflict Dynamics: Causal Linkages and Complex Feedbacks; Presented at Food Insecurity in Protracted Crises-High Level Expert Forum; Ubiquity Press: Rome, Italy, 2012; Available online: http://www.fao.org/fileadmin/templates/cfs_high_level_forum/documents/FI-ConflictDynamics-Hendrix_Cullen.pdf (accessed on 10 August 2018).
- Felitti, V.J.; Anda, R.F.; Nordenberg, D.; Williamson, D.F.; Spitz, A.M.; Edwards, V.; Marks, J.S. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am. J. Prev Med. 1998, 14, 45–258. [Google Scholar] [CrossRef]
- Sameroff, A.J.; Seifer, R.; McDonough, S.C. Contextual contributors to the assessment of infant mental health. In Handbook of Infant, Toddler, and Preschool Mental Health; Del Carmen-Wiggins, R., Carter, A., Eds.; Oxford University Press: New York, NY, USA, 2004; pp. 154–196. ISBN 0-19-514438-4. [Google Scholar]
- Sanson, A.; Oberklaid, F.; Pedlow, R.; Prior, M. Risk indicators: Assessment of infancy predictors of pre-school behavioural maladjustment. J. Child Psychol. Psychiatry 1991, 32, 609–626. [Google Scholar] [CrossRef] [PubMed]
- ACE Interface. ACE Interface Master Trainer Program. Available online: www.aceinterface.com (accessed on 30 July 2018).
- Bellis, M.A.; Hughes, K.; Leckenby, N.; Jones, L.; Baban, A.; Kachaeva, M.; Povilaitis, R.; Pudule, I.; Qirjako, G.; Ulukol, B.; et al. Adverse childhood experiences and associations with health harming behaviors in young adults: Surveys in eight eastern European countries. Bull. World Health Organ. 2014, 92, 641–655. [Google Scholar] [CrossRef] [PubMed]
- Hughes, K.; Bellis, M.A.; Hardcastle, K.A.; Sethi, D.; Butchart, A.; Mikton, C.; Jones, L.; Dunne, M.P. The effect of multiple adverse childhood experiences on health: A systematic review and meta-analysis. Lancet Public Health 2017, 2, e356–e366. [Google Scholar] [CrossRef]
- Blodgett, C.; Lanigan, J.D. The association between adverse childhood experience (ACE) and school success in elementary school children. School Psychol. Q. 2018, 33, 137–146. [Google Scholar] [CrossRef] [PubMed]
- Jimenez, M.D.; Wade, R.; Lin, Y.; Morrow, L.M.; Reichman, N.E. Adverse experiences in early childhood and kindergarten outcomes. Pediatrics 2016, 137, peds-2015. [Google Scholar] [CrossRef] [PubMed]
- Kerker, B.D.; Zhang, J.; Nadeem, E.; Stein, R.E.; Hurlburt, M.S.; Heneghan, A.; Landsverk, J.; McCue Horwitz, S.K. Adverse childhood experiences and mental health, chronic medical conditions, and development in young children. Acad. Pediatric 2015, 15, 510–517. [Google Scholar] [CrossRef] [PubMed]
- Harold, G.T.; Sellers, R. Annual research review: Interparental conflict and youth psychopathology: An evidence review and practice update. J. Child Psychol. Psychiatry 2018, 59, 374–402. [Google Scholar] [CrossRef] [PubMed]
- National Research Council and Institute of Medicine. Depression in Parents, Parenting and Children: Opportunities to Improve Identification, Treatment, and Prevention; Committee on Depression, Parenting Practices, and the Healthy Development of Children; Board of Children, Youth, and Families; Division of Behavioral and Social Sciences and Education; The National Academies Press: Washington, DC, USA, 2009. [Google Scholar]
- Shonkoff, J.P.; Garner, A.S.; American Academy of Pediatrics Committee on Psychosocial Aspects of Child and Family Health; Committee on Early Childhood, Adoption, and Dependent Care; Section on Developmental and Behavioral Pediatrics. The lifelong effects of early childhood adversity and toxic stress. Pediatrics 2012, 129, e232–e246. [Google Scholar] [PubMed]
- Racine, N.; Plamodon, A.; Madigan, S.; McDonald, S.; Tough, S. Maternal adverse childhood experiences and infant development. Pediatrics 2018, 141, e20172495. [Google Scholar] [CrossRef] [PubMed]
- National Scientific Council on the Developing Child. Early Experiences Can Alter Gene Expression and Affect Long-Term Development: Working Paper No. 10. 2010. Available online: www.developingchild.harvard.edu (accessed on 2 August 2018).
- Rifkin-Graboi, A.; Borelli, J.L.; Enlon, M.B. Neurobiology of stress in infancy. In Handbook of Infant Mental Health, 3rd ed.; Zeanah, C.H., Ed.; Guilford Press: New York, NY, USA, 2009; pp. 59–79. ISBN 9781462506460. [Google Scholar]
- Sheridan, M.; Nelson, C.A. Neurobiology of fetal and infant development. In Handbook of Infant Mental Health, 3rd ed.; Zeanah, C.H., Ed.; Guilford Press: New York, NY, USA, 2009; pp. 40–58. ISBN 9781462506460. [Google Scholar]
- National Center on the Developing Child. Five Numbers to Remember About Early Childhood Development (Brief). 2009/2017. Available online: www.developingchild.harvard.edu (accessed on 10 August 2018).
- National Scientific Council on the Developing Child. Excessive Stress Disrupts the Architecture of the Developing Brain: Working Paper No. 3. 2005/2014. Available online: www.developingchild.harvard.edu (accessed on 10 August 2018).
- Dickerson, S.S.; Kemeny, M.E. Acute stressors and cortisol responses: A theoretical integration and synthesis of laboratory research. Psychol. Bull. 2004, 130, 355–391. [Google Scholar] [CrossRef] [PubMed]
- Koss, K.J.; Gunnar, M.R. Annual Research Review: Early adversity, the hypothalamic-pituitary-adrenocortical axis, and child psychopathology. J. Child Psychol. Psychiatry 2017, 59, 327–346. [Google Scholar] [CrossRef] [PubMed]
- Fink, G. Stress: Concepts, definitions, and history. In Reference Module in Neuroscience and Biobehavioral Psychology; Elsevier: New York, NY, USA, 2017; ISBN 978-0-12-809324-5. [Google Scholar] [CrossRef]
- Smith, S.M.; Vale, W.W. The role of the hypothalamic-pituitary-adrenal axis in neuroendocrine responses to stress. Dialogues Clin. Neurosci. 2006, 8, 383–395. [Google Scholar] [PubMed]
- Bush, N.R.; Jones-Mason, K.; Coccia, M.; Caron, Z.; Alkon, A.; Thomas, M.; Coleman-Phox, K.; Wadhwa, P.D.; Laraia, B.A.; Adler, N.E.; et al. Effects of pre- and postnatal maternal stress on infant temperament and autonomic nervous system reactivity and regulation in a diverse, low-income population. Dev. Psychopathol. 2017, 5, 1553–1571. [Google Scholar] [CrossRef] [PubMed]
- Zijlmans, M.; Riksen-Walraven, J.; Weerth, C. Associations between maternal prenatal cortisol concentrations and child outcomes: A systematic review. Neurosci. Biobehav. Rev. 2015, 53, 1–24. [Google Scholar] [CrossRef] [PubMed]
- Luby, J.L.; Barch, D.; Whalen, D.; Belden, A. Association between early life adversity and risk for poor emotional and physical health in adolescence: A putative mechanistic neurodevelopmental pathway. JAMA Pediatric. 2017, 171, 1168–1175. [Google Scholar] [CrossRef] [PubMed]
- Danese, A.; Moffitt, T.E.; Harrington, H.; Milne, B.J.; Polanczyk, G.; Pariante, C.M.; Poulton, R.; Caspi, A. Adverse childhood experiences and adult risk factors for age-related disease: Depression, inflammation, and clustering of metabolic risk markers. Arch. Pediatric. Adolesc. Med. 2009, 163, 135–143. [Google Scholar] [CrossRef] [PubMed]
- Barker, E.; Walton, E.; Cecil, C. Annual Research Review: DNA methylation as a mediator in the association between risk exposure and child and adolescent psychopathology. J. Child Psychol. Psychiatry 2018, 303–322. [Google Scholar] [CrossRef] [PubMed]
- Champagne, F.A. Epigenetic influence of social experiences across the lifespan. Dev. Psychobiol. 2010, 52, 299–311. [Google Scholar] [CrossRef] [PubMed]
- Starkweather, A.; Alhaeeri, A.; Montpetit, A.; Brumelle, J.; Filler, K.; Montpetit, M.; Mohanraj, L.; Lyon, D.; Jackson-Cook, C. An integrative review of factors associated with telomere length and implications for biobehavioral research. Nurs. Res. 2014, 73, 36–50. [Google Scholar] [CrossRef] [PubMed]
- Price, L.; Kao, H.; Burgers, D.; Carpenter, L.; Tyrka, A. Telomeres and early-life stress: An overview. Biol. Psychiatry 2013, 73, 15–23. [Google Scholar] [CrossRef] [PubMed]
- Coimbra, G.; Carvalho, C.; Moretti, P.; Mello, M.; Belangero, S. Stress-related telomere length in children: A systematic review. J. Psychiatr. Res. 2017, 92, 47–54. [Google Scholar] [CrossRef] [PubMed]
- Herman, H.; Steward, D.E.; Dias-Granados, N.; Berger, E.L.; Jackson, B.; Yuen, T. What is resilience? Can. J. Psychiatry 2011, 56, 258–265. [Google Scholar] [CrossRef] [PubMed]
- Wu, G.; Feder, A.; Cohen, H.; Kim, J.J.; Calderon, S.; Charney, D.S.; Mathe, A.A. Understanding resilience. Front. Behav. Neurosci. 2013. [Google Scholar] [CrossRef] [PubMed]
- Matsen, A.; Monn, A. Child and family resilience: A call for integrated science, practice, and professional training. Fam. Relat. 2015, 64, 5–21. [Google Scholar] [CrossRef]
- National Child Trauma CTSN Core Curriculum on Childhood Trauma Task Force. The 12 Core Concepts: Concepts for Understanding Traumatic Stress Responses in Children and Families; Core Curriculum on Childhood Trauma; UCLA-Duke University National Center for Child Traumatic Stress: Los Angeles, CA, USA; Durham, NC, USA, 2012. [Google Scholar]
- Matsen, A. Global perspectives on resilience in children and youth. Child Dev. 2014, 85, 6–20. [Google Scholar] [CrossRef]
- Zeanah, C.H.; Zeanah, P.D. The science of infant mental health. In Handbook of Infant Mental Health, 4th ed.; Zeanah, C.H., Ed.; Guilford Press: New York, NY, USA, 2018. [Google Scholar]
- Zeanah, C.H.; Boris, N.W.; Scheeringa, M.S. Psychopathology in infancy. J. Child Psychol. Psychiatry 1997, 38, 81–99. [Google Scholar] [CrossRef] [PubMed]
- Alpern, L.; Lyons-Ruth, K. Preschool children at social risk: Chronicity and timing of maternal depressive symptoms and child behavior problems at school and at home. Dev. Psychopathol. 1993, 5, 371–387. [Google Scholar] [CrossRef]
- Goodman, S.; Brand, S. Depression and early adverse experiences. In Handbook of Depression, 2nd ed.; Gotlib, I.H., Hammen, C.L., Eds.; Guilford Press: New York, NY, USA, 2009; pp. 249–274, ISBN-13 978-1609181505. [Google Scholar]
- Gunnar, M.; Quevedo, K. The neurobiology of stress and development. Ann. Rev. Psychol. 2007, 58, 145–173. [Google Scholar] [CrossRef] [PubMed]
- Parlari, M.; Frewens, P.; Nazarov, A.; Oremus, C.; MacQueen, G.; Lanius, L.; McKinnon, M. Alterations in empathic responding among women with posttraumatic stress disorder associated with childhood trauma. Brain Behav. 2014, 4, 381–389. [Google Scholar] [CrossRef] [PubMed]
- Pollak, S.D.; Nelson, C.A.; Schlaak, M.F.; Roeber, B.J.; Wewerka, S.S.; Wiik, K.L.; Frenn, K.A.; Loman, M.M.; Gunnar, M.R. Neurodevelopmental effects of early deprivation in post-institutionalized children. Child Dev. 2010, 81, 224–236. [Google Scholar] [CrossRef] [PubMed]
- Zeanah, C.H.; Humphreys, K.L.; Fox, N.A.; Nelson, C.A. Alternatives for abandoned children: Lessons from the Bucharest Early Intervention Project. Curr. Opin. Psychol. 2017, 15, 182–188. [Google Scholar] [CrossRef] [PubMed]
- Vanderwert, R.; Fox, N.A.; Nelson, C.A.; Zeanah, C.H. Normalization of EEG activity among previously institutionalized children placed into foster care: A 12-year follow-up of the Bucharest Early Intervention Project. Dev. Cognit. Neurosci. 2016, 17, 68–75. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Essentials for Childhood: Steps to Create Safe, Stable, and Nurturing Relationships and Environments for All Children. Available online: http://www.cdc.gov/ViolencePrevention/childmaltreatment/essentials/index.html (accessed on 15 July 2018).
- Ellis, W.R.; Dietz, W.S. A new framework for addressing Adverse Childhood Experience: The Building Community Resilience model. Acad. Pediatr. 2017, 17, S86–S93. [Google Scholar] [CrossRef] [PubMed]
- Traub, F.; Boynton-Jarrett, R. Modifiable resilience factors to childhood adversity for clinical pediatric practice. Pediatrics 2017, 139, e20162569. [Google Scholar] [CrossRef] [PubMed]
- Center for the Study of Social Policy. Core Meanings of the Strengthening Families Protective Factors; Center of the Study for Social Policy: Washington, DC, USA, 2015; Available online: https://cssp.org/resource/core-meanings-of-the-strengthening-families-protective-factors/ (accessed on 18 July 2018).
- Lancet. Series Advancing Early Child Development: From Science to Scale. 2016. Available online: Thelancet.com/series/ecd/2016 (accessed on 4 August 2018).
- Verbitsky-Savitz, N.; Hargreaves, M.; Penoyer, S.; Morales, N.; Coffee-Borden, B.; Whitesell, E. Preventing and Mitigating the Effects of ACEs by Building Community Capacity and Resilience: APPI Cross-Site Evaluation Findings; Mathematica Policy Research: Washington, DC, USA, 2016; Available online: http://www.appi-wa.org/ (accessed on 28 July 2018).
- Richter, L.M. Supporting parents to provide nurturing care to young children. Zero To Three 2018, 38, 10–16. [Google Scholar]
- World Health Organization (WHO). Building Resilience: A Key Pillar of Health 2020 and Sustainable Development Goals-Examples from the WHO Small Countries Initiative; Regional Office of the World Health Organization: Copenhagen, Denmark, 2017; Available online: http://www.euro.who.int/en/publications/abstracts/building-resilience-a-key-pillar-of-health-2020-and-the-sustainable-development-goals-examples-from-the-who-small-countries-initiative-2017 (accessed on 30 July 2018).
- Forstadt, L.; Cooper, S.; Andrews, S. Changing medicine and building community: Maine’s Adverse Childhood Experiences Momentum. Perm. J. 2015, 19, 92–95. [Google Scholar] [CrossRef] [PubMed]
- Larkin, H.; Shields, J.J.; Anda, R.F. The health and social consequences of Adverse Childhood Experiences (ACE) across the lifespan: An introduction to prevention and intervention in the community. J. Prev. Interv. Community 2012, 40, 263–270. [Google Scholar] [CrossRef] [PubMed]
- Addams, J. Twenty Years at Hull House; University of Illinois Press: Chicago, IL, USA, 1910/1990. [Google Scholar]
- Weissberg, P.; Greenberg, M.T. Prevention science and collaborative community action research: Combining the best from both perspectives. J. Mental Health 1998, 7, 479–492. [Google Scholar]
- Lewin, K. Action research and minority problems. J. Soc. Issues 1946, 2, 34–46. [Google Scholar] [CrossRef]
- Israel, B.A.; Schulz, A.J.; Parker, E.A.; Becker, A.B. Review of community-based research: Assessing partnership approaches to improve public health. Annu. Rev. Public Health 1998, 19, 173–202. [Google Scholar] [CrossRef] [PubMed]
- Mittelmark, M.B.; Hunt, M.K.; Heath, G.W.; Schmid, T.L. Realistic outcomes: Lessons from community-based research and demonstration programs for the prevention of cardiovascular diseases. J. Public Health Policy 1993, 14, 437–462. [Google Scholar] [CrossRef] [PubMed]
- Branom, C. Community-based participatory research as a social work research and intervention approach. J. Community Pract. 2012, 20, 260–273. [Google Scholar] [CrossRef]
- Reid, S.D.; Reddock, R.; Nickenig, T. Breaking the silence of child sexual abuse in the Caribbean: A community-based action research intervention model. J. Child Sexual Abuse 2014, 23, 256–277. [Google Scholar] [CrossRef] [PubMed]
- McKnight, J.L.; Kretzmann, J. Mapping Community Capacity; Institute for Policy Research, Northwestern University: Evanston, IL, USA, 1996. [Google Scholar]
- Ekono, M.; Yang, J.; Smith, S. Young Children in Deep Poverty; National Center for Children in Poverty, Mailman School of Public Health, Columbia University: New York, NY, USA, 2016. [Google Scholar]
- Corbie-Smith, G.; Thomas, S.B.; Williams, M.V.; Moody-Ayers, S. Attitudes and beliefs of African Americans toward participation in medical research. J. Gen. Int. Med. 1999, 14, 537–546. [Google Scholar] [CrossRef]
- Belle-Isle, L.; Benoit, C.; Pauly, B. Addressing health inequities through social inclusion: The role of community organizations. Action Res. 2014, 12, 177–193. [Google Scholar] [CrossRef]
- Minkler, M. Using participatory action research to build healthy communities. Public Health Rep. 2000, 115, 191. [Google Scholar] [CrossRef] [PubMed]
- Woods-Jaeger, B.A.; Cho, B.; Sexton, C.C.; Slagel, L.; Goggin, K. Promoting resilience: Breaking the intergenerational cycle of adverse childhood experiences. Health Educ. Behav. 2018. [Google Scholar] [CrossRef] [PubMed]
- Burstein, K.; Bryan, T.; Chao, P.-C. Promoting self-determination skills among youth with special needs using participatory action research. J. Dev. Phys. Disabil. 2005, 17, 185–201. [Google Scholar] [CrossRef]
- Cardazone, G.; Sy, A.U.; Chik, I.; Corlew, L.K. Mapping one strong ‘Ohana: Using network analysis and GIS to enhance the effectiveness of a statewide coalition to prevent child abuse and neglect. Am. J. Community Psychol. 2014, 53, 346–356. [Google Scholar] [CrossRef] [PubMed]
- Hall, J.; Porter, L.; Longhi, D.; Becker-Green, J.; Dreyfus, S. Reducing adverse childhood experiences (ACE) by building community capacity: A summary of Washington Family Policy Council research findings. J. Prev. Interv. Community 2012, 40, 325–334. [Google Scholar] [CrossRef] [PubMed]
- Sofolahan-Oladeinde, Y.; Mullins, C.D.; Baquet, C.R. Using community-based participatory research in patient-centered outcomes research to address health disparities in under-represented communities. J. Comp. Eff. Res. 2015, 4, 515–523. [Google Scholar] [CrossRef] [PubMed]
- Maternal Infant, and Early Childhood Home Visiting Technical Assistance Coordinating Center. MIECHV Issue Brief on Family Enrollment and Engagement. 2015. Available online: https://mchb.hrsa.gov/sites/default/files/mchb/MaternalChildHealthInitiatives/HomeVisiting/tafiles/enrollmentandengagement.pdf (accessed on 24 July 2018).
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zeanah, P.; Burstein, K.; Cartier, J. Addressing Adverse Childhood Experiences: It’s All about Relationships. Societies 2018, 8, 115. https://doi.org/10.3390/soc8040115
Zeanah P, Burstein K, Cartier J. Addressing Adverse Childhood Experiences: It’s All about Relationships. Societies. 2018; 8(4):115. https://doi.org/10.3390/soc8040115
Chicago/Turabian StyleZeanah, Paula, Karen Burstein, and Jeanne Cartier. 2018. "Addressing Adverse Childhood Experiences: It’s All about Relationships" Societies 8, no. 4: 115. https://doi.org/10.3390/soc8040115
APA StyleZeanah, P., Burstein, K., & Cartier, J. (2018). Addressing Adverse Childhood Experiences: It’s All about Relationships. Societies, 8(4), 115. https://doi.org/10.3390/soc8040115




