Abstract
Background: Subjective socioeconomic status (SES) is a powerful determinant of health and well-being, capturing individuals’ perceptions of their material conditions and security. While higher perceived financial and basic needs security are generally linked to better health outcomes, little is known about how these associations differ across global contexts. Drawing on data from 23 countries, this study tests whether these relationships are systematically weaker in Global South countries. Methods: Cross-sectional data from Wave 1 of the Global Flourishing Study (n = 207,000) were used to examine associations between subjective SES indicators—financial security and security in basic needs (food, housing, safety)—and two outcomes: self-rated physical health and mental health. All variables were measured on 0–10 scales. Linear regression models were estimated separately by Global South and Global North country status, adjusting for age and sex. Global South classification was based on standard development and geopolitical frameworks. Results: In both global regions, individuals with higher perceived financial and basic needs security reported significantly better mental and physical health. However, the strength of these associations was consistently weaker in Global South countries. Interaction terms confirmed that Global South status moderated the association between subjective SES and health outcomes. Conclusions: These findings suggest global-scale “diminished returns” of subjective SES on health, echoing patterns previously observed within countries. Structural inequalities, weaker public systems, and contextual adversity may dilute the health benefits of perceived security in Global South settings. Global health equity efforts must therefore move beyond individual-level interventions to address the broader systems that constrain the translation of socioeconomic resources into health.
1. Introduction
Socioeconomic conditions are key correlates of health and well-being [1,2,3]. A substantial body of research has shown that individuals with higher socioeconomic status (SES) generally report better physical and mental health, have longer life expectancy, and face lower risks of disability and chronic disease [4]. This association appears consistent across various SES indicators and a wide range of health outcomes [5].
While most research has emphasized objective indicators such as income [6], education [7], and occupational status [8], growing attention has been directed toward subjective SES [9]—individuals’ perceptions of their financial security, stability, and ability to meet basic needs [10,11]. These subjective measures are often more closely linked to stress, self-efficacy, and day-to-day experiences than objective indicators alone, and they may capture the lived experience of economic hardship or advantage more accurately in some settings [12].
Subjective SES includes constructs such as perceived financial security and the sense of having reliable access to basic necessities like food, housing, and safety [12,13]. These perceptions are psychologically salient and have been shown to influence mental and physical health through multiple pathways, including stress regulation, social comparison, and behavioral coping mechanisms [14,15]. Numerous studies have found that people who perceive themselves as financially secure or safe from material deprivation report better mental health, lower levels of depression and anxiety, and fewer physical health complaints [16,17].
However, recent research has raised critical questions about whether the protective effects of socioeconomic resources are uniform across populations. The theory of Marginalization-related Diminished Returns (MDRs) suggests that marginalized and disadvantaged groups tend to receive smaller health and developmental benefits from the same level of socioeconomic resources compared to more privileged groups [18,19]. Most of the evidence on MDRs has come from high-income countries like the United States [18,19], where racial and ethnic minorities often experience weaker protective effects of income, education, and employment on health outcomes due to structural segregation, racism, discrimination, and unequal opportunity structures [20].
Almost all previous research on Marginalization-related Diminished Returns (MDRs) has defined marginalization and disadvantage within a single country or region, typically based on social identities such as race, ethnicity, sexual orientation, rurality, caste, nativity, or neighborhood conditions. However, marginalization can also be conceptualized in a global context. From this perspective, populations in less developed or developing countries may be considered marginalized relative to those in more industrialized, high-income nations. This broader definition allows for the extension of the MDRs framework beyond within-country analyses to cross-national comparisons. Clearly specifying these definitions is essential when applying MDRs in international contexts and should be included in the Introduction section following the conceptual overview of MDRs.
A question that remains underexplored is whether such diminished returns also operate across countries and global regions [21,22,23]. In particular, it can be argued that the health benefits of subjective SES differ between the Global North [24,25]—comprising mostly high-income, industrialized countries—and the Global South [26], which includes many low- and middle-income countries facing legacies of colonialism, underdevelopment, and persistent structural inequality? While research on global health disparities has largely focused on differences in absolute levels of health or healthcare access, less is known about the relative strength of socioeconomic predictors across contexts.
This study seeks to address that gap. Using data from the Global Flourishing Study (GFS) [27,28,29,30,31,32,33], we examine whether subjective SES indicators—perceived financial security and security in food, housing, and safety—are more weakly associated with self-rated mental and physical health in Global South countries compared to Global North countries. Our hypothesis is informed by the logic of MDRs: we expect that even when individuals in Global South settings perceive themselves as socioeconomically secure, the broader structural context may limit the extent to which those perceptions translate into better health outcomes. By testing this hypothesis in a large, diverse, and globally representative sample, this study contributes to the emerging literature on contextual moderators of health returns to SES.
2. Methods
2.1. Study Design and Sample
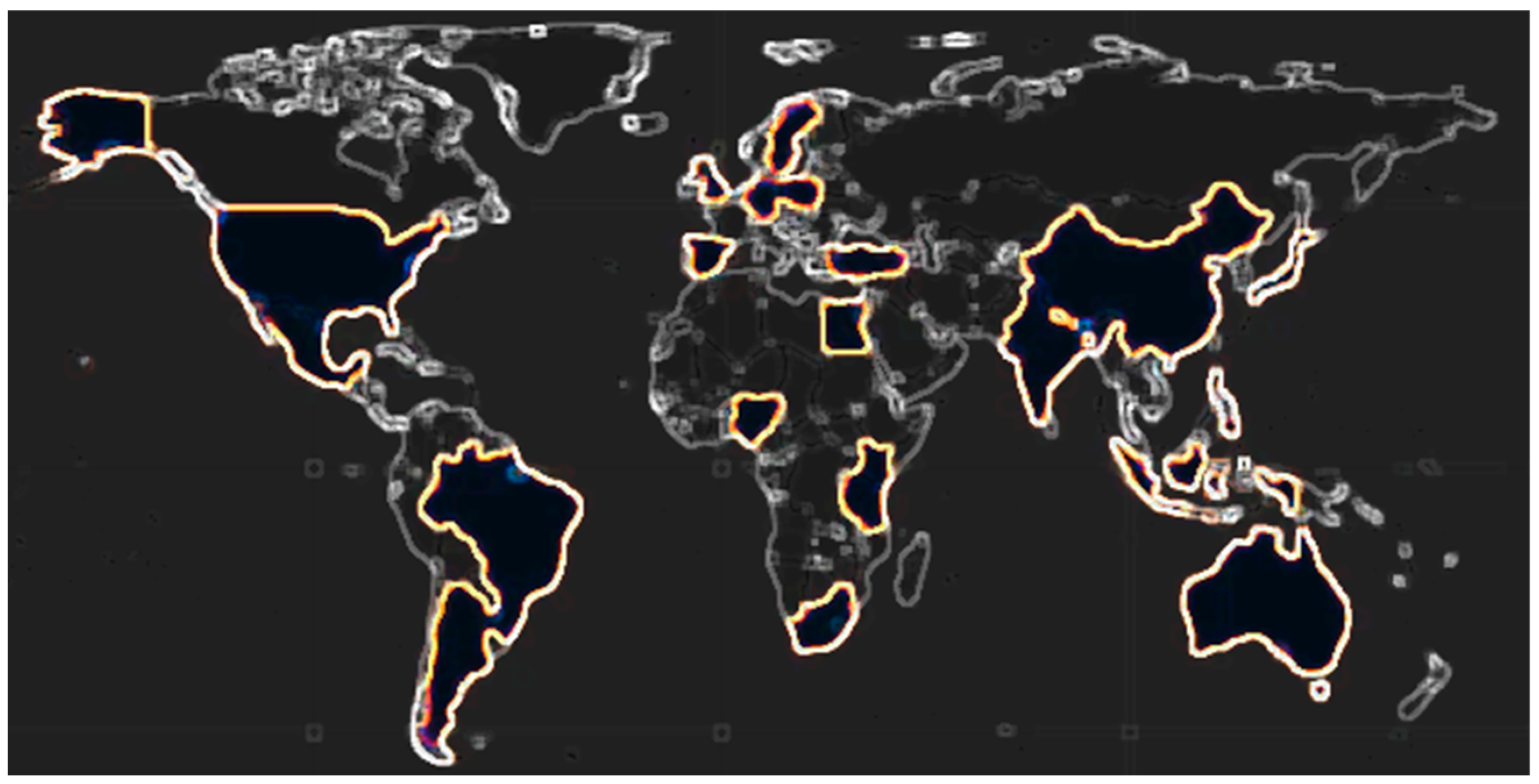
This study utilizes cross-sectional data from Wave 1 of the Global Flourishing Study (GFS) [27,28,29,30,31,32], conducted between 2021 and 2022. The GFS is a large, multi-country survey designed to assess well-being, human flourishing, and the social determinants of health across a broad range of global contexts. The analytic sample consists of approximately 207,000 adults from 23 countries, selected to reflect a wide diversity of economic development, cultural norms, and geographic regions. The countries included span both high-income and low- and middle-income nations (Figure 1), making the dataset well suited for cross-national comparative research on social gradients in health.
Figure 1.
Map of countries included in the GFS.
2.2. Measures
Subjective Socioeconomic Indicators (Independent Variables). We calculated our SES measure based on two subjective socioeconomic status (SES) indicators. This variable was the primary independent variables in this analysis. As each item ranged between 0 to 10, our SES measure ranged from 0 to 20.
2.2.1. Item 1: Perceived Financial Security
Participants rated their current sense of financial security on a scale from 0 (not at all secure) to 10 (completely secure). The exact question was “How often do you worry about being able to meet normal monthly living expenses?”. This measure reflects perceived financial well-being and economic stability in the respondent’s daily life. It was treated as a continuous variable, with higher scores indicating greater perceived financial security and, by extension, higher subjective SES.
2.2.2. Item 2: Perceived Security in Basic Needs
This measure assessed participants’ sense of security in meeting their basic needs, including access to adequate food, safe and stable housing, and physical safety. The specific question read as “How often do you worry about safety, food, or housing”. The response range was between 0 (Worry all of the time) to 10 (Do not ever worry). Participants responded on a 0–10 scale, with higher values indicating greater perceived security in these fundamental domains. This variable was also treated as continuous, with higher scores representing higher subjective SES.
2.3. Self-Rated Health (Dependent Variables)
Two single-item self-reported health measures were used to calculate our SRH as the dependent variable. As each item ranged between 0 and 10, our SRH outcome ranged from 0 to 20. Cronbach alpha of our measure was 0.7251 (Average interitem covariance: 3.171504 and average correlation between these two items = 0.5691).
2.3.1. Item 1: Mental Health
Respondents rated their overall mental health on a scale from 0 (poor) to 10 (excellent). The exact question read as “How would you rate your overall mental health?” [34,35,36]. Although brief, single-item measures of mental health have demonstrated substantial correlation with multi-item scales and are known to predict long-term outcomes such as life satisfaction, psychological distress, and future mental health status. They are widely used in population-level studies due to their efficiency and strong psychometric properties [37,38,39].
2.3.2. Item 2: Physical Health
Respondents similarly rated their physical health on a scale from 0 (poor) to 10 (excellent). The exact question read as “In general, how would you rate your physical health?”. Like the mental health measure, single-item physical health ratings are well validated, correlate highly with multi-dimensional health indices, and are robust predictors of mortality, healthcare use, and functional limitations. Both health outcome variables were modeled as continuous [40,41].
2.4. Moderator
Global South Status: A binary moderator variable was constructed to indicate whether a respondent resided in a Global South country (coded 1) or a Global North country (coded 0). Classification was based on international development status, gross national income, and geopolitical frameworks commonly used in comparative global health and international development studies. The Global South [25,26] countries (n = 14) included: Argentina, Brazil, Egypt, India, Indonesia, Kenya, Mexico, Nigeria, Philippines, South Africa, Tanzania, Türkiye, Hong Kong, and China. The Global North [25,26] countries (n = 9) included: Australia, Germany, Israel, Japan, Poland, Spain, United Kingdom, United States, and Sweden. This dichotomous variable allowed for testing whether the associations between subjective SES and health outcomes differed by global economic and geopolitical context.
2.5. Covariates
Age: Measured continuously as the number of years between a respondent’s birth year and the survey year. Age was treated as a continuous variable in all models to account for the well-established role of age in shaping health outcomes.
Sex: Based on self-report, sex was coded as a binary variable (1 = male, 0 = female). Respondents who identified as a gender other than male or female were coded as missing for this variable due to small sample size and for consistency in binary sex adjustment across models.
2.6. Statistical Analysis
To examine the association between subjective SES (range = 0–20) and health outcome (range = 0–20), we employed a series of linear regression models. Instead of modeling each subjective SES or SRH variable separately, we ran all our models with one (rather than two) predictor and outcome. All models were adjusted for age and sex as covariates. We first estimated our association in the pooled models that included all 23 countries, without any interaction term. Then we incorporated an interaction term between our SES indicator and the Global South status variable. This allowed for a formal test of whether the strength of the SES-health association varied significantly by Global South versus Global North classification. Subsequently, we estimated stratified models within Global South and Global North countries separately to assess the magnitude of association within each context. This stratification allowed for the comparison of effect sizes across geopolitical groupings and further examination of the “diminished returns” hypothesis. All analyses were conducted using Stata 18.0, and continuous variables were checked for linearity and distributional assumptions. No imputation was performed, and analyses were restricted to cases with complete data on all relevant variables.
2.7. Ethics
The Global Flourishing Study (GFS) was initially reviewed and approved by the Harvard University Institutional Review Board (IRB) as human subjects research involving survey data collection across over 20 countries. All respondents provided informed consent, and data were gathered following rigorous ethical and privacy protocols. Following collection, the data were fully de-identified by Gallup prior to being shared with researchers—removing all direct identifiers and preventing re-identification through coded linkage. As a result, the dataset now qualifies as non-human subjects research under U.S. federal regulations (45 CFR 46), and no further IRB review is required for secondary analysis.
3. Results
As shown in Table 1, the sample includes respondents from 23 countries, representing both Global South and Global North contexts. The Global South accounts for a substantial portion of the overall sample, with large contributions from Brazil (6.35%), India (6.14%), and Kenya (5.48%), alongside other countries such as Nigeria, Mexico, and the Philippines. In contrast, the Global North includes high-response countries like the United States (18.43%), Japan (9.88%), and Sweden (7.25%), which together represent a significant share of the total sample. The distribution reflects a broad geographic and economic diversity, enabling meaningful comparisons across regions.

Table 1.
Number of participants per countries.
Table 2 summarizes the descriptive characteristics of the pooled sample. Approximately 31.5% of participants were from countries in the Global North, while 68.5% were from the Global South. The sample was 52.8% female and 47.2% male. In terms of marital status, 54.8% of the respondents reported being married, and 45.2% were not married. The mean age of the participants was approximately 45.8 years (SE = 0.039; 95% CI: 45.726 to 45.878). The average score for perceived financial security was 11.96 (SE = 0.014; 95% CI: 11.930 to 11.985), and the mean score for self-rated health (SRH) was 14.74 (SE = 0.009; 95% CI: 14.718 to 14.754).

Table 2.
Descriptive Data.
Table 3 presents the bivariate correlations among key variables in the pooled sample. Self-reported physical and mental health (SRH) was positively correlated with financial security (r = 0.266), indicating that individuals with higher perceived financial stability reported better health outcomes. SRH was also modestly positively associated with being married (r = 0.101) and with residence in the Global South (r = 0.153), though correlations with age (r = −0.056) and gender (male; r = 0.031) were weak. Financial security itself was negatively correlated with Global South status (r = −0.085), suggesting lower average financial security among respondents from the Global South. Age was positively correlated with both financial security (r = 0.239) and marital status (r = 0.204), reflecting expected life-course patterns.

Table 3.
Correlations across study variables in the pooled sample.
In pooled regression models, financial security was a strong and significant predictor of the outcome across the global sample, with its effect further clarified by interaction with global region. In Model 1, which included only main effects, financial security (measured on a 0–20 scale) was positively associated with the outcome (B = 0.191, SE = 0.001, 95% CI: 0.189 to 0.194, p < 0.001), indicating a meaningful increase in well-being with each unit increase in perceived financial security. The addition of an interaction term in Model 2 revealed a marked difference by region: the main effect of financial security became substantially larger (B = 0.367, SE = 0.003, p < 0.001), while the negative interaction term for the Global South (B = −0.228, SE = 0.003, p < 0.001) indicated a significantly weaker association in that region. This suggests that while financial security is positively associated with well-being globally, the strength of this relationship is much greater in the Global North than in the Global South. Other predictors, such as age, marital status, and gender, remained statistically significant in both models, but their effects were notably smaller than the central role played by financial security and its interaction with region (Table 4).

Table 4.
Summary of Pooled Sample Models.
As shown in Table 5, in stratified regression analyses by global region, financial security demonstrated a strong and consistent association with the outcome, with a notably stronger effect in the Global North compared to the Global South. In the Global North (Model 3), financial security (0–20 scale) was a powerful predictor (B = 0.370, SE = 0.003, 95% CI: 0.365 to 0.376, p < 0.001), indicating that each unit increase in perceived financial security was associated with a substantial rise in the outcome variable. In contrast, while still statistically significant, the effect in the Global South (Model 4) was markedly smaller (B = 0.137, SE = 0.002, 95% CI: 0.133 to 0.140, p < 0.001). This contrast suggests that financial security may play a more prominent role in shaping well-being outcomes in the Global North, where baseline economic stability may heighten the relative impact of perceived financial control. Other variables, such as age, marital status, and gender, also showed expected patterns, but their effects were smaller in magnitude and less consistent across regions compared to the dominant influence of financial security.

Table 5.
Summary of Pooled Sample Models.
4. Discussion
This study adds to a growing body of evidence suggesting that the association between socioeconomic status and health is not uniform across populations or contexts. We found that subjective SES—perceived financial security and perceived basic needs security—was associated with both self-rated health across a large, global sample. Individuals who felt more secure in their finances or confident in their ability to access basic needs consistently reported better health, regardless of their geographic location.
While the association between socioeconomic status (SES) and health is well-established in prior research, our study extends this line of inquiry by examining whether the magnitude of this association systematically varies across geopolitical contexts—specifically, between the Global North and Global South. This cross-contextual comparison is both timely and underexplored. By applying the lens of Marginalization-related Diminished Returns (MDRs) [19], we shift the focus from merely documenting associations to interrogating inequities in the health benefits of perceived SES across settings that differ in structural capacity, economic development, and institutional trust.
The novelty of our work lies not in the identification of the SES–health gradient itself, but in uncovering whether this gradient flattens under marginalizing macro-contexts. A second key contribution is our use of the Global Flourishing Study (GFS) [27,28,29,30,31,32,33]—a large, harmonized, multi-country dataset—which allowed us to test the MDRs framework at a cross-national level using subjective SES [42,43,44]. This measure, which captures perceived social standing, offers important insight that is often missed by objective SES indicators, as it reflects lived experiences and psychosocial stressors more directly.
Whereas many prior MDRs studies have focused on within-country disparities—most commonly across race, ethnicity, or immigrant status in the U.S.—our study introduces country-level marginalization as a new dimension of multi-level analysis [45,46]. This approach expands the empirical reach of the MDRs framework and highlights how national-level structural and institutional constraints may diminish the health-enhancing effects of perceived financial and social standing.
We acknowledge the need to better clarify the rationale for combining self-rated mental and physical health. While these are conceptually distinct domains, our data showed a strong correlation between them (Cronbach’s alpha > 0.7), suggesting acceptable internal consistency. Theoretical frameworks also support this decision: prior work suggests individuals tend to evaluate health across domains in similar ways, influenced by common factors such as affective response styles, chronic stress, and overall perceptions of well-being [47,48,49]. However, we will expand this section with further theoretical justification and relevant citations, and we are open to disaggregating the two domains in future analyses if empirical support is limited.
Although we found statistically significant associations between subjective SES and self-rated health, the effect sizes were modest. These associations should not be interpreted as causal. Rather, the relationship between SES and health is likely bidirectional—with SES influencing health and health, in turn, shaping one’s perception of social standing [50]. Moreover, other unmeasured variables are likely to confound this relationship, so findings must be interpreted with caution.
Subjective SES may influence physical and mental health through multiple psychosocial and biological mechanisms. Individuals who perceive themselves as having low social standing may experience chronic stress, reduced sense of control, and heightened vigilance—psychological states linked to physiological dysregulation, including elevated cortisol, inflammation, and metabolic disturbances [51]. These stress-related processes may contribute to poor health outcomes independent of objective resources. Additionally, perceived low SES may affect health behaviors and erode psychological resilience, amplifying health risks.
It is important to note that our models did not adjust for several key potential confounders—such as education level, employment status, household income, urban/rural residence, access to healthcare, or prevailing cultural and political norms. This omission limits the interpretability of our findings. For instance, two individuals with identical incomes might perceive their SES very differently based on local context, peer comparison, or cultural expectations. Future research should incorporate these contextual variables to more accurately estimate the effects of subjective SES.
Another limitation concerns our use of a binary classification of countries as Global North versus Global South [52,53]. While this distinction is widely used in global health discourse, it masks substantial heterogeneity within each category. For example, countries in the Global South vary considerably in income levels, inequality, political stability, and welfare policies. These contextual differences likely influence how individuals perceive and report both SES and health. Future studies should consider multilevel or country-specific models to capture within-region variation and better assess structural influences. Although our current sample size limited such analyses, this remains an important direction for future research.
The strength of the link between subjective SES and perceived health varied systematically by global region. Consistent with our hypothesis and the framework of Minorities’ Diminished Returns [19], we found that the health benefits of perceived socioeconomic security were significantly weaker in Global South countries. The interaction terms in our regression models confirmed that Global South status moderated the relationship between subjective SES and self-rated health. In essence, even when individuals in the Global South perceive themselves as socioeconomically secure, these perceptions are less predictive of good health compared to individuals in the Global North.
This global pattern parallels what has been observed within countries like the United States, where marginalized racial and ethnic groups often experience smaller health gains from income [54], education [55], and employment [56]. Several mechanisms may explain this phenomenon. First, in the Global South, socioeconomic security might be more precarious or unstable due to weaker institutional protections, more volatile economic conditions, and less comprehensive social safety nets. Thus, even individuals who report feeling secure might be exposed to greater uncertainty and environmental risk, which can undermine the health benefits of that security.
Second, the infrastructure required to convert socioeconomic security into health—such as accessible healthcare, clean environments, and stable public services—might be less available in Global South settings [57,58,59]. This creates a structural ceiling on how much subjective SES can impact health outcomes [60]. Third, social inequality and stress might be more pervasive in some Global South contexts, meaning that the psychological burden of inequality remains high even among those who report higher subjective SES [57].
These findings have important implications. First, they highlight the need to consider contextual modifiers when interpreting the health implications of SES indicators. Second, they call attention to the limitations of individual-level approaches to health promotion in low- and middle-income settings. Simply improving perceived or actual SES may not be enough if the broader structural conditions do not support health equity. Finally, the findings suggest that global public health efforts should move beyond narrow indicators of material well-being and incorporate structural reforms that enable individuals to fully benefit from their socioeconomic resources.
People in the Global South often face significant barriers to achieving high levels of health due to enduring political and structural challenges. Many countries in this region experience ongoing political instability, armed conflicts, and weak or fragile democracies that limit the capacity of governments to provide consistent and equitable public services, including healthcare, education, and social protection. Corruption within public institutions can further erode trust in the system and divert resources away from essential health infrastructure [61,62,63]. In some contexts, poor enforcement of human rights and civil liberties exacerbates social exclusion and psychological distress, particularly among marginalized populations [64,65,66]. These structural and political conditions create a backdrop of chronic stress and insecurity that can undermine both the perceived and actual benefits of socioeconomic resources, contributing to worse health outcomes and limiting the effectiveness of individual-level interventions [67].
Our results also reinforce the value of subjective SES measures in global health research. While objective SES measures are indispensable, subjective measures may better capture personal vulnerability, stress, and perceived opportunity—factors that directly impact well-being.
5. Future Research
Future research should build on the current findings by addressing several limitations and extending the scope of inquiry in meaningful directions. One important avenue is the exploration of heterogeneity within and across world regions. While this study was limited to contrasting Global South and Global North countries, the classification may mask important within-region variability. Future work should examine country-specific patterns and consider contextual features such as political stability, urbanization, healthcare infrastructure, and local economic conditions that may shape how socioeconomic status relates to health. Studies focusing on urban versus rural populations, or regions with varying levels of development, can uncover more granular insights into how context moderates these associations.
Expanding the range of socioeconomic indicators is also essential. This study focused on subjective perceptions of financial and basic needs security, but future research should include more comprehensive SES indicators such as objective income, educational attainment, occupational status, wealth, and housing quality. Including social capital, access to public services, and informal safety nets may also provide a more complete picture of how socioeconomic resources function in diverse global settings. This multidimensional approach would help disentangle which aspects of SES matter most for health and whether the strength of these relationships varies by context.
In addition to broadening the measurement of SES, future studies should move beyond self-rated health outcomes. While self-rated mental and physical health are valuable subjective measures, they are also prone to bias and cross-cultural variation in reporting. Incorporating more objective health metrics—such as clinically diagnosed conditions, physical assessments, or validated psychological scales—can improve the validity of findings. Where feasible, biological markers such as blood pressure, inflammatory cytokines, or stress hormones could be integrated to explore physiological mechanisms underlying the associations between SES and health.
The generalizability of the findings could also be enhanced by examining other life stages. This study focused on adults, but children, adolescents, and older adults may experience different types of socioeconomic vulnerability and may derive different levels of health benefit from perceived security. Developmental stages interact with social environments in unique ways, and understanding these patterns over the life course would deepen our knowledge of when and how SES exerts its influence on health.
Longitudinal research is urgently needed to test the stability and direction of the observed relationships. The cross-sectional design of this study limits causal inference. Future work should leverage repeated measures over time to explore how changes in subjective SES relate to changes in health outcomes. Longitudinal designs would also allow for the examination of cumulative exposure and critical periods of vulnerability. To strengthen causal interpretations, researchers could apply methods such as fixed-effects models, propensity score matching, or instrumental variable approaches to adjust for unmeasured confounding.
Another promising direction is the integration of biological and stress-related measures. By collecting biomarkers related to stress physiology, such as cortisol, C-reactive protein, or epigenetic aging indices, future research can test how socioeconomic insecurity may “get under the skin”. Such data can help unpack the pathways through which perceived SES influences health, particularly under conditions of chronic adversity common in Global South contexts.
Future research should also include a wider array of covariates and potential confounders. While this study controlled for age and sex, additional variables such as employment status, marital status, household size, religious involvement, and exposure to violence could refine our understanding of the SES-health link. These variables may not only confound but also interact with socioeconomic factors, potentially modifying their health effects.
Cross-national studies would further benefit from incorporating policy-level variables. Linking individual-level data with indicators of national welfare policies, healthcare access, labor protections, and social expenditures could clarify how macro-level institutions shape the strength of SES-health associations. Comparative research across different welfare regimes may reveal which policy environments enhance or diminish the health benefits of socioeconomic security.
Another direction involves moving beyond national averages to study subnational and regional disparities. Particularly in large, diverse countries such as Brazil, India, or China, there is likely substantial variation in structural conditions across states or provinces. Analyzing SES-health associations at more localized levels would allow researchers to better understand place-based inequality.
Finally, researchers should consider the cultural interpretation of SES and health. Subjective SES measures may reflect different meanings across cultural and linguistic contexts. Qualitative and mixed-methods research can complement quantitative findings by exploring how individuals conceptualize financial security, basic needs, and health. Such work can improve the validity of international comparisons and illuminate the psychosocial mechanisms linking SES to well-being.
Together, these research directions can deepen our understanding of the complex and context-sensitive ways in which socioeconomic conditions shape health outcomes globally. They can also help guide policy efforts to ensure that socioeconomic improvements lead to tangible health benefits across diverse populations.
6. Limitations
Several limitations should be acknowledged. This study used cross-sectional data, which limits the ability to draw conclusions about causality or directionality. All measures were self-reported and might be influenced by cultural norms or reporting biases. Additionally, the classification of countries into Global North and South is somewhat simplified and may obscure within-country heterogeneity. Despite these limitations, the study provides compelling evidence for context-dependent returns of socioeconomic security on health. Future work should explore these dynamics using longitudinal data and examine whether similar patterns hold for other outcomes such as flourishing, resilience, or life satisfaction.
7. Conclusions
This study demonstrates that while subjective socioeconomic security is positively associated with health worldwide, its health benefits are more limited in Global South countries. These findings extend the concept of diminished returns to the global level and underscore the importance of structural factors in shaping how socioeconomic resources translate into health. Achieving global health equity requires not only increasing access to SES resources but also ensuring that access to these resources can be effectively converted into health and well-being across all contexts.
Funding
This research received no external funding.
Institutional Review Board Statement
The present study utilized data from the Global Flourishing Study (GFS), which is publicly available and fully deidentified. The parent study received Institutional Review Board (IRB) approval from Harvard University, and all data were collected anonymously. Ethical review and approval were waived for this study due to the de-identified and publicly accessible nature of the dataset; this secondary analysis was classified as not involving human subjects research.
Informed Consent Statement
For this analysis, consent was waived due to the fact that this is a secondary analysis of deidentified publicly available data.
Data Availability Statement
Data of the Global Flourishing Study are available through the Center for Open Science upon submission of a pre-registration (https://doi.org/10.17605/OSF.IO/3JTZ8) and will be openly available without pre-registration beginning 2026. Please see https://www.cos.io/gfs-access-data (accessed on 9 June 2025) for more information about data access.
Conflicts of Interest
The author declares no conflict of interest.
References
- Link, B.G.; Phelan, J. Social conditions as fundamental causes of disease. J. Health Soc. Behav. 1995, 36, 80–94. [Google Scholar] [CrossRef]
- Phelan, J.C.; Link, B.G.; Tehranifar, P. Social conditions as fundamental causes of health inequalities: Theory, evidence, and policy implications. J. Health Soc. Behav. 2010, 51, S28–S40. [Google Scholar] [CrossRef]
- Masters, R.K.; Link, B.G.; Phelan, J.C. Trends in education gradients of ‘preventable’ mortality: A test of fundamental cause theory. Soc. Sci. Med. 2015, 127, 19–28. [Google Scholar] [CrossRef] [PubMed]
- Feinstein, J.S. The relationship between socioeconomic status and health: A review of the literature. Milbank Q. 1993, 71, 279–322. [Google Scholar] [CrossRef] [PubMed]
- Chen, E.; Miller, G.E. Socioeconomic status and health: Mediating and moderating factors. Annu. Rev. Clin. Psychol. 2013, 9, 723–749. [Google Scholar] [CrossRef]
- Ettner, S.L. New evidence on the relationship between income and health. J. Health Econ. 1996, 15, 67–85. [Google Scholar] [CrossRef] [PubMed]
- Lawrence, E.M.; Rogers, R.G.; Zajacova, A. Educational Attainment and Mortality in the United States: Effects of Degrees, Years of Schooling, and Certification. Popul. Res. Policy Rev. 2016, 35, 501–525. [Google Scholar] [CrossRef] [PubMed]
- Van Der Noordt, M.; IJzelenberg, H.; Droomers, M.; Proper, K.I. Health effects of employment: A systematic review of prospective studies. Occup. Environ. Med. 2014, 71, 730–736. [Google Scholar] [CrossRef]
- Quon, E.C.; McGrath, J.J. Subjective socioeconomic status and adolescent health: A meta-analysis. Health Psychol. 2014, 33, 433. [Google Scholar] [CrossRef]
- Gundersen, C.; Ziliak, J.P. Food insecurity and health outcomes. Health Aff. 2015, 34, 1830–1839. [Google Scholar] [CrossRef]
- Murthy, V.H. Food insecurity: A public health issue. Public Health Rep. 2016, 131, 655–657. [Google Scholar]
- Guan, N.; Guariglia, A.; Moore, P.; Xu, F.; Al-Janabi, H. Financial stress and depression in adults: A systematic review. PLoS ONE 2022, 17, e0264041. [Google Scholar] [CrossRef]
- Friel, S.; Ford, L. Systems, food security and human health. Food Secur. 2015, 7, 437–451. [Google Scholar] [CrossRef]
- Ejiohuo, O.; Onyeaka, H.; Unegbu, K.C.; Chikezie, O.G.; Odeyemi, O.A.; Lawal, A.; Odeyemi, O.A. Nourishing the mind: How food security influences mental wellbeing. Nutrients 2024, 16, 501. [Google Scholar] [CrossRef] [PubMed]
- Maynard, M.; Andrade, L.; Packull-McCormick, S.; Perlman, C.M.; Leos-Toro, C.; Kirkpatrick, S.I. Food insecurity and mental health among females in high-income countries. Int. J. Environ. Res. Public Health 2018, 15, 1424. [Google Scholar] [CrossRef] [PubMed]
- Trudell, J.P.; Burnet, M.L.; Ziegler, B.R.; Luginaah, I. The impact of food insecurity on mental health in Africa: A systematic review. Soc. Sci. Med. 2021, 278, 113953. [Google Scholar] [CrossRef]
- Onyeaka, H.; Ejiohuo, O.; Taiwo, O.R.; Nnaji, N.D.; Odeyemi, O.A.; Duan, K.; Nwaiwu, O.; Odeyemi, O. The intersection of food security and mental health in the pursuit of sustainable development goals. Nutrients 2024, 16, 2036. [Google Scholar] [CrossRef]
- Assari, S. Unequal Gain of Equal Resources across Racial Groups. Int. J. Health Policy Manag. 2018, 7, 1–9. [Google Scholar] [CrossRef]
- Assari, S. Health Disparities due to Diminished Return among Black Americans: Public Policy Solutions. Soc. Issues Policy Rev. 2018, 12, 112–145. [Google Scholar] [CrossRef]
- Assari, S.; Boyce, S.; Bazargan, M. Subjective Family Socioeconomic Status and Adolescents’ Attention: Blacks’ Diminished Returns. Children 2020, 7, 80. [Google Scholar] [CrossRef]
- Bakhtiari, E. Diminished Returns in Europe: Socioeconomic Status and Ethno-Racial Health Disparities Across 30 Countries in the European Social Survey. J. Racial Ethn. Health Disparities 2022, 9, 2412–2426. [Google Scholar] [CrossRef] [PubMed]
- León-Pérez, G.; Bakhtiari, E. How Education Shapes Indigenous Health Inequalities in the USA and Mexico. J. Racial Ethn. Health Disparities 2025, 12, 837–850. [Google Scholar] [CrossRef] [PubMed]
- Al-Kassab-Córdova, A.; Mezones-Holguin, E.; Kaufman, J.S. Diminished returns of maternal education on children’s vaccination status for indigenous women in Peru. Soc. Sci. Med. 2025, 370, 117862. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.U.; Oleribe, O.; Njie, R.; Taylor-Robinson, S.D. A time for new north–south relationships in global health. Int. J. Gen. Med. 2017, ume 10, 401–408. [Google Scholar] [CrossRef]
- Kowalski, A.M. Global south-global north differences. In No Poverty; Springer: Berlin/Heidelberg, Germany, 2021; pp. 389–400. [Google Scholar]
- Chirisa, I.; Muneta, Z. The Global South and Sustainability: Issues and Constraints. In The Palgrave Handbook of Global Sustainability; Springer: Berlin/Heidelberg, Germany, 2023; pp. 955–968. [Google Scholar]
- Levin, J.; Bradshaw, M.; Johnson, B.R. Association between Jewish religious observance and mental health among Israeli adults: Findings from the Global Flourishing Study. Int. J. Psychiatry Med. 2025, 60, 338–355. [Google Scholar] [CrossRef]
- Lomas, T.; Bradshaw, M.; Case, B.; Cowden, R.G.; Crabtree, S.; English, C.; Fogleman, A.; Johnson, K.A.; Ritter, Z.; Johnson, B.R. The development of the Global Flourishing Study questionnaire: Charting the evolution of a new 109-Item inventory of human flourishing. BMC Glob. Public Health 2025, 3, 30. [Google Scholar] [CrossRef]
- Johnson, B.R.; VanderWeele, T.J. The global flourishing study: A new era for the study of well-being. Int. Bull. Mission. Res. 2022, 46, 272–275. [Google Scholar] [CrossRef]
- VanderWeele, T.J.; Johnson, B.R.; Bialowolski, P.T.; Bonhag, R.; Bradshaw, M.; Breedlove, T.; Case, B.; Chen, Y.; Chen, Z.J.; Counted, V. The Global Flourishing Study: Study profile and initial results on flourishing. Nat. Ment. Health 2025, 3, 636–653. [Google Scholar] [CrossRef] [PubMed]
- Levin, J.; Bradshaw, M.; Johnson, B.R. Religious Differences in Physical and Mental Health among Israeli Jews: Findings from the Global Flourishing Study. J. Relig. Health 2024, 63, 2544–2558. [Google Scholar] [CrossRef]
- Padgett, R.N.; Cowden, R.G.; Chattopadhyay, M.; Han, Y.; Honohan, J.; Ritter, Z.; Srinivasan, R.; Johnson, B.R.; VanderWeele, T.J. Survey sampling design in wave 1 of the Global Flourishing Study. Eur. J. Epidemiol. 2025, 40, 391–406. [Google Scholar] [CrossRef]
- Assari, S.; Najand, B.; Donovan, A. Sex/Gender Differences in the Effects of Childhood Abuse on Future Risk of Depression: Longitudinal Evidence from the Global Flourishing Study. Children 2025, 12, 754. [Google Scholar] [CrossRef] [PubMed]
- Levinson, D.; Kaplan, G. What does self rated mental health represent. J. Public Health Res. 2014, 3, 287. [Google Scholar] [CrossRef]
- Berkman, P.L. Measurement of mental health in a general population survey. Am. J. Epidemiol. 1971, 94, 105–111. [Google Scholar] [CrossRef] [PubMed]
- Grau, L.; West, B.; Gregory, P. “ How do you feel?” Self-Reported Health as an Indicator of Current Physical and Mental Health Status. J. Psychosoc. Nurs. Ment. Heal. Serv. 1998, 36, 24–30. [Google Scholar] [CrossRef]
- Lee, Y. The predictive value of self assessed general, physical, and mental health on functional decline and mortality in older adults. J. Epidemiol. Community Health 2000, 54, 123–129. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, F.; Jhajj, A.K.; Stewart, D.E.; Burghardt, M.; Bierman, A.S. Single item measures of self-rated mental health: A scoping review. BMC Health Serv. Res. 2014, 14, 398. [Google Scholar] [CrossRef] [PubMed]
- Mawani, F.N.; Gilmour, H. Validation of self-rated mental health. Health Rep. 2010, 21, 61–75. [Google Scholar]
- Fayers, P.M.; Sprangers, M.A. Understanding self-rated health. Lancet 2002, 359, 187–188. [Google Scholar] [CrossRef]
- Hill, P.L.; Allemand, M.; Roberts, B.W. Examining the pathways between gratitude and self-rated physical health across adulthood. Personal. Individ. Differ. 2013, 54, 92–96. [Google Scholar] [CrossRef]
- Assari, S.; Boyce, S.; Bazargan, M. Subjective Socioeconomic Status and Children’s Amygdala Volume: Minorities’ Diminish Returns. NeuroSci 2020, 1, 59–74. [Google Scholar] [CrossRef]
- Assari, S.; Preiser, B.; Lankarani, M.M.; Caldwell, C.H. Subjective Socioeconomic Status Moderates the Association between Discrimination and Depression in African American Youth. Brain Sci. 2018, 8, 71. [Google Scholar] [CrossRef] [PubMed]
- Assari, S.; Smith, J.; Mistry, R.; Farokhnia, M.; Bazargan, M. Substance Use among Economically Disadvantaged African American Older Adults; Objective and Subjective Socioeconomic Status. Int. J. Environ. Res. Public Health 2019, 16, 1826. [Google Scholar] [CrossRef] [PubMed]
- Merlo, J.; Chaix, B.; Ohlsson, H.; Beckman, A.; Johnell, K.; Hjerpe, P.; Råstam, L.; Larsen, K. A brief conceptual tutorial of multilevel analysis in social epidemiology: Using measures of clustering in multilevel logistic regression to investigate contextual phenomena. J. Epidemiol. Community Health 2006, 60, 290–297. [Google Scholar] [CrossRef] [PubMed]
- Peugh, J.L. A practical guide to multilevel modeling. J. Sch. Psychol. 2010, 48, 85–112. [Google Scholar] [CrossRef] [PubMed]
- Ames, A.J.; Myers, A.J. Explaining Variability in Response Style Traits: A Covariate-Adjusted IRTree. Educ. Psychol. Meas. 2021, 81, 756–780. [Google Scholar] [CrossRef]
- Ames, A.J. Measuring Response Style Stability Across Constructs With Item Response Trees. Educ. Psychol. Meas. 2022, 82, 281–306. [Google Scholar] [CrossRef]
- He, J.; van de Vijver, F.J.R. A general response style factor: Evidence from a multi-ethnic study in the Netherlands. Personal. Individ. Differ. 2013, 55, 794–800. [Google Scholar] [CrossRef]
- Barakat, C.; Konstantinidis, T. A Review of the Relationship between Socioeconomic Status Change and Health. Int. J. Environ. Res. Public Health 2023, 20, 6249. [Google Scholar] [CrossRef]
- Singh-Manoux, A.; Marmot, M.G.; Adler, N.E. Does subjective social status predict health and change in health status better than objective status? Psychosom. Med. 2005, 67, 855–861. [Google Scholar] [CrossRef]
- Reidpath, D.D.; Allotey, P. The problem of ‘trickle-down science’ from the Global North to the Global South. BMJ Glob. Health 2019, 4, e001719. [Google Scholar] [CrossRef]
- Pratt, B.; de Vries, J. Where is knowledge from the global South? An account of epistemic justice for a global bioethics. J. Med. Ethics 2023, 49, 325–334. [Google Scholar] [CrossRef] [PubMed]
- Assari, S.; Lankarani, M.M.; Caldwell, C.H. Does Discrimination Explain High Risk of Depression among High-Income African American Men? Behav. Sci. 2018, 8, 40. [Google Scholar] [CrossRef] [PubMed]
- Assari, S.; Cobb, S.; Saqib, M.; Bazargan, M. Diminished Returns of Educational Attainment on Heart Disease among Black Americans. Open Cardiovasc. Med. J. 2020, 14, 5–12. [Google Scholar] [CrossRef] [PubMed]
- Ayoubian, A.; Najand, B.; Assari, S. Black americans’ diminished health returns of employment during COVID-19 pandemic. Int. J. Travel Med. Glob. Health 2022, 10, 114–121. [Google Scholar] [CrossRef]
- Nzeakah, C.W.; DadeMatthews, A.O.; Onofa, U.O.; DadeMatthews, O.D.; Ogundare, T. Crippled By Fear: Anxiety Disorders Among Adolescents In Nigeria. Int. J. Psychiatry 2022, 7, 103–115. [Google Scholar] [CrossRef]
- Villarreal, A. The Two Faces of Fear: Violence and Inequality in the Mexican Metropolis; Oxford University Press: Oxford, UK, 2024. [Google Scholar]
- Bogin, B. Fear, violence, inequality, and stunting in Guatemala. Am. J. Hum. Biol. 2022, 34, e23627. [Google Scholar] [CrossRef] [PubMed]
- Osabuohien, E.; Odularu, G.; Ufua, D.; Augustine, D.; Osabohien, R. Socioeconomic shocks, inequality and food systems in the Global South: An introduction. Contemp. Soc. Sci. 2022, 17, 77–83. [Google Scholar] [CrossRef]
- Zhang, Y.; Kim, M.-H. Do public corruption convictions influence citizens’ trust in government? The answer might not be a simple yes or no. Am. Rev. Public Adm. 2018, 48, 685–698. [Google Scholar] [CrossRef]
- Uslaner, E.M. Trust and corruption. In The New Institutional Economics of Corruption; Routledge: Oxford, UK, 2004; pp. 90–106. [Google Scholar]
- Solé-Ollé, A.; Sorribas-Navarro, P. Does corruption erode trust in government. Evid. A Recent Surge Local Scandal. Spain. 2014. Available online: https://ieb.ub.edu/en/publication/2014-26-does-corruption-erode-trust-in-government-evidence-from-a-recent-surge-of-local-scandals-in-spain/ (accessed on 25 May 2025).
- Brownlee, K. A human right against social deprivation. Philos. Q. 2013, 63, 199–222. [Google Scholar] [CrossRef]
- Jiloha, R. Deprivation, discrimination, human rights violation, and mental health of the deprived. Indian J. Psychiatry 2010, 52, 207–212. [Google Scholar] [CrossRef] [PubMed]
- Harris, A.P.; Pamukcu, A. The civil rights of health: A new approach to challenging structural inequality. UCLA L. Rev. 2020, 67, 758. [Google Scholar]
- Assari, S.; Jahromi, M.; Zare, H. Unequal Benefits: How Parental Education Falls Short for Black and Latino Youth. Open J. Educ. Res. 2025, 5, 1232. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).