Quantitative Changes in Vascular and Neural Fibers Induced by Subretinal Fluid Excluding the Peripapillary Region in Patients with Chronic Central Serous Chorioretinopathy
Abstract
1. Introduction
2. Materials and Methods
2.1. Assessment of Retinal Nerve Fiber Layer Thickness and Radial Peripapillary Capillary Density
2.2. Statistical Analyses
3. Results
3.1. Demographic and Clinical Characteristics of Participants
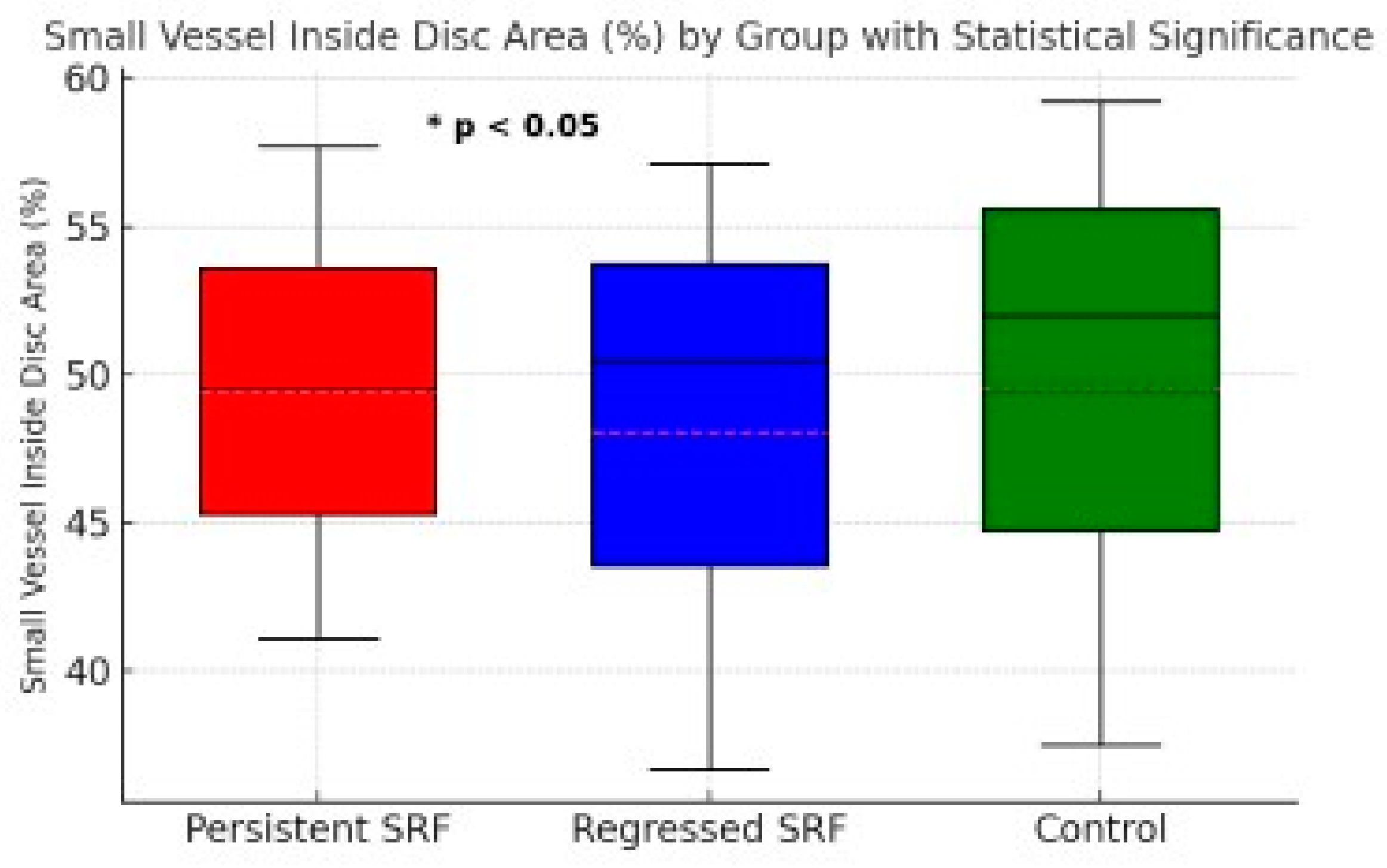
3.2. Radial Peripapillary Capillary Vessel Density (RPC VD)
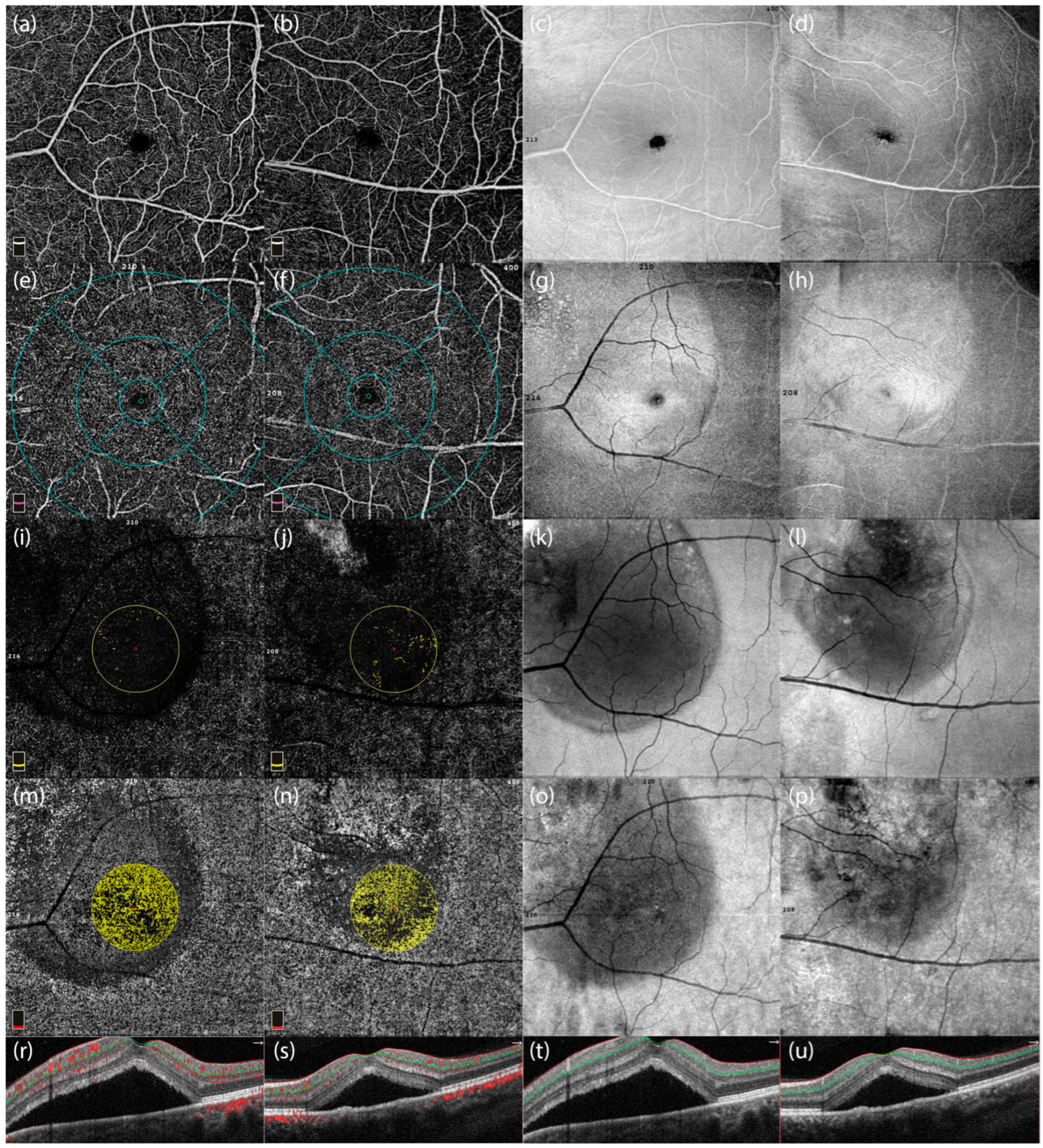
- Subretinal fluid: The visualization demonstrates an extensive fluid pocket, which extends into the peripapillary area, directly impacting the optic nerve head.
- Structural changes: The image highlights how the presence of fluid distorts the normal retinal architecture, including potential thinning of the surrounding neural layers and vascular structures.
- Clinical relevance: This degree of peripapillary involvement emphasizes the importance of early detection and management in CSCR to prevent long-term complications such as optic nerve compression or irreversible damage.

| CSCR Patients with Regressed SRF Median (Min–Max) n: 27 | CSCR Patients with SRF Median (Min–Max) n: 38 | Control Median (Min–Max) n: 65 | p Value | ||
|---|---|---|---|---|---|
| RNFL (µ) | Peripapillary | 112.00 (97.00–145.00) | 117.00 (92.00–151.00) | 113.00 (98.00–140.00) | 0.242 |
| Superior | 136.00 (114.00–239.00) | 132.00 (101.00–175.00) | 130.00 (105.00–165.00) | 0.489 | |
| Inferior | 50.20 (48.00–72.00) | 51.90 (45.00–88.00) | 50.30 (47.00–55.00) | 0.003 | |
| Temporal | 148.00 (119.00–206.00) | 146.00 (123.00–196.00) | 142.00 (114.00–190.00) | 0.609 | |
| Nasal | 74.00 (50.00–89.00) | 78.00 (60.00–115.00) | 75.00 (58.00–113.00) | 0.014 | |
| RPC VDs (%) | Small Vessel Whole Area | 106.00 (48.30–162.00) | 102.00 (46.80–164.00) | 100.00 (71.00–152.00) | 0.599 |
| Small Vessel Inside Disc Area | 50.40 (36.70–57.10) | 49.50 (41.10–57.70) | 52.00 (37.50–59.20) | 0.021 | |
| Small Vessel Peripapillary Area | 53.10 (48.40–58.60) | 52.55 (45.30–57.50) | 52.90 (49.40–57.80) | 0.331 | |
| All Vessel Whole Area | 56.90 (54.10–61.00) | 57.05 (51.50–60.90) | 57.30 (52.70–61.00) | 0.987 | |
| All Vessel Inside Disc Area | 61.30 (50.40–67.40) | 59.70 (47.90–66.80) | 61.40 (47.10–67.90) | 0.090 | |
| All Vessel Peripapillary Area | 59.80 (55.80–64.10) | 59.25 (45.80–63.50) | 59.20 (56.20–63.80) | 0.439 | |
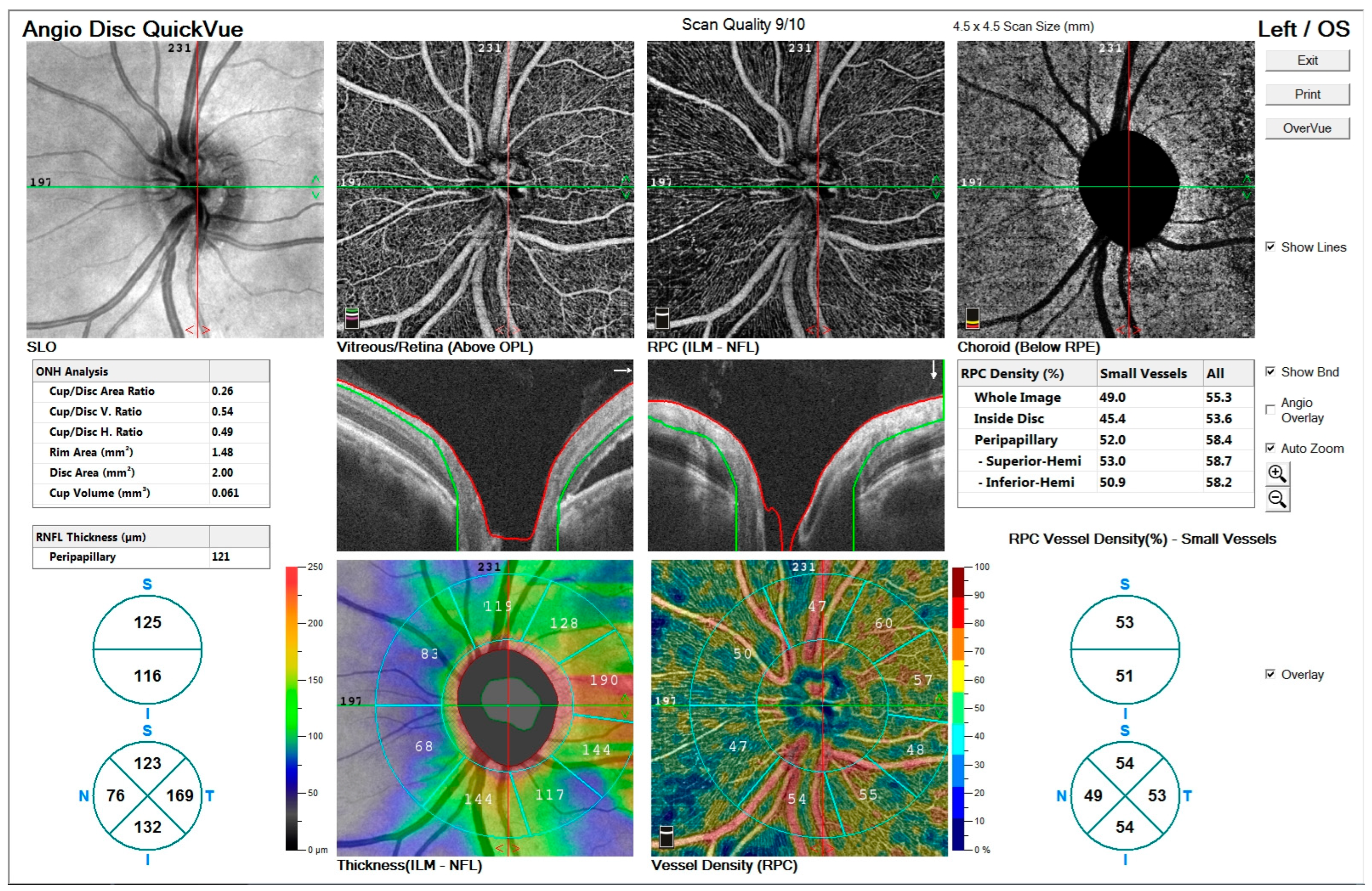
- Figure 3’s Top row: Enface views highlight the vascular structure in different retinal layers, including the vitreous/retina (above OPL), radial peripapillary capillaries (ILM-NFL), and choroid (below RPE).
- Figure 3’s Middle row: ONH analysis provides detailed measurements of cup/disc area ratio, rim area, disc area, and cup volume. Retinal nerve fiber layer (RNFL) thickness and vessel density maps are shown, illustrating structural and vascular integrity.
- Figure 3’s Bottom row: RNFL thickness map (left) and vessel density map (right) offer quantitative insights into the peripapillary region’s structural and vascular changes.
3.3. Radial Nerve Fiber Layer Thickness (RNFL)
3.4. Correlation Analyses
4. Discussion
5. Study Limitations and the Need for Functional Correlates
6. Recommendations for Future Research Directions
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Daruich, A.; Matet, A.; Dirani, A.; Bousquet, E.; Zhao, M.; Farman, N.; Jaisser, F.; Behar-Cohen, F. Central serous chorioretinopathy: Recent findings and new physiopathology hypothesis. Prog. Retin. Eye Res. 2015, 48, 82–118. [Google Scholar] [CrossRef]
- Liew, G.; Quin, G.; Gillies, M.; Fraser-Bell, S. Central serous chorioretinopathy: A review of epidemiology and pathophysiology. Clin. Exp. Ophthalmol. 2013, 41, 201–214. [Google Scholar] [CrossRef] [PubMed]
- Gemenetzi, M.; De Salvo, G.; Lotery, A.J. Central serous chorioretinopathy: An update on pathogenesis and treatment. Eye 2010, 24, 1743–1756. [Google Scholar] [CrossRef] [PubMed]
- Nicholson, B.; Noble, J.; Forooghian, F.; Meyerle, C. Central serous chorioretinopathy: Update on pathophysiology and treatment. Surv. Ophthalmol. 2013, 58, 103–126. [Google Scholar] [CrossRef]
- Goto, K.; Miki, A.; Yamashita, T.; Araki, S.; Takizawa, G.; Ieki, Y.; Kiryu, J. Retinal nerve fiber layer and peripapillary capillary density reduction detected using optical coherence tomography enface images and angiography in optic tract syndrome. J. Neuro-Ophthalmol. 2019, 39, 253–256. [Google Scholar] [CrossRef] [PubMed]
- Cunha-Vaz, J. Mechanisms of retinal fluid accumulation and blood-retinal barrier breakdown. Ophthalmologica 2017, 238, 11–20. [Google Scholar] [CrossRef]
- Wang, M.; Munch, I.C.; Hasler, P.W.; Prünte, C.; Larsen, M. Central serous chorioretinopathy. Acta Ophthalmol. 2008, 86, 126–145. [Google Scholar] [CrossRef] [PubMed]
- Imai, A.; Toriyama, Y.; Iesato, Y.; Hirano, T.; Murata, T. En face swept-source optical coherence tomography detecting thinning of inner retinal layers as an indicator of capillary nonperfusion. Eur. J. Ophthalmol. 2014, 25, 153–158. [Google Scholar] [CrossRef] [PubMed]
- Jirarattanasopa, P.; Ooto, S.; Tsujikawa, A.; Yamashiro, K.; Hangai, M.; Hirata, M.; Matsumote, A.; Yoshimura, N. Assessment of macularchoroidalthicknessbyopticalcoherencetomographyandangiographicchanges in central serous chorioretinopathy. Ophthalmology 2012, 119, 1666–1678. [Google Scholar] [CrossRef] [PubMed]
- Jain, M.; Mohan, S.; van Dijk, E.H.C. Central serous chorioretinopathy: Pathophysiology, systemic associations, and a novel etiological classification. Taiwan. J. Ophthalmol. 2022, 12, 381–393. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Lim, C.Z.F.; Chhablani, J.; Wong, Y.M. Central serous chorioretinopathy: Updates in the pathogenesis, diagnosis and therapeutic strategies. Eye Vis. 2023, 10, 33. [Google Scholar] [CrossRef] [PubMed]
- Semeraro, F.; Morescalchi, F.; Russo, A.; Gambicorti, E.; Pilotto, A.; Parmeggiani, F.; Bartollino, S.; Costagliola, C. Central serous chorioretinopathy: Pathogenesis and management. Clin. Ophthalmol. 2019, 13, 2341–2352. [Google Scholar] [CrossRef] [PubMed]
- Pujari, A.; Surve, A.; Azad, S.V.; Beniwal, A.; Vikas, S.J.; Chawla, R.; Sachan, A.; Kumar, A.; Kumar, A. Optical coherence tomography angiography in central serous chorioretinopathy: The current clinical role and future perspectives. Surv. Ophthalmol. 2021, 67, 68–82. [Google Scholar] [CrossRef]
- Regatieri, C.V.; Novais, E.A.; Branchini, L.; Adhi, M.; Cole, E.D.; Louzada, R.N.; Lane, M.; Reichel, E.; Duker, J.S. Choroidal thickness in older patients with central serous chorioretinopathy. Int. J. Retin. Vitr. 2016, 2, 22. [Google Scholar] [CrossRef] [PubMed]
- Montero, J.A.; Ruiz-Moreno, J.M. Optical coherence tomography characterisation of idiopathic central serous chorioretinopathy. Br. J. Ophthalmol. 2005, 89, 562–564. [Google Scholar] [CrossRef]
- Sikorski, B.L.; Bukowska, D.; Kałuzný, J.; Kowalczyk, A.; Wojtkowski, M. Restoration of photoreceptor structure and function in nonischaemic central retinal vein occlusion. Acta Ophthalmol. 2012, 91, e163–e165. [Google Scholar] [CrossRef]
- Reich, M.; Boehringer, D.; Rothaus, K.; Çakır, B.; Bucher, F.; Daniel, M.C.; Láng, S.; Lagrèze, W.A.; Agostini, H.; Lange, C. Swept-source optical coherence tomography angiography alleviates shadowing artifacts caused by subretinal fluid. Int. Ophthalmol. 2020, 40, 2007–2016. [Google Scholar] [CrossRef]
- Lavinsky, D.; Lavinsky, F. Central serous chorioretinopathy: A review. Curr. Ophthalmol. Rep. 2017, 5, 141–147. [Google Scholar]
- Liew, G.; Quin, G.; Gillies, M.; Fraser-Bell, S. Central serous chorioretinopathy: Epidemiology, pathophysiology, and clinical management. Surv. Ophthalmol. 2020, 65, 78–88. [Google Scholar]
- Breukink, M.B.; Dingemans, A.J.; Hollander, A.I.D.; Keunen, J.E.; MacLaren, R.E.; Fauser, S.; Querques, G.; Hoyng, C.B.; Downes, S.M.; Boon, C.J.F. Chronic central serous chorioretinopathy: Long-term follow-up and vision-related quality of life. Clin. Ophthalmol. 2016, 11, 39–46. [Google Scholar] [CrossRef] [PubMed]
- Shimada, Y.; Imai, D.; Ota, Y.; Kanai, K.; Mori, K.; Murayama, K.; Yoneya, S. Retinal adaptability loss in serous retinal detachment with central serous chorioretinopathy. Investig. Ophthalmol. Vis. Sci. 2010, 51, 3210–3215. [Google Scholar] [CrossRef][Green Version]
- Reznicek, L.; Cserhati, S.; Seidensticker, F.; Liegl, R.; Kampik, A.; Ulbig, M.; Neubauer, A.S.; Kernt, M. Functional and morphological changes in diabetic macular edema over the course of anti-vascular endothelial growth factor treatment. Acta Ophthalmol. 2013, 91, e464–e466. [Google Scholar] [CrossRef] [PubMed]
- Rasheed, M.A.; Goud, A.; Mohamed, A.; Vupparaboina, K.K.; Chhablani, J. Change in choroidal vascularity in acute central serous chorioretinopathy. Indian J. Ophthalmol. 2018, 66, 530–534. [Google Scholar] [PubMed]
- Kim, K.T.; Chae, J.B.; Lee, S.; Seo, E.J.; Kim, D.Y. Analyses of the effects of persistent subretinal fluid on visual/anatomic outcomes according to the type of macular neovascularization during the relaxed treat-and-extend protocol in age-related macular degeneration patients. BMC Ophthalmol. 2021, 21, 294. [Google Scholar] [CrossRef]
- Berni, A.; Oakley, J.D.; Dolz-Marco, R.; Reibaldi, M.; Bandello, F.; Borrelli, E. Topographical quantification of retinal fluid in type 3 MNV and associations with short-term visual outcomes. Sci. Rep. 2021, 11, 13845. [Google Scholar] [CrossRef] [PubMed]
- Ferrara, D.; Calucci, D.; Oréfice, J.L.; Magalhães, É.P.; Oréfice, F.; Costa, R. Proposed physiopathological mechanisms and potential therapeutic targets for central serous chorioretinopathy. Expert Rev. Ophthalmol. 2008, 3, 553–565. [Google Scholar] [CrossRef]
- Lim, J.S.; Moon, C.; Lee, J. Subretinal fluid disturbs the retinal venous blood flow in central serous chorioretinopathy. Sci. Rep. 2022, 12, 8865. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Li, Y.; Meng, X.; Li, F.; Chen, Y. The effect of chronic subretinal fluid on peripapillary vasculature in central serous chorioretinopathy: An optical coherence tomography angiography study. Eye 2022, 36, 1974–1980. [Google Scholar] [CrossRef]
- Mohabati, D.; van Rijssen, T.J.; van Dijk, E.H.C.; Luyten, G.P.M.; Missotten, T.; Hoyng, C.C.B.; Yzer, S.; Boon, C.J.F. Clinical characteristics and long-term visual outcome of severe phenotypes of chronic central serous chorioretinopathy. Clin. Ophthalmol. 2018, 12, 1061–1070. [Google Scholar] [CrossRef] [PubMed]
- Gawęcki, M.; Jaszczuk-Maciejewska, A.; Jurska-Jaśko, A.; Kneba, M.; Grzybowski, A. Impairment of visualacuityandretinalmorphologyfollowingresolvedchroniccentralserouschorioretinopathy. BMC Ophthalmol. 2019, 19, 1171. [Google Scholar] [CrossRef]
- Steinberg, J.S.; Saßmannshausen, M.; Fleckenstein, M.; Fimmers, R.; Ishibashi, T.; Holz, F.G.; Schmitz-Valckenberg, S. Correlation of partialouterretinalthicknesswithscotopicandmesopicfundus-controlledperimetry in patients with reticular drusen. Am. J. Ophthalmol. 2016, 168, 52–61. [Google Scholar] [CrossRef]
- Choi, S.S.; Zawadzki, R.J.; Keltner, J.L.; Werner, J.S. Changes in cellular structures revealed by ultra-high-resolution retinal imaging in optic neuropathies. Investig. Ophthalmol. Vis. Sci. 2008, 49, 2103. [Google Scholar] [CrossRef]
- Diagnosing and Managing Central Serous Chorioretinopathy. (2023, February 6). American Academy of Ophthalmology. Available online: https://www.aao.org/eyenet/article/diagnosing-managing-central-serous-chorioretinopat (accessed on 2 December 2024).
- Han, K.J.; Kim, H.J.; Woo, J.M.; Min, J.K. Comparison of retinal layer thickness and capillary vessel density in thepatientswithspontaneouslyresolvedacutecentralserouschorioretinopathy. J. Clin. Med. 2020, 10, 45. [Google Scholar] [CrossRef] [PubMed]
- Abouammoh, M.A. Advances in the treatment of central serous chorioretinopathy. Saudi J. Ophthalmol. 2015, 29, 278–286. [Google Scholar] [CrossRef] [PubMed]
- Yavuz, S.; Balsak, S.; Karahan, M.; Dursun, B. Investigating the efficacy and safety of oral spironolactone in patients with central serous chorioretinopathy. J. Français D’ophtalmologie 2021, 44, 13–23. [Google Scholar] [CrossRef] [PubMed]
| CSCR Patients with Regressed * SRF Median (Min–Max) n: 27 | CSCR Patients with SRF Median (Min–Max) n: 38 | p Value | |
|---|---|---|---|
| Age (year) | 47.00 (31.00–78.00) | 45.00 (32.00–78.00) | 0.457 |
| Vision (LogMar) | 0.045 (0.154–0.00) | 1.301 (1.00–0.096) | <0.001 |
| IOP (mmHg) | 14.00 (11.00–20.00) | 13.00 (9.00–20.00) | 0.469 |
| p | P1 * | P2 * | P3 * | |
|---|---|---|---|---|
| RNFL Inferior Thickness (µ) | 0.003 | 1 | 0.003 | 0.054 |
| RNFL Nasal Thickness (µ) | 0.014 | 1 | 0.023 | 0.053 |
| RPC Small Vessel Inside Disc Area VDs (%) | 0.021 | 0.538 | 0.019 | 0.940 |
| RNFL Inferior Thickness (µ) | RNFL Nasal Thickness (µ) | ||||
|---|---|---|---|---|---|
| p | r † | p | r | ||
| RPC VDs (%) | Small Vessel Whole Area | 0.206 | −0.160 | 0.048 * | −0.249 |
| Small Vessel Inside Disc Area | 0.393 | −0.109 | 0.014 * | −0.306 | |
| Small Vessel Peripapillary Area | 0.015 * | 0.300 | 0.434 | −0.099 | |
| All Vessel Whole Area | 0.003 ** | 0.358 | 0.498 | −0.085 | |
| All Vessel Inside Disc Area | 0.431 | −0.099 | 0.061 | −0.233 | |
| All Vessel Peripapillary Area | 0.006 ** | 0.335 | 0.835 | −0.026 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kızıldağ Özbay, E.; Sabancı, Ş.; Küçük, M.F.; Erol, M.K. Quantitative Changes in Vascular and Neural Fibers Induced by Subretinal Fluid Excluding the Peripapillary Region in Patients with Chronic Central Serous Chorioretinopathy. Diagnostics 2025, 15, 174. https://doi.org/10.3390/diagnostics15020174
Kızıldağ Özbay E, Sabancı Ş, Küçük MF, Erol MK. Quantitative Changes in Vascular and Neural Fibers Induced by Subretinal Fluid Excluding the Peripapillary Region in Patients with Chronic Central Serous Chorioretinopathy. Diagnostics. 2025; 15(2):174. https://doi.org/10.3390/diagnostics15020174
Chicago/Turabian StyleKızıldağ Özbay, Esra, Şenol Sabancı, Mehmet Fatih Küçük, and Muhammet Kazım Erol. 2025. "Quantitative Changes in Vascular and Neural Fibers Induced by Subretinal Fluid Excluding the Peripapillary Region in Patients with Chronic Central Serous Chorioretinopathy" Diagnostics 15, no. 2: 174. https://doi.org/10.3390/diagnostics15020174
APA StyleKızıldağ Özbay, E., Sabancı, Ş., Küçük, M. F., & Erol, M. K. (2025). Quantitative Changes in Vascular and Neural Fibers Induced by Subretinal Fluid Excluding the Peripapillary Region in Patients with Chronic Central Serous Chorioretinopathy. Diagnostics, 15(2), 174. https://doi.org/10.3390/diagnostics15020174






