Anatomic Variations Important for Dental Implantation in the Mandible—A Systematic Review
Abstract
1. Introduction
- Influence of the mandibular canal and its morphometric characteristics on the dental implant placement;
- Influence of the mental foramen and its morphometric characteristics on the dental implant placement;
- Influence of the incisive canal of the mandible and its morphometric characteristics on the dental implant placement;
- Influence of lingual foramina and lingual canals and their morphometric characteristics on the dental implant placement;
- Influence of mandibular concavity and its morphometric characteristics on the dental implant placement.
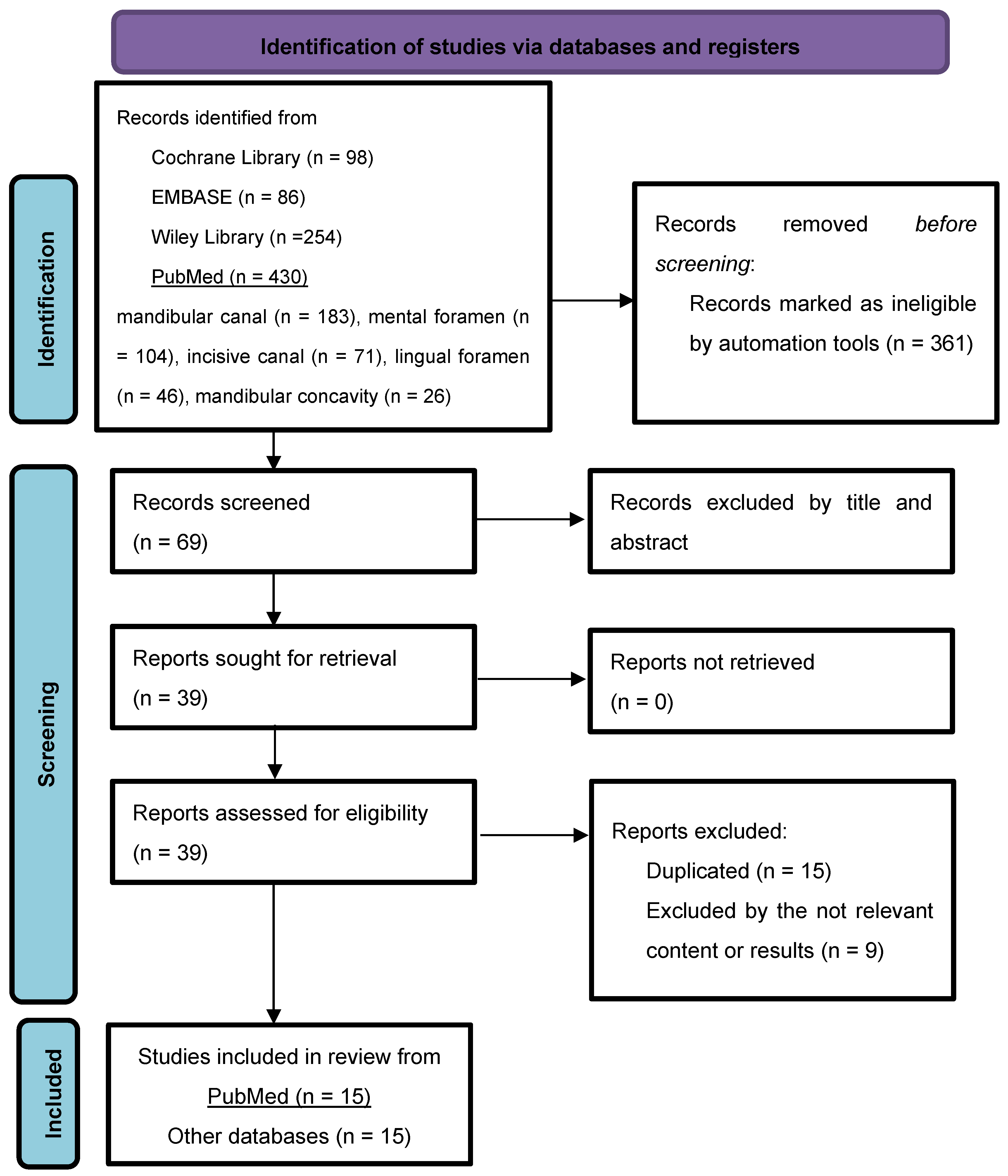
2. Materials and Methods
2.1. Eligibility Criteria
2.2. Information Source
2.3. Search Strategy and Selection Process
2.4. Study Eligibility and Quality Assessment
- Were the criteria for inclusion in the sample clearly defined?
- Were the study subjects and the setting described in detail?
- Was the exposure measured validly and reliably?
- Were objective, standard criteria used for measurement of the condition?
- Were confounding factors identified?
- Were strategies to deal with confounding factors stated?
- Were the outcomes measured validly and reliably?
- Was appropriate statistical analysis used?
2.5. Data Items
2.5.1. Outcomes of Interest
2.5.2. Population
2.5.3. Intervention
2.6. Effect Measures
2.7. Risk of Bias of Included Articles
2.8. Synthesis Method
3. Results
3.1. Study Characteristics
3.2. Results of Individual Studies
3.2.1. Inferior Alveolar Canal (IAC)
3.2.2. Mental Foramen (MF) and Anterior Loop (AL)
3.2.3. Lingual Foramina/Lingual Canal (LF/LC)
3.2.4. Mandibular Incisive Canal (MIC)
3.2.5. Mandibular Concavity
4. Discussion
4.1. Limitations of the Evidence Included in This Review
4.2. Implications of the Results for Practice, Policy, and Future Research
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Prasad, D.; Shetty, M. Anatomical Considerations in Implant Selection and Positioning. Int. J. Oral Implant. Clin. Res. 2013, 4, 24–29. [Google Scholar] [CrossRef]
- Hong, D.G.K.; Oh, J.H. Recent advances in dental implants. Maxillofac. Plast. Reconstr. Surg. 2017, 39, 33. [Google Scholar] [CrossRef]
- La Monaca, G.; Pranno, N.; Annibali, S.; Di Carlo, S.; Pompa, G.; Cristalli, M.P. Immediate flapless full-arch rehabilitation of edentulous jaws on 4 or 6 implants according to the prosthetic-driven planning and guided implant surgery: A retrospective study on clinical and radiographic outcomes up to 10 years of follow-up. Clin. Implant. Dent. Relat. Res. 2022, 24, 831–844. [Google Scholar] [CrossRef]
- Alzahrani, K.M. Implant Bio-mechanics for Successful Implant Therapy: A Systematic Review. J. Int. Soc. Prev. Community Dent. 2020, 10, 700–714. [Google Scholar] [CrossRef]
- Sailer, I.; Karasan, D.; Todorovic, A.; Ligoutsikou, M.; Pjetursson, B.E. Prosthetic failures in dental implant therapy. Periodontol. 2000 2022, 88, 130–144. [Google Scholar] [CrossRef]
- Jamil, F.A.; Mohammed, J.A.; Hasan, T.A.; Rzoqi, M.G. The reliability of surgeons to avoid traumatic insertion of dental implants into high-risk regions: A panoramic radiograph study. BMC Oral Health 2020, 20, 96. [Google Scholar] [CrossRef]
- Lurie, A.G. Doses, Benefits, Safety, and Risks in Oral and Maxillofacial Diagnostic Imaging. Health Phys. 2019, 116, 163–169. [Google Scholar] [CrossRef]
- Awad, M.F.; Karout, L.; Arnous, G.; Rawashdeh, M.A.; Hneiny, L.; Saade, C. A systematic review on the current status of adult diagnostic reference levels in head, chest and abdominopelvic Computed Tomography. J. Radiol. Prot. 2020, 40, R71–R98. [Google Scholar] [CrossRef] [PubMed]
- Kofler, B.; Jenetten, L.; Runge, A.; Degenhart, G.; Fischer, N.; Hörmann, R.; Steurer, M.; Widmann, G. ALADA Dose Optimization in the Computed Tomography of the Temporal Bone: The Diagnostic Potential of Different Low-Dose CT Protocols. Diagnostics 2021, 11, 1894. [Google Scholar] [CrossRef]
- Tallarico, M. Computerization and Digital Workflow in Medicine: Focus on Digital Dentistry. Materials 2020, 13, 2172. [Google Scholar] [CrossRef] [PubMed]
- Juodzbalys, G.; Wang, H.L.; Sabalys, G. Anatomy of Mandibular Vital Structures. Part II: Mandibular Incisive Canal, Mental Foramen and Associated Neurovascular Bundles in Relation with Dental Implantology. J. Oral Maxillofac. Res. 2010, 1, e3. [Google Scholar] [CrossRef]
- Kim, S.T.; Hu, K.S.; Song, W.C.; Kang, M.K.; Park, H.D.; Kim, H.J. Location of the mandibular canal and the topography of its neurovascular structures. J. Craniofac. Surg. 2009, 20, 936–939. [Google Scholar] [CrossRef]
- Barbosa, D.A.F.; de Mendonça, D.S.; de Carvalho, F.S.R.; Kurita, L.M.; de Barros Silva, P.G.; Neves, F.S.; Costa, F.W.G. Systematic review and meta-analysis of lingual foramina anatomy and surgical-related aspects on cone-beam computed tomography: A PROSPERO-registered study. Oral Radiol. 2022, 38, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Barbosa, D.A.; Kurita, L.M.; Pimenta, A.V.; Teixeira, R.C.; Silva, P.G.; Ribeiro, T.R.; de Melo, D.P.; Costa, F.W.G. Mandibular incisive canal-related prevalence, morphometric parameters, and implant placement implications: A multicenter study of 847 CBCT scans. Med. Oral Patol. Oral Cir. Bucal 2020, 25, e337–e345. [Google Scholar] [CrossRef]
- Del Castillo-Pardo de Vera, J.L.; López-Arcas Calleja, J.M.; Burgueño-García, M. Hematoma of the floor of the mouth and airway obstruction during mandibular dental implant placement: A case report. Oral Maxillofac. Surg. 2008, 12, 223–226. [Google Scholar] [CrossRef]
- Trost, M.; Mundt, T.; Biffar, R.; Heinemann, F. The lingual foramina, a potential risk in oral surgery. A retrospective analysis of location and anatomic variability. Ann. Anat. 2020, 231, 151515. [Google Scholar] [CrossRef] [PubMed]
- Kessler, A.T.; Bhatt, A.A. Review of the Major and Minor Salivary Glands, Part 1: Anatomy, Infectious, and Inflammatory Processes. J. Clin. Imaging Sci. 2018, 8, 47. [Google Scholar] [CrossRef]
- Nickenig, H.J.; Wichmann, M.; Eitner, S.; Zöller, J.E.; Kreppel, M. Lingual concavities in the mandible: A morphological study using cross-sectional analysis determined by CBCT. J. Craniomaxillofac. Surg. 2015, 43, 254–259. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ 2009, 339, b2700. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Syst. Rev. 2021, 10, 89. [Google Scholar] [CrossRef]
- Moola, S.; Munn, Z.; Tufanaru, C.; Aromataris, E.; Sears, K.; Sfetcu, R.; Currie, M.; Lisy, K.; Qureshi, R.; Mattis, P.; et al. Systematic reviews of etiology and risk (2020). In JBI Manual for Evidence Synthesis; Aromataris, E., Lockwood, C., Porritt, K., Pilla, B., Jordan, Z., Eds.; JBI: Los Angeles, CA, USA, 2024; Available online: https://synthesismanual.jbi.global (accessed on 1 December 2024).
- Sterne, J.A.C.; Hernán, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef] [PubMed]
- Risk of Bias Tools, Version 2 of the ROBINS-I Tool. Available online: https://sites.google.com/site/riskofbiastool/welcome/robins-i-v2 (accessed on 9 December 2024).
- Cooke, A.; Smith, D.; Booth, A. Beyond PICO: The SPIDER tool for qualitative evidence synthesis. Qual Health Res. 2012, 22, 1435–1443. [Google Scholar] [CrossRef]
- Aljarbou, F.A.; Aldosimani, M.; Althumairy, R.I.; Alhezam, A.A.; Aldawsari, A.I. An analysis of the first and second mandibular molar roots proximity to the inferior alveolar canal and cortical plates using cone beam computed tomography among the Saudi population. Saudi Med. J. 2019, 40, 189–194. [Google Scholar] [CrossRef] [PubMed]
- Sekerci, A.E.; Sisman, Y.; Payveren, M.A. Evaluation of location and dimensions of mandibular lingual foramina using cone-beam computed tomography. Surg. Radiol. Anat. 2014, 36, 857–864. [Google Scholar] [CrossRef]
- Bayrak, S.; Demirturk-Kocasarac, H.; Yaprak, E.; Ustaoglu, G.; Noujeim, M. Correlation between the visibility of submandibular fossa and mandibular canal cortication on panoramic radiographs and submandibular fossa depth on CBCT. Med. Oral Patol. Oral Cir. Bucal 2018, 23, e105–e111. [Google Scholar] [CrossRef]
- Fouda, S.M.; Ellakany, P.; Madi, M.; Zakaria, O.; Al-Harbi, F.A.; El Tantawi, M. Do Morphological Changes in the Anterior Mandibular Region Interfere with Standard Implant Placement? A Cone Beam Computed Tomographic Cross-Sectional Study. Sci. World J. 2020, 2020, 8861301. [Google Scholar] [CrossRef] [PubMed]
- Genç, T.; Duruel, O.; Kutlu, H.B.; Dursun, E.; Karabulut, E.; Tözüm, T.F. Evaluation of anatomical structures and variations in the maxilla and the mandible before dental implant treatment. Dent. Med. Probl. 2018, 55, 233–240. [Google Scholar] [CrossRef]
- Alqutaibi, A.Y.; Alassaf, M.S.; Elsayed, S.A.; Alharbi, A.S.; Habeeb, A.T.; Alqurashi, M.A.; Albulushi, K.A.; Elboraey, M.O.; Alsultan, K.; Mahmoud, I.I. Morphometric Analysis of the Midline Mandibular Lingual Canal and Mandibular Lingual Foramina: A Cone Beam Computed Tomography (CBCT) Evaluation. Int. J. Environ. Res. Public. Health 2022, 19, 16910. [Google Scholar] [CrossRef]
- Shen, Y.W.; Chang, W.C.; Huang, H.L.; Tsai, M.T.; Fuh, L.J.; Hsu, J.T. Assessment of the Retromolar Canal in Taiwan Subpopulation: A Cross-Sectional Cone-Beam Computed Tomography Study in a Medical Center. Tomography 2021, 7, 219–227. [Google Scholar] [CrossRef] [PubMed]
- Surathu, N.; Flanagan, D.; Surathu, N.; Nittla, P.P. A CBCT Assessment of the Incidence and Location of the Lingual Foramen in the Anterior Mandible. J. Oral Implantol. 2022, 48, 92–98. [Google Scholar] [CrossRef]
- Sanchez-Perez, A.; Boix-Garcia, P.; Lopez-Jornet, P. Cone-Beam CT Assessment of the Position of the Medial Lingual Foramen for Dental Implant Placement in the Anterior Symphysis. Implant. Dent. 2018, 27, 43–48. [Google Scholar] [CrossRef] [PubMed]
- Vasegh, Z.; Safi, Y.; Amid, R.; Ahsaie, M.G.; Amiri, M.J.; Minooei, Z. Quantitative Evaluation of Bone-Related Factors at the Implant Site by Cone-Beam Computed Tomography. J. Long. Term. Eff. Med. Implant. 2022, 32, 33–43. [Google Scholar] [CrossRef]
- Gümüşok, M.; Akarslan, Z.Z.; Başman, A.; Üçok, Ö. Evaluation of accessory mental foramina morphology with cone-beam computed tomography. Niger. J. Clin. Pract. 2017, 20, 1550–1554. [Google Scholar] [CrossRef] [PubMed]
- Wong, S.K.; Patil, P.G. Measuring anterior loop length of the inferior alveolar nerve to estimate safe zone in implant planning: A CBCT study in a Malaysian population. J. Prosthet. Dent. 2018, 120, 210–213. [Google Scholar] [CrossRef]
- Sener, E.; Onem, E.; Akar, G.C.; Govsa, F.; Ozer, M.A.; Pinar, Y.; Mert, A.; Sen, B.G.B. Anatomical landmarks of mandibular interforaminal region related to dental implant placement with 3D CBCT: Comparison between edentulous and dental mandibles. Surg. Radiol. Anat. 2018, 40, 615–623. [Google Scholar] [CrossRef] [PubMed]
- Koivisto, T.; Chiona, D.; Milroy, L.L.; McClanahan, S.B.; Ahmad, M.; Bowles, W.R. Mandibular canal location: Cone-beam computed tomography examination. J. Endod. 2016, 42, 1018–1021. [Google Scholar] [CrossRef]
- Yang, X.W.; Zhang, F.F.; Li, Y.H.; Wei, B.; Gong, Y. Characteristics of intrabony nerve canals in mandibular interforaminal region by using cone-beam computed tomography and a recommendation of safe zone for implant and bone harvesting. Clin. Implant. Dent. Relat. Res. 2017, 19, 530–538. [Google Scholar] [CrossRef] [PubMed]
- Yoon, T.Y.; Patel, M.; Michaud, R.A.; Manibo, A.M. Cone Beam Computerized Tomography Analysis of the Posterior and Anterior Mandibular Lingual Concavity for Dental Implant Patients. J. Oral Implantol. 2017, 43, 12–18. [Google Scholar] [CrossRef]
- Zhang, W.; Tullis, J.; Weltman, R. Cone Beam Computerized Tomography Measurement of Alveolar Ridge at Posterior Mandible for Implant Graft Estimation. J. Oral Implantol. 2015, 41, e231–e237. [Google Scholar] [CrossRef] [PubMed]
- Marimuthu, T.; Krithika, C.; Devadoss, P.; Kumar, S.M. Prevalence and measurement of anterior loop of the mandibular canal using CBCT: A cross sectional study. Clin. Implant. Dent. Relat. Res. 2018, 20, 531–534. [Google Scholar] [CrossRef]
- Lu, C.I.; Won, J.; Al-Ardah, A.; Santana, R.; Rice, D.; Lozada, J. Assessment of the Anterior Loop of the Mental Nerve Using Cone Beam Computerized Tomography Scan. J. Oral Implantol. 2015, 41, 632–639. [Google Scholar] [CrossRef] [PubMed]
- Raju, N.; Zhang, W.; Jadhav, A.; Ioannou, A.; Eswaran, S.; Weltman, R. Cone-Beam Computed Tomography Analysis of the Prevalence, Length, and Passage of the Anterior Loop of the Mandibular Canal. J. Oral Implantol. 2019, 45, 463–468. [Google Scholar] [CrossRef] [PubMed]
- Vujanovic-Eskenazi, A.; Valero-James, J.M.; Sánchez-Garcés, M.A.; Gay-Escoda, C. A retrospective radiographic evaluation of the anterior loop of the mental nerve: Comparison between panoramic radiography and cone beam computerized tomography. Med. Oral Patol. Oral Cir. Bucal 2015, 20, e239–e245. [Google Scholar] [CrossRef] [PubMed]
- Kavarthapu, A.; Thamaraiselvan, M. Assessing the variation in course and position of inferior alveolar nerve among south Indian population: A cone beam computed tomographic study. Indian J. Dent. Res. 2018, 29, 405–409. [Google Scholar] [CrossRef] [PubMed]
- He, X.; Jiang, J.; Cai, W.; Pan, Y.; Yang, Y.; Zhu, K.; Zheng, Y. Assessment of the appearance, location and morphology of mandibular lingual foramina using cone beam computed tomography. Int. Dent. J. 2016, 66, 272–279. [Google Scholar] [CrossRef] [PubMed]
- Çitir, M.; Gunduz, K.; Kasap, P. Investigation the anterior mandibular lingual concavity by using cone-beam computed tomography. Folia Morphol. 2021, 80, 916–922. [Google Scholar] [CrossRef]
- Kong, Z.L.; Wang, G.G.; Liu, X.Y.; Ye, Z.Y.; Xu, D.Q.; Ding, X. Influence of bone anatomical morphology of mandibular molars on dental implant based on CBCT. BMC Oral Health 2021, 21, 528. [Google Scholar] [CrossRef] [PubMed]
- Tsai, Y.-W.C.; Huang, R.-Y.; Cheng, C.-D.; Cheng, W.-C.; Cochran, D.L.; Nguyen, T.T.; Shieh, Y.-S.; Lin, F.-G.; Sung, C.-E. Risk assessment of labial bone perforation in the anterior mandibular region: A virtual immediate implant placement study. Int. J. Implant. Dent. 2021, 7, 68. [Google Scholar] [CrossRef]
- Alqutaibi, A.Y.; Alghauli, M.A.; Aboalrejal, A.; Mulla, A.K.; Almohammadi, A.A.; Aljayyar, A.W.; Alharbi, S.O.; Almuzaini, E.S.; Alsaeedi, A.K.; Arabi, L.F.; et al. Quantitative and qualitative 3D analysis of mandibular lingual concavities: Implications for dental implant planning in the posterior mandible. Clin. Exp. Dent. Res. 2024, 10, e858. [Google Scholar] [CrossRef] [PubMed]
- Kanewoff, E.; Alhallak, R.; de Carvalho Machado, V.; Chrcanovic, B.R. Immediate implant placement in the anterior mandible: A cone beam computed tomography study. BMC Oral Health 2024, 24, 393. [Google Scholar] [CrossRef]
- Gu, L.; Zhu, C.; Chen, K.; Liu, X.; Tang, Z. Anatomic study of the position of the mandibular canal and corresponding mandibular third molar on cone-beam computed tomography images. Surg. Radiol. Anat. 2018, 40, 609–614. [Google Scholar] [CrossRef] [PubMed]
- Vasiljevic, M.; Selakovic, D.; Rosic, G.; Stevanovic, M.; Milanovic, J.; Arnaut, A.; Milanovic, P. Anatomical Factors of the Anterior and Posterior Maxilla Affecting Immediate Implant Placement Based on Cone Beam Computed Tomography Analysis: A Narrative Review. Diagnostics 2024, 14, 1697. [Google Scholar] [CrossRef]
- Pavlovic, Z.R.; Milanovic, P.; Vasiljevic, M.; Jovicic, N.; Arnaut, A.; Colic, D.; Petrovic, M.; Stevanovic, M.; Selakovic, D.; Rosic, G. Assessment of Maxillary Molars Interradicular Septum Morphological Characteristics as Criteria for Ideal Immediate Implant Placement-The Advantages of Cone Beam Computed Tomography Analysis. Diagnostics 2022, 12, 1010. [Google Scholar] [CrossRef]
- Hoshi, K.; Ikebe, T.; Ota, Y.; Kishimoto, H.; Kurata, T.; Kurita, H.; Sakamaki, K.; Takenobu, T.; Harada, S.; Ogasawara, T.; et al. Guide for surgical procedures in oral and maxillofacial areas during coronavirus disease 2019 pandemic. J. Oral Maxillofac. Surg. Med. Pathol. 2022, 34, 294–314. [Google Scholar] [CrossRef] [PubMed]
- Levine, M.H.; Goddard, A.L.; Dodson, T.B. Inferior alveolar nerve canal position: A clinical and radiographic study. J. Oral Maxillofac. Surg. 2007, 65, 470–474. [Google Scholar] [CrossRef] [PubMed]
- Bürklein, S.; Grund, C.; Schäfer, E. Relationship between Root Apices and the Mandibular Canal: A Cone-beam Computed Tomographic Analysis in a German Population. J. Endod. 2015, 41, 1696–1700. [Google Scholar] [CrossRef] [PubMed]
- Maló, P.; de Araújo Nobre, M.; Lopes, A.; Ferro, A.; Botto, J. The All-on-4 treatment concept for the rehabilitation of the completely edentulous mandible: A longitudinal study with 10 to 18 years of follow-up. Clin. Implant. Dent. Relat. Res. 2019, 21, 565–577. [Google Scholar] [CrossRef] [PubMed]
- Steigmann, L.; Di Gianfilippo, R.; Steigmann, M.; Wang, H.L. Classification Based on Extraction Socket Buccal Bone Morphology and Related Treatment Decision Tree. Materials 2022, 15, 733. [Google Scholar] [CrossRef]
- Eto, V.M.; Figueiredo, N.C.; Eto, L.F.; Azevedo, G.M.; Silva, A.I.V.; Andrade, I. Bone thickness and height of the buccal shelf area and the mandibular canal position for miniscrew insertion in patients with different vertical facial patterns, age, and sex. Angle Orthod. 2023, 93, 185–194. [Google Scholar] [CrossRef]
- Aleluia, R.B.; Duplat, C.B.; Crusoé-Rebello, I.; Neves, F.S. Assessment of the mandibular buccal shelf for orthodontic anchorage: Influence of side, gender and skeletal patterns. Orthod. Craniofac. Res. 2021, 24, 83–91. [Google Scholar] [CrossRef] [PubMed]
- Gandhi, V.; Upadhyay, M.; Tadinada, A.; Yadav, S. Variability associated with mandibular buccal shelf area width and height in subjects with different growth pattern, sex, and growth status. Am. J. Orthod. Dentofac. Orthop. 2021, 159, 59–70. [Google Scholar] [CrossRef] [PubMed]
- Gupta, A.; Pubreja, L.; Malik, R.; Gupta, N. Evaluation of the Dimensions of Anterior Loop of Mental Nerve in CBCT: A Radiographic Analysis. J. Maxillofac. Oral Surg. 2020, 19, 168–172. [Google Scholar] [CrossRef] [PubMed]
- Giroh, V.R.; Hebbale, M.; Mhapuskar, A.; Modak, R.; Agarwal, P. Prevalence of Anterior Loop and other Patterns of Mental Nerve in a Sample Population of an Indian City: A Retrospective Study. Ann. Maxillofac. Surg. 2022, 12, 11–16. [Google Scholar] [CrossRef]
- Ghandourah, A.O.; Badaoud, M.B.; Dahlawi, A.; Alghamdi, A.; Alhazmi, F.; Sembawa, S.N.; Demyati, A.K. A radiographic analysis of the location of the mental foramen. Saudi Dent. J. 2023, 35, 354–358. [Google Scholar] [CrossRef] [PubMed]
- Wei, X.; Gu, P.; Hao, Y.; Wang, J. Detection and characterization of anterior loop, accessory mental foramen, and lateral lingual foramen by using cone beam computed tomography. J. Prosthet. Dent. 2020, 124, 365–371. [Google Scholar] [CrossRef] [PubMed]
- Pelé, A.; Berry, P.A.; Evanno, C.; Jordana, F. Evaluation of Mental Foramen with Cone Beam Computed Tomography: A Systematic Review of Literature. Radiol. Res. Pract. 2021, 2021, 8897275. [Google Scholar] [CrossRef] [PubMed]
- Greenstein, G.; Tarnow, D. The mental foramen and nerve: Clinical and anatomical factors related to dental implant placement: A literature review. J. Periodontol. 2006, 77, 1933–1943. [Google Scholar] [CrossRef]
- Silvestri, F.; Nguyen, J.F.; Hüe, O.; Mense, C. Lingual foramina of the anterior mandible in edentulous patients: CBCT analysis and surgical risk assessment. Ann. Anat. 2022, 244, 151982. [Google Scholar] [CrossRef] [PubMed]
- Yildirim, Y.D.; Güncü, G.N.; Galindo-Moreno, P.; Velasco-Torres, M.; Juodzbalys, G.; Kubilius, M.; Gervickas, A.; Al-Hezaimi, K.; Al-Sadhan, R.; Yilmaz, H.G.; et al. Evaluation of mandibular lingual foramina related to dental implant treatment with computerized tomography: A multicenter clinical study. Implant. Dent. 2014, 23, 57–63. [Google Scholar] [CrossRef]
- Muley, P.; Kale, L.; Choudhary, S.; Aldhuwayhi, S.; Thakare, A.; Mallineni, S.K. Assessment of Accessory Canals and Foramina in the Mandibular Arch Using Cone-Beam Computed Tomography and a New Classification for Mandibular Accessory Canals. Biomed. Res. Int. 2022, 2022, 5542030. [Google Scholar] [CrossRef]
- de Mello, J.S.; Faot, F.; Correa, G.; Chagas Júnior, O.L. Success rate and complications associated with dental implants in the incisive canal region: A systematic review. Int. J. Oral Maxillofac. Surg. 2017, 46, 1584–1591. [Google Scholar] [CrossRef] [PubMed]
- Ferreira Barbosa, D.A.; Barros, I.D.; Teixeira, R.C.; Menezes Pimenta, A.V.; Kurita, L.M.; Barros Silva, P.G.; Costa, F. Imaging Aspects of the Mandibular Incisive Canal: A PROSPERO-Registered Systematic Review and Meta-Analysis of Cone Beam Computed Tomography Studies. Int. J. Oral Maxillofac. Implant. 2019, 34, 423–433. [Google Scholar] [CrossRef] [PubMed]
- Çimen, T.; Asar, N.V.; Goyushov, S.; Duruel, O.; Tözüm, T.F. Effects of Crest Morphology on Lingual Concavity in Mandibular Molar Region: An Observational Study. J. Oral. Maxillofac. Res. 2023, 14, e3. [Google Scholar] [CrossRef]
- Haj Yahya, B.; Chaushu, G.; Hamzani, Y. Computed Tomography for the Assessment of the Potential Risk After Implant Placement in Fresh Extraction Sites in the Posterior Mandible. J. Oral Implantol. 2021, 47, 2–8. [Google Scholar] [CrossRef]
- Chan, H.L.; Benavides, E.; Yeh, C.Y.; Fu, J.H.; Rudek, I.E.; Wang, H.L. Risk assessment of lingual plate perforation in posterior mandibular region: A virtual implant placement study using cone-beam computed tomography. J. Periodontol. 2011, 82, 129–135. [Google Scholar] [CrossRef] [PubMed]
- Jacobs, R.; Salmon, B.; Codari, M.; Hassan, B.; Bornstein, M.M. Cone beam computed tomography in implant dentistry: Recommendations for clinical use. BMC Oral Health 2018, 18, 88. [Google Scholar] [CrossRef]
| Study | Year | Country | Sample | Age | Phenomenon of Interest | Design—CBCT Unit/Software | Evaluation | Research Type |
|---|---|---|---|---|---|---|---|---|
| Aljarbou FA et al. [25] | 2019 | Saudi Arabia | 60 (36 males, 24 females) | 29.59 ± 14.08 | Inferior alveolar canal | Cross-section Planmeca Promax® 3D Max/Planmeca Romexis® 3.6 | The distance from the outer boundary of the buccal cortical plate to the buccal root surface; the distance from the outer boundary of the lingual cortical plate to the lingual root surface; cortical boundary of the IAC to the nearest root surface. | Quantitative |
| Sekerci AE et al. [26] | 2014 | Turkey | 500 (237 females and 263 males) | 30.25 ± 12.5 | Lingual foramina | Retrospective cross-sectional in-built software (NNT) Dell Precision T5400 workstation (Dell, Round Rock, TX, USA) | Frequency and location of lingual foramina, maximum width of lingual foramina in the vertical and horizontal directions. Vertical distance of the lingual foramina to the lower border and alveolar crest of the mandible. | Quantitative |
| Bayrak S et al. [27] | 2018 | Turkey | 500 (234 males, 266 females) | 37.49 (range 10–87) | Lingual concavity | Retrospective cross-sectional I-CAT 3D Imaging System/I-CAT Vision software | SF types were classified as follows: type I, a flat impression < 2 mm deep; type II, a 2 to 3 mm concavity; and type III, a concavity > 3 mm. Thickness between mandibular canal and three mandibular cortical regions (inferior, buccal, lingual cortex). | Quantitative |
| Fouda SM et al. [28] | 2020 | Saudi Arabia | 71 CBCT scans (26 edentulous, 45 dentate) | 59.0 edentulous and 47.7 dentate | Lingual foramen | Cross-sectional Kodak 9500 Cone Beam 3D System/CS 3D | Vertical bone height, buco-lingual thickness on three different levels, presence of lingual foramen between two mandibular central incisors. The distances from the base of the lingual canal to the crest of the alveolar bone and to the base of the mandible were measured. The length of the canal was measured from the orifice of the lingual foramen to the base of the lingual canal in the same segment horizontally. | Quantitative |
| Genç T et al. [29] | 2018 | Turkey | 72 (33 males, 54 females) | 52.9 ± 10.7 | Mandibular canal, mental foramen, lingual foramen | NA | Vertical size of the mandibular canal; distance between the mandibular canal/mental foramen and the lingual foramen and the inferior border of the mandible and alveolar crest; localization of the mental foramen—the mesial side of the first premolar—between the first premolar and second premolar, and the distal side of the second premolar; diameter and location of the lingual foramen; prevalence of the anterior alveolar loop (aAL). | Quantitative |
| Barbosa DA et al. [14] | 2020 | Brazil | 646 (245 males, 401 females) | NA (six age groups) | Incisive canal | Retrospective, multicenter CS 9000 3D, Gendex CB-500, i-CAT Next Generation, i-CAT Classic/Carestream 3D | Presence or absence of the MIC. The distance from the MIC to alveolar bone crest was measured; buccal plate, lingual plate, and inferior cortex; distance from the mic to adjacent teeth apexes, MIC length, MIC vertical and horizontal diameter. | Quantitative |
| Alqutaibi AY et al. [30] | 2022 | Saudi Arabia | 320 (160 males, 160 females) | 41 ± 14.2 | Lingual canal Lingual foramina | Retrospective study, KaVo 3D eXam, KaVo/RadiAntDICOM Viewer (Version 2022.1.1) | Presence or absence of the mandibular lingual foramen, the mandibular lingual canal, the distance from the inferior border of the mandible to the superior borer of the foramen at its lingual and buccal terminals, the distance from the buccal cortex to the beginning of the MLC, the length of the canal/canals, the diameter at the lingual and buccal terminals for each canal, the canal direction (straight or divergent/convergent). | Quantitative |
| Shen YW et al. [31] | 2021 | Taiwan | 68 (30 males, 38 females) | NA | Retromolar canal—anatomical variation in mandibular canal | Asahi AZ3000/Mimics 15.0 | Parameters were measured: the diameter of the retromolar foramen (RMF), the horizontal distance from the midpoint of the RMF to the distal cementoenamel junction (CEJ) of the second molar, and the vertical distance from the midpoint of the RMF to the upper border of the mandibular canal below the second molar. | Quantitative |
| Surathu N et al. [32] | 2022 | Turkey | 65 mandibles (42 males and 23 females) | 21 to 80 years | Lingual foramen | Cross-sectional NA | The midline of the mandible in all samples was identified using the genial tubercles. This area was then examined for lingual foramina and the distance between the superior lingual foramen and the base of the mandible in an attempt to identify whether there was a relevant anatomical consistency in the location of this foramen. | Quantitative |
| Sanchez-Perez A et al. [33] | 2018 | Spain | 112 (49 males and 63 females) | 50 | Lingual foramen | Retrospective cross-sectional Planmeca ProMax 3D Max | Length of the exit canal; distance from the canal to the buccal, inferior, lingual cortex; distance from the canal to the closest alveolus or marginal crest; angulation of exit canal; diameter of orifice; presence of anatomical variation. | Quantitative |
| Vasegh Z et al. [34] | 2022 | Iran | 38 | 65.16 ± 10.88 for males and 64.33 ± 10.61 for females | Buccal and lingual concavity | Cross-sectional NewTom VGi/NNT 3D software | Ridge height in anterior mandible, ridge height considering the mental foramen, ridge height in the posterior mandible considering the inferior alveolar nerve canal. | Quantitative |
| Gümüşok M et al. [35] | 2017 | Turkey | 645 (281 males, 364 females) | 41 | Mental foramen, accessory mental foramen | Cross-section Promax 3D® | The numbers of AMF, its horizontal and vertical diameters, location with respect to the MF, and distance to the MF were determined. The horizontal and vertical diameters of the MF were also measured. In dentate cases, the positions of the teeth in the neighborhood of AMF were evaluated considering their root(s). | Quantitative |
| Wong SK et al. [36] | 2018 | Malaysia | 100 (50 males and 50 females) | NA | Anterior loop prevalence and length | eXamVisionQ, KaVo Dental software | The IAN was traced along with the anterior loop and part of the incisive nerve, while an entry and exit of the mental foramen were analyzed from the cross-sectional view. Vertical lines were drawn on the panoramic view from the slice that corresponded to the anterior and posterior walls of the mental foramen and the most anterior point of the anterior loop length (AnLL) as seen from the cross-sectional view. The study analyzed the canal height in the region of the mental foramen and length of canal | Quantitative |
| Sener E. et al. [37] | 2018 | Turkey | 70 dry mandibles (35 edentulous and 35 dentate) | NA | Mandibular incisive canal/lingual foramen | Retrospective cross-sectional/Kodak 9000 3D/Kodak Dental Imaging Software v. 6.11.6.2 and 3D module v. 2.1 | Mesio-distal length of the MIC, diameters of the LF opening (lingual diameter) and lingual canal ending (labial diameter) located on the midline of the mandible and superior to the mental spine, labial and lingual heights as the distance between the lingual canal and mandibular base on the sagittal slices of the CBCT images. | Quantitative |
| Koivisto T et al. [38] | 2016 | Minnesota USA | 106 (34 males and 72 females) | 18 to 69 years | Mandibular canal | Retrospective cross-sectional/NA/Next Generation i-CAT | Root apices of the posterior teeth to MC with the aim to evaluate the location of the mandibular canal, bone thickness, and diameter of MC and the presence of the anterior loop. | Quantitative |
| Yang XW et al. [39] | 2017 | China | 824 hemimandibles (166 males and 246 females) | 11 to 81 years | Mandibular incisive canal (MIC) | Retrospective cross-sectional/NewTom VG CBCT/by QR-NNT Version 2.21 software | The anterior border of the mental foramen and the most anterior of the inferior alveolar nerve; the lengths of the anterior extension of the anterior loop (aAL) and MIC; the lengths of caudal extension of the anterior loop (cAL), the diameter of the MIC; the diameter of the MIC; the horizontal distance from the MIC to the buccal and lingual cortical borders of the mandible; and the vertical distance from the MIC to the apex of the tooth, alveolar crest, and inferior margin of the mandible. | Quantitative |
| Yoon TY et al. [40] | 2017 | Florida USA | 104 (47 males and 55 females) | 54.8 (21–89 years) | Posterior and anterior mandible concavity | Retrospective cross-sectional study Sirona XG3 CBCT/Galaxis/Galileo Implant Viewer | The most prominent lingual aspect of bone was marked as a reference point (SLP). A vertical line (VL) was drawn from the SLP meeting the horizontal line (HL) effectively forming the legs of a triangle. The angle of the lingual concavity (ALC) was measured using the HL of the border of the mandible that formed the hypotenuse of the triangle. The mandibular morphology type was classified as parallel, concave, and convex. | Quantitative |
| Zhang W et al. [41] | 2015 | Texas USA | 59 (28 males and 31 females) | 19–74 years | Alveolar ridge | Retrospective cross-sectional/ Kodak 9500 unit/Anatomage Invivo 5.1 software | All measurements were performed from molar sites in the posterior right mandible. Cross-sectional views were generated along the distal surface of the mesial root of mandibular molars or in the middle of the edentulous socket. Alveolar height, width, and buccal bone thickness were measured on the cross-sectional views separately for the first, second, and third molar. | Quantitative |
| J PC et al. [42] | 2018 | India | 85 | NA | Anterior loop | NA | The length of the loop was measured in mm. Five lines were drawn to standardize the nerve loop length measurement in all CBCTs. | Quantitative |
| Lu Cl et al. [43] | 2015 | California USA | 122 (61 males and 61 females) | Three age groups: 21–40, 41–60, and 61–80 years | Anterior loop | Retrospective cross-sectional I-CAT Cone Beam 3D Dental Imaging System/I-CAT Vision software | Study described the precise position of a 3D image to make imaginary lines for the analysis of anterior loop length. The measure of length of the mental nerve was compared with both sided of the mandible, according to gender and sex. | Quantitative |
| Raju N et al. [44] | 2019 | Texas USA | 124 (56 male and 68 females) | 16–83 years | Anterior loop | Retrospective cross-sectional/ Kodak 9500 scanner/Invivo 5.0 software | Study observed the prevalence of the anterior loop, the length of the anterior loop, available bone coronally to the mental foramen and the anterior loop, passage of the anterior loop. | Quantitative |
| Vujanovic-Eskenazi A et al. [45] | 2015 | Spain | 82 (26 males and 56 females) | 56.56 years (range 18–80) | Mental foramen/loop | Retrospective descriptive study/ Kodak 9500 3D/NA | The distance from the lower border of the mandible to the lower point of the mental foramen and anterior extension of the mental loop to the most mesial point of the mental foramen on both types of scans. | Mixed |
| Kavarthapu A et al. [46] | 2018 | India | 139 (106 males and 33 females) | 15–75 | Inferior alveolar nerve | Retrospective cross-sectional/NA/Sirona Galaxis Galileos Viewer Version 1.9 | CN—distance from the alveolar crest to the bone directly superior to the IAN; BN—distance from the buccal cortex to the bone directly lateral to the IAN; LN—distance from the lingual cortex of the bone directly medial to the IAN; IN—distance from the inferior border of the mandible to the bone directly inferior to the IAN. | Quantitative |
| He X et al. [47] | 2016 | China | 200 (97 males and 103 females) | 27 (10–70) | Lingual foramina | Retrospective cross-sectional Kodak 9500 Cone Beam 3D System/CS 3D Imaging Software | Presence, frequency, location, and morphological variations. Linear measurements, as diameter, distance between the lingual foramen and the alveolar ridge crest (L1), the distance between the lingual foramen and the tooth apex (L2), and the vertical distance from the mandibular border to the lingual foramen (L3). Lingual foramina were classified as follows: in localization, occurrence, and according to the direction of the canal. | Quantitative |
| Çitir M et al. [48] | 2021 | Turkey | 106 (45 males and 61 females) | 55.7 ± 10.31 | Lingual concavity | Retrospective cross-sectional Galileos (Sirona Dental Systems)/SIRONA Sidexis XG 2.61 viewer software | Maximum bone height and width, concavity depth, lingual slope angle, lingual concavity angle and morphology of the bone of the anterior region of the mandible were measured. Standard measures of the region 4–6 mm anterior of the mental foramen were examined. The bone in the anterior region was classified as type I lingual concavity, type II inclined to lingual, type III enlarging towards labiolingual, and type IV buccal concavity. | Mixed |
| Kong Zl et al. [49] | 2021 | China | 201 (100 males and 101 females) | 18–66 | Lingual concavity in molar region | Retrospective cross-sectional KaVo 3D eXam/E-3D Medical Software V16.19 | The long axis of the tooth determinate from the apex of the mesial root to the line that connects the midpoint of the buccolingual counterpart of the tooth crown, the long axis of the alveolar process marked by bisecting the buccal line and lingual line of the alveolar process, the angles between these imaginary lines, the width between the buccal and lingual alveolar plates at the lower point of the alveolar bone and the perpendicular line forming the angle, the long axis of the basal bone, and the upper internal angle. | Quantitative |
| Tsai YC et al. [50] | 2021 | Taiwan | 149 | NA | Lingual concavity (anterior) | Retrospective observational study CBCT machine NewTom 5G/software ImplantMax 4.0 | The study evaluated morphological and dimensional parameters: concavity depth, concavity angle, torque, and deep bone thickness. Also, the study performed virtual implant selection and placement to define possible labial bone perforation during planning implant placement and four classes of crestal and radicular dentoalveolar phenotype. | Quantitative |
| Alqutaibi AY et al. [51] | 2024 | Saudi Arabia | 150 (75 males and 75 females) | 18 to 29 and over 30 | Lingual concavity (posterior) | Retrospective cross-sectional study TUDH’s CBCT machine (Kavo Dental), and measurements were performed using the RadiAnt DICOM viewer | The cross-sectional view used to evaluate the morphology of the inferior mandible canal, alveolar crest, and mandibular lingual concavity in the region of the left and right first and second molar. The ridge was defined as a U, C, or P shape. Also, the most superior and inferior prominent point and deepest point of concavity were detected. | Quantitative |
| Kanewoff E et al. [52] | 2024 | Brazil | 239 (98 males and 141 females) | 50.9 ± 15.6 | Lingual concavity | Retrospective study i-CAT CBCT system i-CAT 3D imaging system | The study performed implant placement simulation in two ways: the prosthetic-driven ideal position and bone-driven ideal position, according to the secure distance from adjacent anatomical structures. Measures performed were as follows: number and localization of lingual foramen, labial concavity angle, labial concavity depth, mandible basal bone height, tooth torque, mandibular bone thickness, angle measurement. | Quantitative |
| Gu L et al. [53] | 2018 | China | 749 | 37.5 ± 13.6 | Mandibular canal | Retrospective CBCT scanner (Planmeca, Planmeca Romexis software) | Position of the mandibular canal relative to the roots in four class (apical, buccal, lingual, and interradicular) and contact relation of the mandibular third molar and the mandibular canal in each class. | Qualitative |
| Author of the Study | D1 | D2 | D3 | D4 | D5 | D6 | D7 | Overall |
|---|---|---|---|---|---|---|---|---|
| Aljarbou FA et al. 2019 [25] | ☺ | |||||||
| Sekerci AE et al. 2014 [26] | ☺ | |||||||
| Bayrak S et al. 2018 [27] | ☺ | |||||||
| Fouda SM et al. 2020 [28] | ☺ | |||||||
| Genç T et al. 2018 [29] |  | |||||||
| Barbosa DA et al. 2020 [14] | ☺ | |||||||
| Alqutaibi AY et al. 2022 [30] | ☺ | |||||||
| Shen YW et al. 2021 [31] |  | |||||||
| Surathu N et al. 2022 [32] |  | |||||||
| Sanchez-Perez A et al. 2018 [33] | ☺ | |||||||
| Vasegh Z et al. 2022 [34] |  | |||||||
| Gümüşok M et al. 2017 [35] |  | |||||||
| Wong SK et al. 2018 [36] | ☺ | |||||||
| Sener E. et al. 2018 [37] | ☺ | |||||||
| Koivisto T et al. 2016 [38] | ☺ | |||||||
| Yang XW et al 2017 [39] | ☺ | |||||||
| Yoon TY et al. 2017 [40] | ☺ | |||||||
| Zhang W et al. 2015 [41] | ☺ | |||||||
| J PC et al. 2018 [42] |  | |||||||
| Lu Cl et al. 2015 [43] | ☺ | |||||||
| Raju N et al. 2019 [44] | ☺ | |||||||
| Vujanovic-Eskenazi A et al. 2015 [45] | ☺ | |||||||
| Kavarthapu A et al. 2018 [46] | ☺ | |||||||
| He X et al. 2016 [47] | ☺ | |||||||
| Çitir M et al. 2021 [48] | ☺ | |||||||
| Kong Zl et al. 2021 [49] | ☺ | |||||||
| Tsai YC et al. 2021 [50] | ☺ | |||||||
| Alqutaibi AY et al. 2024 [51] | ☺ | |||||||
| Kanewoff E et al. 2024 [52] | ☺ | |||||||
| Gu L et al. 2018 [53] | ☺ |
 ), and red indicates a high level of bias (☹).
), and red indicates a high level of bias (☹).| Author | Distance to Buccal Cortical Plate | Distance to Lingual Cortical Plate | Distance to Alveolar Crest | Distance to Inferior Border of Mandible | Vertical Size of Canal | Shortest Distance from Canal to Tooth Apices |
|---|---|---|---|---|---|---|
| Aljarbou et al. [25] | 4.64 ± 1.63 | 3.63 ± 1.40 | NA | NA | NA | 3.16 ± 1.95 |
| Genç et al. [29] | NA | NA | 11.58 ± 3.42 | 7.58 ± 1.33 | 2.53 ± 0.51 | NA |
| Kavarthapu et al. [46] | 4.68 ± 1.34 | 2.48 ± 1.15 | 15.04 ± 3.32 | 7.23 ± 1.73 | NA | NA |
| Author | MF and Alveolar Crest | MF and Base of Mandible | MF Vertical Diameter | MF Horizontal Diameter | AL Length | AL and Alveolar Bone | AL and Base of Mandible |
|---|---|---|---|---|---|---|---|
| Genç et al. [29] | 9.23 ± 3.26 | 11.50 ± 1.86 | NA | NA | NA | NA | NA |
| Gümüşok et al. [35] | NA | NA | 3.11 ± 0.89 | 2.80 ± 0.99 | NA | NA | NA |
| Wong et al. [36] | NA | NA | NA | NA | 3.77 ± 1.74 | NA | NA |
| J, PC et al. [42] | NA | NA | NA | NA | 2.79 ± NA | NA | NA |
| Lu et al. [43] | NA | NA | NA | NA | 1.46 ± 1.25 | NA | NA |
| Raju et al. [44] | 12.92 ± 3.55 | NA | NA | NA | 1.73 ± NA | 17.06 ±2.69 | NA |
| Vujanovic-Eskenazi et al. [45] | NA | NA | NA | NA | 1.59 ± 0.93 | NA | 11.43 ± 1.81 |
| Distance from Alveolar Crest | Distance from Base of Mandible | Distance from Buccal Cortex | Distance from Lingual Cortex | Length of Canal | Diameter of Canal | |
|---|---|---|---|---|---|---|
| Sekerci et al. [26] | 20.30 ± 4.59 | 9.31 ± 3.86 | NA | NA | NA | 1.02 ± 0.37 |
| Fouda et al. [28] | 17.99 ± 4.86 | 8.05 ± 2.37 | NA | NA | 8.30 ± 1.99 | NA |
| Genc et al. [29] | 13.62 ± 4.35 | 11.35 ± 3.41 | NA | NA | NA | NA |
| Alqutaib et al. [30] | NA | NA | NA | NA | 5.49 ± 1.89 | NA |
| Surathu et al. [32] | NA | 15.06 ± 1.91 | NA | NA | NA | NA |
| Sanchez-Perez et al. [33] | 11.80 ± 3.25 | 7.75 ± 2.51 | 4.94 ± 1.60 | 8.62 ± 1.36 | 8.93 ± 1.94 | 1.44 ± 0.45 |
| Sener et al. [37] | NA | NA | NA | NA | NA | 0.78 ± 0.30 |
| He et al. [47] | 16.62 ± 8.57 | 13.66 ± 8.51 | NA | NA | NA | 0.86 ± 0.32 |
| Author | MIC to Alveolar Crest—Initial | MIC to Buccal Cortex—Initial | MIC to Lingual Cortex—Initial | MIC to Base of Mandible—Initial | MIC to Alveolar Crest—End | MIC to Buccal Cortex—End | MIC to Lingual Cortex—End | MIC to Base of Mandible—End | Incisive Canal Length | Incisive Canal Diameter |
|---|---|---|---|---|---|---|---|---|---|---|
| Barbosa et al. [14] | 16.48 ± 5.52 | 2.62 ± 1.26 | 5.12 ± 1.71 | 9.40 ± 1.88 | 18.72 ± 3.47 | 4.00 ± 1.41 | 4.59 ± 1.66 | 8.87 ± 2.01 | NA | NA |
| Sener et al. [37] | NA | NA | NA | NA | NA | NA | NA | NA | 2.82 ± 1.26 | 2.40 ± 0.65 |
| Yang et al. [39] | NA | NA | NA | NA | NA | NA | NA | NA | 10.50 ± 4.81 | 2.01 ± 0.47 |
| Author | Anterior Concavity Depth | Anterior Concavity Length | Anterior Angulation | Posterior Concavity Depth | Posterior Concavity Length | Posterior Angulation |
|---|---|---|---|---|---|---|
| Bayrak et al. [27] | NA | NA | NA | 2.69 ± 0.84 | NA | NA |
| Vasegh et al. [34] | 1.47 ± 0.58 | NA | 10.20 ± 5.34 | 1.85 ± 0.52 | NA | 10.66 ± 5.96 |
| Yoon et al. [40] | 2.54 ± 1.08 | 18.23 ± 3.55 | 83.27 ± 8.68 | 3.84 ± 1.98 | 16.10 ± 2.89 | 75.48 ± 12.71 |
| Çitir et al. [48] | 3.66 ± 0.97 | NA | 60.78 ± 2.70 | NA | NA | NA |
| Tsai et al. [50] | 4.44 ± 1.96 | NA | NA | NA | NA | NA |
| Alqutaibi et al. [51] | NA | NA | NA | 1.98 ± 0.78 | 11.73 ± 2.48 | 47.95 ± 11.83 |
| Kanewoff et al. [52] | 3.20 ± 1.50 | NA | NA | NA | NA | NA |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rajkovic Pavlovic, Z.; Stepovic, M.; Bubalo, M.; Zivanovic Macuzic, I.; Vulovic, M.; Folic, N.; Milosavljevic, J.; Opancina, V.; Stojadinovic, D. Anatomic Variations Important for Dental Implantation in the Mandible—A Systematic Review. Diagnostics 2025, 15, 155. https://doi.org/10.3390/diagnostics15020155
Rajkovic Pavlovic Z, Stepovic M, Bubalo M, Zivanovic Macuzic I, Vulovic M, Folic N, Milosavljevic J, Opancina V, Stojadinovic D. Anatomic Variations Important for Dental Implantation in the Mandible—A Systematic Review. Diagnostics. 2025; 15(2):155. https://doi.org/10.3390/diagnostics15020155
Chicago/Turabian StyleRajkovic Pavlovic, Zlata, Milos Stepovic, Marija Bubalo, Ivana Zivanovic Macuzic, Maja Vulovic, Nevena Folic, Jovana Milosavljevic, Valentina Opancina, and Dobrivoje Stojadinovic. 2025. "Anatomic Variations Important for Dental Implantation in the Mandible—A Systematic Review" Diagnostics 15, no. 2: 155. https://doi.org/10.3390/diagnostics15020155
APA StyleRajkovic Pavlovic, Z., Stepovic, M., Bubalo, M., Zivanovic Macuzic, I., Vulovic, M., Folic, N., Milosavljevic, J., Opancina, V., & Stojadinovic, D. (2025). Anatomic Variations Important for Dental Implantation in the Mandible—A Systematic Review. Diagnostics, 15(2), 155. https://doi.org/10.3390/diagnostics15020155






