A Retrospective Analysis: Investigating Factors Linked to High Lung-RADS Scores in a Nonsmoking, Non-Family History Population
Abstract
1. Introduction
2. Materials and Methods
Statistical Analysis
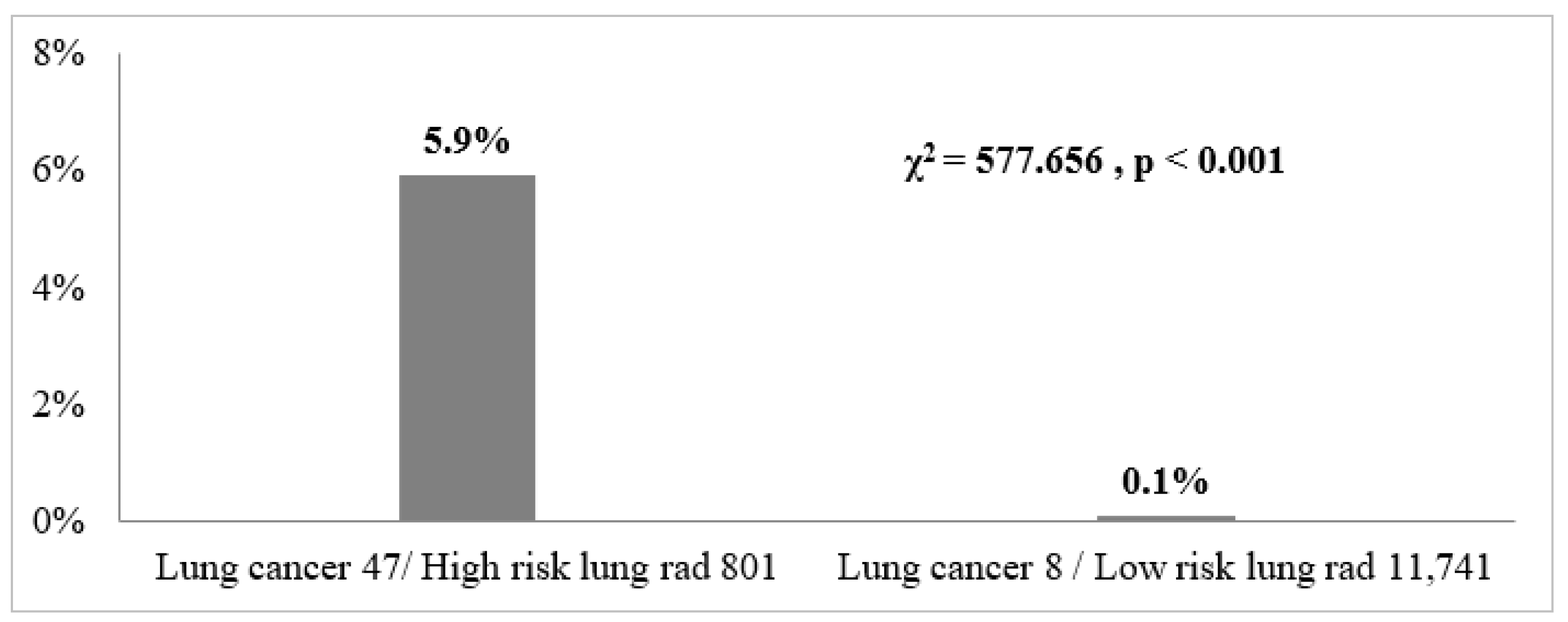
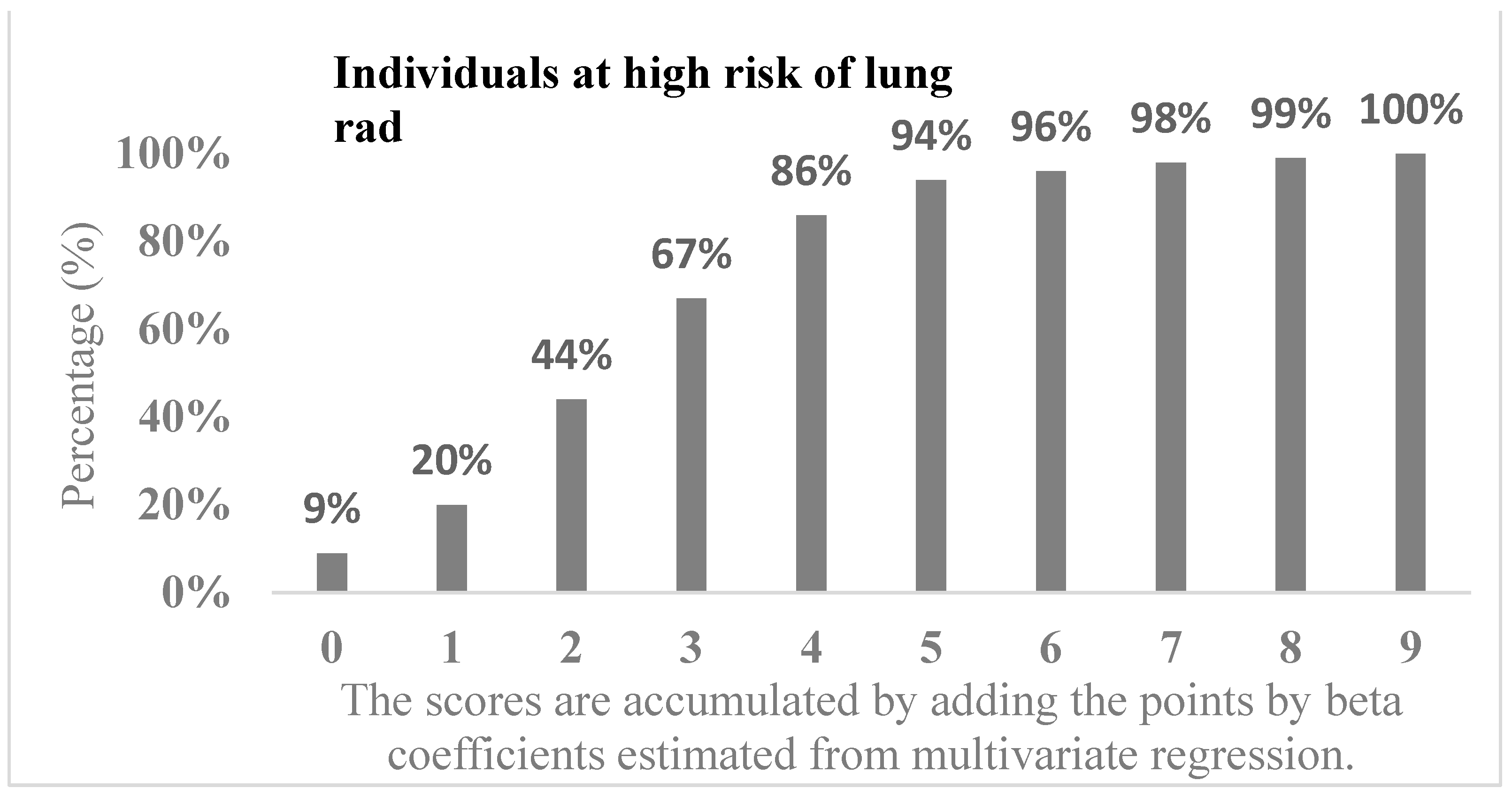
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- National Lung Screening Trial Research Team; Aberle, D.R.; Adams, A.M.; Berg, C.D.; Black, W.C.; Clapp, J.D.; Fagerstrom, R.M.; Gareen, I.F.; Gatsonis, C.; Marcus, P.M.; et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N. Engl. J. Med. 2011, 365, 395–409. [Google Scholar] [CrossRef] [PubMed]
- American College of Radiology. Lung CT Screening Reporting & Data System (Lung-RADS®) 11 August 2014. Available online: https://www.acr.org/Clinical-Resources/Reporting-and-Data-Systems/Lung-Rads (accessed on 1 March 2024).
- Potter, A.L.; Bajaj, S.S.; Yang, C.J. The 2021 USPSTF lung cancer screening guidelines: A new frontier. Lancet Respir. Med. 2021, 9, 689–691. [Google Scholar] [CrossRef] [PubMed]
- Houston, K.A.; Henley, S.J.; Li, J.; White, M.C.; Richards, T.B. Patterns in lung cancer incidence rates and trends by histologic type in the United States, 2004–2009. Lung Cancer 2014, 86, 22–28. [Google Scholar] [CrossRef] [PubMed]
- Barta, J.A.; Powell, C.A.; Wisnivesky, J.P. Global epidemiology of lung cancer. Ann. Glob. Health 2019, 85, 8. [Google Scholar] [CrossRef] [PubMed]
- Risch, H.A.; Howe, G.R.; Jain, M.; Burch, J.D.; Holowaty, E.J.; Miller, A.B. Are female smokers at higher risk for lung cancer than male smokers? A case-control analysis by histologic type. Am. J. Epidemiol. 1993, 138, 281–293. [Google Scholar] [CrossRef] [PubMed]
- Risch, H.A.; Howe, G.R.; Jain, M.; Burch, J.D.; Holowaty, E.J.; Miller, A.B. Lung cancer risk for female smokers. Science 1994, 263, 1206–1208. [Google Scholar] [CrossRef] [PubMed]
- Bain, C.; Feskanich, D.; Speizer, F.E.; Thun, M.; Hertzmark, E.; Rosner, B.A.; Colditz, G.A. Lung cancer rates in men and women with comparable histories of smoking. J. Natl. Cancer Inst. 2004, 96, 826–834. [Google Scholar] [CrossRef] [PubMed]
- Hovanec, J.; Siemiatycki, J.; Conway, D.I.; Olsson, A.; Stücker, I.; Guida, F.; Jöckel, K.H.; Pohlabeln, H.; Ahrens, W.; Brüske, I.; et al. Lung cancer and socioeconomic status in a pooled analysis of case-control studies. PLoS ONE 2018, 13, e0192999. [Google Scholar] [CrossRef] [PubMed]
- Zang, E.A.; Wynder, E.L. Differences in lung cancer risk between men and women: Examination of the evidence. J. Natl. Cancer Inst. 1996, 88, 183–192. [Google Scholar] [CrossRef]
- De Matteis, S.; Consonni, D.; Pesatori, A.C.; Bergen, A.W.; Bertazzi, P.A.; Caporaso, N.E.; Lubin, J.H.; Wacholder, S.; Landi, M.T. Are women who smoke at higher risk for lung cancer than men who smoke? Am. J. Epidemiol. 2013, 177, 601–612. [Google Scholar] [CrossRef]
- You, D.; Wang, D.; Wu, Y.; Chen, X.; Shao, F.; Wei, Y.; Zhang, R.; Lange, T.; Ma, H.; Xu, H.; et al. Associations of genetic risk, BMI trajectories, and the risk of non-small cell lung cancer: A population-based cohort study. BMC Med. 2022, 20, 203. [Google Scholar] [CrossRef]
- Zhao, J.; Barta, J.A.; McIntire, R.; Shusted, C.; Zeigler-Johnson, C.; Juon, H.S. Racial difference in BMI and lung cancer diagnosis: Analysis of the National Lung Screening Trial. BMC Cancer 2022, 22, 797. [Google Scholar] [CrossRef] [PubMed]
- Jiang, L.; Sun, Y.Q.; Brumpton, B.M.; Langhammer, A.; Chen, Y.; Mai, X.M. Body mass index and incidence of lung cancer in the HUNT study: Using observational and Mendelian randomization approaches. BMC Cancer 2022, 22, 1152. [Google Scholar] [CrossRef]
- Mannino, D.M.; Aguayo, S.M.; Petty, T.L.; Redd, S.C. Low lung function and incident lung cancer in the United States: Data from the First National Health and Nutrition Examination Survey follow-up. Arch. Intern. Med. 2003, 163, 1475–1480. [Google Scholar] [CrossRef] [PubMed]
- Forder, A.; Zhuang, R.; Souza, V.G.P.; Brockley, L.J.; Pewarchuk, M.E.; Telkar, N.; Stewart, G.L.; Benard, K.; Marshall, E.A.; Reis, P.P.; et al. Mechanisms Contributing to the Comorbidity of COPD and Lung Cancer. Int. J. Mol. Sci. 2023, 24, 2859. [Google Scholar] [CrossRef]
- Park, H.Y.; Kang, D.; Shin, S.H.; Choi, H.; Jang, S.H.; Lee, C.H.; Cho, J. Pulmonary tuberculosis and the incidence of lung cancer among patients with chronic obstructive pulmonary disease. Ann. Am. Thorac. Soc. 2022, 19, 640–648. [Google Scholar] [CrossRef]
- Kim, H.; Kim, H.Y.; Goo, J.M.; Kim, Y. Lung cancer CT screening and lung-RADS in a tuberculosis-endemic country: The Korean lung cancer screening project (K-LUCAS). Radiology 2020, 296, 181–188. [Google Scholar] [CrossRef]
- Kocher, F.; Hilbe, W.; Seeber, A.; Pircher, A.; Schmid, T.; Greil, R.; Auberger, J.; Nevinny-Stickel, M.; Sterlacci, W.; Tzankov, A.; et al. Longitudinal analysis of 2293 NSCLC patients: A comprehensive study from the TYROL registry. Lung Cancer 2015, 87, 193–200. [Google Scholar] [CrossRef] [PubMed]
- Chen, T.Y.; Fang, Y.H.; Chen, H.L.; Chang, C.H.; Huang, H.; Chen, Y.S.; Hsiung, C.A. Impact of cooking oil fume exposure and fume extractor use on lung cancer risk in non-smoking Han Chinese women. Sci. Rep. 2020, 10, 6774. [Google Scholar] [CrossRef]
- Xue, Y.; Jiang, Y.; Jin, S.; Li, Y. Association between cooking oil fume exposure and lung cancer among Chinese nonsmoking women: A meta-analysis. OncoTargets Ther. 2016, 9, 2987–2992. [Google Scholar] [CrossRef]
- Yu, I.T.; Chiu, Y.L.; Au, J.S.; Wong, T.W.; Tang, J.L. Dose-response relationship between cooking fumes exposures and lung cancer among Chinese nonsmoking women. Cancer Res. 2006, 66, 4961–4967. [Google Scholar] [CrossRef] [PubMed]
- Ko, Y.C.; Cheng, L.S.; Lee, C.H.; Huang, J.J.; Huang, M.S.; Kao, E.L.; Wang, H.Z.; Lin, H.J. Chinese food cooking and lung cancer in women nonsmokers. Am. J. Epidemiol. 2000, 151, 140–147. [Google Scholar] [CrossRef] [PubMed]
- Bigert, C.; Gustavsson, P.; Straif, K.; Pesch, B.; Brüning, T.; Kendzia, B.; Schüz, J.; Stücker, I.; Guida, F.; Brüske, I.; et al. Lung cancer risk among cooks when accounting for tobacco smoking: A pooled analysis of case-control studies from Europe, Canada, New Zealand, and China. J. Occup. Environ. Med. 2015, 57, 202–209. [Google Scholar] [CrossRef] [PubMed]
- Swanton, C.; Hill, W.; Lim, E.; Lee, C.; Weeden, C.E.; Augustine, M.; Chen, K.; Kuan, F.C.; Marongiu, F.; Rodrigues, F.; et al. LBA1 Mechanism of action and an actionable inflammatory axis for air pollution induced non-small cell lung cancer: Towards molecular cancer prevention. Ann. Oncol. 2022, 33, S1413. [Google Scholar] [CrossRef]
- Liu, X.; Mubarik, S.; Wang, F. Lung cancer death attributable to long-term ambient particulate matter (PM(2.5)) exposure in East Asian countries during 1990–2019. Front. Med. 2021, 8, 742076. [Google Scholar] [CrossRef] [PubMed]
- Turner, M.C.; Andersen, Z.J.; Baccarelli, A.; Diver, W.R.; Gapstur, S.M.; Pope, C.A., III; Prada, D.; Samet, J.; Thurston, G.; Cohen, A. Outdoor air pollution and cancer: An overview of the current evidence and public health recommendations. CA Cancer J. Clin. 2020, 70, 460–479. [Google Scholar] [CrossRef]
- Tseng, C.H.; Tsuang, B.J.; Chiang, C.J.; Ku, K.C.; Tseng, J.S.; Yang, T.Y.; Hsu, K.H.; Chen, K.C.; Yu, S.L.; Lee, W.C.; et al. The relationship between air pollution and lung cancer in nonsmokers in Taiwan. J. Thorac. Oncol. 2019, 14, 784–792. [Google Scholar] [CrossRef]
| Total | With High-Risk Group | Without High-Risk Group | ||
|---|---|---|---|---|
| Variables | N = 12,542 (%) | N = 801 (%) | N = 11,741 (%) | p-Value |
| Age (mean ± SD), year | 53.0 ± 11.3 | 56.7 ± 10.9 | 52.8 ± 11.2 | <0.001 |
| Age | <0.001 | |||
| ≤55 | 7234 (58) | 374 (47) | 6860 (58) | |
| >55 | 5308 (42) | 427 (53) | 4881 (42) | |
| Sex | <0.001 | |||
| Male | 7192 (57) | 400 (50) | 6792 (58) | |
| Female | 5350 (43) | 401 (50) | 4949 (42) | |
| BMI | <0.001 | |||
| Not overweight (<25) | 7722 (62) | 546 (68) | 7176 (61) | |
| Overweight (25–29) | 4820 (38) | 255 (32) | 4565 (39) | |
| Previous chest symptom * | 0.212 | |||
| Yes | 2389 (19) | 166 (21) | 2223 (19) | |
| No | 10,153 (81) | 635 (79) | 9518 (81) | |
| Previous respiratory symptom | 0.001 | |||
| Cough | 2303 (18) | 176 (22) | 2127 (18) | |
| Dyspnea/breathless when exercising | 1399 (11) | 108 (14) | 1291 (11) | |
| No | 8840 (71) | 517 (65) | 8323 (71) | |
| Underlying chest disease | <0.001 | |||
| Asthma | 409 (3) | 40 (5) | 369 (3) | |
| Tuberculosis | 157 (1) | 27 (3) | 130 (1) | |
| Obstructive pulmonary disease | 204 (2) | 18 (2) | 186 (2) | |
| No | 11,772 (94) | 716 (89) | 11,056 (94) | |
| Smoking habit | 0.218 | |||
| ≥20 pack-year | 10,532 (84) | 685 (86) | 9847 (84) | |
| No smoking Or <20 pack-year | 2010 (16) | 116 (15) | 1894 (16) | |
| Residential location | 0.286 | |||
| Living in South Taiwan | 9288 (74) | 606 (76) | 8682 (74) | |
| Not living in South Taiwan | 3254 (26) | 195 (24) | 3059 (26) | |
| Cooking habit | <0.001 | |||
| High-risk | 1794 (14) | 154 (19) | 1640 (14) | |
| Low-risk | 10,748 (86) | 647 (81) | 10,101 (86) |
| Univariate | Multivariate | |||
|---|---|---|---|---|
| Variables | OR (95% CI) | p-Value | aOR (95% CI) | p-Value |
| Age | ||||
| ≤55 | Ref | Ref | ||
| >55 | 1.61 (1.39–1.85) | <0.001 | 1.56 (1.35–1.80) | <0.001 |
| Sex | ||||
| Male | Ref | Ref | ||
| Female | 1.38 (1.19–1.59) | <0.001 | 1.30 (1.12–1.51) | 0.001 |
| BMI | ||||
| Not overweight (<25) | 1.36 (1.17–1.59) | <0.001 | 1.29 (1.10–1.51) | 0.002 |
| Overweight (≥25) | Ref | Ref | ||
| Previous respiratory symptom | ||||
| Yes | 1.35 (1.16–1.56) | <0.001 | 1.25 (1.08–1.46) | 0.004 |
| No | Ref | Ref | ||
| Underlying chest disease | ||||
| Obstructive pulmonary disease | 1.54 (1.16–2.03) | 0.003 | 1.48 (1.11–1.97) | 0.007 |
| Pulmonary tuberculosis | 3.10 (2.03–4.70) | <0.001 | 2.72 (1.78–4.16) | <0.001 |
| No | Ref | Ref | ||
| Smoking habit | ||||
| No smoking Or <20 pack-year | Ref | |||
| ≥20 pack-year | 0.88 (0.72–1.08) | 0.218 | ||
| Residential location | ||||
| Living in South Taiwan | 1.10 (0.93–1.29) | 0.286 | ||
| Not living in South Taiwan | Ref | |||
| Cooking habit | ||||
| High-risk | 1.47 (1.22–1.76) | <0.001 | ||
| Low-risk | Ref |
| Variables | Points |
|---|---|
| Age > 55 | 2 |
| Female | 1 |
| Underweight (<25) | 1 |
| Previous respiratory symptom | 1 |
| Obstructive pulmonary disease | 2 |
| Pulmonary tuberculosis | 4 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, C.-S.; Yu, H.-C.; Yin, C.-H.; Chen, J.-S.; Chen, Y.-S.; Chen, I.-S. A Retrospective Analysis: Investigating Factors Linked to High Lung-RADS Scores in a Nonsmoking, Non-Family History Population. Diagnostics 2024, 14, 784. https://doi.org/10.3390/diagnostics14080784
Chen C-S, Yu H-C, Yin C-H, Chen J-S, Chen Y-S, Chen I-S. A Retrospective Analysis: Investigating Factors Linked to High Lung-RADS Scores in a Nonsmoking, Non-Family History Population. Diagnostics. 2024; 14(8):784. https://doi.org/10.3390/diagnostics14080784
Chicago/Turabian StyleChen, Chi-Shen, Hsien-Chung Yu, Chun-Hao Yin, Jin-Shuen Chen, Yao-Shen Chen, and I-Shu Chen. 2024. "A Retrospective Analysis: Investigating Factors Linked to High Lung-RADS Scores in a Nonsmoking, Non-Family History Population" Diagnostics 14, no. 8: 784. https://doi.org/10.3390/diagnostics14080784
APA StyleChen, C.-S., Yu, H.-C., Yin, C.-H., Chen, J.-S., Chen, Y.-S., & Chen, I.-S. (2024). A Retrospective Analysis: Investigating Factors Linked to High Lung-RADS Scores in a Nonsmoking, Non-Family History Population. Diagnostics, 14(8), 784. https://doi.org/10.3390/diagnostics14080784





