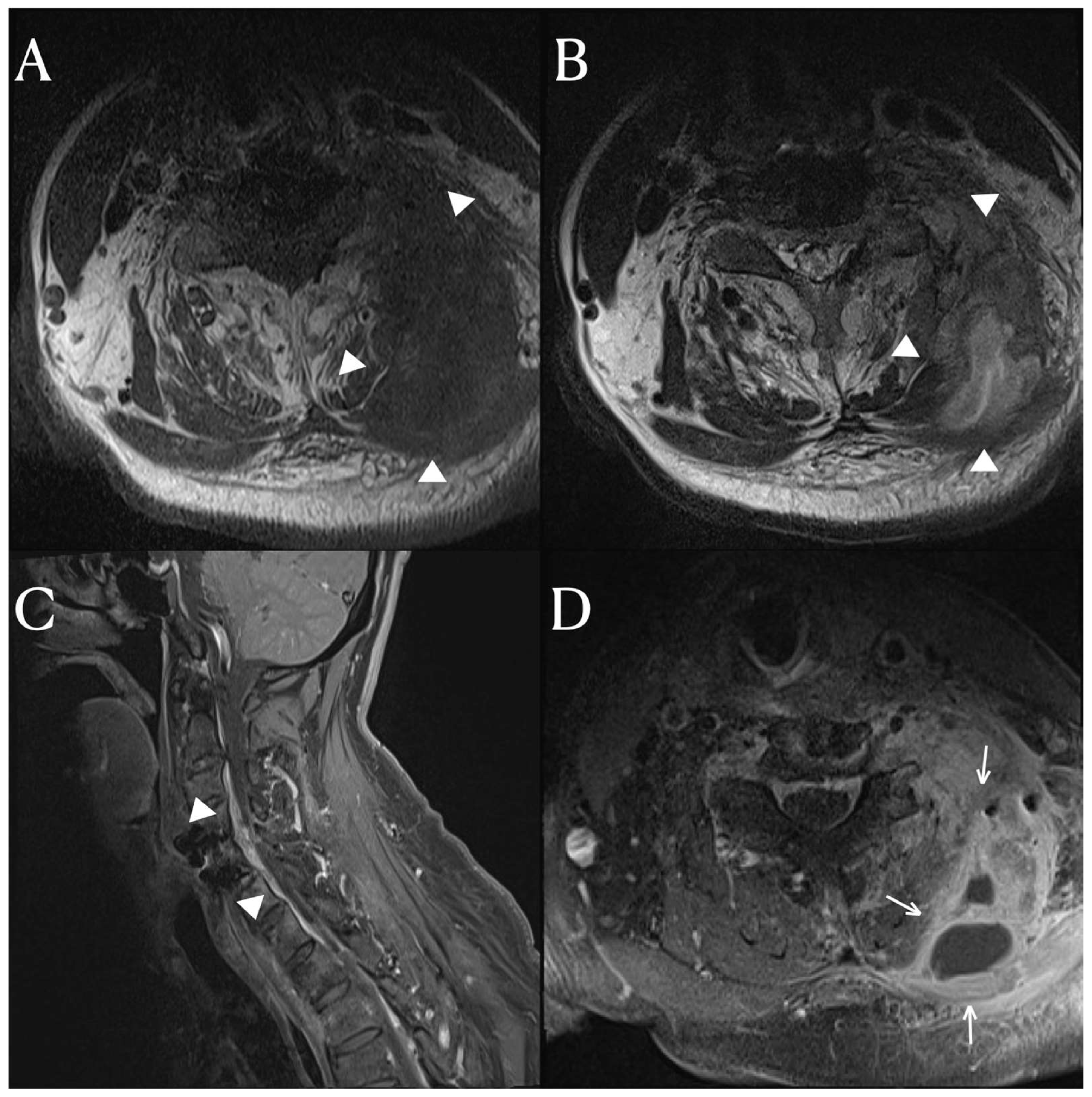
A 65-year-old patient presented a fever that began three weeks prior. He had a complete spinal cord injury below the C4 level 20 years ago in an accident and underwent anterior cervical discectomy and fusion (ACDF) on C4-5 due to a fracture and dislocation of the cervical 4–5 vertebrae. This patient was diagnosed with a urinary tract infection at another hospital and treated with antibiotics. Urinary tract infections are commonly seen in patients with neurogenic bladders in spinal cord injury. Despite treatment, the fever persisted. The patient was referred to our hospital for further evaluation and treatment due to the persistent fever. Upon examination at our hospital, there was a mass-like lesion in the posterior neck. The inflammatory markers were still elevated. We performed cervical spine MRI scans, which revealed an anterior epidural space abscess and inter-intramuscular abscess involving the left posterior neck area, extending from C3 to C6 (
Figure 1). In addition to the soft tissue infection, there was also osteomyelitis in the lamina and transverse processes of the cervical spine, for which vancomycin and a taxolactam (piperacillin sodium and tazobactam) were administered. To address the abscess, a 10 cm incision was made in the left posterior cervical area, allowing for massive irrigation and abscess removal, followed by a curettage of the cervical posterior bony arch. After the abscess removal and bony curettage, primary closure was performed. The duration of antibiotic treatment was anticipated to be between 4 and 8 weeks, depending on the clinical symptoms and the results of the inflammatory markers.
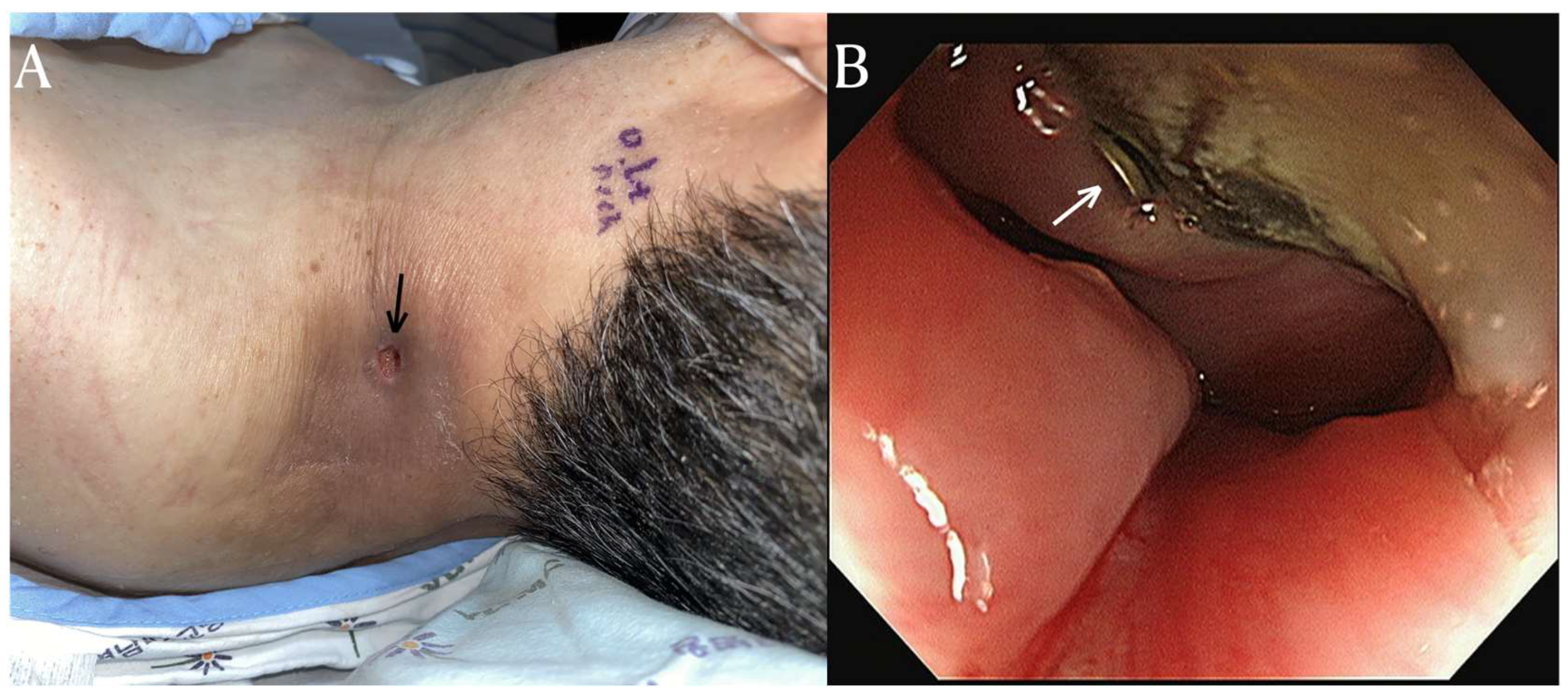
After three months of antibiotic treatment, the patient was discharged due to the improvement of the infection and abscess. However, the patient was readmitted a month later with symptoms of a systemic infection and the formation of an abscess on the posterolateral side once again. To manage the pus drainage, an incision and open drainage were performed. During the subsequent course of antibiotic treatment, food particles were observed in the previously excised drainage pathway. Furthermore, an endoscopic examination revealed an esophageal rupture with protruding hardware of the cervical fusion. (
Figure 2) Considering the medical risks of operative repair, a percutaneous endoscopic gastrostomy was performed, and there were no further recurrences of infection after that.
Esophageal rupture can occur due to trauma, cervical operations, or during endoscopic examinations [
1]. It is a rare complication reported in 0.02% of patients after acute Anterior Cervical Discectomy and Fusion (ACDF) [
2]. However, there are no reports of rupture in patients with chronic ACDF. Symptoms of esophageal rupture can vary depending on the location. Lower esophageal rupture may present with chest pain, vomiting, and shortness of breath [
3], while upper esophageal rupture may cause neck pain, dysphonia, and hoarseness. However, in the case of our patient with a high-level complete cervical injury, an accurate perception and localization of pain was impossible. Musculoskeletal damage often leads to increased spasticity or neuropathic pain in areas where sensation is absent. Clinicians must, therefore, be cautious to detect systemic or localized pathologies the patient might not perceive.
Imaging findings of esophageal rupture typically include pleural effusion, pneumothorax, and subcutaneous emphysema [
4].Commonly, chest X-ray or chest CT scans reveal mediastinal or pleural symptoms. In the case of our patient, the chest X-ray showed no specific findings, and signs of infection were primarily in the posterolateral neck area without any symptoms of subcutaneous emphysema. The infection occurred deep within the cervical spine without any skin infection, which is different from the typical pattern of spinal osteomyelitis that usually involves the endplate and intervertebral disc first. We speculated that the infection spread to the epidural space and cervical muscles through the cervical fascia. Therefore, although esophageal rupture is rarely reported in chronic ACDF patients and is challenging to detect solely through imaging, it is crucial to consider this condition in the differential diagnosis of atypical deep cervical soft tissue infections.
Author Contributions
Conceptualization, J.P. and D.G.L.; methodology, D.G.L.; formal analysis, D.G.L.; investigation, J.P. and D.G.L.; writing—original draft preparation, J.P.; writing—review and editing, D.G.L.; visualization, J.P.; funding acquisition, D.G.L. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Basic Science Research Program though the National Research Funding of Korea (NRF) and funded by the Ministry of Education (2022R1I1A3071887).
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board of Yeungnam University (YUMC 2023-11-051 and date of approval; 1 December 2023).
Informed Consent Statement
Written informed consent has been obtained from the family members of patient to publish this paper.
Data Availability Statement
Data are available on a reasonable request from the authors.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Søreide, J.A.; Viste, A. Esophageal perforation: Diagnostic work-up and clinical decision-making in the first 24 hours. Scand. J. Trauma Resusc. Emerg. Med. 2011, 19, 66. [Google Scholar] [CrossRef] [PubMed]
- Hershman, S.H.; Kunkle, W.A.; Kelly, M.P.; Buchowski, J.M.; Ray, W.Z.; Bumpass, D.B.; Gum, J.L.; Peters, C.M.; Singhatanadgige, W.; Kim, J.Y. Esophageal perforation following anterior cervical spine surgery: Case report and review of the literature. Glob. Spine J. 2017, 7, 28S–36S. [Google Scholar] [CrossRef] [PubMed]
- Pate, J.W.; Walker, W.A.; Cole, F.H., Jr.; Owen, E.W.; Johnson, W.H. Spontaneous rupture of the esophagus: A 30-year experience. Ann. Thorac. Surg. 1989, 47, 689–692. [Google Scholar] [CrossRef] [PubMed]
- White, C.S.; Templeton, P.A.; Attar, S. Esophageal perforation: CT findings. AJR Am. J. Roentgenol. 1993, 160, 767–770. [Google Scholar] [CrossRef] [PubMed]
| Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).