Forced Straightening of the Back Does Not Improve Body Shape
Abstract
1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Methods
- a.
- In a corrected, active position, without a backrest (Figure 1). The corrected position was assumed in accordance with the examiner’s instructions. Attention was paid to the complete, active, and physiological alignment of the spine in a way that required the subject to exert the least amount of effort. The activities performed included lifting the sternum, increasing the anterior pelvic tilt, positioning the head at the axis of the spine, setting the shoulder blades in a physiological position, and slightly inclining the torso [37].
- b.
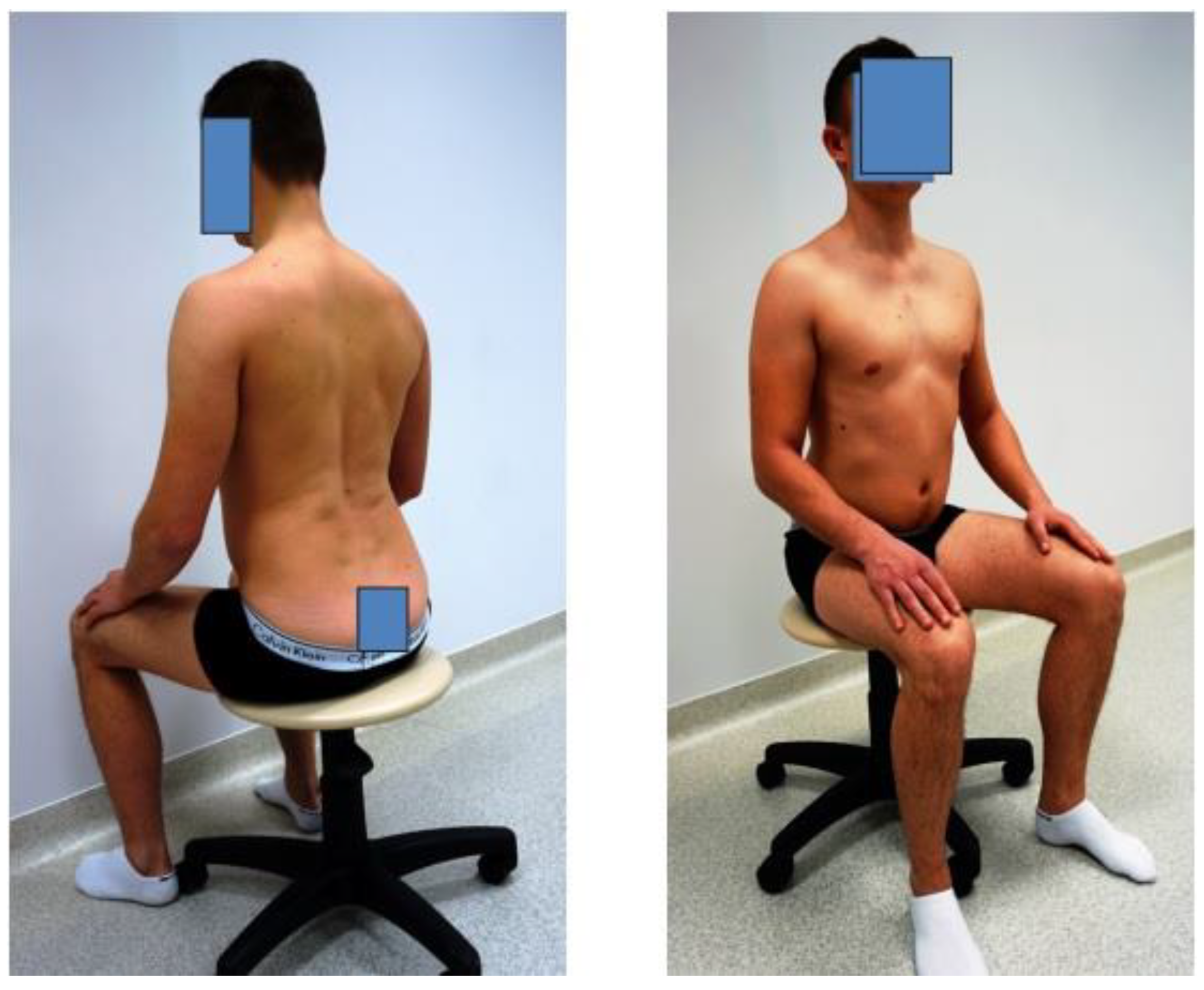
- In a forced position, where the instructions were as follows: “Sit up straight, intensively pull back your shoulder blades” (Figure 2).
- c.
- In a passive, free position without a backrest or muscle involvement and with posterior pelvic tilt; this is the so-called passive position (Figure 3).
- I.
- The angular parameters of the position of the sternum body (called the α angle) and the angular parameters of the sacrum position (called the β angle) in relation to the horizontal line, constituting the sagittal axis of the body. Saunders digital inclinometer (Baseline Digital Inclinometer Range of Movement Measurement Tool, New York, NY, USA) was used to conduct the assessment. The measuring tool that was used is characterized by a high measurement accuracy. The measurement resolution is 0.1 degrees, and the measurement accuracy is ±1 degree;
- II.
- The angular parameters of the thoracic spine curves (kyphosis angle called ω1) and lumbar spine curves (lordosis angle called ω2) measured using the DIERS Formetric 4D system (DICAM 3) (Figure 4). The resolution of the device is 0.01 degrees, and the accuracy is 0.25 degrees [39]. The DIERS system uses raster stereography, so it is free from any radiation. The DIERS Formetric is a light optical visualizing system based on video raster stereography. Therefore, the system comprises a light projector that creates a line grid on the back of the patient, which is noted with an imaging unit. Computer software evaluates the line bend and creates a three-dimensional model of the surface that is analogous to a plaster cast using the method of photogrammetry.
- (a)
- Of sacral angle and sternal angle: γ = β − α;
- (b)
- Of sternal angle and thoracic kyphosis: γ1 = 180 − (α + ω1);
- (c)
- Of sternal angle and lumbar lordosis: γ2 = 180 − (β + ω2).
2.3. Statistical Analysis
3. Results
3.1. Measured Angles Based on 3 Positions
3.2. Percentage Errors
3.3. Comparison of the Angle between Groups
3.4. Correlation between Angles
3.5. Confidence Intervals
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Waters, C.N.; Ling, E.P.; Chu, A.H.; Ng, S.H.; Chia, A.; Lim, Y.W.; Müller-Riemenschneider, F. Assessing and understanding sedentary behaviour in office-based working adults: A mixed-method approach. BMC Public Health 2016, 16, 360. [Google Scholar] [CrossRef] [PubMed]
- Harrison, D.D.; Harrison, S.O.; Croft, A.C.; Harrison, D.E.; Troyanovich, S.J. Sitting biomechanics part I: Review of the literature. J. Manip. Physiol. Ther. 1999, 22, 594–609. [Google Scholar] [CrossRef] [PubMed]
- O’Sullivan, K.; McCarthy, R.; White, A.; O’Sullivan, L.; Dankaerts, W. Lumbar posture and trunk muscle activation during a typing task when sitting on a novel dynamic ergonomic chair. Ergonomics 2012, 55, 1586–1595. [Google Scholar] [CrossRef] [PubMed]
- Claus, A.P.; Hides, J.A.; Moseley, G.L.; Hodges, P.W. Thoracic and lumbar posture behaviour in sitting tasks and standing: Progressing the biomechanics from observations to measurements. Appl. Ergon. 2016, 53, 161–168. [Google Scholar] [CrossRef] [PubMed]
- Toomingas, A.; Forsman, M.; Mathiassen, S.E.; Heiden, M.; Nilsson, T. Variation between seated and standing/walking postures among male and female call centre operators. BMC Public Health 2012, 12, 154. [Google Scholar] [CrossRef] [PubMed]
- Morvan, G.; Mathieu, P.; Vuillemin, V.; Guerini, H.; Bossard, P.; Zeitoun, F.; Wybier, M. Standardized way for imaging of the sagittal spinal balance. Eur. Spine J. 2011, 20, 602–608. [Google Scholar] [CrossRef] [PubMed]
- Win, A.M.; Yen, L.W.; Tan, K.H.; Lim, R.B.; Chia, K.S.; Mueller-Riemenschneider, F. Patterns of physical activity and sedentary behavior in a representative sample of a multi-ethnic South-East Asian population: A cross-sectional study. BMC Public Health 2015, 15, 318. [Google Scholar] [CrossRef]
- Diaz, K.M.; Howard, V.J.; Hutto, B.; Colabianchi, N.; Vena, J.E.; Safford, M.M.; Blair, S.N.; Hooker, S.P. Patterns of Sedentary Behavior and Mortality in U.S. Middle-Aged and Older Adults: A National Cohort Study. Ann. Intern. Med. 2017, 167, 465–475. [Google Scholar] [CrossRef]
- Matthews, C.E.; Chen, K.Y.; Freedson, P.S.; Buchowski, M.S.; Beech, B.M.; Pate, R.R.; Troiano, R.P. Amount of time spent in sedentary behaviors in the United States, 2003–2004. Am. J. Epidemiol. 2008, 167, 875–881. [Google Scholar] [CrossRef]
- Zimmerman, F.J.; Christakis, D.A.; Meltzoff, A.N. Television and DVD/video viewing in children younger than 2 years. Arch. Pediatr. Adolesc. Med. 2007, 161, 473–479. [Google Scholar] [CrossRef]
- Arundell, L.; Salmon, J.; Koorts, H.; Contardo Ayala, A.M.; Timperio, A. Exploring when and how adolescents sit: Cross-sectional analysis of activPAL-measured patterns of daily sitting time, bouts and breaks. BMC Public Health 2019, 19, 653. [Google Scholar] [CrossRef] [PubMed]
- Fischer-Grote, L.; Kothgassner, O.D.; Felnhofer, A. Risk factors for problematic smartphone use in children and adolescents: A review of existing literature. Neuropsychiatry 2019, 33, 179–190. [Google Scholar] [CrossRef] [PubMed]
- Parrish, A.M.; Trost, S.G.; Howard, S.J.; Batterham, M.; Cliff, D.; Salmon, J.; Okely, A.D. Evaluation of an intervention to reduce adolescent sitting time during the school day: The ‘Stand Up for Health’ randomised controlled trial. J. Sci. Med. Sport 2018, 21, 1244–1249. [Google Scholar] [CrossRef] [PubMed]
- Dunstan, D.W.; Salmon, J.; Owen, N.; Armstrong, T.; Zimmet, P.Z.; Welborn, T.A.; Cameron, A.J.; Dwyer, T.; Jolley, D.; Shaw, J.E.; et al. Associations of TV viewing and physical activity with the metabolic syndrome in Australian adults. Diabetologia 2005, 48, 2254–2261. [Google Scholar] [CrossRef] [PubMed]
- Edwards, J. The importance of postural habits in perpetuating myofascial trigger point pain. Acupunct. Med. 2005, 23, 77–82. [Google Scholar] [CrossRef] [PubMed]
- Czaprowski, D.; Leszczewska, J.; Sitarski, D. Does “ideal” sitting position exist? Adv. Rehabil. 2014, 28, 47–54. (In Polish) [Google Scholar] [CrossRef]
- Scannell, J.P.; McGill, S.M. Lumbar posture-should it, and can it, be modified? A study of passive tissue stiffness and lumbar position during activities of daily living. Phys. Ther. 2003, 83, 907–917. [Google Scholar] [CrossRef]
- O’Sullivan, P.B.; Dankaerts, W.; Burnett, A.F.; Farrell, G.T.; Jefford, E.; Naylor, C.S.; O’Sullivan, K.J. Effect of different upright sitting postures on spinal-pelvic curvature and trunk muscle activation in a pain-free population. Spine 2006, 31, 707–712. [Google Scholar] [CrossRef]
- Kebaetse, M.; McClure, P.; Pratt, N.A. Thoracic position effect on shoulder range of motion, strength, and three-dimensional scapular kinematics. Arch. Phys. Med. Rehabil. 1999, 80, 945–950. [Google Scholar] [CrossRef]
- Hey, H.W.; Wong, C.G.; Lau, E.T.; Tan, K.A.; Lau, L.L.; Liu, K.G.; Wong, H.K. Differences in erect sitting and natural sitting spinal alignment-insights into a new paradigm and implications in deformity correction. Spine J. 2017, 17, 183–189. [Google Scholar] [CrossRef]
- Pynt, J.; Higgs, J.; Mackey, M. Historical perspective milestones in the evolution of lumbar spinal postural health in seating. Spine 2002, 27, 2180–2189. [Google Scholar] [CrossRef] [PubMed]
- Søndergaard, K.H.; Olesen, C.G.; Søndergaard, E.K.; de Zee, M.; Madeleine, P. The variability and complexity of sitting postural control are associated with discomfort. J. Biomech. 2010, 43, 1997–2001. [Google Scholar] [CrossRef] [PubMed]
- Massaccesi, M.; Pagnotta, A.; Soccetti, A.; Masali, M.; Masiero, C.; Greco, F. Investigation of work-related disorders in truck drivers using RULA method. Appl. Ergon. 2003, 34, 303–307. [Google Scholar] [CrossRef] [PubMed]
- Gascon, S.S.; Gilmer, G.G.; Hanks, M.M.; Washington, J.K.; Oliver, G.D. Biomechanical influences of a postural compression garment on scapular positioning. Int. J. Sports Phys. Ther. 2018, 13, 700–706. [Google Scholar] [CrossRef] [PubMed]
- Dolan, K.J.; Green, A. Lumbar spine reposition sense: The effect of a ‘slouched’ posture. Man. Ther. 2006, 11, 202–207. [Google Scholar] [CrossRef] [PubMed]
- Womersley, L.; May, S. Sitting posture of subjects with postural backache. J. Manip. Physiol. Ther. 2006, 29, 213–218. [Google Scholar] [CrossRef] [PubMed]
- Gogola, A.; Saulicz, E.; Matyja, M.; Myśliwiec, A.; Tuczyńska, A.; Kuszewski, M.; Gutowska, A. Analysis of the relationship between the quality of body posture and occlusion in children and adolescents. Fizjoterapia Pol. 2015, 15, 52–58. [Google Scholar]
- Simão, S.S.S.; Romero, V.U.; Baraldil, K.; Oda, A.L.; Viana, C.F.; de Magalhães Leal Chiappetta, A.L.; Pieri, A. Clinical evaluation of the relationship of posture, breathing and swallowing in chronic-state post-stroke patients: Case report. Rev. CEFAC 2013, 15, 1371–1378. [Google Scholar] [CrossRef][Green Version]
- Peeters, G.M.; Burton, N.W.; Brown, W.J. Associations between sitting time and a range of symptoms in mid-age women. Prev. Med. 2013, 56, 135–141. [Google Scholar] [CrossRef]
- Li, C.; Zhao, Y.; Yu, Z.; Han, X.; Lin, X.; Wen, L. Sagittal imbalance of the spine is associated with poor sitting posture among primary and secondary school students in China: A cross-sectional study. BMC Musculoskelet. Disord. 2022, 23, 98. [Google Scholar] [CrossRef]
- Czaprowski, D.; Pawłowska, P.; Stoliński, L.; Kotwicki, T. Active self-correction of back posture in children instructed with ‘straighten your back’ command. Man. Ther. 2014, 19, 392–398. [Google Scholar] [CrossRef] [PubMed]
- Kiebzak, W.P.; Żurawski, A.Ł.; Kosztołowicz, M. Alignment of the Sternum and Sacrum as a Marker of Sitting Body Posture in Children. Int. J. Environ. Res. Public Health 2022, 19, 16287. [Google Scholar] [CrossRef] [PubMed]
- Caneiro, J.P.; O’Sullivan, P.; Burnett, A.; Barach, A.; O’Neil, D.; Tveit, O.; Olafsdottir, K. The influence of different sitting postures on head/neck posture and muscle activity. Man. Ther. 2010, 15, 54–60. [Google Scholar] [CrossRef] [PubMed]
- Gunning, J.L.; Callaghan, J.P.; McGill, S.M. Spinal posture and prior loading history modulate compressive strength and type of failure in the spine: A biomechanical study using a porcine cervical spine model. Clin. Biomech. 2001, 16, 471–480. [Google Scholar] [CrossRef]
- Driscoll, C.R.; Aubin, C.E.; Canet, F.; Dansereau, J.; Labelle, H. The impact of intra-operative sternum vertical displacement on the sagittal curves of the spine. Eur. Spine J. 2010, 19, 421–426. [Google Scholar] [CrossRef][Green Version]
- Vaz, G.; Roussouly, P.; Berthonnaud, E.; Dimnet, J. Sagittal morphology and equilibrium of pelvis and spine. Eur. Spine J. 2002, 11, 80–87. [Google Scholar] [CrossRef]
- Kiebzak, W.; Dwornik, M.; Żurawska, J.; Żurawski, A. sEMG assessment of the activity of the rectus abdominis and multifidus muscles in different sitting postures. Pol. J. Physiother. 2017, 17, 52–62. [Google Scholar]
- Mork, P.J.; Westgaard, R.H. Back posture and low back muscle activity in female computer workers: A field study. Clin. Biomech. 2009, 24, 169–175. [Google Scholar] [CrossRef]
- Drerup, B.; Ellger, B.; Meyer zu Bentrup, F.; Hierholzer, E. Rasterstereographische Funktionsaufnahmen. Orthopäde 2001, 30, 242–250. [Google Scholar] [CrossRef]
- Claus, A.P.; Hides, J.A.; Moseley, G.L.; Hodges, P.W. Is ‘ideal’ sitting posture real? Measurement of spinal curves in four sitting postures. Man. Ther. 2009, 14, 404–408. [Google Scholar] [CrossRef]
- Kendall, F.; McCreary, E.; Provance, P.G.; Rodgers, M.; Romani, W.A. Muscle Testing and Function with Posture and Pain; Lippincott Williams & Wilkins: Baltimore, MD, USA, 2005. [Google Scholar]
- Kamaci, S.; Yucekul, A.; Demirkiran, G.; Berktas, M.; Yazici, M. The Evolution of Sagittal Spinal Alignment in Sitting Position During Childhood. Spine 2015, 40, 787–793. [Google Scholar] [CrossRef] [PubMed]
- Kamali, F.; Shirazi, S.A.; Ebrahimi, S.; Mirshamsi, M.; Ghanbari, A. Comparison of manual therapy and exercise therapy for postural hyperkyphosis: A randomized clinical trial. Physiother. Theory Pract. 2016, 32, 92–97. [Google Scholar] [CrossRef] [PubMed]
- Junges, S.; Dias, R.; Sartori, J.; Ferreira, L.; Gomes da Silva, I. Change in pressure expiratory with the use of the method Pilates in adult women with hyperkyphosis. Fisioter Bras. 2017, 18, 643–649. [Google Scholar]
- Tribus, C.B. Scheuermann’s kyphosis in adolescents and adults: Diagnosis and management. J. Am. Acad. Orthop. Surg. 1998, 6, 36–43. [Google Scholar] [CrossRef] [PubMed]
- Lowe, T.G. Scheuermann’s kyphosis. Neurosurg. Clin. N. Am. 2007, 18, 305–315. [Google Scholar] [CrossRef] [PubMed]
- Nilsson, C.; Wykman, A.; Leanderson, J. Spinal sagittal mobility and joint laxity in young ballet dancers. A comparative study between first-year students at the Swedish Ballet School and a control group. Knee Surg. Sports Traumatol. Arthrosc. 1993, 1, 206–208. [Google Scholar] [CrossRef]
- Clément, J.L.; Geoffray, A.; Yagoubi, F.; Chau, E.; Solla, F.; Oborocianu, I.; Rampal, V. Relationship between thoracic hypokyphosis, lumbar lordosis and sagittal pelvic parameters in adolescent idiopathic scoliosis. Eur. Spine J. 2013, 22, 2414–2420. [Google Scholar] [CrossRef]
- Kotwicki, T. Sagittal and transversal plane deformity in thoracic scoliosis. Stud. Health Technol. Inform. 2002, 91, 251–256. [Google Scholar]
- Yong, Q.; Zhen, L.; Zezhang, Z.; Bangping, Q.; Feng, Z.; Tao, W.; Jun, J.; Xu, S.; Xusheng, Q.; Weiwei, M.; et al. Comparison of sagittal spinopelvic alignment in Chinese adolescents with and without idiopathic thoracic scoliosis. Spine 2012, 37, 714–720. [Google Scholar] [CrossRef]
- Legaye, J.; Duval-Beaupere, G.; Hecquet, J.; Marty, C. Pelvic incidence: A fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur. Spine J. 1998, 7, 99–103. [Google Scholar] [CrossRef]
- Mac-Thiong, J.; Labelle, H.; Berthonnaud, E.; Betz, R.R.; Roussouly, P. Sagittal spinopelvic balance in normal children and adolescents. Eur. Spine J. 2007, 16, 227–234. [Google Scholar] [CrossRef] [PubMed]
- Marty, C.; Boisaubert, B.; Descamps, H.; Montigny, J.; Hecquet, J.; Legaye, J.; Duval-Beaupere, G. The sagittal anatomy of the sacrum among young adults, infants, and spondylolisthesis patients. Eur. Spine J. 2002, 22, 119–125. [Google Scholar] [CrossRef] [PubMed]
- Zmyślna, A.; Kiebzak, W.; Żurawski, A.; Pogorzelska, J.; Kotela, I.; Kowalski, T.J.; Śliwiński, Z.; Śliwiński, G. Effect of physiotherapy on spinal alignment in children with postural defects. Int. J. Occup. Med. Environ. Health 2019, 32, 25–32. [Google Scholar] [CrossRef] [PubMed]
- Ghandhari, H.; Hesarikia, H.; Ameri, E.; Noori, A. Assessment of normal sagittal alignment of the spine and pelvis in children and adolescents. Biomed. Res. Int. 2013, 2013, 842624. [Google Scholar] [CrossRef]
- Kiebzak, W.P. Application of Euclidean geometry in the assessment of body posture in a sitting position. Pol. Ann. Med. 2022, 29, 167–171. [Google Scholar] [CrossRef]
- Żurawski, A.; Śliwiński, Z.; Nowak-Starz, G.; Kiebzak, W.P. Monitoring changes in the shape of the spine in children with postural disorders. Med. Stud. Stud. Med. 2023, 39, 132–139. [Google Scholar] [CrossRef]
- Weiss, H.R.; Werkmann, M. Unspecific chronic low back pain—A simple functional classification tested in a case series of patients with spinal deformities. Scoliosis 2009, 4, 4–10. [Google Scholar] [CrossRef]




| Corrected Position | Forced Position | Passive Position | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M (SD) | Median | Mode | Min | Max | M (SD) | Median | Mode | Min | Max | M (SD) | Median | Mode | Min | Max | |
| α | 64.20 (2.44) | 64.00 | 65.00 | 60.00 | 69.70 | 70.52 (11.05) | 74.10 | 74.90 | 47.30 | 88.30 | 84.19 (11.02) | 83.20 | 91.00 | 58.20 | 111.60 |
| β | 113.39 (4.98) | 113.40 | 1150 | 100.0 | 127.0 | 91.22 (8.83) | 89.70 | 87.40 | 74.10 | 125.50 | 81.64 (10.82) | 80.20 | 72.00 | 62.00 | 118.80 |
| ω1 | 41.39 (4.33) | 41.73 | 41.50 | 26.46 | 49.70 | 43.41 (13.74) | 47.00 | 55.20 | 12.30 | 70.90 | 57.57 (13.34) | 59.00 | 63.30 | 20.50 | 89.00 |
| ω2 | 37.68 (3.51) | 37.68 | 38.60 | 28.30 | 46.60 | 12.77 (12.31) | 11.40 | 4.30 | −15.80 | 39.90 | −5.14 (15.87) | −6.90 | −27.30 | −39.25 | 38.40 |
| ϒ | 49.19 (5.38) | 49.00 | 48.00 | 34.60 | 61.30 | 20.70 (15.83) | 17.70 | −5.40 | −9.40 | 65.20 | −2.54 (17.64) | −3.30 | 1.00 | −46.70 | 44.00 |
| ϒ1 | 74.41 (4.84) | 74.50 | 73.40 | 62.50 | 87.40 | 66.06 (22.60) | 63.50 | 51.00 | 27.30 | 114.80 | 38.24 (19.78) | 39.50 | 15.40 | −10.50 | 93.20 |
| ϒ2 | 78.11 (4.14) | 78.10 | 77.60 | 66.00 | 88.20 | 96.70 (15.40) | 96.60 | 112.30 | 62.90 | 136.70 | 100.96 (15.59) | 101.90 | 108.8 0 | 61.80 | 139.40 |
| Corrected Position | Forced Position | Passive Position | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Me,t (°) | Me,emp (°) | Ep% (%) | Me,t (°) | Me,emp (°) | Ep% (%) | Me,t (°) | Me,emp (°) | Ep% (%) | |
| ϒ | 49.19 | 49.00 | 0.40 | 20.70 | 17.70 | 16.38 | −2.54 | −3.30 | 22.22 |
| ϒ1 | 74.41 | 74.50 | 0.26 | 66.06 | 63.50 | 4.92 | 38.24 | 39.50 | 3.40 |
| ϒ2 | 78.11 | 78.10 | 0.12 | 96.70 | 96.60 | 0.31 | 100.96 | 101.90 | 0.99 |
| Angle | Corrected Position a | Forced Position b | Passive Position c | F | p | Post Hoc |
|---|---|---|---|---|---|---|
| α | 64.20 ± 2.44 | 70.52 ± 11.05 | 84.19 ± 11.02 | 334.752 | 0.000 | a < b < c |
| β | 113.39± 4.98 | 91.22 ± 8.83 | 81.64 ± 10.82 | 161.445 | 0.000 | a > b = c |
| ω1 | 41.39 ± 4.33 | 43.41 ± 13.74 | 57.57 ± 13.34 | 965.185 | 0.000 | a < b < c |
| ω2 | 37.65 ± 3.51 | 12.77 ± 12.31 | −5.14 ± 15.87 | 890.653 | 0.000 | a > b > c |
| ϒ | 49.19 ± 5.38 | 20.70 ± 15.83 | −2.54 ± 17.64 | 909.821 | 0.000 | a > b > c |
| ϒ1 | 74.41 ± 4.84 | 66.06 ± 22.60 | 38.24 ± 19.78 | 310.125 | 0.000 | a > b > c |
| ϒ2 | 78.11 ± 4.14 | 96.70 ± 15.40 | 100.96 ± 15.59 | 237.499 | 0.000 | a < b < c |
| Common Sense | Angle | Corrected Position | Forced Position | Passive Position |
|---|---|---|---|---|
| ϒ | α | −0.391 * | −0.843 * | −0.812 * |
| β | 0.892 * | 0.737 * | 0.801 * | |
| ϒ1 | α | −0.130 * | −0.890 * | −0.763 * |
| ω1 | −0.134 * | −0.930 * | −0.844 * | |
| ϒ2 | β | −0.210 * | −0.411 * | −0.441 * |
| ω2 | −0.811 * | −0.705 * | −0.751 * |
| 90% CI in the Corrected Position | 90% CI in the Forced Position | 90% CI in the Passive Position | |
|---|---|---|---|
| α | 61.00–67.90 | 52.8–83.25 | 70.95–99.05 |
| β | 107.10–119.70 | 81.12–102.60 | 68.70–96.20 |
| ω1 | 35.30–46.82 | 26.10–58.56 | 39.09–73.16 |
| ω2 | 32.67–42.02 | −4.32–29.92 | −24.52–17.30 |
| ϒ | 42.15–56.55 | 0.68–41.88 | −26.00–20.65 |
| ϒ1 | 68.04–81.06 | 38.52–98.60 | 12.35–65.17 |
| ϒ2 | 72.57–83.99 | 76.42–116.55 | 79.95–120.66 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kiebzak, W.P.; Ha, S.-Y.; Kosztołowicz, M.; Żurawski, A. Forced Straightening of the Back Does Not Improve Body Shape. Diagnostics 2024, 14, 250. https://doi.org/10.3390/diagnostics14030250
Kiebzak WP, Ha S-Y, Kosztołowicz M, Żurawski A. Forced Straightening of the Back Does Not Improve Body Shape. Diagnostics. 2024; 14(3):250. https://doi.org/10.3390/diagnostics14030250
Chicago/Turabian StyleKiebzak, Wojciech Piotr, Sun-Young Ha, Michał Kosztołowicz, and Arkadiusz Żurawski. 2024. "Forced Straightening of the Back Does Not Improve Body Shape" Diagnostics 14, no. 3: 250. https://doi.org/10.3390/diagnostics14030250
APA StyleKiebzak, W. P., Ha, S.-Y., Kosztołowicz, M., & Żurawski, A. (2024). Forced Straightening of the Back Does Not Improve Body Shape. Diagnostics, 14(3), 250. https://doi.org/10.3390/diagnostics14030250







