Two-Stage Lumbar Dynamic Stabilization Surgery: A Comprehensive Analysis of Screw Loosening Rates and Functional Outcomes Compared to Single-Stage Approach in Osteopenic and Osteoporotic Patients
Abstract
1. Introduction
2. Methods
2.1. Study Approval
2.2. Study Design
2.3. Radiological Analysis
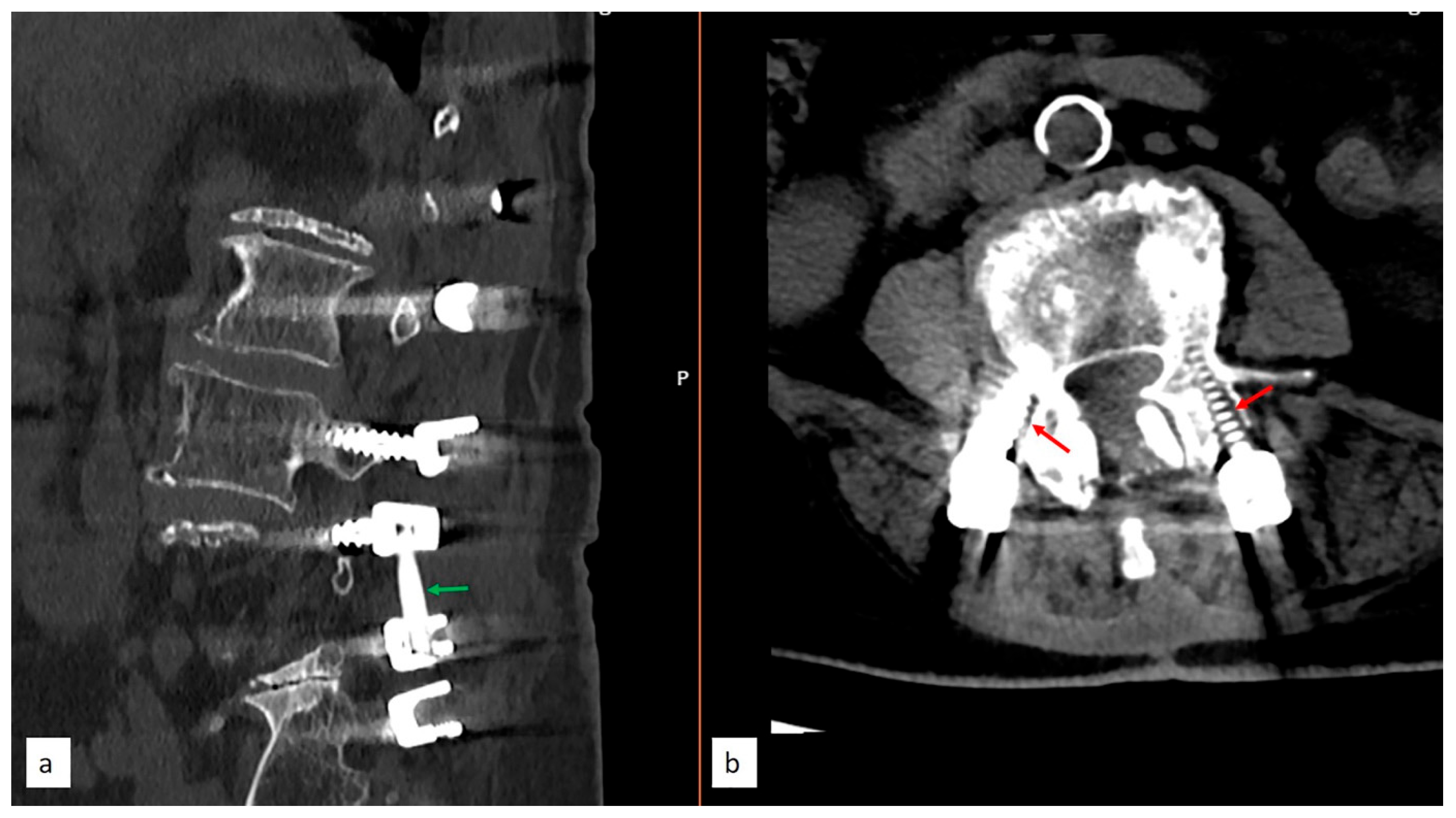
2.4. Surgical Technique and Nuances
2.5. Statistical Analysis
3. Results
- Patient Characteristics
- 2.
- Distribution of Screw Loosening across Surgical Levels and Sections
- 3.
- Rate of Screw Loosening
- 4.
- Clinical Outcomes and Complications
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Khalifé, M.; Devriese, F.; Ferrero, E.; Zadegan, F.; Ajavon, L.; Mazel, C. Dynesys® dynamic stabilization outcomes in degenerative spine surgery. Acta Orthop. Belg. 2021, 87, 795–803. [Google Scholar] [CrossRef]
- Li, T.; Yan, J.; Ren, Q.; Hu, J.; Wang, F.; Liu, X. Efficacy and Safety of Lumbar Dynamic Stabilization Device Coflex for Lumbar Spinal Stenosis: A Systematic Review and Meta-analysis. World Neurosurg. 2023, 170, 7–20. [Google Scholar] [CrossRef]
- Rienmüller, A.C.; Krieg, S.M.; Schmidt, F.A.; Meyer, E.L.; Meyer, B. Reoperation rates and risk factors for revision 4 years after dynamic stabilization of the lumbar spine. Spine J. 2019, 19, 113–120. [Google Scholar] [CrossRef] [PubMed]
- Peng, B.-G.; Gao, C.-H. Is Dynesys dynamic stabilization system superior to posterior lumbar fusion in the treatment of lumbar degenerative diseases? World J. Clin. Cases 2020, 8, 5496–5500. [Google Scholar] [CrossRef] [PubMed]
- Kocak, T.; Cakir, B.; Reichel, H.; Mattes, T. Screw loosening after posterior dynamic stabilization—Review of the literature. Acta Chir. Orthop. Traumatol. Cechoslov. 2010, 77, 134–139. [Google Scholar] [CrossRef]
- Wu, X.; Shi, J.; Wu, J.; Cheng, Y.; Peng, K.; Chen, J.; Jiang, H. Pedicle screw loosening: The value of radiological imagings and the identification of risk factors assessed by extraction torque during screw removal surgery. J. Orthop. Surg. Res. 2019, 14, 6. [Google Scholar] [CrossRef]
- Bokov, A.; Bulkin, A.; Aleynik, A.; Kutlaeva, M.; Mlyavykh, S. Pedicle Screws Loosening in Patients With Degenerative Diseases of the Lumbar Spine: Potential Risk Factors and Relative Contribution. Glob. Spine J. 2018, 9, 55–61. [Google Scholar] [CrossRef]
- Aycan, M.; Demir, T.F. Toggling effect on pullout performance of pedicle screws: Review. Int. Adv. Res. Eng. J. 2020, 4, 161–172. [Google Scholar] [CrossRef]
- Wray, S.; Mimran, R.; Vadapalli, S.; Shetye, S.S.; McGilvray, K.C.; Puttlitz, C.M. Pedicle screw placement in the lumbar spine: Effect of trajectory and screw design on acute biomechanical purchase. J. Neurosurg. Spine 2015, 22, 503–510. [Google Scholar] [CrossRef] [PubMed]
- Mu, S.; Wang, J.; Gong, S. Mechanical Analysis of Posterior Pedicle Screw System Placement and Internal Fixation in the Treatment of Lumbar Fractures. Comput. Math. Methods Med. 2022, 2022, 6497754. [Google Scholar] [CrossRef] [PubMed]
- Song, M.; Sun, K.; Li, Z.; Zong, J.; Tian, X.; Ma, K.; Wang, S. Stress distribution of different lumbar posterior pedicle screw insertion techniques: A combination study of finite element analysis and biomechanical test. Sci. Rep. 2021, 11, 12968. [Google Scholar] [CrossRef] [PubMed]
- Jendoubi, K.; Khadri, Y.; Bendjaballah, M.; Slimane, N. Effects of the Insertion Type and Depth on the Pedicle Screw Pullout Strength: A Finite Element Study. Appl. Bionics Biomech. 2018, 2018, 1460195. [Google Scholar] [CrossRef] [PubMed]
- Chang, H.K.; Ku, J.; Ku, J.; Kuo, Y.H.; Chang, C.C.; Wu, C.L.; Lirng, J.F.; Wu, J.C.; Huang, W.C.; Cheng, H.; et al. Correlation of bone density to screw loosening in dynamic stabilization: An analysis of 176 patients. Sci. Rep. 2021, 11, 17519. [Google Scholar] [CrossRef] [PubMed]
- Özer, A.F.; Başak, A.T.; Özbek, M.A.; Hekimoğlu, M.; Aydın, A.L.; Ateş, Ö.; Günerbüyük, C.; Akgül, T.; Sasani, M.; Öktenoğlu, T. Lumbar Dynamic Stabilization With 2-Stage Surgery: Early Results. Int. J. Spine Surg. 2022, 16, 638–645. [Google Scholar] [CrossRef] [PubMed]
- Rometsch, E.; Spruit, M.; Zigler, J.E.; Menon, V.K.; Ouellet, J.A.; Mazel, C.; Härtl, R.; Espinoza, K.; Kandziora, F. Screw-Related Complications After Instrumentation of the Osteoporotic Spine: A Systematic Literature Review With Meta-Analysis. Glob. Spine J. 2019, 10, 69–88. [Google Scholar] [CrossRef] [PubMed]
- Noordeen, S.; Fleming, C.; Gokulakrishnan, R.; Sivanandan, M.H. The Functional Outcome of Surgical Management of Spondylolisthesis with Posterior Stabilization and Fusion. J. Orthop. Case Rep. 2024, 14, 119–124. [Google Scholar] [CrossRef] [PubMed]
- Guan, J.; Liu, T.; Yu, X.; Li, W.; Feng, N.; Jiang, G.; Zhao, H.; Yang, Y. Biomechanical and clinical research of Isobar semi-rigid stabilization devices for lumbar degenerative diseases: A systematic review. Biomed. Eng. Online 2023, 22, 95. [Google Scholar] [CrossRef]
- Galbusera, F.; Volkheimer, D.; Reitmaier, S.; Berger-Roscher, N.; Kienle, A.; Wilke, H.-J. Pedicle screw loosening: A clinically relevant complication? Eur. Spine J. 2015, 24, 1005–1016. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.-C.; Huang, W.-C.; Tsai, H.-W.; Ko, C.-C.; Wu, C.-L.; Tu, T.-H.; Cheng, H. Pedicle screw loosening in dynamic stabilization: Incidence, risk, and outcome in 126 patients. Neurosurg. Focus 2011, 31, E9. [Google Scholar] [CrossRef]
- Kuo, C.-H.; Chang, P.-Y.; Tu, T.-H.; Fay, L.-Y.; Chang, H.-K.; Wu, J.-C.; Huang, W.-C.; Cheng, H. The Effect of Lumbar Lordosis on Screw Loosening in Dynesys Dynamic Stabilization: Four-Year Follow-Up with Computed Tomography. BioMed Res. Int. 2015, 2015, 152435. [Google Scholar] [CrossRef]
- Akgun, M.Y.; Toklu, S.; Gunerbuyuk, C.; Ates, O.; Aydin, A.L.; Baran, O.; Oktenoglu, T.; Sasani, M.; Ozer, A.F. Foraminoplasty with Partial Pediculectomy in Degenerative Spondylolisthesis Cases with Nerve Compression. World Neurosurg. 2023, 172, e532–e539. [Google Scholar] [CrossRef]
- Lee, C.-H.; Jahng, T.-A.; Hyun, S.-J.; Kim, C.H.; Park, S.-B.; Kim, K.-J.; Chung, C.K.; Kim, H.-J.; Lee, S.-E. Dynamic stabilization using the Dynesys system versus posterior lumbar interbody fusion for the treatment of degenerative lumbar spinal disease: A clinical and radiological outcomes-based meta-analysis. Neurosurg. Focus 2016, 40, E7. [Google Scholar] [CrossRef] [PubMed]
- Ohtonari, T.; Nishihara, N.; Suwa, K.; Ota, T.; Koyama, T. Dynamic stabilization for degenerative spondylolisthesis and lumbar spinal instability. Neurol. Med.-Chir. 2014, 54, 698–706. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kanno, H.; Onoda, Y.; Hashimoto, K.; Aizawa, T.; Ozawa, H. Innovation of Surgical Techniques for Screw Fixation in Patients with Osteoporotic Spine. J. Clin. Med. 2022, 11, 2577. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.; Shi, L.; Liu, D.; Wu, Z.; Gao, P.; Liu, W.; Li, X.; Guo, Z. Evaluating Screw Stability After Pedicle Screw Fixation With PEEK Rods. Glob. Spine J. 2021, 13, 393–399. [Google Scholar] [CrossRef] [PubMed]
- Xu, F.; Zhou, S.; Zou, D.; Li, W.; Sun, Z.; Jiang, S. The relationship between S1 screw loosening and postoperative outcome in patients with degenerative lumbar scoliosis. BMC Musculoskelet. Disord. 2022, 23, 186. [Google Scholar] [CrossRef] [PubMed]
- Banno, T.; Hasegawa, T.; Yamato, Y.; Togawa, D.; Yoshida, G.; Kobayashi, S.; Yasuda, T.; Arima, H.; Oe, S.; Mihara, Y.; et al. Multi-Rod Constructs Can Increase the Incidence of Iliac Screw Loosening after Surgery for Adult Spinal Deformity. Asian Spine J. 2019, 13, 500–510. [Google Scholar] [CrossRef] [PubMed]
- Panjabi, M.M. The stabilizing system of the spine. Part II. Neutral zone and instability hypothesis. J. Spinal Disord. 1992, 5, 390–396. [Google Scholar] [CrossRef] [PubMed]
- Parithimarkalaignan, S.; Padmanabhan, T.V. Osseointegration: An update. J. Indian Prosthodont. Soc. 2013, 13, 2–6. [Google Scholar] [CrossRef]
- Rowe, P.; Koller, A.; Sharma, S. Physiology, Bone Remodeling. [Updated 17 March 2023]. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2024. [Google Scholar] [PubMed]
- Mavčič, B.; Antolič, V. Optimal mechanical environment of the healing bone fracture/osteotomy. Int. Orthop. 2012, 36, 689–695. [Google Scholar] [CrossRef]
- Sheen, J.R.; Mabrouk, A.; Garla, V.V. Fracture Healing Overview. [Updated 8 April 2023 ]. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2024. [Google Scholar] [PubMed]
- Xu, F.; Zou, D.; Li, W.; Sun, Z.; Jiang, S.; Zhou, S.; Li, Z. Hounsfield units of the vertebral body and pedicle as predictors of pedicle screw loosening after degenerative lumbar spine surgery. Neurosurg. Focus 2020, 49, E10. [Google Scholar] [CrossRef] [PubMed]
- Cornaz, F.; Farshad, M.; Widmer, J. Location of pedicle screw hold in relation to bone quality and loads. Front. Bioeng. Biotechnol. 2022, 10, 953119. [Google Scholar] [CrossRef]
- Mizuno, T.; Kasai, Y.; Sakakibara, T.; Yoshikawa, T.; Inaba, T. Biomechanical study of rotational micromovement of the pedicle screw. SpringerPlus 2016, 5, 1016. [Google Scholar] [CrossRef] [PubMed][Green Version]
- El-Rich, M.; Arnoux, P.-J.; Wagnac, E.; Brunet, C.; Aubin, C.-E. Finite element investigation of the loading rate effect on the spinal load-sharing changes under impact conditions. J. Biomech. 2009, 42, 1252–1262. [Google Scholar] [CrossRef]
- Wu, Z.-X.; Gong, F.-T.; Liu, L.; Ma, Z.-S.; Zhang, Y.; Zhao, X.; Yang, M.; Lei, W.; Sang, H.-X. A comparative study on screw loosening in osteoporotic lumbar spine fusion between expandable and conventional pedicle screws. Arch. Orthop. Trauma Surg. 2011, 132, 471–476. [Google Scholar] [CrossRef]
- Mustafy, T.; Arnoux, P.-J.; Benoit, A.; Bianco, R.-J.; Aubin, C.-E.; Villemure, I. Load-sharing biomechanics at the thoracolumbar junction under dynamic loadings are modified by anatomical features in adolescent and pediatric vs adult functional spinal units. J. Mech. Behav. Biomed. Mater. 2018, 88, 78–91. [Google Scholar] [CrossRef]
- Hekimoğlu, M.; Başak, A.; Yılmaz, A.; Yıldırım, H.; Aydın, A.L.; Karadag, K.; Özer, A.F. Adjacent Segment Disease (ASD) in Incidental Segmental Fused Vertebra and Comparison With the Effect of Stabilization Systems on ASD. Cureus 2021, 13, e18647. [Google Scholar] [CrossRef] [PubMed]
- Stam, W.T.; Deunk, J.; Elzinga, M.J.; Bloemers, F.W.; Giannakopoulos, G.F. The Predictive Value of the Load Sharing Classification Concerning Sagittal Collapse and Posterior Instrumentation Failure: A Systematic Literature Review. Glob. Spine J. 2019, 10, 486–492. [Google Scholar] [CrossRef]
- Costăchescu, B.; Niculescu, A.-G.; Grumezescu, A.M.; Teleanu, D.M. Screw Osteointegration-Increasing Biomechanical Resistance to Pull-Out Effect. Materials 2023, 16, 5582. [Google Scholar] [CrossRef]
- Javed, F.; Ahmed, H.B.; Crespi, R.; Romanos, G.E. Role of primary stability for successful osseointegration of dental implants: Factors of influence and evaluation. Interv. Med. Appl. Sci. 2013, 5, 162–167. [Google Scholar] [CrossRef]
- Lopez, C.D.; Alifarag, A.M.; Torroni, A.; Tovar, N.; Diaz-Siso, J.R.; Witek, L.; Rodriguez, E.D.; Coelho, P.G. Osseodensification for enhancement of spinal surgical hardware fixation. J. Mech. Behav. Biomed. Mater. 2017, 69, 275–281. [Google Scholar] [CrossRef] [PubMed]



| Characteristics | Two-Stage Procedure (n = 52) | Single-Stage Procedure (n = 67) | p-Value |
|---|---|---|---|
| Age (years) | 57.09 ± 4.54 | 58.92 ± 4.84 | t 0.343 |
| Age Groups | |||
| 2 (3.8%) | 3 (4.5%), | b 0.975 |
| 21 (40.4%), | 26 (38.8%) | |
| 29 (55.8%) | 38 (56.7%) | |
| Gender | |||
| 34 (65.4%) | 47 (70.1%) | b 0.580 |
| 18 (34.6%) | 20 (29.9%) | |
| Comorbidities | |||
| 9 (17.3%) | 8 (11.9%) | b 0.407 |
| 43 (82.7%) | 59 (88.1%) | |
| T-score Mean | −2.39 ± 0.47 | −2.45 ± 0.45 | t 0.453 |
| Age Groups (Steroid Users) | |||
| <50 years | 2 (22.2%) | 3 (37.5%) | f 0.142 |
| 50–60 years | 3 (33.3%) | 5 (62.5%) | |
| 60–85 years | 4 (44.4%) | 0 | |
| Age Groups (Degenerative Disk Disease) | |||
| <50 years | 0 | 0 | |
| 50–60 years | 14 (32.6%) | 21 (35.6%) | b 0.750 |
| 60–85 years | 29 (32.6%) | 38 (64.4%) | |
| T-score (Steroid Users) | |||
| <50 years | −2.10 ± 0.56 | −2.18 ± 0.59 | t 0.564 |
| 50–60 years | −2.48 ± 0.20 | −2.82 ± 0.23 | t 0.099 |
| 60–85 years | −2.23 ± 0.53 | - | - |
| T-score (Non-Steroid Users/Degenerative Disk Disease) | |||
| <50 years | - | - | - |
| 50–60 years | −2.18 ± 0.41 | −2.10 ± 0.22 | t 0.879 |
| 60–80 years | −2.52 ± 0.49 | −2.62 ± 0.44 | t 0.534 |
| Screw Length (mm) | 45.8 ± 2.4 | 46.3 ± 2.1 | t 0.286 |
| Screw Diameter (mm) | 6.2 ± 0.3 | 6.1 ± 0.4 | t 0.654 |
| Follow-up Period (months) | 48 | 48 | - |
| Complications | |||
| 1 (1.8%) | 1 (1.5%) | a 1.000 |
| 5 (9.6%) | 16 (23.9%) | b 0.048 * |
| 11 (2.83%) | 79 (14.63%) | b 0.001 ** |
| 0 | 1 (1.5%) | a 1.000 |
| 1 (1.8%) | 2 (3.0%) | a 1.000 |
| 191.7 ± 41.4 min | 211.2 ± 37.3 min | |
| 357.33 ± 121.6 mL | 591.25 ± 246.3 mL | |
| Surgical Level | Number of Patients; n(%) | Two-Stage Procedure Patient Count by Surgical Level (n = 52) | Two-Stage Procedure Screw Loosening Patient Count No/Percent | Single-Stage Procedure Patient Count by Surgical Level (n = 67) | Single-Stage Procedure Screw Loosening Patient Count No/Percent |
|---|---|---|---|---|---|
| L1–S1 | 5 (4.2%) | 1 (1.92%) | 0 | 4 (5.97%) | 3 |
| L2–L4 | 5 (4.2%) | 1 (1.92%) | 0 | 4 (5.97%) | 0 |
| L2–L5 | 10 (8.4%) | 3 (5.77%) | 0 | 7 (10.45%) | 0 |
| L2–iliac | 8 (6.72%) | 4 (7.69%) | 1 | 4 (5.97%) | 2 |
| L3–S1 | 21 (17.65%) | 9 (17.31%) | 0 | 12 (17.91%) | 1 |
| L3–iliac | 5 (4.2%) | 3 (5.77%) | 1 | 2 (2.99%) | 1 |
| L4–S1 | 16 (13.45%) | 7 (13.46%) | 0 | 9 (13.43%) | 0 |
| T9–L5 | 7 (5.88%) | 5 (9.62%) | 0 | 2 (2.99%) | 1 |
| T10–iliac | 13 (10.92%) | 7 (13.46%) | 1 | 6 (8.96%) | 1 |
| T6–S1 | 1 (0.84%) | 1 (1.92%) | 0 | 0 (0%) | 0 |
| T10–S1 | 13 (10.92%) | 5 (9.62%) | 0 | 8 (11.94%) | 1 |
| T11–S1 | 2 (1.68%) | 1 (1.92%) | 0 | 1 (1.49%) | 1 |
| L2–S1 | 9 (7.56%) | 3 (5.77%) | 0 | 6 (8.96%) | 1 |
| T11–iliac | 4 (3.36%) | 2 (3.85%) | 2 | 2 (2.99%) | 4 |
| Toplam | 119 patients | 52 patients | 11 screws in 5 patients total loosening 9.6% | 67 patients | 79 screws in 16 patients total loosening 23.9% |
| Surgical Level | Pedicular Loosening | Corpus Loosening | Tip Loosening | Total Loosening | Total Loosening (%) | Pedicular vs. Corpus p-Value | Total Loosening p-Value | |
|---|---|---|---|---|---|---|---|---|
| T11 | 3 | 1 | 0 | 4 | 4.44% | 0.620 | 0.166 | |
| T12 | 7 | 4 | 3 | 14 | 15.56% | 0.746 | 0.031 | |
| L1 | 5 | 3 | 2 | 10 | 11.11% | 0.719 | 0.665 | |
| L2 | 1 | 4 | 2 | 7 | 7.78% | 0.200 | 0.040 | |
| L3 | 1 | 3 | 1 | 5 | 5.56% | 0.351 | <0.001 | |
| L4 | 2 | 5 | 1 | 8 | 8.89% | 0.262 | 0.002 | |
| L5 | 4 | 4 | 1 | 9 | 10.00% | >0.999 | 0.006 | |
| Iliac | 5 | 3 | 6 | 14 | 15.56% | 0.719 | 0.001 | |
| S1 | 9 | 6 | 4 | 19 | 21.11% | 0.777 | 0.964 | |
| Total | 37 | 33 | 20 | 90 | ||||
| Surgical Stage | Number of Loosened Screws | Number of Integrated Screws | Total Number of Screws | Screw Loosening Rate | p-Value |
|---|---|---|---|---|---|
| Single-Stage | 79 | 461 | 540 | 14.63% | p < 0.001 RR: 0.88, 95% CI: 0.84–0.91 |
| Two-Stage | 11 | 378 | 389 | 2.83% | |
| Total | 90 | 839 | 929 | 9.69% |
| Clinical Parameters | Preoperative | Preoperative (2nd Stage) | 6 Month | 12 Month | 24 Month | 48 Month | p-Value |
|---|---|---|---|---|---|---|---|
| VAS | |||||||
| Single-Stage | 8.78 ± 2.73 | 3.6 ± 1.3 | 3.5 ± 1.0 | 3.2 ± 0.9 | 2.9 ± 0.6 | <0.001 | |
| Two-Stage | 8.65 ± 2.51 | 7.54 ± 2.05 | 3.8 ± 1.2 | 3.0 ± 1.1 | 2.8 ± 1.0 | 2.4 ± 0.6 | <0.001 |
| ODI | |||||||
| Single-Stage | 69.71 ± 10.82 | 28.2 ± 4.5 | 25.8 ± 3.7 | 23.1 ± 2.9 | 19.1 ± 2.2 | <0.001 | |
| Two-Stage | 71.23 ± 12.06 | 65.86 ± 11.01 | 28.7 ± 4.9 | 23.1 ± 3.3 | 21.4 ± 3.1 | 18.3 ± 2.4 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hekimoglu, M.; Akgun, M.Y.; Ozer, H.; Basak, A.T.; Ucar, E.A.; Oktenoglu, T.; Ates, O.; Ozer, A.F. Two-Stage Lumbar Dynamic Stabilization Surgery: A Comprehensive Analysis of Screw Loosening Rates and Functional Outcomes Compared to Single-Stage Approach in Osteopenic and Osteoporotic Patients. Diagnostics 2024, 14, 1505. https://doi.org/10.3390/diagnostics14141505
Hekimoglu M, Akgun MY, Ozer H, Basak AT, Ucar EA, Oktenoglu T, Ates O, Ozer AF. Two-Stage Lumbar Dynamic Stabilization Surgery: A Comprehensive Analysis of Screw Loosening Rates and Functional Outcomes Compared to Single-Stage Approach in Osteopenic and Osteoporotic Patients. Diagnostics. 2024; 14(14):1505. https://doi.org/10.3390/diagnostics14141505
Chicago/Turabian StyleHekimoglu, Mehdi, Mehmet Yigit Akgun, Hidir Ozer, Ahmet Tulgar Basak, Ege Anil Ucar, Tunc Oktenoglu, Ozkan Ates, and Ali Fahir Ozer. 2024. "Two-Stage Lumbar Dynamic Stabilization Surgery: A Comprehensive Analysis of Screw Loosening Rates and Functional Outcomes Compared to Single-Stage Approach in Osteopenic and Osteoporotic Patients" Diagnostics 14, no. 14: 1505. https://doi.org/10.3390/diagnostics14141505
APA StyleHekimoglu, M., Akgun, M. Y., Ozer, H., Basak, A. T., Ucar, E. A., Oktenoglu, T., Ates, O., & Ozer, A. F. (2024). Two-Stage Lumbar Dynamic Stabilization Surgery: A Comprehensive Analysis of Screw Loosening Rates and Functional Outcomes Compared to Single-Stage Approach in Osteopenic and Osteoporotic Patients. Diagnostics, 14(14), 1505. https://doi.org/10.3390/diagnostics14141505







