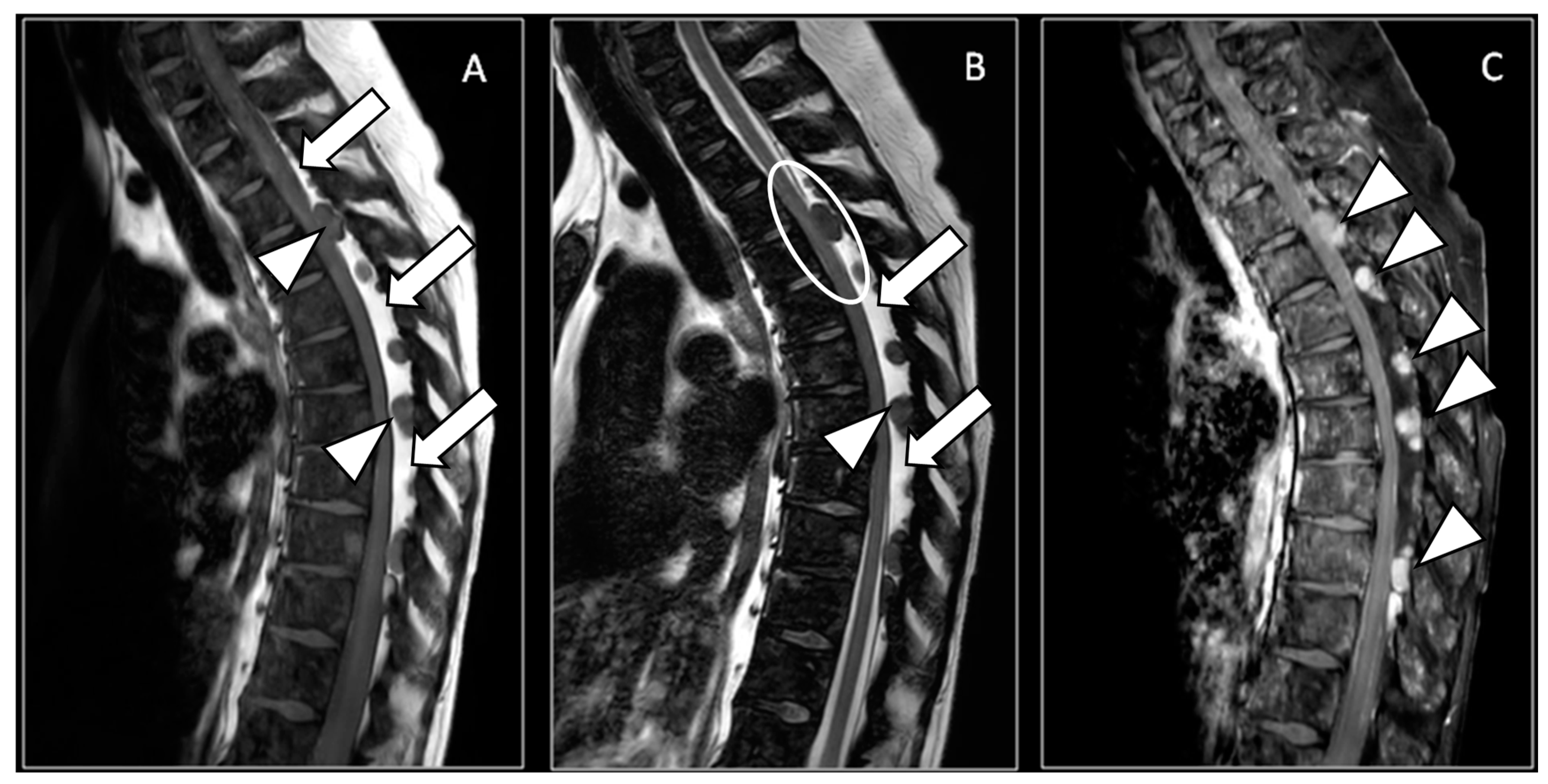
Breast Cancer Leptomeningeal Metastases on Spinal Epidural Lipomatosis
Abstract
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gennari, A.; André, F.; Barrios, C.H.; Cortés, J.; de Azambuja, E.; DeMichele, A.; Dent, R.; Fenlon, D.; Gligorov, J.; Hurvitz, S.A.; et al. ESMO Clinical Practice Guideline for the diagnosis, staging and treatment of patients with metastatic breast cancer. Ann. Oncol. 2021, 32, 1475–1495. [Google Scholar] [CrossRef] [PubMed]
- Franzoi, M.A.; Hortobagyi, G.N. Leptomeningeal carcinomatosis in patients with breast cancer. Crit. Rev. Oncol. Hematol. 2019, 135, 85–94. [Google Scholar] [CrossRef] [PubMed]
- Fogel, G.R.; Cunningham, P.Y., 3rd; Esses, S.I. Spinal epidural lipomatosis: Case reports, literature review and meta-analysis. Spine J. 2005, 5, 202–211. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rossi, A.; Sancini, G.; Amadori, E.; Cenni, P.; Palleschi, M.; Prochowski Iamurri, A. Breast Cancer Leptomeningeal Metastases on Spinal Epidural Lipomatosis. Diagnostics 2024, 14, 1496. https://doi.org/10.3390/diagnostics14141496
Rossi A, Sancini G, Amadori E, Cenni P, Palleschi M, Prochowski Iamurri A. Breast Cancer Leptomeningeal Metastases on Spinal Epidural Lipomatosis. Diagnostics. 2024; 14(14):1496. https://doi.org/10.3390/diagnostics14141496
Chicago/Turabian StyleRossi, Alice, Giada Sancini, Elena Amadori, Patrizia Cenni, Michela Palleschi, and Andrea Prochowski Iamurri. 2024. "Breast Cancer Leptomeningeal Metastases on Spinal Epidural Lipomatosis" Diagnostics 14, no. 14: 1496. https://doi.org/10.3390/diagnostics14141496
APA StyleRossi, A., Sancini, G., Amadori, E., Cenni, P., Palleschi, M., & Prochowski Iamurri, A. (2024). Breast Cancer Leptomeningeal Metastases on Spinal Epidural Lipomatosis. Diagnostics, 14(14), 1496. https://doi.org/10.3390/diagnostics14141496





