Updates on Treatment Modalities for Primary Rhegmatogenous Retinal Detachment Repair
Abstract
:1. Introduction
1.1. History of Surgical RRD Treatment
1.2. The Aim of the Paper
2. Relevant Sections
2.1. Pathophysiology and Mechanisms of RRD
2.2. Methods of Surgical Procedures for RRD
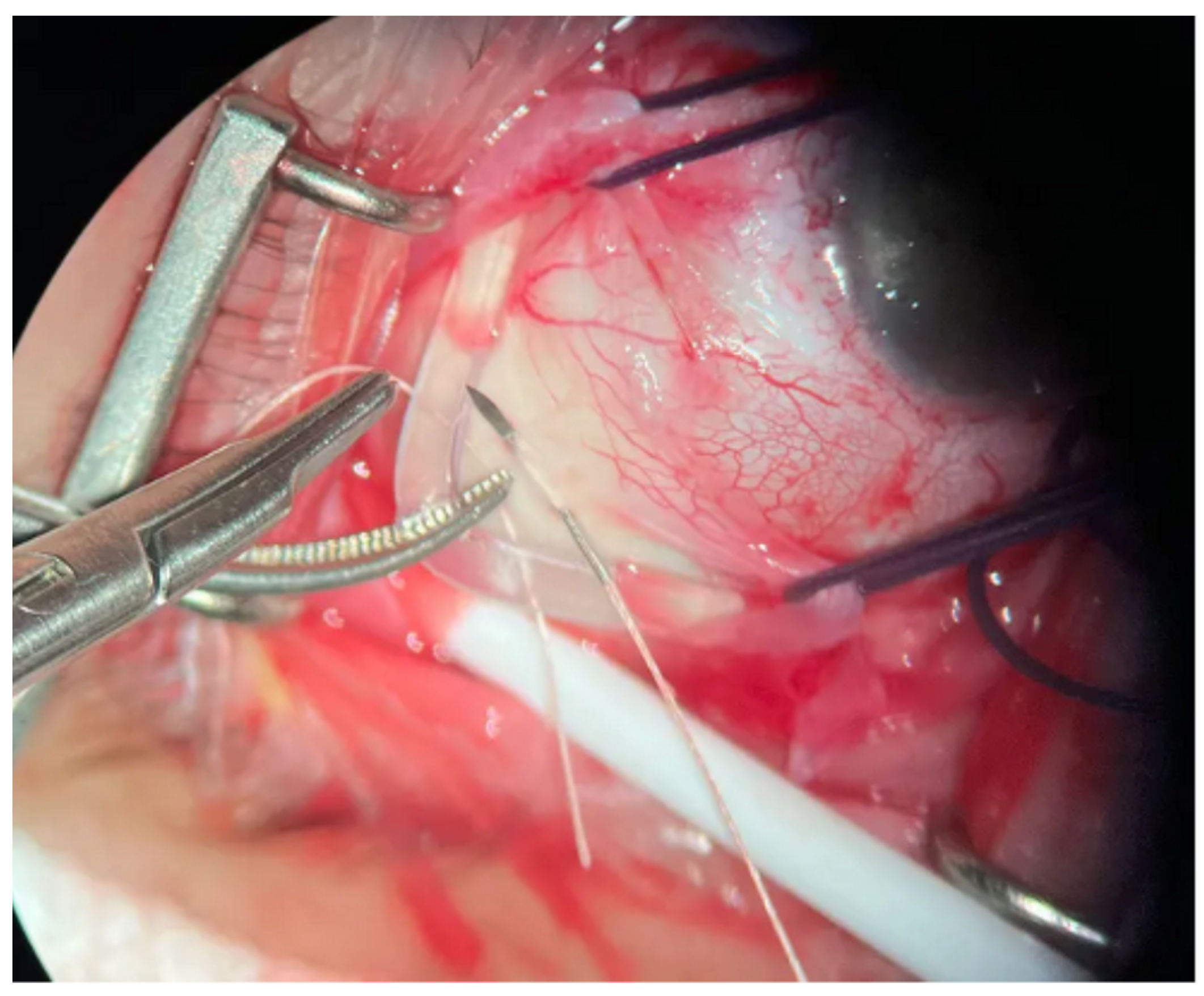
2.3. Scleral Buckling
2.4. Pneumatic Retinopexy
2.5. Pars Plana Vitrectomy
3. Discussion
4. Conclusions
5. Future Directions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| RD | retinal detachment |
| RRD | rhegmatogenous retinal detachment |
| PR | pneumatic retinopexy |
| SB | scleral buckling |
| PPV | pars plana vitrectomy |
| SRF | subretinal fluid |
| VR | vitreoretinal |
| PVR | proliferative vitreoretinopathy |
| MIVS | minimal invasive vitrectomy surgery |
| OCT | intraoperative optic coherence tomography |
| SOSR | single-operation success rate |
| SSAS | single surgery anatomic success |
| RCTs | randomized clinical trials |
| HUS | heads up visualizing systems |
References
- Ghazi, N.G.; Green, W.R. Pathology and pathogenesis of retinal detachment. Eye 2002, 16, 411–421. [Google Scholar] [CrossRef]
- The repair of rhegmatogenous retinal detachments. Ophthalmology 1990, 97, 1562–1572. [CrossRef] [PubMed]
- Kohli, P.; Tripathy, K. Scleral Buckling. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2024. [Google Scholar] [PubMed]
- Mitry, D.; Charteris, D.G.; Fleck, B.W.; Campbell, H.; Singh, J. The epidemiology of rhegmatogenous retinal detachment: Geographical variation and clinical associations. Br. J. Ophthalmol. 2010, 94, 678–684. [Google Scholar] [CrossRef]
- Tornquist, R.; Stenkula, S.; Tornquist, P. Retinal detachment. A study of a population-based patient material in Sweden 1971–1981. I. Epidemiology. Acta Ophthalmol. 1987, 65, 213–222. [Google Scholar] [CrossRef]
- Alfaar, A.S.; Wiedemann, P.; Rehak, M.; Wolf, A. The rising tide of rhegmatogenous retinal detachment in Germany: A nationwide analysis of the incidence, from 2005 to 2021. Graefes Arch Clin Exp Ophthalmol. 2024; ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, S.G.; Flynn, H.W. Pars plana vitrectomy for primary rhegmatogenous retinal detachment. Clin. Ophthalmol. 2008, 2, 57–63. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Havener, W.H. Retinal detachment: An insidious cause of blindness. Geriatrics 1975, 30, 85–87. [Google Scholar] [PubMed]
- Beran, D.I.; Murphy-Lavoie, H. Acute, painless vision loss. J. La State Med. Soc. 2009, 161, 214–216, 218–223. [Google Scholar] [PubMed]
- Feltgen, N.; Walter, P. Rhegmatogenous retinal detachment—an ophthalmologic emergency. Dtsch. Arztebl. Int. 2014, 111, 12–21. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Banker, A.S.; Freeman, W.R. Retinal detachment. Ophthalmol. Clin. N. Am. 2001, 14, 695–704. [Google Scholar] [CrossRef] [PubMed]
- Sánchez-Ramos, J.A.; Blanco-D’Mendieta, L.K.; Soto-Hernández Mde, L.; Márquez-González, H.; Sepúlveda-Vildósola, A.C. Desprendimiento recidivante de retina. Factores de riesgo [Risk factors for recurrent retinal detachment]. Rev. Med. Inst. Mex. Seguro Soc. 2014, 52, 34–37. (In Spanish) [Google Scholar] [PubMed]
- Saraf, S.S.; Lacy, M.; Hunt, M.S.; Lee, C.S.; Lee, A.Y.; Chee, Y.E.; IRIS Registry Research Analytic Centers. Demographics and Seasonality of Retinal Detachment, Retinal Breaks, and Posterior Vitreous Detachment from the Intelligent Research in Sight Registry. Ophthalmol. Sci. 2022, 2, 100145. [Google Scholar] [CrossRef] [PubMed]
- Schick, T.; Heimann, H.; Schaub, F. Netzhautablösung—Teil 1 [Retinal Detachment Part 1—Epidemiology, Risk Factors, Clinical Characteristics, Diagnostic Approach]. Klin. Monbl Augenheilkd. 2020, 237, 1479–1491. (In German) [Google Scholar] [CrossRef] [PubMed]
- Gonin, J. Le Decollement de la Retine. Pathogenie-Traitment; LibrairePayot: Lausanne, Switzerland, 1934. [Google Scholar]
- Wolfensberger, T.J. Jules Gonin. Pioneer of retinal detachment surgery. Indian. J. Ophthalmol. 2003, 51, 303–308. [Google Scholar] [PubMed]
- Custodis, E. Bedeutet die plombenaufnahung auf die sklera einen fortschritt in der operatven behandlung der netzhautablosung. Ber. Dtsch. Ophthalmol. Ges. 1953, 58, 102. [Google Scholar]
- Hirose, T.; Schepens, C.L. Retinal detachment. Arch. Ophthalmol. 1973, 89, 259–260. [Google Scholar] [CrossRef] [PubMed]
- Schepens, C.L. Retinal detachment and aphakia. AMA Arch. Ophthalmol. 1951, 45, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Schepens, C.L.; Okamura, I.D.; Brockhurst, R.J.; Regan, C.D.J. The scleral buckling procedures. V: Synthetic sutures and silicone implants. Arch. Ophthalmol. 1960, 64, 868–881. [Google Scholar] [CrossRef] [PubMed]
- Davis, M.J.; Mudvari, S.S.; Shott, S.; Rezaei, K.A. Clinical Characteristics Affecting the Outcome of Pneumatic Retinopexy. Arch. Ophthalmol. 2011, 129, 163–166. [Google Scholar] [CrossRef]
- Lincoff, H.; Kreissig, I. Changing patterns in the surgery for retinal detachment: 1929 to 2000. Klin Monbl Augenheilkd 2000, 216, 352–359. [Google Scholar] [CrossRef] [PubMed]
- Haritoglou, C.; Wolf, A. Operative Möglichkeiten bei Ablatio retinae [Surgical managment of retinal detachment]. Klin. Monbl Augenheilkd. 2015, 232, 669–675. (In German) [Google Scholar] [CrossRef] [PubMed]
- Velez-Montoya, R.; Jacobo-Oceguera, P.; Flores-Preciado, J.; Dalma-Weiszhausz, J.; Guerrero-Naranjo, J.; Salcedo-Villanueva, G.; Garcia-Aguirre, G.; Fromow-Guerra, J.; Morales-Canton, V. Primary Repair of Moderate Severity Rhegmatogenous Retinal Detachment: A Critical Decision-Making Algorithm. Med. Hypothesis Discov. Innov. Ophthalmol. 2016, 5, 18–31. [Google Scholar] [PubMed] [PubMed Central]
- Shah, S.; Chou, B.; Patel, M.; Watane, A.; Shah, L.; Yannuzzi, N.; Sridhar, J. Review and analysis of history and utilization of pneumatic retinopexy after pneumatic retinopexy versus vitrectomy for the management of primary rhegmatogenous retinal detachment outcomes randomized trial (PIVOT). Curr. Opin. Ophthalmol. 2024, 35, 217–222. [Google Scholar] [CrossRef] [PubMed]
- Kreissig, I. Surgical techniques for repair of primary retinal detachment: Part II. Comparison of present techniques in relation to morbidity. Folia Med. 2010, 52, 5–11. [Google Scholar] [PubMed]
- Kunikata, H.; Abe, T.; Nakazawa, T. Historical, Current and Future Approaches to Surgery for Rhegmatogenous Retinal Detachment. Tohoku J. Exp. Med. 2019, 248, 159–168. [Google Scholar] [CrossRef] [PubMed]
- Kreissig, I. A 50-year review of minimal extraocular surgery for retinal detachment: Five hurdles had to be overcome for its acceptance. Eye 2020, 34, 285–289. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lin, J.B.; Narayanan, R.; Philippakis, E.; Yonekawa, Y.; Apte, R.S. Retinal detachment. Nat. Rev. Dis. Prim. 2024, 10, 18. [Google Scholar] [CrossRef] [PubMed]
- Govers, B.M.; van Huet, R.A.C.; Roosing, S.; Keijser, S.; Los, L.I.; den Hollander, A.I.; Klevering, B.J. The genetics and disease mechanisms of rhegmatogenous retinal detachment. Prog. Retin. Eye Res. 2023, 97, 101158. [Google Scholar] [CrossRef] [PubMed]
- Mitry, D.; Fleck, B.W.; Wright, A.F.; Campbell, H.; Charteris, D.G. Pathogenesis of rhegmatogenous retinal detachment: Predisposing anatomy and cell biology. Retina 2010, 30, 1561–1572. [Google Scholar] [CrossRef] [PubMed]
- Tabibian, D.; Hoogewoud, F.; Mavrakanas, N.; Schutz, J.S. Misdirected aqueous flow in rhegmatogenous retinal detachment: A pathophysiology update. Surv. Ophthalmol. 2015, 60, 51–59. [Google Scholar] [CrossRef] [PubMed]
- Kuhn, F.; Aylward, B. Rhegmatogenous retinal detachment: A reappraisal of its pathophysiology and treatment. Ophthalmic Res. 2014, 51, 15–31. [Google Scholar] [CrossRef] [PubMed]
- Warren, A.; Wang, D.W.; Lim, J.I. Rhegmatogenous retinal detachment surgery: A review. Clin. Exp. Ophthalmol. 2023, 51, 271–279. [Google Scholar] [CrossRef] [PubMed]
- Haugstad, M.; Moosmayer, S.; Bragadόttir, R. Primary rhegmatogenous retinal detachment—Surgical methods and anatomical outcome. Acta Ophthalmol. 2017, 95, 247–251. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, S.G.; Garoon, R.; Smiddy, W.E.; Flynn, H.W., Jr. The legacy of Jules Gonin: One hundred years of identifying and treating retinal breaks. Graefes Arch. Clin. Exp. Ophthalmol. 2018, 256, 1051–1052. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Schepens, C.L.; Okamura, I.D.; Brockhurst, R.J. The scleral buckling procedures. I: Surgical techniques ad management. Arch. Ophthalmol. 1957, 58, 797–811. [Google Scholar] [CrossRef] [PubMed]
- Zaidi, A.A.; Alvarado, R.; Irvine, A. Pneumatic retinopexy: Success rate and complications. Br. J. Ophthalmol. 2006, 90, 427–428. [Google Scholar] [CrossRef] [PubMed]
- Tornambe, P.E. Pneumatic retinopexy: The evolution of case selection and surgical technique. A twelve-year study of 302 eyes. Trans. Am. Ophthalmol. Soc. 1997, 95, 551–578. [Google Scholar] [PubMed] [PubMed Central]
- Huang, C.Y.; Mikowski, M.; Wu, L. Pneumatic retinopexy: An update. Graefes Arch. Clin. Exp. Ophthalmol. 2022, 260, 711–722. [Google Scholar] [CrossRef] [PubMed]
- Chronopoulos, A.; Hattenbach, L.O.; Schutz, J.S. Pneumatic retinopexy: A critical reappraisal. Surv. Ophthalmol. 2021, 66, 585–593. [Google Scholar] [CrossRef] [PubMed]
- Abecia, E.; Pinilla, I.; Olivan, J.M.; Larrosa, J.M.; Polo, V.; Honrubia, F.M. Anatomic results and complications in a long-term follow-up of pneumatic retinopexy cases. Retina 2000, 20, 156–161. [Google Scholar] [CrossRef] [PubMed]
- Hillier, R.J.; Felfeli, T.; Berger, A.R.; Wong, D.T.; Altomare, F.; Dai, D.; Giavedoni, L.R.; Kertes, P.J.; Kohly, R.P.; Muni, R.H. The Pneumatic Retinopexy versus Vitrectomy for the Management of Primary Rhegmatogenous Retinal Detachment Outcomes Randomized Trial (PIVOT). Ophthalmology 2019, 126, 531–539. [Google Scholar] [CrossRef] [PubMed]
- Yannuzzi, N.A.; Li, C.; Fujino, D.; Kelly, S.P.; Lum, F.; Flynn, H.W., Jr.; Parke, D.W., 3rd. Clinical Outcomes of Rhegmatogenous Retinal Detachment Treated with Pneumatic Retinopexy. JAMA Ophthalmol. 2021, 139, 848–853. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mandelcorn, E.D.; Mandelcorn, M.S.; Manusow, J.S. Update on pneumatic retinopexy. Curr. Opin. Ophthalmol. 2015, 26, 194–199. [Google Scholar] [CrossRef] [PubMed]
- Ozturk, Y.; Ağın, A.; Yucel Gencoglu, A.; Talan, M.; Bulut, M.N. Comparison of Intraocular Tamponade in Patients with Peripheral Tear-Induced Retinal Detachment and Coexisting Macular Hole without High Myopia. Klin. Monbl Augenheilkd. 2023, 240, 897–902. (In English) [Google Scholar] [CrossRef] [PubMed]
- Ciarmatori, N.; Pellegrini, M.; Nasini, F.; Talli, P.M.; Sarti, L.; Mura, M. The State of Intraoperative OCT in Vitreoretinal Surgery: Recent Advances and Future Challenges. Tomography 2023, 9, 1649–1659. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mirshahi, A.; Khalilipour, E.; Faghihi, H.; Riazi-Esfahani, H.; Mirshahi, R.; Mehrjardi, H.Z.; Najibzadeh, E.; Amini, A.; Nabavi, A. Pars plana vitrectomy combined with phacoemulsification versus pars plana vitrectomy only for treatment of phakic rhegmatogenous retinal detachment: A systematic review and meta-analysis. Int. Ophthalmol. 2023, 43, 697–706. [Google Scholar] [CrossRef] [PubMed]
- Mason, R.H.; Minaker, S.A.; Marafon, S.B.; Figueiredo, N.; Hillier, R.J.; Muni, R.H. Retinal displacement following rhegmatogenous retinal detachment: A systematic review and meta-analysis. Surv. Ophthalmol. 2022, 67, 950–964. [Google Scholar] [CrossRef] [PubMed]
- Kolipaka, G.P.; Rao, A. Secondary glaucoma following vitreo-retinal surgeries. Indian. J. Ophthalmol. 2023, 71, 18–25. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Davidović, S.; Živković, M.; Risimić, D.; Rapajić, M.; Teodorović, S.; Barišić, S. Macular Parameters Change during Silicon Oil Tamponade for Retinal Detachment Surgery. Medicina 2023, 59, 334. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kanclerz, P.; Grzybowski, A. Complications Associated with the Use of Expandable Gases in Vitrectomy. J. Ophthalmol. 2018, 2018, 8606494. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kovačević, I.; Gaković, A.; Stefanović, I.; Djurić, S.; Čanadanović, V.; Davidović, S.; Biševac, J. Ekstrakcija intraokularnog stranog tela- prikaz dva slučaja. (Intraocular foreign body extraction- two cases report). Srp. Arh. Za Celok. Lek. 2013, 141, 81–84. [Google Scholar]
- Motta, L.; Frisina, R.; Ripa, M.; Gius, I.; Greggio, A.; Tozzi, L.; De Salvo, G.; Meduri, A. Postoperative complications after successful primary rhegmatogenous retinal detachment repair. BMC Ophthalmol. 2023, 23, 77. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Chizzolini, M.; Martini, F.; Melis, R.; Montericcio, A.; Raimondi, R.; Allegrini, D.; Romano, M.R. Pneumatic retinopexy versus scleral buckling for the management of primary rhegmatogenous retinal detachment. Eur. J. Ophthalmol. 2023, 33, 498–505. [Google Scholar] [CrossRef] [PubMed]
- Kawano, S.; Imai, T.; Sakamoto, T.; Japan-Retinal Detachment Registry Group. Scleral buckling versus pars plana vitrectomy in simple phakic macula-on retinal detachment: A propensity score-matched, registry-based study. Br. J. Ophthalmol. 2022, 106, 857–862. [Google Scholar] [CrossRef] [PubMed]
- Subedi, S.; Thapa, R.; Pradhan, E.; Bajiyama, S.; Sharma, S.; Duwal, S.; Poudel, M.; Poudyal, G. Outcomes of Microincision Pars Plana Vitrectomy In Rhegmatogenous Retinal Detachment. J. Nepal. Health Res. Counc. 2023, 20, 983–987. [Google Scholar] [CrossRef] [PubMed]
- Barca, F.; Caporossi, T.; Rizzo, S. Silicone oil: Different physical proprieties and clinical applications. Biomed. Res. Int. 2014, 2014, 502143. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Rizzo, S.; Barca, F. Vitreous substitute and tamponade substances for microincision vitreoretinal surgery. Dev. Ophthalmol. 2014, 54, 92–101. [Google Scholar] [CrossRef] [PubMed]
- Romano, M.R.; Ferrara, M.; Nepita, I.; D’Amato Tothova, J.; Giacometti Schieroni, A.; Reami, D.; Mendichi, R.; Liggieri, L.; Repetto, R. Biocompatibility of intraocular liquid tamponade agents: An update. Eye 2021, 35, 2699–2713. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kusaba, K.; Tsuboi, K.; Handa, T.; Shiraki, Y.; Kataoka, T.; Kmaei, M. Primary rhegmatogenous retinal detachment: Evaluation of a minimally restricted face-down positioning after pars plana vitrectomy and gas tamponade. Int. J. Ophthalmol. 2021, 14, 936–939. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Adelman, R.A.; Parnes, A.J.; Siperrley, J.O.; Ducournau, D.; European Vitreo-Retinal Society (EVRS) Retinal Detachment Study Group. Strategy for the management of uncomplicated retinal detachments: The European vitreo-retinal society retinal detachment study report 1. Ophthalmology 2013, 120, 1804–1808. [Google Scholar] [CrossRef]
- Adelman, R.A.; Parnes, A.J.; Sipperley, J.O.; Ducournau, D.; European Vitreo-Retinal Society (EVRS) Retinal Detachment Study Group. Strategy for the management of complex retinal detachments: The European vitreo-retinal society retinal detachment study report 2. Ophthalmology 2013, 120, 1809–1813. [Google Scholar] [CrossRef] [PubMed]
- Adelman, R.A.; Parnes, A.J.; Michalewska, Z.; Ducournau, D.; European Vitreo-Retinal Society (EVRS) Retinal Detachment Study Group. Clinical variables associated with failure of retinal detachment repair: The European vitreo-retinal society retinal detachment study report number 4. Ophthalmology 2014, 121, 1715–1719. [Google Scholar] [CrossRef] [PubMed]
- Heimann, H.; Bartz-Schmidt, K.U.; Bornfeld, N.; Weiss, C.; Hilgers, R.D.; Foerster, M.H.; Scleral Buckling versus Primary Vitrectomy in Rhegmatogenous Retinal Detachment Study Group. Scleral buckling versus primary vitrectomy in rhegmatogenous retinal detachment: A prospective randomized multicenter clinical study. Ophthalmology 2007, 114, 2142–2154. [Google Scholar] [CrossRef] [PubMed]
- Muni, R.H.; Bansal, A.; Lee, W.W.; Escaf, L.C. minimal gas vitrectomy with scleral buckle to minimize retinal displacement in rhegmatogenous retinal detachment with inferior breaks. Retin. Cases Brief. Rep. 2023, 17, 247–250. [Google Scholar] [CrossRef] [PubMed]
- Echegaray, J.J.; Vanner, E.A.; Zhang, L.; Fortun, J.A.; Albini, T.A.; Berrocal, A.M.; Smiddy, W.E.; Flynn, H.W., Jr.; Sridhar, J.; Gregori, N.Z.; et al. Outcomes of Pars Plana Vitrectomy Alone versus Combined Scleral Buckling plus Pars Plana Vitrectomy for Primary Retinal Detachment. Ophthalmol. Retina 2021, 5, 169–175. [Google Scholar] [CrossRef] [PubMed]
- Quiroz-Reyes, M.A.; Babar, Z.U.; Hussain, R.; Loh, Z.C.; Quiroz-Gonzalez, E.A.; Quiroz-Gonzalez, M.A.; Lima-Gomez, V. Management, risk factors and treatment outcomes of rhegmatogenous retinal detachment associated with giant retinal tears: Scoping review. Int. J. Retina Vitr. 2024, 10, 35. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Eshtiaghi, A.; Dhoot, A.S.; Mihalache, A.; Popovic, M.M.; Nichani, P.A.H.; Sayal, A.P.; Yu, H.J.; Wykoff, C.C.; Kertes, P.J.; Muni, R.H. Pars Plana Vitrectomy with and without Supplemental Scleral Buckle for the Repair of Rhegmatogenous Retinal Detachment: A Meta-analysis. Ophthalmol. Retina 2022, 6, 871–885. [Google Scholar] [CrossRef] [PubMed]
- Popovic, M.M.; Muni, R.H.; Nichani, P.; Kertes, P.J. Pars plana vitrectomy, scleral buckle, and pneumatic retinopexy for the management of rhegmatogenous retinal detachment: A meta-analysis. Surv. Ophthalmol. 2022, 67, 184–196. [Google Scholar] [CrossRef] [PubMed]
- Heussen, N.; Hilgers, R.D.; Heimann, H.; Collins, L.; Grisanti, S.; SPR study group. Scleral buckling versus primary vitrectomy in rhegmatogenous retinal detachment study (SPR study): Multiple-event analysis of risk factors for reoperations. SPR Study report no. 4. Acta Ophthalmol. 2011, 89, 622–628. [Google Scholar] [CrossRef] [PubMed]
- Starr, M.R.; Ryan, E.H.; Yonekawa, Y. Primary Retinal Detachment Outcomes Study: Summary of reports number 1 to number 18. Curr. Opin. Ophthalmol. 2023, 34, 211–217. [Google Scholar] [CrossRef] [PubMed]
- Jeon, G.S.; Han, J.R. Effectiveness of Scleral Buckling with a Wide-Field Surgical Microscope and Chandelier Illumination in Retinal Detachment Repair. Ophthalmologica 2019, 242, 31–37. [Google Scholar] [CrossRef] [PubMed]
- Tabandeh, H.; Khachaturov, A.; Rezaei, K.A.; Boyer, D.S. Supplemental scleral buckle in the era of small incision vitrectomy and wide-angle viewing systems. Retina 2020, 40, 1894–1899. [Google Scholar] [CrossRef] [PubMed]
- Bopp, S. Traumaassoziierte rhegmatogene Netzhautablösung im Kindesalter [Trauma-associated juvenile rhegmatogenous retinal detachment]. Klin. Monbl Augenheilkd. 2013, 230, 879–887. (In German) [Google Scholar] [CrossRef] [PubMed]
- Rossin, E.J.; Tsui, I.; Wong, S.C.; Hou, K.K.; Prakhunhungsit, S.; Blair, M.P.; Shapiro, M.J.; Leishman, L.; Nagiel, A.; Lifton, J.A.; et al. Traumatic Retinal Detachment in Patients with Self-Injurious Behavior: An International Multicenter Study. Ophthalmol. Retina 2021, 5, 805–814. [Google Scholar] [CrossRef] [PubMed]
- Tan, A.; Bertrand-Boiché, M.; Angioi-Duprez, K.; Berrod, J.P.; Conart, J.B. Outcomes of combined phacoemulsification and pars plana vitrectomy for rhegmatogenous retinal detachment: A Comparative Study. Retina 2021, 41, 68–74. [Google Scholar] [CrossRef] [PubMed]
- Gerstenberger, E.; Stoffelns, B.; Nickels, S.; Münzel, T.; Wild, P.S.; Beutel, M.E.; Schmidtmann, I.; Lackner, K.J.; Pfeiffer, N.; Schuster, A.K. Incidence of Retinal Detachment in Germany: Results from the Gutenberg Health Study. Ophthalmologica 2021, 244, 133–140. [Google Scholar] [CrossRef] [PubMed]
- German Society of Ophthalmology (Deutsche Ophthalmologische Gesellschaft, DOG); German Retina Society e. V. (Retinologische Gesellschaft e. V., RG); Professional Association of German Ophthalmologists in Germany (Berufsverband der Augenärzte Deutschlands e. V., BVA). Statement of the German Ophthalmological Society (DOG), the Retinological Society (RG) and the Professional Association of Ophthalmologists in Germany (BVA) on the timing of treatment of rhegmatogenous retinal detachment: Dated October 2020. Ophthalmologe 2021, 118 (Suppl. S2), 132–134. (In English) [Google Scholar] [CrossRef] [PubMed]
- Bucher, F.; Daniel, M.C.; Böhringer, D.; Lange, C.; Reinhard, T.; Agostini, H.; Lang, S.J. Eindellende Operationen zur Behandlung der rhegmatogenen Amotio in Deutschland: Ein Geist der Vergangenheit oder gelebte Praxis? [Scleral Buckling Surgery in Germany for Rhegmatogenous Retinal Detachment: A Spirit of the Past or Current Practice?]. Klin. Monbl Augenheilkd. 2020, 237, 780–786. (In German) [Google Scholar] [CrossRef] [PubMed]
- Feltgen, N.; Callizo, J.; Hattenbach, L.O.; Hoerauf, H. The urgency of surgical treatment for rhegmatogenous retinal detachment. Ophthalmologe 2021, 118 (Suppl. S2), 160–165. (In English) [Google Scholar] [CrossRef] [PubMed]
- Jackson, T.L.; Donachie, P.H.; Sallam, A.; Sparrow, J.M.; Johnston, R.L. United Kingdom National Ophthalmology Database study of vitreoretinal surgery: Report 3, retinal detachment. Ophthalmology 2014, 121, 643–648. [Google Scholar] [CrossRef] [PubMed]
- Madi, H.A.; Keller, J. Increasing frequency of hospital admissions for retinal detachment and vitreo-retinal surgery in England 2000–2018. Eye 2022, 36, 1610–1614. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Rizzo, S.; Belting, C.; Genovesi-Ebert, F. Retinal detachment after small-incision, sutureless pars plana vitrectomy: Possible causative agents. Graefes Arch. Clin. Exp. Ophthalmol. 2010, 248, 1401–1406. [Google Scholar] [CrossRef] [PubMed]
- Ludwig, C.A.; Vail, D.; Al-Moujahed, A.; Callaway, N.F.; Saroj, N.; Moshfeghi, A.; Moshfeghi, D.M. Epidemiology of rhegmatogenous retinal detachment in commercially insured myopes in the United States. Sci. Rep. 2023, 13, 9430. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Vail, D.; Pan, C.; Pershing, S.; Mruthyunjaya, P. Association of Rhegmatogenous Retinal Detachment and Outcomes with the Day of the Week That Patients Undergo a Repair or Receive a Diagnosis. JAMA Ophthalmol. 2020, 138, 156–163. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Callaway, N.F.; Vail, D.; Al-Moujahed, A.; Ludwig, C.; Ji, M.H.; Mahajan, V.B.; Pershing, S.; Moshfeghi, D.M. Sex Differences in the Repair of Retinal Detachments in the United States. Am. J. Ophthalmol. 2020, 219, 284–294. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Reeves, M.G.; Pershing, S.; Afshar, A.R. Choice of Primary Rhegmatogenous Retinal Detachment Repair Method in US Commercially Insured and Medicare Advantage Patients, 2003–2016. Am. J. Ophthalmol. 2018, 196, 82–90. [Google Scholar] [CrossRef] [PubMed]
- Savastano, A.; Weinberg, T.; Faraldi, F.; Caporossi, T.; Rizzo, S. Scleral Buckling Using Chandelier and Releasable Suture: A Useful Surgical Variant. Retina 2023, 43, 363–366. [Google Scholar] [CrossRef] [PubMed]
- Soni, C.; Hainsworth, D.P.; Almony, A. Surgical management of rhegmatogenous retinal detachment: A meta-analysis of randomized controlled trials. Ophthalmology 2013, 120, 1440–1447. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z. A Modified Suturing Technique to Produce Temporary Scleral Buckling Effect for Noncomplex Rhegmatogenous Retinal Detachment. Retina 2024, 44, 928–933. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Heussen, N.; Feltgen, N.; Walter, P.; Hoerauf, H.; Hilgers, R.D.; Heimann, H.; SPR Study Group. Scleral buckling versus primary vitrectomy in rhegmatogenous retinal detachment study (SPR Study): Predictive factors for functional outcome. Study report no. 6. Graefes Arch. Clin. Exp. Ophthalmol. 2011, 249, 1129–1136. [Google Scholar] [CrossRef] [PubMed]
- Radice, P.; Carini, E.; Seidenari, P.; Govetto, A. Standardized scleral buckling approach in the management of noncomplex primary rhegmatogenous retinal detachment. Eur. J. Ophthalmol. 2021, 31, 1993–2002. [Google Scholar] [CrossRef] [PubMed]
- Fallico, M.; Alosi, P.; Reibaldi, M.; Longo, A.; Bonfiglio, V.; Avitabile, T.; Russo, A. Scleral Buckling: A Review of Clinical Aspects and Current Concepts. J. Clin. Med. 2022, 11, 314. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Fischer, C.V.; Kulanga, M.; Hoerauf, H. Trends in der Ablatiochirurgie: Was hat sich im Vergleich zu 2001 geändert? [Trends in retinal detachment surgery: What has changed compared to 2001?]. Ophthalmologe 2018, 115, 663–668. (In German) [Google Scholar] [CrossRef] [PubMed]
- Rush, R.; Simunovic, M.P.; Sheth, S.; Chang, A.; Hunyor, A.P. 23-Gauge Pars Plana Vitrectomy Versus Scleral Buckling Versus Combined Pars Plana Vitrectomy–Scleral Buckling for Medium-Complexity Retinal Detachment Repair. Asia-Pac. J. Ophthalmol. 2014, 3, 215–219. [Google Scholar] [CrossRef] [PubMed]
- Čanadanović, V.; Babić, N.; Davidović, S.; Miljković, A.; Brunet, S.; Barišić, S. Ishod operacije katarakte kod pacijenata sa šećernom bolesti. (Outcome of cataract surgery in diabetic patient). Med. Preged 2018, LXXI, 217–221. [Google Scholar]
- Ilhan, C.; Citirik, M.; Dulger, S.C.; Ozdemir, M. Long-term Complications of Conventional and Chandelier-Assisted Scleral Buckle for Primary Repair of Rhegmatogenous Retinal Detachment. J. Curr. Ophthalmol. 2022, 34, 323–327. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Dhoot, A.S.; Popovic, M.M.; Nichani, P.A.H.; Eshtiaghi, A.; Mihalache, A.; Sayal, A.P.; Yu, H.; Wykoff, C.C.; Kertes, P.J.; Muni, R.H. Pars plana vitrectomy versus scleral buckle: A comprehensive meta-analysis of 15,947 eyes. Surv. Ophthalmol. 2022, 67, 932–949. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Liu, B.; Liu, J.; Wen, D.; Wang, M.; Shao, Y.; Li, X. Comparison of 27-gauge beveled-tip and 25-gauge flat-tip microincision vitrectomy surgery in the treatment of proliferative diabetic retinopathy: A randomized controlled trial. BMC Ophthalmol. 2023, 23, 504. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Pollack, J.S.; Sabherwal, N. Small gauge vitrectomy: Operative techniques. Curr. Opin. Ophthalmol. 2019, 30, 159–164. [Google Scholar] [CrossRef] [PubMed]
- Doi, Y.; Muraoka, Y.; Tsujikawa, A. Evaluation of the Efficiency and Safety of a 27-Gauge 20,000 Cuts per Minute Vitreous Cutter. Clin. Ophthalmol. 2023, 17, 2037–2043. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Fung, N.S.K.; Mak, A.K.H.; Brelen, M.; Tsang, C.W.; Mohamed, S.; Lam, W.C. Performance, safety and efficiency comparison between 10,000 and 5000 cuts per minute vitrectomy using a 25G cutter: A prospective randomized controlled study. Int. J. Retina Vitr. 2023, 9, 15. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Blinder, K.J.; Awh, C.C.; Tewari, A.; Garg, S.J.; Srivastava, S.K.; Kolesnitchenko, V. Introduction to hypersonic vitrectomy. Curr. Opin. Ophthalmol. 2019, 30, 133–137. [Google Scholar] [CrossRef] [PubMed]
- Nepita, I.; Stocchino, A.; Dodero, A.; Castellano, M.; Ferrara, M.; Romano, M.R.; Repetto, R. Dynamic Pressure Measurements During Vitrectomy in a Model of the Eye. Transl. Vis. Sci. Technol. 2022, 11, 21. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Shinkai, Y.; Yoneda, K.; Sotozono, C. Ex vivo Comparison of Intraocular Pressure Fluctuation during Pars Plana Vitrectomy Performed Using 25- and 27-Gauge Systems. Ophthalmic Res. 2022, 65, 210–215. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Del Turco, C.; D’Amico Ricci, G.; Dal Vecchio, M.; Bogetto, C.; Panico, E.; Giobbio, D.C.; Romano, M.R.; Panico, C.; La Spina, C. Heads-up 3D eye surgery: Safety outcomes and technological review after 2 years of day-to-day use. Eur. J. Ophthalmol. 2021, 3, 11206721211012856. [Google Scholar] [CrossRef] [PubMed]
- Asani, B.; Siedlecki, J.; Schworm, B.; Mayer, W.J.; Kreutzer, T.C.; Luft, N.; Priglinger, S.G. 3D Heads-Up Display vs. Standard Operating Microscope Vitrectomy for Rhegmatogenous Retinal Detachment. Front. Med. 2020, 7, 615515. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Saito, Y.; Horiguchi, H.; Mizobuchi, K.; Katagiri, S.; Gunji, H.; Nakano, T. Effectiveness of the Heads-Up Surgery System for Retinal Surgery in a Patient with Severe Photophobia. Int. Med. Case Rep. J. 2021, 14, 583–589. [Google Scholar] [CrossRef]

| Surgical Method for Primary RRD Surgery | Buckling Surgery | PPV |
|---|---|---|
| Preferred Lens Status | Phakic | Pseudophakic/Aphakic |
| Location of retinal break | No difference In inferior break, no gas tamponade is possible | Preferrably upper quadrants of retina Inferior breaks are difficult to manage with standard gas or standard silicon oil tamponade (additional buckle is preferrable or use of heavy density silicon oil) |
| Release of VR traction | Indirect | Direct |
| Drainage of SRF | From outside | From inside |
| Postoperative positioning | Required with intraocular gas tamponade | Usually required |
| Postoperative inflammation | Significant | Mild |
| Postoperative pain | Usually pronounced | Mild of moderate |
| Surgical trauma | Higher | Lower |
| Advantages |
|
|
| Complications |
|
|
| Previous corneal surgery | Possibility of impaired visualisation | Possibility of impaired visualization Flap slippage in flap-based corneal surgery |
| Postoperative recovery time | Multifactorial, Longer | Mutlifactorial, Shorter |
| Dependance on devices | Low | High |
| Costs | Low | High |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Davidović, S.; Babović, S.; Miljković, A.; Pavin, S.; Bolesnikov-Tošić, A.; Barišić, S. Updates on Treatment Modalities for Primary Rhegmatogenous Retinal Detachment Repair. Diagnostics 2024, 14, 1493. https://doi.org/10.3390/diagnostics14141493
Davidović S, Babović S, Miljković A, Pavin S, Bolesnikov-Tošić A, Barišić S. Updates on Treatment Modalities for Primary Rhegmatogenous Retinal Detachment Repair. Diagnostics. 2024; 14(14):1493. https://doi.org/10.3390/diagnostics14141493
Chicago/Turabian StyleDavidović, Sofija, Siniša Babović, Aleksandar Miljković, Svetlana Pavin, Ana Bolesnikov-Tošić, and Sava Barišić. 2024. "Updates on Treatment Modalities for Primary Rhegmatogenous Retinal Detachment Repair" Diagnostics 14, no. 14: 1493. https://doi.org/10.3390/diagnostics14141493
APA StyleDavidović, S., Babović, S., Miljković, A., Pavin, S., Bolesnikov-Tošić, A., & Barišić, S. (2024). Updates on Treatment Modalities for Primary Rhegmatogenous Retinal Detachment Repair. Diagnostics, 14(14), 1493. https://doi.org/10.3390/diagnostics14141493






