Frailty as an Independent Predictor of Adverse Outcomes in Patients Undergoing Direct Myocardial Revascularization
Abstract
1. Introduction
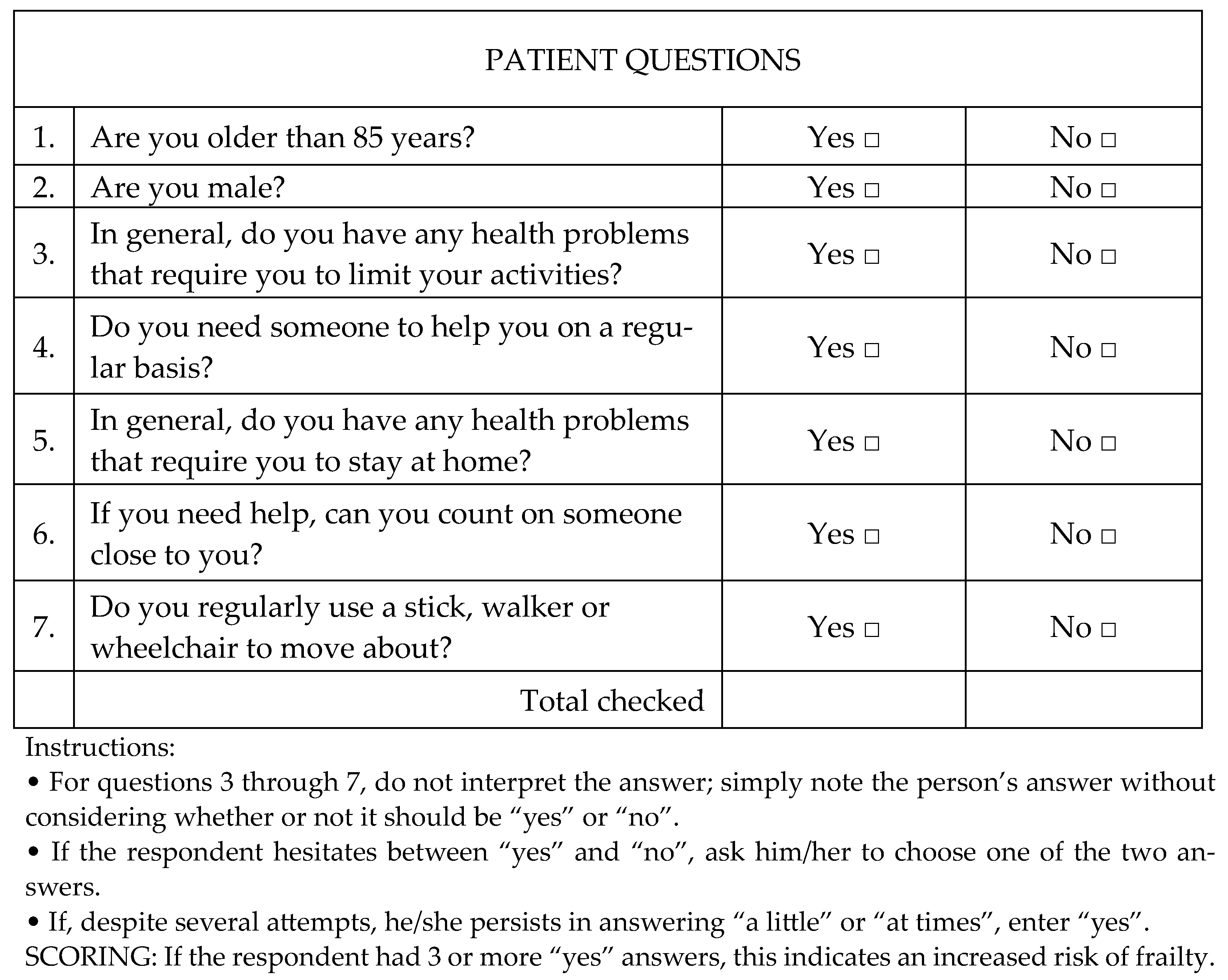
2. Materials and Methods
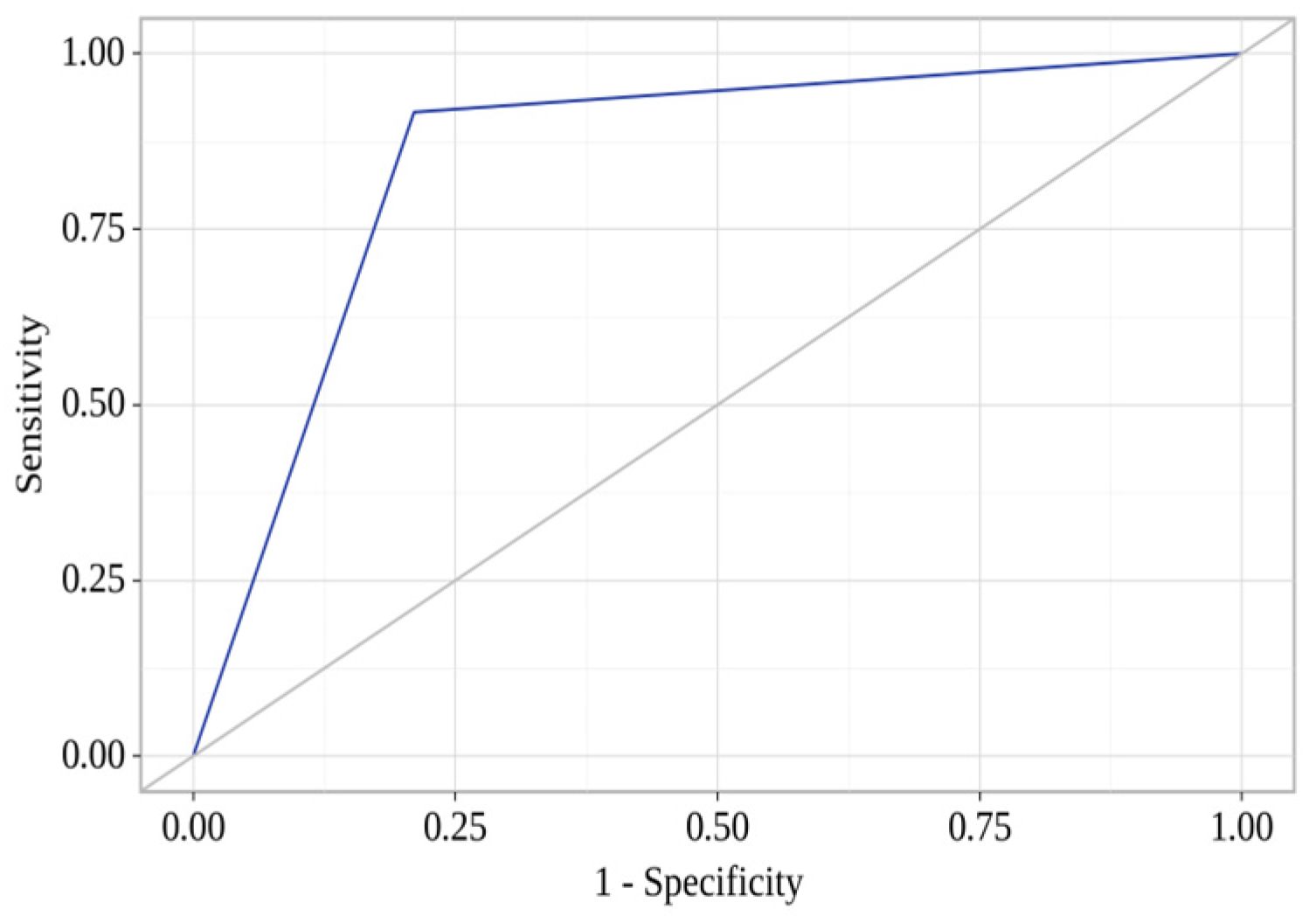
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AFib | atrial fibrillation |
| AFL | atrial flutter |
| AH | arterial hypertension |
| BMI | body mass index |
| BP | blood pressure |
| CABG | coronary artery bypass grafting |
| CAD | coronary artery disease |
| CEE | carotid endarterectomy |
| CI | confidence interval |
| CPB | cardiopulmonary bypass |
| CRF | chronic renal failure |
| DM | diabetes mellitus |
| FC | functional class |
| GFR | glomerular filtration rate |
| HDL | high-density lipoprotein |
| HF | heart failure |
| ICU | intensive care unit |
| MODS | multiple organ dysfunction syndrome |
| MV | mechanical ventilation |
| OR | odds ratio |
| PAD | peripheral arteries diseases |
| PCI | percutaneous coronary intervention |
| PICS | postinfarction cardiac sclerosis |
| RR | relative risk |
| TIA | transient ischemic attack |
References
- Neumann, F.; Sousa–Uva, M.; Ahlsson, A.; Alfonso, F.; Banning, A.; Benedetto, U.; Byrne, R.; Collet, J.; Falk, V.; Head, S.; et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur. Heart J. 2019, 40, 87–165. [Google Scholar] [CrossRef] [PubMed]
- Bokeriia, L.A.; IIu, S.; Alshibaia, M.M. Modern approaches to surgical treatment of patients with complicated and combined forms of coronary heart diseases. Vestn. Ross. Akad. Meditsinskikh Nauk 2009, 12, 39–42. (In Russian) [Google Scholar] [PubMed]
- Boyd, O.; Jackson, N. How is risk defined in high–risk surgical patient management? Crit. Care 2005, 9, 390–396. [Google Scholar] [CrossRef] [PubMed]
- Bäck, C.; Hornum, M.; Olsen, P.S.; Møller, C.H. 30-day mortality in frail patients undergoing cardiac surgery: The results of the frailty in cardiac surgery (FICS) copenhagen study. Scand. Cardiovasc. J. 2019, 53, 348–354. [Google Scholar] [CrossRef] [PubMed]
- Siregar, S.; Groenwold, R.H.; de Heer, F.; Bots, M.L.; van der Graaf, Y.; van Herwerden, L.A. Performance of the original EuroSCORE. Eur. J. Cardiothorac. Surg. 2012, 41, 746–754. [Google Scholar] [CrossRef] [PubMed]
- Nezic, D.; Spasic, T.; Micovic, S.; Kosevic, D.; Petrovic, I.; Lausevic-Vuk, L.; Unic-Stojanovic, D.; Borzanovic, M. Consecutive Observational Study to Validate EuroSCORE II Performances on a Single-Center, Contemporary Cardiac Surgical Cohort. J. Cardiothorac. Vasc. Anesth. 2016, 30, 345–351. [Google Scholar] [CrossRef] [PubMed]
- Shih, T.; Paone, G.; Theurer, P.F.; McDonald, D.; Shahian, D.M.; Prager, R.L. The Society of Thoracic Surgeons Adult Cardiac Surgery Database Version 2.73: More Is Better. Ann. Thorac. Surg. 2015, 100, 516–521. [Google Scholar] [CrossRef] [PubMed]
- Higgins, T.; Estafanous, F.; Loop, F.; Beck, G.; Blum, J.; Paranandi, L. Stratification of morbidity and mortality outcome by preoperative risk factors in coronary artery bypass patients. A clinical severity score. JAMA 1992, 267, 2344–2348. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, F.M.R.L.; Barbosa, K.T.F.; Rodrigues, M.M.P.; Fernandes, M.D.G.M. Frailty syndrome in the elderly: Conceptual analysis according to Walker and Avant. Rev. Bras. Enferm. 2020, 73 (Suppl. S3), e20190601. [Google Scholar] [CrossRef]
- Koh, L.Y.; Hwang, N.C. Frailty in Cardiac Surgery. J. Cardiothorac. Vasc. Anesth. 2019, 33, 521–531. [Google Scholar] [CrossRef] [PubMed]
- Kloos, J.; Bassiri, A.; Ho, V.P.; Sinopoli, J.; Vargas, L.T.; Linden, P.A.; Towe, C.W. Frailty is associated with 90-day mortality in urgent thoracic surgery conditions. JTCVS Open 2023, 17, 336–343. [Google Scholar] [CrossRef] [PubMed]
- McIsaac, D.; Taljaard, M.; Bryson, G.; Beaulé, P.; Gagné, S.; Hamilton, G.; Hladkowicz, E.; Huang, A.; Joanisse, J.; Lavallée, L.; et al. Frailty as a Predictor of Death or New Disability after Surgery: A Prospective Cohort Study. Ann. Surg. 2020, 271, 283–289. [Google Scholar] [CrossRef] [PubMed]
- Arora, R.C.; Brown, C.H., 4th; Sanjanwala, R.M.; McKelvie, R. “NEW” Prehabilitation: A 3-Way Approach to Improve Postoperative Survival and Health-Related Quality of Life in Cardiac Surgery Patients. Can. J. Cardiol. 2018, 34, 839–849. [Google Scholar] [CrossRef] [PubMed]
- Higginbotham, O.; O’Neill, A.; Barry, L.; Leahy, A.; Robinson, K.; O’Connor, M.; Galvin, R. The diagnostic and predictive accuracy of the PRISMA-7 screening tool for frailty in older adults: A systematic review protocol. HRB Open Res. 2020, 3, 26. [Google Scholar] [CrossRef] [PubMed]
- Zazzara, M.B.; Vetrano, D.L.; Carfì, A.; Onder, G. Frailty and chronic disease. Panminerva Med. 2019, 61, 486–492. [Google Scholar] [CrossRef] [PubMed]
- Vetrano, D.L.; Palmer, K.; Marengoni, A.; Marzetti, E.; Lattanzio, F.; Roller-Wirnsberger, R.; Lopez Samaniego, L.; Rodríguez-Mañas, L.; Bernabei, R.; Onder, G.; et al. Frailty and Multimorbidity: A Systematic Review and Meta-analysis. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2019, 74, 659–666. [Google Scholar] [CrossRef] [PubMed]
- Tazzeo, C.; Rizzuto, D.; Calderón-Larrañaga, A.; Roso-Llorach, A.; Marengoni, A.; Welmer, A.K.; Onder, G.; Trevisan, C.; Vetrano, D.L. Multimorbidity patterns and risk of frailty in older community-dwelling adults: A population-based cohort study. Age Ageing 2021, 50, 2183–2191. [Google Scholar] [CrossRef] [PubMed]
- Alvarez–Nebreda, M.; Bentov, N.; Urman, R.; Setia, S.; Huang, J.; Pfeifer, K.; Bennett, K.; Ong, T.; Richman, D.; Gollapudi, D.; et al. Recommendations for Preoperative Management of Frailty from the Society for Perioperative Assessment and Quality Improvement (SPAQI). J. Clin. Anesth. 2018, 47, 33–42. [Google Scholar] [CrossRef] [PubMed]
- Eamer, G.; Taheri, A.; Chen, S.; Daviduck, Q.; Chambers, T.; Shi, X.; Khadaroo, R. Comprehensive geriatric assessment for older people admitted to a surgical service. Cochrane Database Syst. Rev. 2018, 1, CD012485. [Google Scholar] [CrossRef] [PubMed]
- Aguayo, G.; Donneau, A.; Vaillant, M.; Schritz, A.; Franco, O.; Stranges, S.; Malisoux, L.; Guillaume, M.; Witte, D. Agreement Between 35 Published Frailty Scores in the General Population. Am. J. Epidemiol. 2017, 186, 420–434. [Google Scholar] [CrossRef] [PubMed]
- Cooper, Z.; Rogers, S.O., Jr.; Ngo, L.; Guess, J.; Schmitt, E.; Jones, R.; Ayres, D.; Walston, J.; Gill, T.; Gleason, L.; et al. Comparison of Frailty Measures as Predictors of Outcomes after Orthopedic Surgery. J. Am. Geriatr. Soc. 2016, 64, 2464–2471. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, S.; Wiben, A.; Kruse, M.; Jacobsen, K.K.; Lembeck, M.A.; Holm, E.A. Predictive validity of PRISMA-7 as a screening instrument for frailty in a hospital setting. BMJ Open 2020, 10, e038768. [Google Scholar] [CrossRef] [PubMed]
- Wang, G.Q.; Gao, Y.L.; Deng, P. Validation of a seven-question tool (PRISMA-7) in predicting prognosis of older adults in the emergency department: A prospective study. Am. J. Emerg. Med. 2023, 73, 131–136. [Google Scholar] [CrossRef] [PubMed]
- Hall, D.; Arya, S.; Schmid, K. Association of frailty screening initiative with postoperative survival at 30, 180, and 365 days. JAMA Surg. 2017, 152, 233–240. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.; Buth, K.; Martin, B.; Yip, A.; Hirsch, G. Frail patients are at increased risk for mortality and prolonged institutional care after cardiac surgery. Circulation 2010, 121, 973–978. [Google Scholar] [CrossRef] [PubMed]
- Clark, K.; Leathers, T.; Rotich, D.; He, J.; Wirtz, K.; Daon, E.; Flynn, B. Gait Speed Is Not Associated with Vasogenic Shock or Cardiogenic Shock following Cardiac Surgery, but Is Associated with Increased Hospital Length of Stay. Crit. Care Res. Pract. 2018, 2018, 1538587. [Google Scholar] [CrossRef] [PubMed]
- Imaoka, Y.; Kawano, T.; Hashiguchi, A.; Fujimoto, K.; Yamamoto, K.; Nishi, T.; Otsuka, T.; Yano, S.; Mukasa, A. Modified frailty index predicts postoperative outcomes of spontaneous intracerebral hemorrhage. Clin. Neurol. Neurosurg. 2018, 175, 137–143. [Google Scholar] [CrossRef] [PubMed]
- Ali, T.; Lehman, E.; Aziz, F. Modified Frailty Index Can Be Used to Predict Adverse Outcomes and Mortality after Lower Extremity Bypass Surgery. Ann. Vasc. Surg. 2018, 46, 168–177. [Google Scholar] [CrossRef] [PubMed]
- Nashef, S.A.; Roques, F.; Michel, P.; Gauducheau, E.; Lemeshow, S.; Salamon, R. European system for cardiac operative risk evaluation (EuroSCORE). Eur. J. Cardio-Thorac. Surg. Off. J. Eur. Assoc. Cardio-Thorac. Surg. 1999, 16, 9–13. [Google Scholar] [CrossRef]
- Sündermann, S.; Dademasch, A.; Seifert, B.; Rodriguez Cetina Biefer, H.; Emmert, M.; Walther, T.; Jacobs, S.; Mohr, F.; Falk, V.; Starck, C. Frailty is a predictor of short– and mid–term mortality after elective cardiac surgery independently of age. Interact. Cardiovasc. Thorac. Surg. 2014, 18, 580–585. [Google Scholar] [CrossRef] [PubMed]
- Reichart, D.; Rosato, S.; Nammas, W.; Onorati, F.; Dalén, M.; Castro, L.; Gherli, R.; Gatti, G.; Franzese, I.; Faggian, G.; et al. Clinical frailty scale and outcome after coronary artery bypass grafting. Eur. J. Cardio–Thorac. Surg. Off. J. Eur. Assoc. Cardio–Thorac. Surg. 2018, 54, 1102–1109. [Google Scholar] [CrossRef] [PubMed]
- Usman, M.S.; Siddiqi, T.J.; Anker, S.D.; Bakris, G.L.; Bhatt, D.L.; Filippatos, G.; Fonarow, G.C.; Greene, S.J.; Januzzi, J.L., Jr.; Khan, M.S.; et al. Effect of SGLT2 Inhibitors on Cardiovascular Outcomes Across Various Patient Populations. J. Am. Coll. Cardiol. 2023, 81, 2377–2387. [Google Scholar] [CrossRef] [PubMed]
- Afilalo, J. The Clinical Frailty Scale: Upgrade Your Eyeball Test. Circulation 2017, 135, 2025–2027. [Google Scholar] [CrossRef] [PubMed]
| Parameter | Patient Characteristics (n = 387) |
|---|---|
| Mean age, years (Me [Q1; Q3]) | 65.0 [59.0; 69.0] |
| Men, n (%) | 283 (73.1) |
| BMI, kg/m2 (Me [Q1; Q3]) | 29.3 [26.6; 32.1] |
| Smoking, n (%) | 178 (45.9) |
| Duration of CAD, years (Me [Q1; Q3]) | 2.0 [1.0; 5.0] |
| FC III-IV angina, n (%) | 70 (18.1) |
| PICS, n (%) | 221 (57.1) |
| Atherosclerosis of the extracranial brachiocephalic arteries, n (%) | 225 (58.1) |
| FC III-IV HF, n (%) | 32 (8.3) |
| PCI in history, n (%) | 73 (18.9) |
| TIA/Stroke in history, n (%) | 43 (11.1) |
| CEE in history, n (%) | 4 (1.0) |
| Ulcers, n (%) | 13 (3.4) |
| AH, n (%) | 323 (83.5) |
| AFL/AFib in preoperative period, n (%) | 44 (11.4) |
| Pacemaker implantation in history, n (%) | 2 (0.5) |
| DM II type, n (%) | 98 (25.3) |
| Impaired glucose tolerance, n (%) | 74 (19.1) |
| PAD, n (%) | 124 (32.0) |
| CRF, n (%) | 43 (11.1) |
| Bone fractures in history, n (%) | 30 (7.8) |
| Femoral neck fractures in family history, n (%) | 13 (3.4) |
| Rheumatoid arthritis, n (%) | 2 (0.5) |
| Secondary osteoporosis, n (%) | 7 (1.8) |
| Left main coronary artery stenosis, n (%) Number of diseased coronary arteries, pcs (Me [Q1; Q3]) | 86 (22.2) 2.0 [2.0; 3.0] |
| Parameter | Group of Patients without Frailty, n0 = 300 (77.5%) | Group of Frail Patients, n1 = 87 (22.5%) | p (Cramer’s V) |
|---|---|---|---|
| Mean age, years (Me [Q1; Q3]) | 65.0 [59.0; 70.0] | 64.0 [59.5; 67.0] | 0.128 |
| Men, n (%) | 209 (69.9) | 74 (84.1) | 0.008 * (0.134) |
| BMI, kg/m2 (Me [Q1; Q3]) | 29.1 [26.6; 31.8] | 30.1 [26.1; 32.7] | 0.459 |
| Smoking, n (%) | 130 (43.5) | 48 (54.5) | 0.067 |
| Duration of CAD, years (Me [Q1; Q3]) | 2.0 [1.0; 5.0] | 4.0 [1.0; 5.5] | 0.092 |
| Duration of AH, years (Me [Q1; Q3]) | 10.0 [5.0; 15.0] | 7.0 [3.0; 16.5] | 0.459 |
| FC III-IV Angina, n (%) | 55 (21.1) | 11 (15.7) | 0.319 |
| PICS, n (%) | 162 (54.2) | 59 (67.0) | 0.032 * (0.109) |
| Atherosclerosis of the extracranial brachiocephalic arteries, n (%) | 188 (62.9) | 44 (50.0) | 0.030 * (0.110) |
| III-IV HF, n (%) | 22 (8.3) | 6 (7.5) | 1.000 1 |
| PCI in history, n (%) | 55 (18.3) | 22 (25.3) | 0.153 |
| Stroke in history, n (%) | 30 (10.0) | 6 (6.8) | 0.412 1 |
| TIA in history, n (%) | 5 (1.7) | 2 (2.3) | 0.660 1 |
| CEE in history, n (%) | 3 (1.0) | 1 (1.1) | 1.000 1 |
| Ulcers, n (%) | 9 (3.0) | 9 (10.2) | 0.009 1* (0.144) |
| AH, n (%) | 247 (82.3) | 79 (90.8) | 0.056 |
| AFib in preoperative period, n (%) | 32 (12.7) | 8 (11.6) | 1.000 1 |
| AFL in preoperative period, n (%) | 4 (1.7) | 2 (2.6) | 0.636 1 |
| Pacemaker implantation in history, n (%) | 1 (0.3) | 1 (1.1) | 0.404 1 |
| Type II DM, n (%) | 82 (27.4) | 18 (20.5) | 0.189 |
| PAD, n (%) | 87 (29.1) | 37 (42.0) | 0.022 * (0.116) |
| CRF, n (%) | 41 (13.7) | 7 (8.0) | 0.161 |
| Apnea, n (%) | 10 (3.3) | 1 (1.1) | 0.468 1 |
| Bone fractures in history, n (%) | 17 (5.7) | 13 (14.9) | 0.010 1* (0.145) |
| Femoral neck fractures in family history, n (%) | 11 (3.7) | 2 (2.3) | 0.741 1 |
| Rheumatoid arthritis, n (%) | 1 (0.3) | 1 (1.1) | 0.400 1 |
| Secondary osteoporosis, n (%) | 8 (2.7) | 2 (2.3) | 1.000 1 |
| EuroSCORE II (Me [Q1; Q3]) | 1.6 [1.2; 2.0] | 1.4 [1.1; 1.7] | 0.063 |
| Parameter | Group of Patients without Frailty, n0 = 300 (77.5%) | Group of Frail Patients, n1 = 87 (22.5%) | p |
|---|---|---|---|
| CPB time, min (Me [Q1; Q3]) | 76.0 [65.0; 97.0] | 77.0 [64.0; 86.5] | 0.920 |
| Aortic cross-clamping, min (Me [Q1; Q3]) | 52.0 [40.0; 64.0] | 51.0 [40.0; 58.0] | 0.432 |
| Number of grafts, pcs (Me [Q1; Q3]) | 2.0 [2.0; 3.0] | 2.0 [2.0; 3.0] | 0.389 |
| Minimal systolic BP, mmHg (Me [Q1; Q3]) | 100.0 [92.0; 107.0] | 98.0 [96.0; 104.0] | 0.327 |
| MV time, min (Me [Q1; Q3]) | 645.0 [548.0; 825.0] | 640.0 [550.5; 879.0] | 0.787 |
| Blood loss on the first day after surgery, mL (Me [Q1; Q3]) | 300.0 [250.0; 400.0] | 350.0 [300.0; 500.0] | 0.092 |
| ICU length of stay, hours (Me [Q1; Q3]) | 21.5 [19.5; 24.5] | 23.0 [19.0; 43.0] | 0.310 |
| Outcome and Complications | Group of Patients without Frailty, n0 = 300 (77.5%) | Group of Frail Patients, n1 = 87 (22.5%) | p |
|---|---|---|---|
| Various complications, n (%) | 57 (19.6) | 30 (35.7) | 0.002 * (0.159) |
| Death, n (%) | 1 (0.3) | 4 (4.5) | 0.010 1* (0.156) |
| Myocardial infarction, n (%) | 2 (0.7) | 2 (2.3) | 0.218 1 |
| Stroke, n (%) | 4 (1.3) | 5 (5.7) | 0.031 1* (0.122) |
| Infectious complications, n (%) | 11 (3.7) | 6 (6.8) | 0.238 1 |
| HF with extended inotropic support, n (%) | 20 (6.7) | 9 (10.2) | 0.259 1 |
| Rhythm disturbances, n (%) | 31 (10.5) | 17 (19.5) | 0.025 * (0.115) |
| Pleural puncture, n (%) | 5 (1.7) | – | 0.593 1 |
| Sternal diastasis, n (%) | 1 (0.3) | 1 (1.1) | 0.404 1 |
| MODS, n (%) | 1 (0.3) | 2 (2.3) | 0.131 1 |
| Death within a year after CABG, n (%) | 2 (0.6) | 10 (11.5) | ˂0.001 1* (0.290) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Krivoshapova, K.; Tsygankova, D.; Bazdyrev, E.; Barbarash, O. Frailty as an Independent Predictor of Adverse Outcomes in Patients Undergoing Direct Myocardial Revascularization. Diagnostics 2024, 14, 1419. https://doi.org/10.3390/diagnostics14131419
Krivoshapova K, Tsygankova D, Bazdyrev E, Barbarash O. Frailty as an Independent Predictor of Adverse Outcomes in Patients Undergoing Direct Myocardial Revascularization. Diagnostics. 2024; 14(13):1419. https://doi.org/10.3390/diagnostics14131419
Chicago/Turabian StyleKrivoshapova, Kristina, Daria Tsygankova, Evgeny Bazdyrev, and Olga Barbarash. 2024. "Frailty as an Independent Predictor of Adverse Outcomes in Patients Undergoing Direct Myocardial Revascularization" Diagnostics 14, no. 13: 1419. https://doi.org/10.3390/diagnostics14131419
APA StyleKrivoshapova, K., Tsygankova, D., Bazdyrev, E., & Barbarash, O. (2024). Frailty as an Independent Predictor of Adverse Outcomes in Patients Undergoing Direct Myocardial Revascularization. Diagnostics, 14(13), 1419. https://doi.org/10.3390/diagnostics14131419







