External Tertiary-Care-Hospital Validation of the Epidemiological SEER-Based Nomogram Predicting Downgrading in High-Risk Prostate Cancer Patients Treated with Radical Prostatectomy
Abstract
1. Introduction
2. Materials and Methods
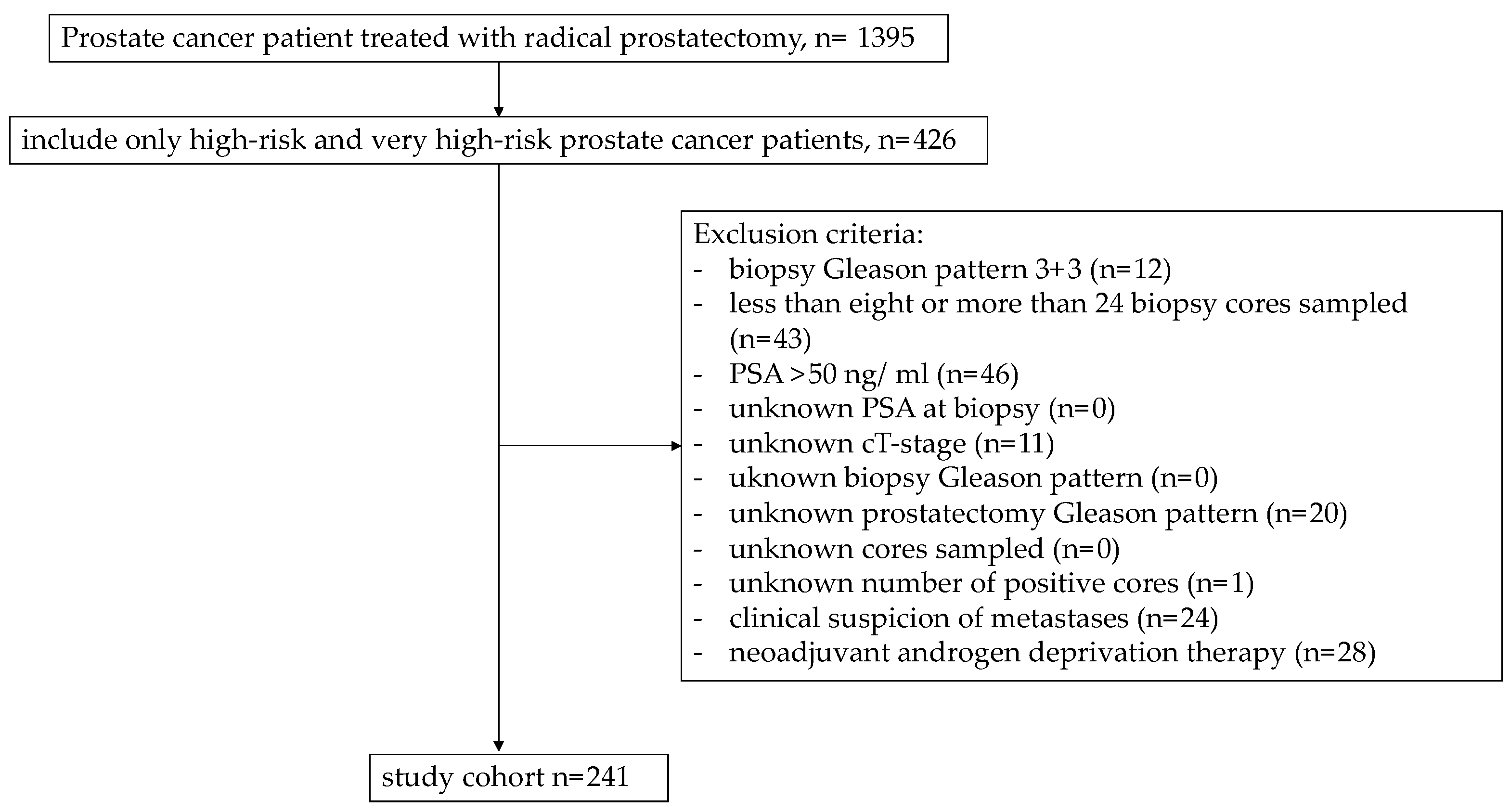
2.1. Patient Population
2.2. Covariates and Study Endpoints
2.3. Statistical Analyses
3. Results
3.1. Descriptive Characteristics
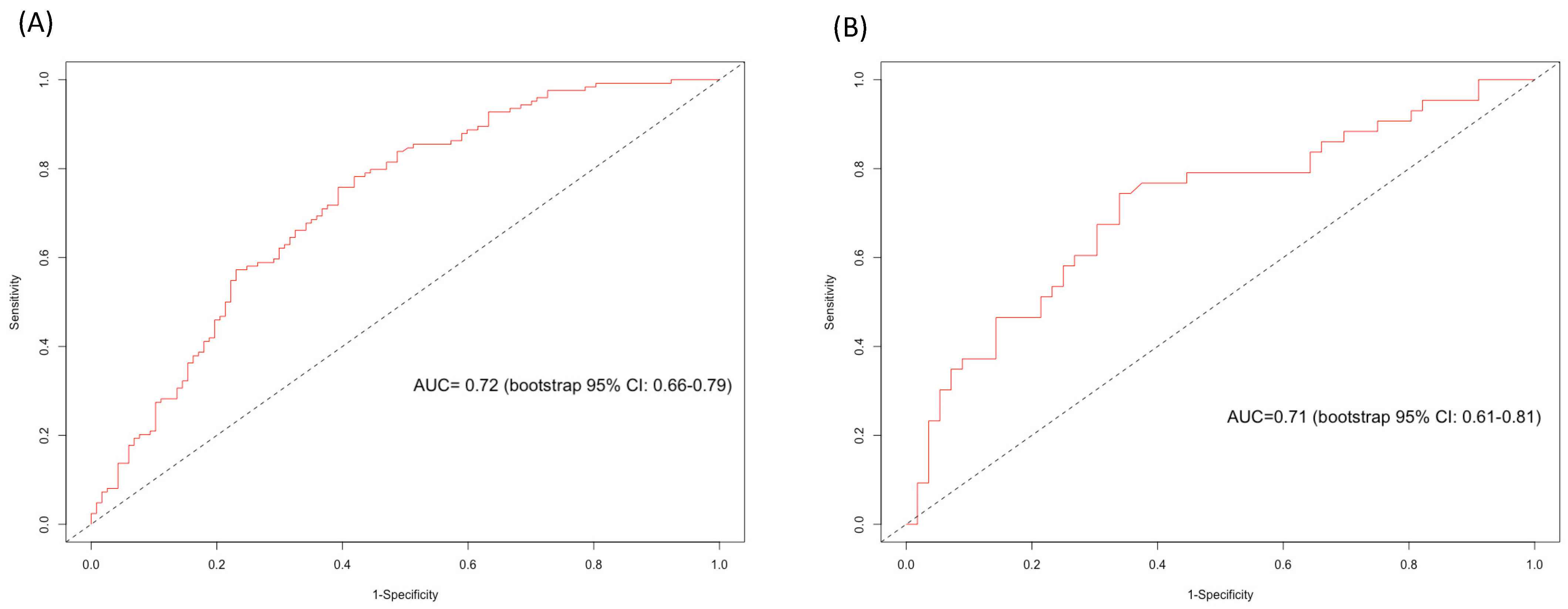
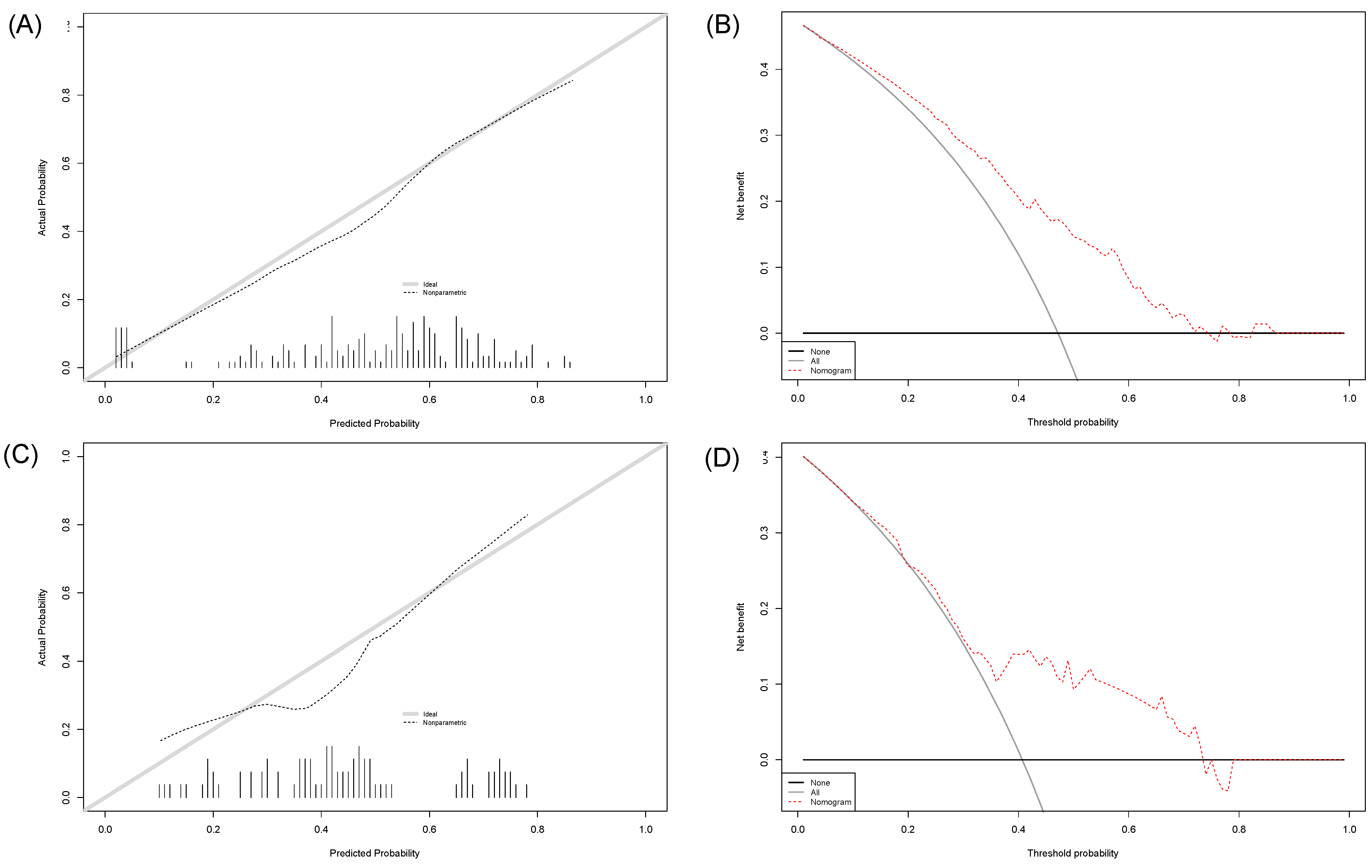
3.2. External Validation of the SEER-Based Nomogram Predicting Any Downgrading in NCCN Biopsied High-Risk Prostate Cancer Patients
3.3. Nomogram Cutoffs for Any-Downgrading Predictions
3.4. External Validation of the SEER-Based Nomogram Predicting Significant Downgrading in NCCN Biopsied High-Risk Prostate Cancer Patients
3.5. Nomogram Cutoffs for Significant-Downgrading Predictions
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Athanazio, D.; Gotto, G.; Shea-Budgell, M.; Yilmaz, A.; Trpkov, K. Global Gleason Grade Groups in Prostate Cancer: Concordance of Biopsy and Radical Prostatectomy Grades and Predictors of Upgrade and Downgrade. Histopathology 2017, 70, 1098–1106. [Google Scholar] [CrossRef] [PubMed]
- Epstein, J.I.; Feng, Z.; Trock, B.J.; Pierorazio, P.M. Upgrading and Downgrading of Prostate Cancer from Biopsy to Radical Prostatectomy: Incidence and Predictive Factors Using the Modified Gleason Grading System and Factoring in Tertiary Grades. Eur. Urol. 2012, 61, 1019–1024. [Google Scholar] [CrossRef] [PubMed]
- Goel, S.; Shoag, J.E.; Gross, M.D.; al Hussein Al Awamlh, B.; Robinson, B.; Khani, F.; Baltich Nelson, B.; Margolis, D.J.; Hu, J.C. Concordance Between Biopsy and Radical Prostatectomy Pathology in the Era of Targeted Biopsy: A Systematic Review and Meta-Analysis. Eur. Urol. Oncol. 2020, 3, 10–20. [Google Scholar] [CrossRef] [PubMed]
- Flammia, R.S.; Hoeh, B.; Hohenhorst, L.; Sorce, G.; Chierigo, F.; Panunzio, A.; Tian, Z.; Saad, F.; Leonardo, C.; Briganti, A.; et al. Adverse Upgrading and/or Upstaging in Contemporary Low-Risk Prostate Cancer Patients. Int. Urol. Nephrol. 2022, 54, 2521–2528. [Google Scholar] [CrossRef] [PubMed]
- Hoeh, B.; Flammia, R.; Hohenhorst, L.; Sorce, G.; Chierigo, F.; Tian, Z.; Saad, F.; Gallucci, M.; Briganti, A.; Terrone, C.; et al. Up- and Downgrading in Single Intermediate-Risk Positive Biopsy Core Prostate Cancer. Prostate Int. 2022, 10, 21–27. [Google Scholar] [CrossRef] [PubMed]
- Wenzel, M.; Preisser, F.; Wittler, C.; Hoeh, B.; Wild, P.J.; Tschäbunin, A.; Bodelle, B.; Würnschimmel, C.; Tilki, D.; Graefen, M.; et al. Correlation of MRI-Lesion Targeted Biopsy vs. Systematic Biopsy Gleason Score with Final Pathological Gleason Score after Radical Prostatectomy. Diagnostics 2021, 11, 882. [Google Scholar] [CrossRef] [PubMed]
- Humke, C.; Hoeh, B.; Preisser, F.; Wenzel, M.; Welte, M.N.; Theissen, L.; Bodelle, B.; Koellermann, J.; Steuber, T.; Haese, A.; et al. Concordance between Preoperative MpMRI and Pathological Stage and Its Influence on Nerve-Sparing Surgery in Patients with High-Risk Prostate Cancer. Curr. Oncol. 2022, 29, 2385–2394. [Google Scholar] [CrossRef]
- Rührup, J.; Preisser, F.; Theißen, L.; Wenzel, M.; Roos, F.C.; Becker, A.; Kluth, L.A.; Bodelle, B.; Köllermann, J.; Chun, F.K.H.; et al. MRI-Fusion Targeted vs. Systematic Prostate Biopsy–How Does the Biopsy Technique Affect Gleason Grade Concordance and Upgrading After Radical Prostatectomy? Front Surg. 2019, 6, 55. [Google Scholar] [CrossRef] [PubMed]
- Chun, F.K.H.; Steuber, T.; Erbersdobler, A.; Currlin, E.; Walz, J.; Schlomm, T.; Haese, A.; Heinzer, H.; McCormack, M.; Huland, H.; et al. Development and Internal Validation of a Nomogram Predicting the Probability of Prostate Cancer Gleason Sum Upgrading Between Biopsy and Radical Prostatectomy Pathology. Eur. Urol. 2006, 49, 820–826. [Google Scholar] [CrossRef]
- Chun, F.K.H.; Briganti, A.; Shariat, S.F.; Graefen, M.; Montorsi, F.; Erbersdobler, A.; Steuber, T.; Salonia, A.; Currlin, E.; Scattoni, V.; et al. Significant Upgrading Affects a Third of Men Diagnosed with Prostate Cancer: Predictive Nomogram and Internal Validation. BJU Int. 2006, 98, 329–334. [Google Scholar] [CrossRef]
- Hoeh, B.; Flammia, R.S.; Hohenhorst, L.; Sorce, G.; Chierigo, F.; Tian, Z.; Saad, F.; Gallucci, M.; Briganti, A.; Terrone, C.; et al. Non-Organ Confined Stage and Upgrading Rates in Exclusive PSA High-Risk Prostate Cancer Patients. Prostate 2022, 82, 687–694. [Google Scholar] [CrossRef] [PubMed]
- Nocera, L.; Wenzel, M.; Collà Ruvolo, C.; Würnschimmel, C.; Tian, Z.; Gandaglia, G.; Fossati, N.; Chun, F.K.H.; Mirone, V.; Graefen, M.; et al. The Impact of Race/Ethnicity on Upstaging and/or Upgrading Rates among Intermediate Risk Prostate Cancer Patients Treated with Radical Prostatectomy. World J. Urol. 2022, 40, 103–110. [Google Scholar] [CrossRef] [PubMed]
- Wenzel, M.; Würnschimmel, C.; Chierigo, F.; Mori, K.; Tian, Z.; Terrone, C.; Shariat, S.F.; Saad, F.; Tilki, D.; Graefen, M.; et al. Pattern of Biopsy Gleason Grade Group 5 (4 + 5 vs. 5 + 4 vs. 5 + 5) Predicts Survival After Radical Prostatectomy or External Beam Radiation Therapy. Eur. Urol. Focus 2022, 8, 710–717. [Google Scholar] [CrossRef] [PubMed]
- Würnschimmel, C.; Wenzel, M.; Chierigo, F.; Flammia, R.S.; Mori, K.; Tian, Z.; Shariat, S.F.; Saad, F.; Briganti, A.; Suardi, N.; et al. Presence of Biopsy Gleason Pattern 5 + 3 Is Associated with Higher Mortality after Radical Prostatectomy but Not after External Beam Radiotherapy Compared to Other Gleason Grade Group IV Patterns+. Prostate 2021, 81, 778–784. [Google Scholar] [CrossRef]
- Wenzel, M.; Würnschimmel, C.; Chierigo, F.; Flammia, R.S.; Tian, Z.; Shariat, S.F.; Gallucci, M.; Terrone, C.; Saad, F.; Tilki, D.; et al. Nomogram Predicting Downgrading in National Comprehensive Cancer Network High-Risk Prostate Cancer Patients Treated with Radical Prostatectomy. Eur. Urol. Focus 2021, 8, 1133–1140. [Google Scholar] [CrossRef] [PubMed]
- Würnschimmel, C.; Kachanov, M.; Wenzel, M.; Mandel, P.; Karakiewicz, P.I.; Maurer, T.; Steuber, T.; Tilki, D.; Graefen, M.; Budäus, L. Twenty-Year Trends in Prostate Cancer Stage and Grade Migration in a Large Contemporary German Radical Prostatectomy Cohort. Prostate 2021, 81, 849–856. [Google Scholar] [CrossRef]
- Wenzel, M.; Würnschimmel, C.; Ruvolo, C.C.; Nocera, L.; Tian, Z.; Saad, F.; Briganti, A.; Tilki, D.; Graefen, M.; Kluth, L.A.; et al. Increasing Rates of NCCN High and Very High-Risk Prostate Cancer versus Number of Prostate Biopsy Cores. Prostate 2021, 81, 874–881. [Google Scholar] [CrossRef]
- Hoeh, B.; Preisser, F.; Mandel, P.; Wenzel, M.; Humke, C.; Welte, M.N.; Müller, M.; Köllermann, J.; Wild, P.; Kluth, L.A.; et al. Inverse Stage Migration in Radical Prostatectomy—A Sustaining Phenomenon. Front Surg. 2021, 8, 612813. [Google Scholar] [CrossRef]
- Mohler, J.L.; Antonarakis, E.S.; Armstrong, A.J.; D’Amico, A.V.; Davis, B.J.; Dorff, T.; Eastham, J.A.; Enke, C.A.; Farrington, T.A.; Higano, C.S.; et al. Prostate Cancer, Version 2.2019. JNCCN J. Natl. Compr. Cancer Netw. 2019, 17, 479–505. [Google Scholar] [CrossRef]
- Scattoni, V.; Raber, M.; Abdollah, F.; Roscigno, M.; Dehò, F.; Angiolilli, D.; Maccagnano, C.; Gallina, A.; Capitanio, U.; Freschi, M.; et al. Biopsy Schemes with the Fewest Cores for Detecting 95% of the Prostate Cancers Detected by a 24-Core Biopsy. Eur. Urol. 2010, 57, 1–8. [Google Scholar] [CrossRef]
- Ghani, K.R.; Dundas, D.; Patel, U. Bleeding after Transrectal Ultrasonography-Guided Prostate Biopsy: A Study of 7-Day Morbidity after a Six-, Eight- and 12-Core Biopsy Protocol. BJU Int. 2004, 94, 1014–1020. [Google Scholar] [CrossRef] [PubMed]
- Abdollah, F.; Klett, D.E.; Sood, A.; Sammon, J.D.; Pucheril, D.; Dalela, D.; Diaz, M.; Peabody, J.O.; Trinh, Q.D.; Menon, M. Predicting Pathological Outcomes in Patients Undergoing Robot-Assisted Radical Prostatectomy for High-Risk Prostate Cancer: A Preoperative Nomogram. BJU Int. 2015, 116, 703–712. [Google Scholar] [CrossRef] [PubMed]
- van Leenders, G.L.H.; van der Kwast, T.H.; Grignon, D.J.; Evans, A.J.; Kristiansen, G.; Kweldam, C.F.; Litjens, G.; McKenney, J.K.; Melamed, J.; Mottet, N.; et al. The 2019 International Society of Urological Pathology (ISUP) Consensus Conference on Grading of Prostatic Carcinoma. Am. J. Surg. Pathol. 2020, 44, e87. [Google Scholar] [CrossRef] [PubMed]
- Collins, G.S.; Reitsma, J.B.; Altman, D.G.; Moons, K.G.M. Transparent Reporting of a Multivariable Prediction Model for Individual Prognosis or Diagnosis (TRIPOD): The TRIPOD Statement. BMJ 2015, 350, 55–63. [Google Scholar] [CrossRef] [PubMed]
- R: The R Project for Statistical Computing. Available online: https://www.r-project.org/ (accessed on 12 June 2022).
- Whitson, J.M.; Porten, S.P.; Cowan, J.E.; Simko, J.P.; Cooperberg, M.R.; Carroll, P.R. Factors Associated with Downgrading in Patients with High Grade Prostate Cancer. Urol. Oncol. Semin. Orig. Investig. 2013, 31, 442–447. [Google Scholar] [CrossRef]
- Ranasinghe, W.; Reichard, C.A.; Nyame, Y.A.; Sundi, D.; Tosoian, J.J.; Wilkins, L.; Alam, R.; Achim, M.F.; Wang, X.; Stephenson, A.J.; et al. Downgrading from Biopsy Grade Group 4 Prostate Cancer in Patients Undergoing Radical Prostatectomy for High or Very High Risk Prostate Cancer. J. Urol. 2020, 204, 748–753. [Google Scholar] [CrossRef]
- Wang, S.; Ryan Russell, J.; Drescher, M.; Park, A.; Legesse, T.; Kundra, V.; Tran, P.T.; Phelan, M.; Naslund, M.; Minhaj Siddiqui, M. Prostate Cancer Grade Downgrading at Time of Prostatectomy Provides Risk-Stratification Insight into Future Tumor Behavior after Prostatectomy. Prostate 2022, 82, 1520–1528. [Google Scholar] [CrossRef]
- Wenzel, M.; Preisser, F.; Theissen, L.H.; Humke, C.; Welte, M.N.; Wittler, C.; Kluth, L.A.; Karakiewicz, P.I.; Chun, F.K.H.; Mandel, P.; et al. The Effect of Adverse Patient Characteristics on Perioperative Outcomes in Open and Robot-Assisted Radical Prostatectomy. Front Surg. 2020, 7, 584897. [Google Scholar] [CrossRef] [PubMed]
- Zhu, D.; Shyr, W.; Toker, M.; Fram, E.; Cheng, J.; Kovac, E.Z.; Agalliu, I.; Aboumohamed, A.; Watts, K.L. The Impact of Surgical Downgrading on Prostate Cancer Recurrence: Systematic Review and Analysis of a Multiethnic Population. World J. Urol. 2022, 40, 709–718. [Google Scholar] [CrossRef]
| Characteristic | Overall 1 n = 241 (100%) | Downgrading 1 n = 124 (51%) | No Downgrading 1 n = 117 (49%) | p-Value 2 |
|---|---|---|---|---|
| Age at diagnosis (years) | 67 (63, 72) | 67 (62, 71) | 67 (64, 72) | 0.2 |
| Diabetes mellitus | 20 (8%) | 8 (7%) | 12 (10%) | 0.3 |
| Hypertension | 87 (36%) | 45 (36%) | 42 (36%) | >0.9 |
| PSA at diagnosis (ng/mL) | 10 (6, 21) | 8 (6, 12) | 14 (7, 24) | <0.001 |
| Number of prostate-biopsy cores | 13 (12, 14) | 13 (12, 14) | 13 (12, 14) | 0.14 |
| Number of positive prostate-biopsy cores | 6 (4, 8) | 6 (4, 8) | 6 (4, 8) | 0.8 |
| NCCN risk category | ||||
| High risk | 144 (60%) | 76 (61%) | 68 (58%) | 0.6 |
| Very high risk | 97 (40%) | 48 (39%) | 49 (42%) | |
| cT Stage | 0.2 | |||
| cT1 | 85 (35%) | 42 (34%) | 43 (37%) | |
| cT2 | 136 (56%) | 76 (61%) | 60 (51%) | |
| cT3a | 11 (5%) | 3 (2%) | 8 (7%) | |
| cT3b | 8 (3%) | 3 (2%) | 5 (4%) | |
| cT4 | 1 (1%) | 0 (0%) | 1 (1%) | |
| Gleason score at biopsy | ||||
| 3 + 4 | 22 (9%) | 1 (1%) | 21 (18%) | |
| 4 + 3 | 25 (10%) | 6 (5%) | 19 (16%) | |
| 4 + 4 | 95 (39%) | 59 (48%) | 36 (31%) | |
| 3 + 5 | 20 (8%) | 15 (12%) | 5 (4%) | |
| 5 + 3 | 1 (1%) | 0 (0%) | 1 (1%) | |
| 4 + 5 | 57 (24%) | 27 (22%) | 30 (26%) | |
| 5 + 4 | 14 (6%) | 10 (8%) | 4 (3%) | |
| 5 + 5 | 7 (3%) | 6 (5%) | 1 (1%) | |
| pT Stage | 0.004 | |||
| T2a | 8 (3%) | 6 (5%) | 2 (2%) | |
| T2b | 2 (1%) | 0 (0%) | 2 (2%) | |
| T2c | 65 (27%) | 43 (35%) | 22 (19%) | |
| T3a | 96 (40%) | 48 (39%) | 48 (41%) | |
| T3b | 67 (28%) | 27 (22%) | 40 (34%) | |
| T4 | 3 (1%) | 0 (0%) | 3 (3%) | |
| Gleason score at radical prostatectomy | ||||
| 3 + 3 | 5 (2%) | 5 (4%) | 0 (0%) | |
| 3 + 4 | 62 (26%) | 51 (41%) | 11 (10%) | |
| 4 + 3 | 66 (27%) | 50 (40%) | 16 (14%) | |
| 4 + 4 | 18 (8%) | 3 (2%) | 15 (13%) | |
| 3 + 5 | 6 (3%) | 2 (2%) | 4 (3%) | |
| 5 + 3 | 2 (0.5%) | 1 (1%) | 1 (1%) | |
| 4 + 5 | 68 (28%) | 10 (8%) | 58 (50%) | |
| 5 + 4 | 13 (5%) | 2 (2%) | 11 (10%) | |
| 5 + 5 | 1 (0.5%) | 0 (0%) | 1 (1%) | |
| Concordance | ||||
| Concordance | 68 (29%) | - | 68 (29%) | |
| Downgrading | 124 (51%) | 124 (51%) | - | |
| Upgrading | 49 (20%) | - | 49 (20%) | |
| Downgrading from any 5 + X to ≤ 4 + 4 | - | 43 (35%) | - |
| A: Nomogram Cut-Offs Predicting Any Downgrading between Biopsy and RP Gleason | |||
| Cutoff | Number of Patients above Nomogram Cutoff (%) | Number of Downgraded Patients above Nomogram Cutoff (True Positives) (%) | Number of Patients above Nomogram Cutoff without Downgrading (False Positives) (%) |
| 10 | 219 (90.9) | 123 (56.2) | 96 (43.8) |
| 15 | 219 (90.9) | 123 (56.2) | 96 (43.8) |
| 20 | 216 (89.6) | 122 (56.5) | 94 (43.5) |
| 25 | 212 (88.0) | 121 (57.1) | 91 (42.9) |
| 30 | 200 (83.0) | 118 (59.0) | 81 (41.0) |
| 35 | 188 (78.0) | 114 (60.6) | 74 (39.4) |
| 40 | 181 (75.1) | 110 (60.8) | 71 (39.2) |
| 45 | 158 (65.6) | 101 (63.9) | 57 (36.1) |
| 50 | 135 (56.0) | 89 (65.9) | 45 (34.1) |
| 55 | 112 (46.5) | 77 (68.8) | 35 (31.2) |
| 56 | 105 (43.6) | 73 (69.5) | 32 (30.5) |
| 57 | 101 (41.9) | 72 (71.3) | 29 (28.7) |
| 58 | 92 (38.2) | 66 (71.7) | 26 (28.3) |
| 59 | 88 (36.5) | 62 (70.5) | 26 (29.5) |
| 60 | 78 (32.4) | 55 (70.5) | 23 (29.5) |
| 61 | 70 (29.0) | 49 (70.0) | 21 (30.0) |
| 62 | 63 (26.1) | 45 (71.4) | 18 (28.6) |
| 63 | 60 (24.9) | 42 (70.0) | 18 (30.0) |
| 64 | 59 (24.5) | 41 (69.5) | 18 (30.5) |
| 65 | 59 (24.5) | 41 (69.5) | 18 (30.5) |
| 66 | 49 (20.3) | 35 (71.4) | 14 (28.6) |
| 67 | 42 (17.4) | 30 (71.4) | 12 (28.6) |
| 68 | 36 (14.9) | 25 (69.4) | 11 (30.6) |
| 69 | 34 (14.1) | 25 (73.5) | 9 (26.5) |
| 70 | 28 (11.6) | 21 (75.0) | 7 (25.0) |
| 75 | 16 (6.6) | 11 (68.8) | 5 (31.2) |
| 80 | 4 (1.7) | 3 (75.0) | 1 (25.0) |
| B: Nomogram Cut-Offs Predicting Significant Downgrading from Any Gleason Pattern 5 to RP Gleason ≥4 + 4 | |||
| Cutoff | Number of Patients above Nomogram Cutoff (%) | Number of Downgraded Patients above Nomogram Cutoff (True Positives) (%) | Number of Patients above Nomogram Cutoff without Downgrading (False Positives) (%) |
| 10 | 99 (100) | 43 (43.4) | 56 (56.6) |
| 15 | 95 (96) | 43 (45.3) | 52 (54.7) |
| 20 | 90 (90.9) | 41 (45.6) | 49 (54.4) |
| 25 | 87 (87.9) | 41 (47.1) | 46 (52.9) |
| 30 | 79 (79.8) | 38 (48.1) | 41 (51.9) |
| 35 | 73 (73.7) | 36 (49.3) | 37 (50.7) |
| 40 | 58 (58.6) | 33 (56.9) | 25 (43.2) |
| 41 | 57 (57.6) | 33 (57.9) | 24 (42.1) |
| 42 | 52 (52.5) | 32 (61.5) | 20 (38.5) |
| 43 | 47 (47.5) | 29 (61.7) | 18 (38.3) |
| 44 | 43 (43.4) | 26 (60.5) | 17 (39.5) |
| 45 | 41 (41.4) | 26 (63.4) | 15 (36.6) |
| 46 | 38 (38.4) | 24 (63.2) | 14 (36.8) |
| 47 | 35 (35.4) | 22 (62.9) | 13 (37.1) |
| 48 | 31 (31.3) | 20 (64.5) | 11 (35.5) |
| 49 | 28 (28.3) | 20 (71.4) | 8 (28.6) |
| 50 | 25 (25.3) | 17 (68.0) | 8 (32.0) |
| 51 | 23 (23.2) | 16 (69.6) | 7 (30.4) |
| 52 | 22 (22.2) | 16 (72.7) | 6 (27.3) |
| 53 | 21 (21.2) | 16 (76.2) | 5 (23.8) |
| 54 | 20 (20.2) | 15 (75.0) | 5 (25.0) |
| 55 | 20 (20.2) | 15 (75.0) | 5 (25.0) |
| 60 | 20 (20.2) | 15 (75.0) | 5 (25.0) |
| 65 | 20 (20.2) | 15 (75.0) | 5 (25.0) |
| 70 | 13 (13.1) | 10 (76.9) | 3 (23.1) |
| 75 | 4 (4.0) | 3 (75.0) | 1 (25) |
| 80 | 0 (0) | 0 (0) | 0 (0) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cano Garcia, C.; Wenzel, M.; Piccinelli, M.L.; Hoeh, B.; Landmann, L.; Tian, Z.; Humke, C.; Incesu, R.-B.; Köllermann, J.; Wild, P.J.; et al. External Tertiary-Care-Hospital Validation of the Epidemiological SEER-Based Nomogram Predicting Downgrading in High-Risk Prostate Cancer Patients Treated with Radical Prostatectomy. Diagnostics 2023, 13, 1614. https://doi.org/10.3390/diagnostics13091614
Cano Garcia C, Wenzel M, Piccinelli ML, Hoeh B, Landmann L, Tian Z, Humke C, Incesu R-B, Köllermann J, Wild PJ, et al. External Tertiary-Care-Hospital Validation of the Epidemiological SEER-Based Nomogram Predicting Downgrading in High-Risk Prostate Cancer Patients Treated with Radical Prostatectomy. Diagnostics. 2023; 13(9):1614. https://doi.org/10.3390/diagnostics13091614
Chicago/Turabian StyleCano Garcia, Cristina, Mike Wenzel, Mattia Luca Piccinelli, Benedikt Hoeh, Lea Landmann, Zhe Tian, Clara Humke, Reha-Baris Incesu, Jens Köllermann, Peter J. Wild, and et al. 2023. "External Tertiary-Care-Hospital Validation of the Epidemiological SEER-Based Nomogram Predicting Downgrading in High-Risk Prostate Cancer Patients Treated with Radical Prostatectomy" Diagnostics 13, no. 9: 1614. https://doi.org/10.3390/diagnostics13091614
APA StyleCano Garcia, C., Wenzel, M., Piccinelli, M. L., Hoeh, B., Landmann, L., Tian, Z., Humke, C., Incesu, R.-B., Köllermann, J., Wild, P. J., Würnschimmel, C., Graefen, M., Tilki, D., Karakiewicz, P. I., Kluth, L. A., Chun, F. K. H., & Mandel, P. (2023). External Tertiary-Care-Hospital Validation of the Epidemiological SEER-Based Nomogram Predicting Downgrading in High-Risk Prostate Cancer Patients Treated with Radical Prostatectomy. Diagnostics, 13(9), 1614. https://doi.org/10.3390/diagnostics13091614






