The Role of Cardiac Biomarkers in the Diagnosis of Hypertensive Emergency
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Statistical Analysis
3. Results
3.1. Demographic and Clinical Characteristics
3.2. Bivariate and Multivariate Regression Analysis
3.3. Receiver Operator Characteristic
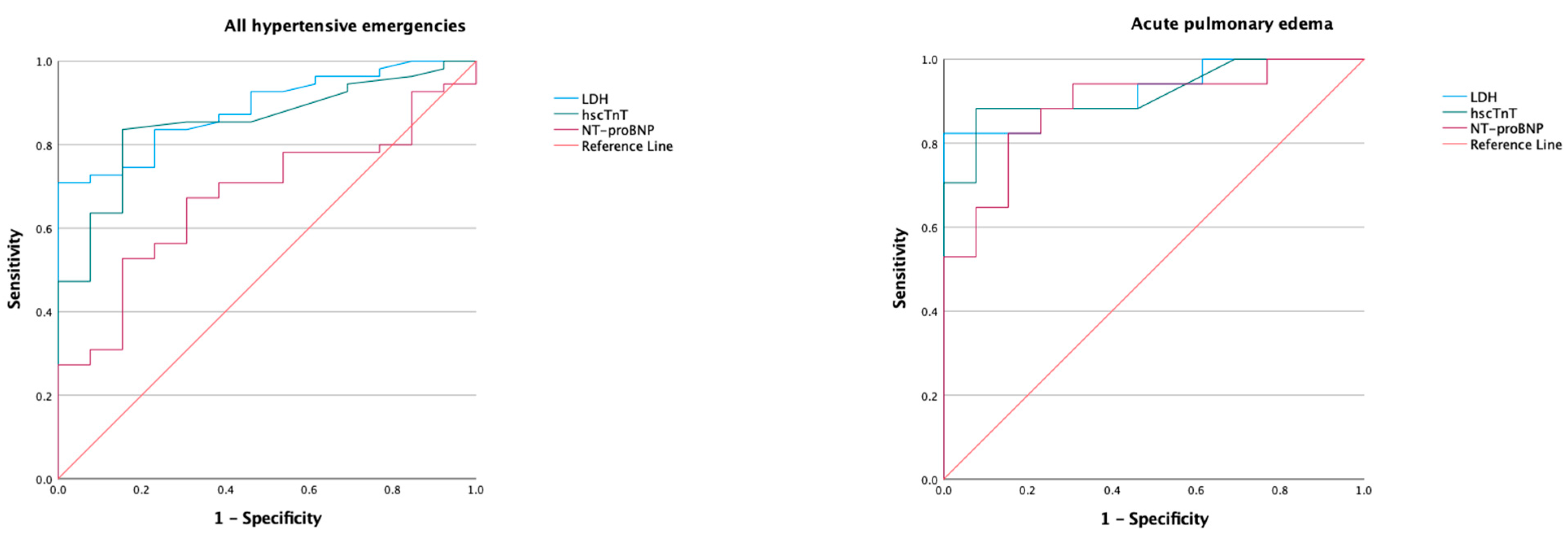
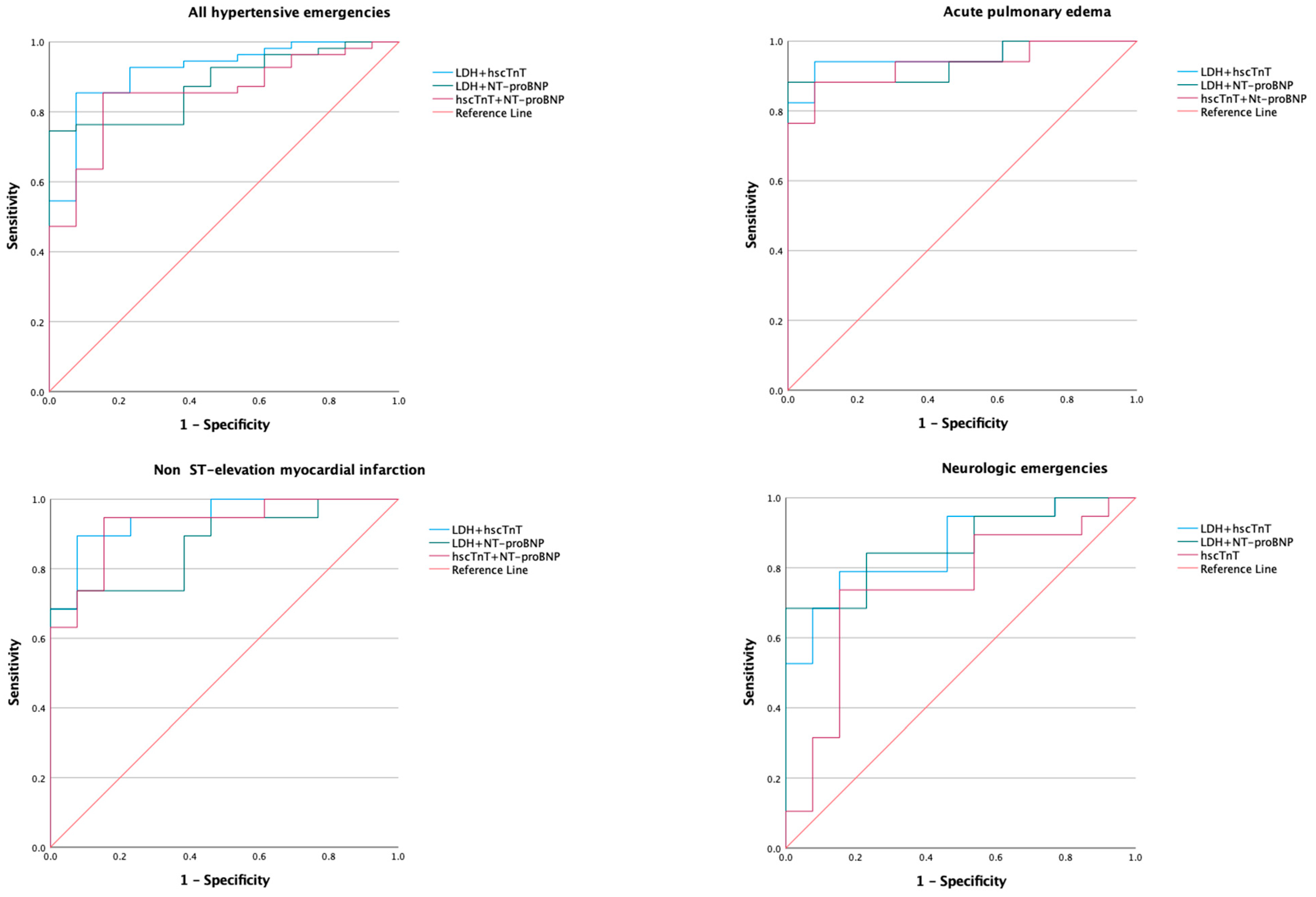
3.3.1. Lactate Dehydrogenase
3.3.2. High-Sensitivity Cardiac Troponin T
3.3.3. NT-proBNP
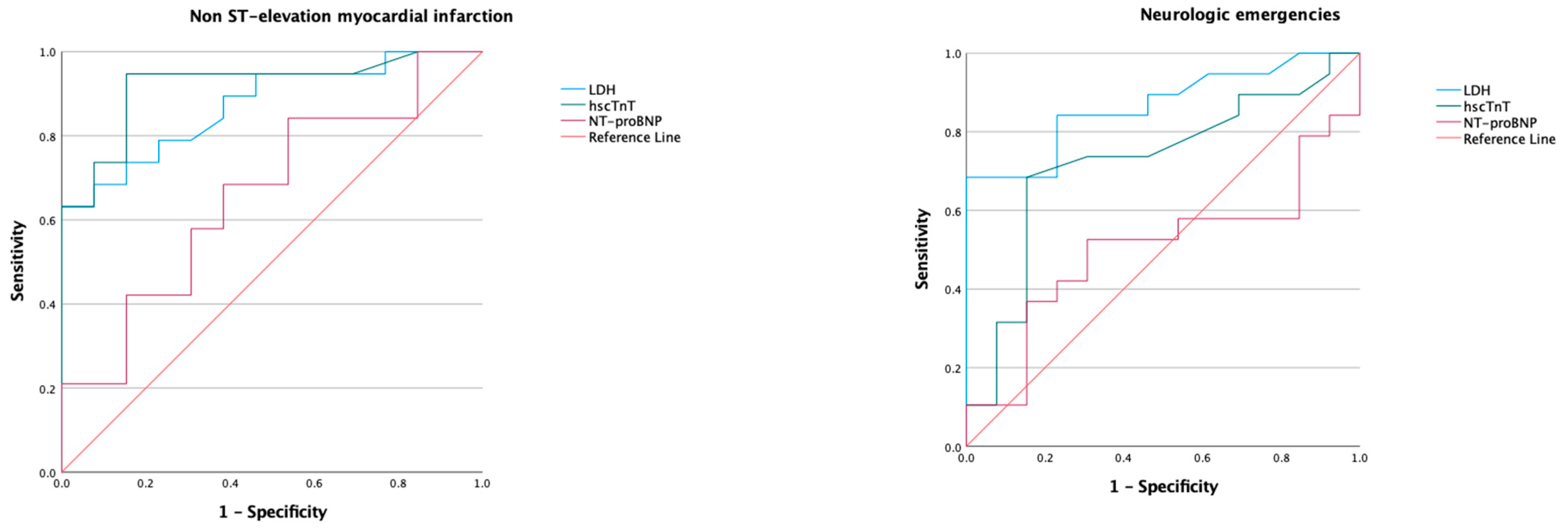
3.3.4. Model of Biomarkers
3.3.5. The Area under the Curve for Biomarkers Based on eGFR
4. Discussion
- LDH consistently showed diagnostic utility in differentiating the spectrum of hypertensive emergency from hypertensive urgency.
- hscTnT demomnstrateddiagnostic utility in the composite of hypertensive emergencies, NSTEMI, and acute pulmonary edema but not in the subgroup with neurological emergencies.
- NT-proBNP has diagnostic value for acute pulmonary edema but has poor utility in the composite of hypertensive emergency and in NSTEMI.
- Models of combinations of LDH and hscTnT had diagnostic utility for the composite of hypertensive emergencies, acute pulmonary edema, and NSTEMI. The combination of LDH with NT-proBNP did not perform differently from LDH.
Limitation of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Galson, S.W.; Stanifer, J.W.; Hertz, J.T.; Temu, G.; Thielman, N.; Gafaar, T.; Staton, C.A. The burden of hypertension in the emergency department and linkage to care: A prospective cohort study in Tanzania. PLoS ONE 2019, 14, 0211287. [Google Scholar] [CrossRef] [PubMed]
- Mobula, L.M.; Fisher, M.L.; Lau, N.; Estelle, A.; Wood, T.; Plyler, W. Prevalence of Hypertension among Patients Attending Mobile Medical Clinics in the Philippines after Typhoon Haiyan. PLoS Curr. 2016, 8. [Google Scholar] [CrossRef] [PubMed]
- van den Born, B.J.H.; Lip, G.Y.H.; Brguljan-Hitij, J.; Cremer, A.; Segura, J.; Morales, E.; Mahfoud, F.; Amraoui, F.; Persu, A.; Kahan, T.; et al. ESC Council on hypertension position document on the management of hypertensive emergencies. Eur. Heart J. Cardiovasc. Pharmacother. 2019, 5, 37–46. [Google Scholar] [CrossRef] [PubMed]
- Astarita, A.; Covella, M.; Vallelonga, F.; Cesareo, M.; Totaro, S.; Ventre, L.; Apra, F.; Veglio, F.; Milan, A. Hypertensive emergencies and urgencies in emergency departments: A systematic review and meta-analysis. J. Hypertens. 2020, 38, 1203–1210. [Google Scholar] [CrossRef]
- Williams, B.; Mancia, G.; Spiering, W.; Agabiti Rosei, E.; Azizi, M.; Burnier, M.; Clement, D.L.; Coca, A.; De Simone, G.; Dominiczak, A.; et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology (ESC) and the European Society of Hypertension (ESH). Eur. Heart J. 2018, 39, 3021–3104. [Google Scholar] [CrossRef]
- di Somma, S.; Sentimentale, A.; Magrini, L.; Tega, F.; Marino, R.; Ferri, E.; Fioretti, F.; Trabalzini, A.; Bertazzoni, G. Elevated B-type natriuretic peptide blood levels during hypertensive crisis: A novel diagnostic marker of acute coronary and cerebrovascular events? High Blood Press. Cardiovasc. Prev. 2008, 15, 23–28. [Google Scholar] [CrossRef]
- el Maraghi, S.; Yahia, H.; Heikal, A.; Ashraf, M. B-type natriuretic peptide in hypertensive crises: Diagnostic use in hypertensive urgencies and emergencies. Egyp J. Crit. Care Med. 2013, 1, 61–67. [Google Scholar] [CrossRef]
- Thygesen, K.; Alpert, J.S.; Jaffe, A.S.; Chaitman, B.R.; Bax, J.J.; Morrow, D.A.; White, H.D. Fourth universal definition of myocardial infarction (2018). J. Am. Coll. Cardiol. 2018, 72, 2231–2264. [Google Scholar] [CrossRef]
- Sciacovelli, L.; Aita, A.; Padoan, A.; Antonelli, G.; Plebani, M. ISO 15189 accreditation and competence: A new opportunity for laboratory medicine. J. Lab. Precis. Med. 2017, 2, 79. [Google Scholar] [CrossRef]
- DeLong, E.R.; DeLong, D.M.; Clarke-Pearson, D.L. Comparing the Areas under Two or More Correlated Receiver Operating Characteristic Curves: A Nonparametric Approach. Biometrics 1988, 44, 837. [Google Scholar] [CrossRef]
- Vallelonga, F.; Cesareo, M.; Menon, L.; Leone, D.; Lupia, E.; Morello, F.; Totaro, S.; Aggiusti, C.; Salvetti, M.; Ioverno, A.; et al. Hypertensive emergencies and urgencies: A preliminary report of the ongoing Italian multicentric study ERIDANO. Hypertens. Res. 2023, 20, 1–12. [Google Scholar] [CrossRef]
- Salvetti, M.; Paini, A.; Colonetti, E.; Tarozzi, L.; Bertacchini, F.; Aggiusti, C.; Stassaldi, D.; Rosei, C.A.; Rosei, E.A.; Muiesan, M.L. Hypertensive emergencies and urgencies: A single-centre experience in Northern Italy 2008–2015. J. Hypertens. 2020, 38, 52–58. [Google Scholar] [CrossRef] [PubMed]
- Fragoulis, C.; Dimitriadis, K.; Siafi, E.; Iliakis, P.; Kasiakogias, A.; Kalos, T.; Leontsinis, I.; Andrikou, I.; Konstantinidis, D.; Nihoyannopoulos, P.; et al. Profile and management of hypertensive urgencies and emergencies in the emergency cardiology department of a tertiary hospital: A 12-month registry. Eur. J. Prev. Cardiol. 2022, 29, 194–201. [Google Scholar] [CrossRef] [PubMed]
- Martins, J.T.; Li, D.J.; Baskin, L.B.; Jialal, I.; Keffer, J.H. Comparison of cardiac troponin I and lactate dehydrogenase isoenzymes for the late diagnosis of myocardial injury. Am. J. Clin. Pathol. 1996, 106, 705–708. [Google Scholar] [CrossRef] [PubMed]
- Khan, A.A.; Allemailem, K.S.; Alhumaydhi, F.A.; Gowder, S.J.T.; Rahmani, A.H. The Biochemical and Clinical Perspectives of Lactate Dehydrogenase: An Enzyme of Active Metabolism. Endocr. Metab. Immune Disord. Drug Targets 2020, 20, 855–868. [Google Scholar] [CrossRef] [PubMed]
- Wang, A.; Tian, X.; Zuo, Y.; Wang, X.; Xu, Q.; Meng, X.; Chen, P.; Li, H.; Wang, Y. High lactate dehydrogenase was associated with adverse outcomes in patients with acute ischemic stroke or transient ischemic attack. Ann. Palliat. Med. 2021, 10, 101850195. [Google Scholar] [CrossRef]
- Jaiswar, S.P.; Amrit, G.; Rekha, S.; Natu, S.N.; Mohan, S. Lactic Dehydrogenase: A Biochemical Marker for Preeclampsia–Eclampsia. J. Obstet. Gynaecol. India 2011, 61, 645. [Google Scholar] [CrossRef] [PubMed]
- Kim, W.; Kim, B.S.; Kim, H.J.; Lee, J.H.; Shin, J.; Shin, J.H. Clinical implications of cardiac troponin-I in patients with hypertensive crisis visiting the emergency department. Ann. Med. 2022, 54, 507–515. [Google Scholar] [CrossRef] [PubMed]
- Thiele, S.; Britz, S.; Landsiedel, L.; Wallaschofski, H.; Lohmann, T. Short-term changes in hsCRP and NT-proBNP levels in hypertensive emergencies. Horm. Metab. Res. 2008, 40, 561–565. [Google Scholar] [CrossRef]
- Silver, M.A.; Maisel, A.; Yancy, C.W.; McCullough, P.A.; Burnett, J.C.; Francis, G.S.; Mehra, M.R.; Peacock, W.F.; Fonarow, G.; Gibler, W.B.; et al. BNP Consensus Panel 2004: A clinical approach for the diagnostic, prognostic, screening, treatment monitoring, and therapeutic roles of natriuretic peptides in cardiovascular diseases. Congest. Heart Fail. 2004, 10, 1–30. [Google Scholar] [CrossRef]
- Kim, B.S.; Lee, Y.; Lim, Y.H.; Shin, J.; Shin, J.H. Association between B-type natriuretic peptide and long-term mortality in patients with acute severe hypertension visiting the emergency department. Sci. Rep. 2022, 12, 21001. [Google Scholar] [CrossRef] [PubMed]
- de Lemos, J.A.; Morrow, D.A.; Bentley, J.H.; Omland, T.; Sabatine, M.S.; McCabe, C.H.; Hall, C.; Cannon, C.P.; Braunwald, E. The prognostic value of B-type natriuretic peptide in patients with acute coronary syndromes. N. Engl. J. Med. 2001, 345, 1014–1021. [Google Scholar] [CrossRef] [PubMed]
- Viau, D.M.; Sala-Mercado, J.A.; Spranger, M.D.; O’Leary, D.S.; Levy, P.D. The pathophysiology of hypertensive acute heart failure. Heart 2015, 101, 1861–1867. [Google Scholar] [CrossRef] [PubMed]
- De Lemos, J.A.; McGuire, D.K.; Drazner, M.H. B-type natriuretic peptide in cardiovascular disease. Lancet 2003, 362, 316–322. [Google Scholar] [CrossRef] [PubMed]

| Variables | Hypertensive Crisis | p-Value | Type of Hypertensive Emergency | p-Value * | |||
|---|---|---|---|---|---|---|---|
| Hypertensive Urgency (n = 16) | Hypertensive Emergency (n = 66) | Acute Pulmonary Edema (n = 24) | Non-ST Elevation Myocardial Infarction (n = 20) | Neurological Emergencies (n = 22) | |||
| Age in years, mean (SD) | 49.5 (15.6) | 47.9 (13.2) | 0.673 | 48.0 (15.7) | 53.2 (11.6) | 42.8 (9.6) | 0.099 |
| Males, n (%) | 5 (31.3) | 44 (66.7) | 0.077 | 15 (62.5) | 14 (70) | 15 (68.2) | |
| Systolic blood pressure (mmHg) | 216.1 (27.6) | 217.1 (28.8) | 0.902 | 223.4 (27.3) | 202.9 (26.7) | 223.2 (29) | 0.094 |
| Diastolic blood pressure (mmHg) | 118.4 (16.6) b,d | 130.2 (19.9) | 0.015 | 136 (18.5) a,c | 116.7 (16.8) b,d | 136.1 (18.5) a,c | <0.001 |
| Mean arterial pressure (mmHg) | 151 (16.8) | 159.2 (20.4) | 0.122 | 165.1 (18.6) c | 145.4 (17.2) b,d | 165.2 (19.4) c | <0.001 |
| Cornell voltage indices (mm) | 21.5 [5.8–28.3] b | 30 [21–40] | 0.005 | 37 [30.3–45.8] a,c | 21.5 [17.5–26.5] b | 27 [18.5–43] | <0.001 |
| Hemoglobin (g/dL) | 13.8 (1.8) | 13.8 (2.2) | 0.810 | 13 (2.0) | 14.3 (2.3) | 14.1 (2) | 0.155 |
| Platelet count (×109/L) | 276.5 [250.5–373] | 283 [252–346] | 0.951 | 286 [254.3–343.8] | 286 [268–440] | 277 (202.5–340.5) | 0.803 |
| Creatinine (μmol/L) | 82.5 [64–99.5] b | 110.5 [90.8–190.8] | <0.001 | 192.5 [101–266] | 107.5 [90.3–124] | 103.5 (82–119) | <0.001 |
| eGFR (mL/min/1.73 m2 | 81.5 [64–105.8] b | 63 [36.5–79.5] | 0.006 | 36.5 [23–65.5] a,d | 66.5 [43.3–80.5] | 71.5 [62.8–98.5] b | <0.001 |
| Lactate dehydrogenase (U/L) | 200 [170–231] b,c,d | 283 [230.8–330.5] | <0.001 | 282 [269.5–342.5] a | 285 [226–353] a | 282 [229–314.3] a | <0.001 |
| Haptoglobin (g/L) | 1.93 [1.6–2.3] | 1.97 [1.22–2.64] | 0.797 | 1.88 [1.08–2.68] | 2.3 [1.72–2.87] | 1.97 [1.1–2.6] | 0.600 |
| hscTnT (ng/L) | 11 [8–14] b,c | 40 [17.5–165] | <0.001 | 56.5 [32.3–161.5] a,d | 182 [25–277.3] a,d | 17 [12–25] b,c | <0.001 |
| NT-proBNP (ng/L) | 136 [51–396] b | 528 [113–2117] | 0.024 | 1985 [532.8–4577] a,d | 315 [113–1435] | 151 [21.5–845.5] b | <0.001 |
| Variable | Unadjusted OR (95% CI) | p-Value | Adjusted OR (95% CI) | p-Value * |
|---|---|---|---|---|
| Age in years, mean (SD) | 0.99 (0.95–1.04) | 0.685 | - | - |
| Male gender | 0.23 (0.07–0.74) | 0.013 | 4.57 (0.69–30.4) | 0.116 |
| Systolic BP (mmHg) | 1.00 (0.98–1.02) | 0.898 | - | - |
| Diastolic BP (mmHg) | 1.04 (1.00–1.07) | 0.047 | - | - |
| Mean arterial pressure (mmHg) | 1.02 (0.99–1.05) | 0.115 | - | - |
| Creatinine (μmol/L) | 1.04 (1.01–1.06) | 0.004 | 1.03 (0.99–1.08) | 0.111 |
| Hemoglobin (g/dL) | 0.99 (0.79–1.26) | 0.976 | - | - |
| LDH > 190 U/L | 14.7 (3.53–62.4) | <0.001 | 20.04 (1.66–242) | 0.018 |
| Haptoglobin (g/L) | 1.23 (0.85–1.79) | 0.271 | - | - |
| Haptoglobin > 2.0 (g/L) | 1.51 (0.49–4.67) | 0.474 | - | - |
| Platelet × 109/L | 1.00 (0.99–1.00) | 0.860 | - | - |
| hscTnT (ng/L) | 1.10 (0.97–1.25) | 0.121 | - | - |
| NT-proBNP (ng/L) | 1.00 (1.00–1.01) | 0.107 | - | - |
| NT-proBNP > 300 ng/L | 4.02 (1.15–14.0) | 0.029 | 0.20 (0.02–2.06) | 0.175 |
| Cornell voltage indices (mm) | 1.09 (1.032–1.15) | 0.002 | 1.10 (1.00–1.21) | 0.045 |
| Type of Hypertensive Emergency and Biomarker | AUC (95% CI) | Cut-Off Point * | Sensitivity, % | Specificity, % | Positive Likelihood Ratio | Negative Likelihood Ratio | p Value for AUC |
|---|---|---|---|---|---|---|---|
| All hypertensive emergencies: | |||||||
| LDH | 0.88 (0.80 to 0.97) | 225 | 83 | 77 | 3.11 | 0.22 | <0.001 |
| hscTnT | 0.85 (0.80 to 0.96) | 14.5 | 83 | 85 | 5.60 | 0.19 | <0.001 |
| NT-proBNP | 0.67 (0.53 to 0.81) | 208 | 67 | 69 | 2.06 | 0.52 | 0.059 |
| LDH + hscTnT | 0.92 (0.84 to 1.00) | - | - | - | <0.001 | ||
| LDH + NT-proBNP | 0.88 (0.80 to 0.96) | - | - | - | <0.001 | ||
| hscTnT + NT-proBNP | 0.85 (0.75 to 0.95) | - | - | - | <0.001 | ||
| Acute pulmonary edema: | |||||||
| LDH | 0.92 (0.83 to 1.00) | 232 | 82 | 85 | 5.47 | 0.21 | <0.001 |
| hscTnT | 0.92 (0.82 to 1.00) | 17.5 | 88 | 85 | 5.87 | 0.14 | <0.001 |
| NT-proBNP | 0.89 (0.77 to 1.00) | 437 | 88 | 77 | 3.83 | 0.16 | <0.001 |
| LDH + hscTnT | 0.96 (0.88 to 1.00) | - | - | - | <0.001 | ||
| LDH + NT-proBNP | 0.94 (0.85 to 1.00) | - | - | - | <0.001 | ||
| hscTnT + NT-proBNP | 0.93 (0.84 to 1.00) | - | - | - | <0.001 | ||
| Non-ST-elevation myocardial infarction: | |||||||
| LDH | 0.87 (0.75 to 0.99) | 218 | 84 | 61 | 2.15 | 0.16 | <0.001 |
| hscTnT | 0.92 (0.82 to 1.00) | 17.5 | 90 | 85 | 6.00 | 0.12 | <0.001 |
| NT-proBNP | 0.66 (0.47 to 0.085) | 202 | 58 | 62 | 1.53 | 0.68 | 0.130 |
| LDH + hscTnT | 0.95 (0.88 to 1.00) | - | - | - | <0.001 | ||
| LDH + NT-proBNP | 0.87 (0.75 to 0.99) | - | - | - | <0.001 | ||
| hscTnT + NT-proBNP | 0.93 (0.84 to 1.00) | - | - | - | <0.001 | ||
| Neurological emergencies: | |||||||
| LDH | 0.87 (0.74 to 0.99) | 225 | 84 | 77 | 3.65 | 0.21 | 0.001 |
| hscTnT | 0.72 (0.54 to 0.91) | 14.5 | 68 | 85 | 4.53 | 0.38 | 0.035 |
| NT-proBNP | 0.50 (0.30 to 0.71) | 208 | 53 | 70 | 1.77 | 0.67 | 0.985 |
| LDH + hscTnT | 0.86 (0.73 to 0.99) | - | - | - | 0.001 | ||
| LDH + NT-proBNP | 0.87 (0.74 to 0.99) | - | - | - | 0.022 | ||
| hscTnT + NT-proBNP | 0.74 (0.56 to 0.92) | - | - | - | 0.001 | ||
| Acute pulmonary edema and neurological emergencies: | |||||||
| LDH | 0.89 (0.81 to 0.98) | 225 | 86 | 77 | 3.74 | 0.18 | <0.001 |
| hscTnT | 0.82 (0.69 to 0.94) | 18.5 | 78 | 85 | 5.20 | 0.26 | 0.001 |
| NT-proBNP | 0.68 (0.53 to 0.84) | 215 | 69 | 70 | 2.30 | 0.44 | 0.051 |
| LDH + hscTnT | 0.91 (0.82 to 0.99) | - | - | - | <0.001 | ||
| LDH + NT-proBNP | 0.89 (0.79 to 0.98) | - | - | - | 0.001 | ||
| hscTnT + NT-proBNP | 0.81 (0.69 to 0.94) | - | - | - | <0.001 |
| Biomarker and Models | Difference between Areas | Standard Error | 95% CI | z Statistic | p Value |
|---|---|---|---|---|---|
| LDH vs. hscTnT | 0.035 | 0.057 | −0.077 to 0.147 | 0.611 | 0.541 |
| LDH vs. NT-proBNP | 0.210 | 0.072 | 0.067 to 0.352 | 2.912 | 0.004 |
| LDH vs. LDH+hscTnT | 0.033 | 0.030 | −0.026 to 0.092 | 1.094 | 0.274 |
| LDH vs. LDH+NT-proBNP | 0.006 | 0.012 | −0.018 to 0.031 | 0.510 | 0.610 |
| LDH vs. hscTnT+NT-proBNP | 0.033 | 0.058 | −0.082 to 0.147 | 0.563 | 0.573 |
| hscTnT vs. NT-proBNP | 0.176 | 0.077 | 0.024 to 0.327 | 2.277 | 0.023 |
| hscTnT vs. LDH+hscTnT | 0.068 | 0.037 | −0.004 to 0.139 | 1.855 | 0.064 |
| hscTnT vs. LDH+NT-proBNP | 0.029 | 0.058 | −0.086 to 0.143 | 0.492 | 0.623 |
| hscTnT vs. hscTnT+NT-proBNP | 0.002 | 0.005 | −0.008 to 0.012 | 0.398 | 0.690 |
| NT-proBNP vs. LDH+hscTnT | 0.243 | 0.074 | 0.099 to 0.388 | 3.306 | <0.001 |
| NT-proBNP vs. LDH+NT-proBNP | 0.204 | 0.065 | 0.076 to 0.332 | 3.124 | 0.002 |
| NT-proBNP vs. hscTnT+NT-proBNP | 0.178 | 0.079 | 0.022 to 0.333 | 2.242 | 0.025 |
| LDH+hscTnT vs. LDH+NT-proBNP | 0.039 | 0.034 | −0.027 to 0.105 | 1.168 | 0.243 |
| LDH+hscTnT vs. hscTnT+NT-proBNP | 0.066 | 0.038 | −0.008 to 0.140 | 1.741 | 0.082 |
| LDH+NT-proBNP vs. hscTnT+NT-proBNP | 0.027 | 0.060 | −0.090 to 0.144 | 0.445 | 0.656 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Talle, M.A.; Doubell, A.F.; Robbertse, P.-P.S.; Lahri, S.; Herbst, P.G. The Role of Cardiac Biomarkers in the Diagnosis of Hypertensive Emergency. Diagnostics 2023, 13, 1605. https://doi.org/10.3390/diagnostics13091605
Talle MA, Doubell AF, Robbertse P-PS, Lahri S, Herbst PG. The Role of Cardiac Biomarkers in the Diagnosis of Hypertensive Emergency. Diagnostics. 2023; 13(9):1605. https://doi.org/10.3390/diagnostics13091605
Chicago/Turabian StyleTalle, Mohammed A., Anton F. Doubell, Pieter-Paul S. Robbertse, Sa’ad Lahri, and Philip G. Herbst. 2023. "The Role of Cardiac Biomarkers in the Diagnosis of Hypertensive Emergency" Diagnostics 13, no. 9: 1605. https://doi.org/10.3390/diagnostics13091605
APA StyleTalle, M. A., Doubell, A. F., Robbertse, P.-P. S., Lahri, S., & Herbst, P. G. (2023). The Role of Cardiac Biomarkers in the Diagnosis of Hypertensive Emergency. Diagnostics, 13(9), 1605. https://doi.org/10.3390/diagnostics13091605






