Evaluation of the RDW Index (Red Cell Distribution Width) in Women with Breast Cancer Treated with Doxorubicin in a One-Year Follow-Up Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Blood Samples and Measurements
2.3. Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Siegel, R.; Miller, K.; Jemal, A. Cancer Statistics. CA Cancer J. Clin. 2021, 71, 7–33. [Google Scholar] [CrossRef] [PubMed]
- INCA. Estimate: Incidence of Cancer in Brazil. MS/SVS/DASIS/CGIAE/Sistema de Informação Sobre Mortalidade 2021. Available online: https://www.inca.gov.br/numeros-de-cancer (accessed on 24 May 2021).
- Curigliano, G.; Cardinale, D.; Dent, S.; Criscitiello, C.; Aseyev, O.; Lenihan, D.; Cipolla, C.M. Cardiotoxicity of anticancer treatments: Epidemiology, detection, and management. CA Cancer J. Clin. 2016, 66, 309–325. [Google Scholar] [CrossRef] [PubMed]
- Förhécz, Z.; Gombos, T.; Borgulya, G.; Pozsonyi, Z.; Prohászka, Z.; Jánoskuti, L. Red cell distribution width in heart failure: Prediction of clinical events and relation-ship with markers of ineffective erythropoiesis, inflammation, renal function, and nutritional state. Am. Heart J. 2009, 158, 659–666. [Google Scholar] [CrossRef] [PubMed]
- Demir, A.; Yarali, N.; Fisgin, T.; Duru, F.; Kara, A. Most reliable indices in differentiation between thalassemia trait and iron deficiency anemia. Pediatr. Int. 2002, 44, 612–616. [Google Scholar] [CrossRef] [PubMed]
- Zeben, D.; Bieger, R.; Wermeskerken, R.K.A.; Castel, A.; Hermans, J. Evaluation of microcytosis using serum ferritin and red blood cell distribution width. Eur. J. Haematol. 1990, 44, 106–109. [Google Scholar] [CrossRef]
- Gunebakmaz, O.; Kaya, M.G.; Duran, M.; Akpek, M.; Elcik, D.; Eryol, N.K. Red blood cell distribution width in ‘Non-Dippers’ versus ‘Dippers’. Cardiology 2012, 123, 154–159. [Google Scholar] [CrossRef]
- Nishizaki, Y.; Yamagami, S.; Suzuki, H.; Joki, Y.; Takahashi, S.; Sesoko, M.; Yamashita, H.; Kuremoto, K.; Shinozaki, T.; Daida, H. Red blood cell distribution width as an effective tool for detecting fatal heart failure in super-elderly patients. Intern. Med. 2012, 51, 2271–2276. [Google Scholar] [CrossRef]
- Karabulut, A.; Uzunlar, B. Correlation between red cell distribution width and coronary ectasia in the acute myocardial infarction. Clin. Appl. Thromb. Hemost. 2012, 18, 551–552. [Google Scholar] [CrossRef]
- Yesil, A.; Senates, E.; Bayoglu, I.; Erdem, E.D.; Demirtunç, R.; Övünç, A.O.K. Red cell distribution width: A novel marker of activity in inflammatory bowel disease. Gut Liver 2011, 5, 460–467. [Google Scholar] [CrossRef]
- de Gonzalo-Calvo, D.; de Luxan-Delgado, B.; Rodriguez-Gonzalez, S.; García-Macia, M.; Suárez, F.M.; Solano, J.J.; Rodríguez-Colunga, M.J.; Coto-Montes, A. Interleukin 6, soluble tumor necrosis factor receptor I and red blood cell distribution width as biological markers of functional dependence in an elderly population: A translational approach. Cytokine 2012, 58, 193–198. [Google Scholar] [CrossRef]
- Huang, D.; Ma, R.; Xiang, Y. Utility of red cell distribution width as a prognostic factor in young breast cancer patients. Medicine 2016, 95, e3430. [Google Scholar] [CrossRef] [PubMed]
- Lu, F.; Pan, S.; Qi, Y.; Li, X.; Wang, J. The Clinical Application Value of RDW, CA153, and MPV in Breast Cancer. Clin. Lab. 2021, 67. [Google Scholar] [CrossRef] [PubMed]
- Yoo, Y.; Park, S.; Kim, H.; Jung, H.-E.; Kim, J.-Y.; Kim, M.-H. Preoperative Routine Laboratory Markers for Predicting Postoperative Recurrence and Death in Patients with Breast Cancer. J. Clin. Med. 2021, 10, 2610. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Lee, H.; Cho, J.; Park, H.-K.; Yang, H.-J. Correlations between female breast density and biochemical markers. J. Phys. Ther. Sci. 2015, 27, 2097–2100. [Google Scholar] [CrossRef] [PubMed]
- Chiba, T.; Marusawa, H.; Ushijima, T. Inflammation associated cancer development in digestive organs: Mechanisms and roles for genetic and epigenetic modulation. Gastroenterology 2012, 143, 550–563. [Google Scholar] [CrossRef]
- Baicus, C.; Caraiola, S.; Rimbas, M.; Patrascu, R.; Baicus, A.; Badea, C.; Balanescu, E.; Balea, M.; Constantin, G.; Constantinescu, I.; et al. Utility of routine hematological and inflammation parameters for the diagnosis of cancer in involuntary weight loss. J. Investig. Med. 2011, 59, 951–955. [Google Scholar] [CrossRef]
- López-Sendón, J.; Álvarez-Ortega, C.; Zamora Auñon, P.; Buño Soto, A.; Lyon, A.R.; Farmakis, D.; Cardinale, D.; Canales Albendea, M.; Feliu Batlle, J.; Rodríguez Rodríguez, I.; et al. Classification, prevalence, and outcomes of anticancer therapy-induced cardiotoxicity: The CARDIOTOX registry. Eur. Heart J. 2020, 41, 1720–1729. [Google Scholar] [CrossRef]
- Hu, L.; Li, M.; Ding, Y.; Pu, L.; Liu, J.; Xie, J.; Cabanero, M.; Li, J.; Xiang, R.; Xiong, S. Prognostic value of RDW in cancers: A systematic review and meta-analysis. Oncotarget 2016, 8, 16027–16035. [Google Scholar] [CrossRef]
- Takeuchi, H.; Abe, M.; Takumi, Y.; Hashimoto, T.; Miyawaki, M.; Okamoto, T.; Sugio, K. Elevated red cell distribution width to platelet count ratio predicts poor prognosis in patients with breast cancer. Sci. Rep. 2019, 9, 3033. [Google Scholar] [CrossRef]
- Simões, R.; Silva, L.M.; de Oliveira, A.N.; Alves, M.T.; Pestana, R.M.C.; de Souza, I.D.P.; Oliveira, H.H.M.; Soares, C.E.; Sabino, A.D.P.; Gomes, K.B. Identification of clinical and laboratory variables associated with cardiotoxicity events due to doxorubicin in breast cancer patients: A 1-Year Follow-Up Study. Cardiovasc. Toxicol. 2021, 21, 106–114. [Google Scholar] [CrossRef]
- Pareek, N.; Cevallos, J.; Moliner, P.; Shah, M.; Tan, L.L.; Chambers, V.; Baksi, A.J.; Khattar, R.S.; Sharma, R.; Rosen, S.D.; et al. Activity and outcomes of a cardio-oncology service in the United Kingdom-a five-year experience. Eur. J. Heart Fail. 2018, 20, 1721–1731. [Google Scholar] [CrossRef] [PubMed]
- Salgado, R.; Denkert, C.; Demaria, S.; Sirtaine, N.; Klauschen, F.; Pruneri, G.; Wienert, S.; Van den Eynden, G.; Baehner, F.L.; Penault-Llorca, F.; et al. The evaluation of tumor-infiltrating lymphocytes (TILs) in breast cancer: Recommendations by an International TILs Working Group 2014. Ann. Oncol. 2015, 26, 259–271. [Google Scholar] [CrossRef] [PubMed]
- Stanton, S.E.; Disis, M.L. Clinical significance of tumor-infiltrating lymphocytes in breast cancer. J. Immunother. Cancer 2016, 4, 59. [Google Scholar] [CrossRef] [PubMed]
- Denkert, C.; Von Minckwitz, G.; Darb-Esfahani, S.; Lederer, B.; Heppner, B.I.; Weber, K.E.; Budczies, J.; Huober, J.; Klauschen, F.; Furlanetto, J.; et al. Tumour-infiltrating lymphocytes and prognosis in different subtypes of breast cancer: A pooled analysis of 3771 patients treated with neoadjuvant therapy. Lancet Oncol. 2018, 19, 40–50. [Google Scholar] [CrossRef] [PubMed]
- Denkert, C.; Loibl, S.; Noske, A.; Roller, M.; Müller, B.M.; Komor, M.; Budczies, J.; Darb-Esfahani, S.; Kronenwett, R.; Hanusch, C.; et al. Tumor-associated lymphocytes as an independent predictor of response to neoadjuvant chemotherapy in breast cancer. J. Clin. Oncol. 2010, 28, 105–113. [Google Scholar] [CrossRef]
- Lee, H.S.; Jung, E.J.; Kim, J.M.; Kim, J.Y.; Kim, T.H.; Jang, J.Y.; Woo, J.W.; Lee, J.; Park, T.; Jeong, S.-H. The usefulness of red blood cell distribution width and its ratio with platelet count in breast cancer after surgery and adjuvant treatment: A retrospective study. Gland. Surg. 2022, 11, 1864–1873. [Google Scholar] [CrossRef]
- Yao, D.; Wang, Z.; Cai, H.; Li, Y.; Li, B. Relationship between red cell distribution width and prognosis in patients with breast cancer after operation: A retrospective cohort study. Biosci. Rep. 2019, 39, BSR20190740. [Google Scholar] [CrossRef]
- Csendes, J.A.; Muñoz, A.; Burgos, A. Blood count and C-reactive protein evolution in gastric cancer patients with total gastrectomy surgery. ABCD Arq. Bras. Cir. Dig. 2014, 27, 234–236. [Google Scholar] [CrossRef]
- Pudil, R.; Mueller, C.; Čelutkienė, J.; Henriksen, P.A.; Lenihan, D.; Dent, S.; Barac, A.; Stanway, S.; Moslehi, J.; Suter, T.M.; et al. Role of serum biomarkers in cancer patients receiving cardiotoxic cancer therapies: A position statement from the Cardio-Oncology Study Group of the Heart Failure Association and the Cardio-Oncology Council of the European Society of Cardiology. Eur. J. Heart Fail. 2020, 22, 1966–1983. [Google Scholar] [CrossRef]
- Schneeweiss, A.; Chia, S.; Hickish, T.; Harvey, V.; Eniu, A.; Waldron-Lynch, M.; Eng-Wong, J.; Kirk, S.; Cortés, J. Long-term efficacy analysis of the randomised, phase II TRYPHAENA cardiac safety study: Evaluating pertuzumab and trastuzumab plus standard neoadjuvant anthracycline-containing and anthracycline-free chemotherapy regimens in patients with HER2-positive early breast câncer. Eur. J. Cancer 2018, 89, 27–35. [Google Scholar] [CrossRef]
- Santos, M.H.H. Detection of subclinical trastuzumab-induced cardiotoxicity in patients with breast cancer. Arq. Bras. Cardiol. 2013, 101, 2–3. [Google Scholar] [CrossRef] [PubMed]
- Zou, H.; Liu, S.-H.; Yang, R.; Wu, X.-J.; Cao, Y.-P.; Huang, H.-F. Combination of Neutrophil-to-Lymphocyte Ratio and Red Cell Distribution Width with Serum Tumor Markers for the Differential Diagnosis of Breast Cancer and its Association with Pathological Features and Molecular Types. Clin. Breast. Cancer 2022, 22, e526–e535. [Google Scholar] [CrossRef] [PubMed]
- Simões, R.; Silva, L.M.; Cruz, A.L.V.M.; Fraga, V.G.; Sabino, A.D.P.; Gomes, K.B. Troponin as a cardiotoxicity marker in breast cancer patients receiving T anthracycline-based chemotherapy: A narrative review. Biomed. Pharmacother. 2018, 107, 989–996. [Google Scholar] [CrossRef] [PubMed]
- De Iuliis, F.; Salerno, G.; Taglieri, L.; De Biase, L.; Lanza, R.; Cardelli, P.; Scarpa, S. Tumour serum biomarkers evaluation to predict chemotherapy-induced cardiotoxicity in breast cancer patients. Tumour Biol. 2016, 37, 3379–3387. [Google Scholar] [CrossRef]
- Bracun, V.; Aboumsallem, J.P.; van der Meer, P.; de Boer, R.A. Cardiac biomarkers in patients with cancer: Considerations, Clinical Implications, and Future Avenues. Curr. Oncol. Rep. 2020, 22, 67–78. [Google Scholar] [CrossRef]
| Variable | Patients (n = 80) |
|---|---|
| Mean age | 50.3 ± 12.7 years |
| Histological diagnosis—n (%) | |
| Invasive ductal carcinoma | 72 (90%) |
| Invasive lobular carcinoma | 6 (7%) |
| Special types | 2 (8%) |
| Molecular diagnosis—n (%) | |
| Luminal | 25 (32%) |
| HER2 | 34 (43%) |
| Triple-negative | 20 (25%) |
| ER—n (%) | |
| Positive | 39 (49%) |
| Negative | 40 (51%) |
| PR—n (%) | |
| Positive | 28 (35%) |
| Negative | 51 (65%) |
| Dose DOXO | 379 ± 62 mg/m2 |
| Trastuzumab deruxtecan—n (%) | |
| Yes | 33 (41%) |
| No | 47 (59%) |
| RT Post-CT—n (%) | |
| Yes | 53 (66%) |
| No | 27 (34%) |
| Death—n (%) | |
| Yes | 4 (5%) |
| No | 76 (95%) |
| Cardiotoxicity—n (%) | |
| Yes | 54 (68%) |
| No | 26 (32%) |
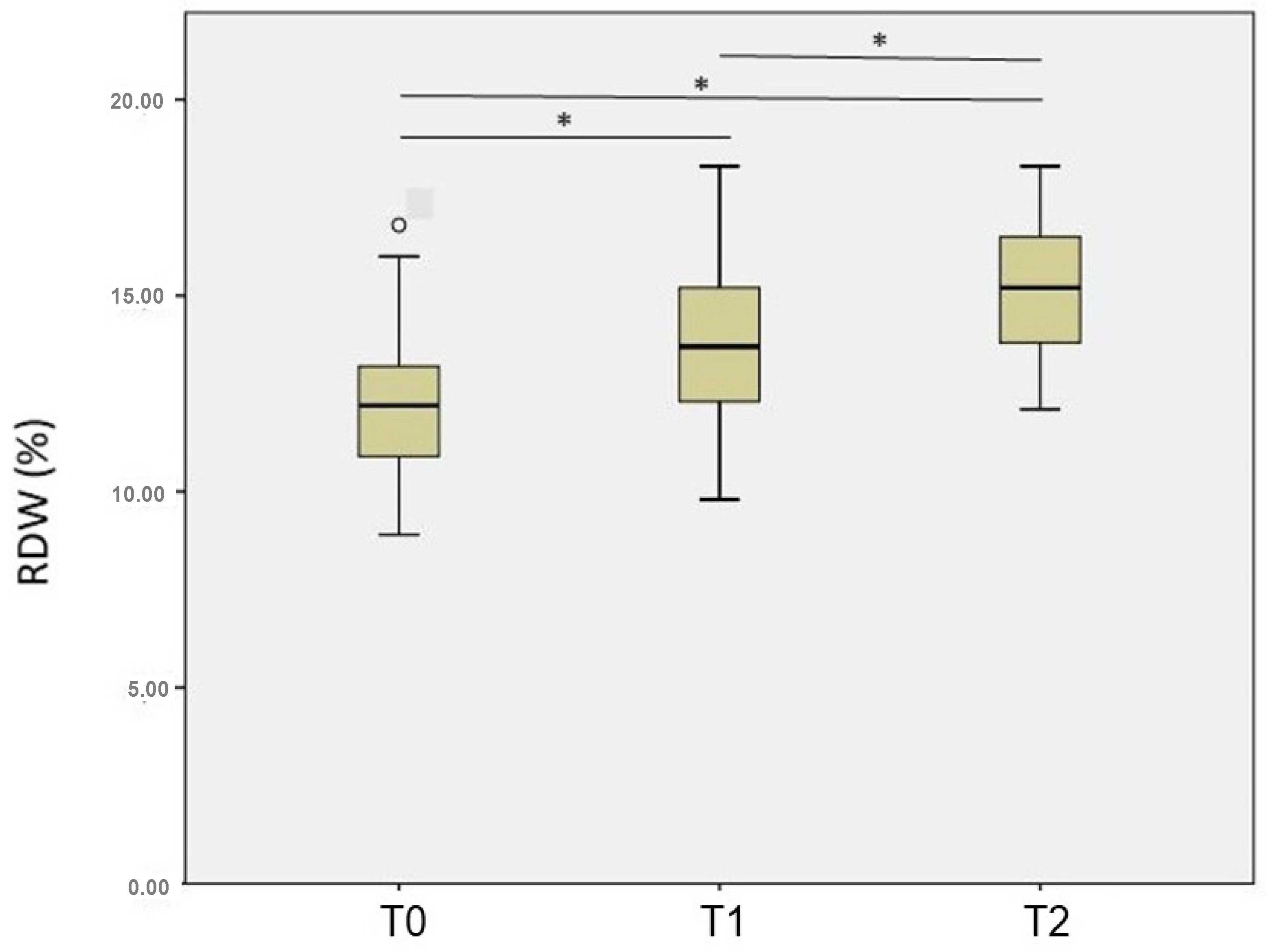
| RDW | |||
|---|---|---|---|
| T0 | T1 | T2 | |
| Molecular diagnosis | |||
| Luminal | 12.0 (11.0—12.8) | 14.5 (12.4—16.7) | 14.6 (13.6—16.7) |
| HER2 | 12.4 (11.1—14.1) | 13.4 (12.3—14.1) | 14.8 (13.8—16.1) |
| Triple-negative | 11.0 (9.8—12.3) | 13.9 (12.4—15.9) | 15.5 (12.4—16.1) |
| p-Value K | 0.126 | 0.176 | 0.708 |
| Trastuzumab use | |||
| Yes | 12.4 (11.1—13.9) | 13.2 (12.3—14.1) | 14.8 (14.1—16.4) |
| No | 11.8 (10.7—12.8) | 14.1 (12.4—15.9) | 14.6 (13.4—16.6) |
| p-Value M | 0.167 | 0.058 | 0.688 |
| Cardiotoxicity | |||
|---|---|---|---|
| Yes (n = 54) | No (n = 26) | p-Value M | |
| Initial Time (T0) | |||
| RDW index | 12.0 (10.8—12.8) | 12.7 (10.9—14.2) | 0.178 |
| CRP | 10.2 (5.0—22.5) | 10.4 (5.7—15.6) | 0.699 |
| cTnI | 0.012 (0.012—0.012) | 0.012 (0.012—0.012) | 0.557 |
| NT-proBNP | 52.4 (34.8—85.3) | 63.3 (49.0—86.7) | 0.223 |
| Per CT (T1) | |||
| RDW | 13.2 (12.3—14.6) | 14.3 (13.2—15.3) | 0.129 |
| CRP | 9.7 (5.0—17.9) | 7.2 (5.0—12.9) | 0.491 |
| cTnI | 0.017 (0.012—0.028) | 0.012 (0.012—0.013) | 0.002 * |
| NT-proBNP | 77.2 (45.1—162.0) | 42.1 (32.8—53.5) | 0.001 * |
| One year Post-CT (T2) | |||
| RDW | 15.2 (13.6—16.5) | 14.2 (13.5—15.7) | 0.197 |
| CRP | 6.4 (5.0—12.5) | 8.2 (6.0—10.1) | 0.288 |
| cTnI | 0.012 (0.012—0.018) | 0.012 (0.012—0.012) | 0.308 |
| NT-proBNP | 80.3 (38.0—147.0) | 48.7 (32.8—66.3) | 0.011 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Simões, R.; Ferreira, A.C.; Silva, L.M.; Sabino, A.d.P.; Carvalho, M.d.G.; Gomes, K.B. Evaluation of the RDW Index (Red Cell Distribution Width) in Women with Breast Cancer Treated with Doxorubicin in a One-Year Follow-Up Study. Diagnostics 2023, 13, 1552. https://doi.org/10.3390/diagnostics13091552
Simões R, Ferreira AC, Silva LM, Sabino AdP, Carvalho MdG, Gomes KB. Evaluation of the RDW Index (Red Cell Distribution Width) in Women with Breast Cancer Treated with Doxorubicin in a One-Year Follow-Up Study. Diagnostics. 2023; 13(9):1552. https://doi.org/10.3390/diagnostics13091552
Chicago/Turabian StyleSimões, Ricardo, Amanda Cambraia Ferreira, Luciana Maria Silva, Adriano de Paula Sabino, Maria das Graças Carvalho, and Karina Braga Gomes. 2023. "Evaluation of the RDW Index (Red Cell Distribution Width) in Women with Breast Cancer Treated with Doxorubicin in a One-Year Follow-Up Study" Diagnostics 13, no. 9: 1552. https://doi.org/10.3390/diagnostics13091552
APA StyleSimões, R., Ferreira, A. C., Silva, L. M., Sabino, A. d. P., Carvalho, M. d. G., & Gomes, K. B. (2023). Evaluation of the RDW Index (Red Cell Distribution Width) in Women with Breast Cancer Treated with Doxorubicin in a One-Year Follow-Up Study. Diagnostics, 13(9), 1552. https://doi.org/10.3390/diagnostics13091552






