Our Cases and Literature Review for Presence of Bladder Hernias in the Inguinal Region in Children
Abstract
1. Introduction
2. Materials and Methods
3. Results
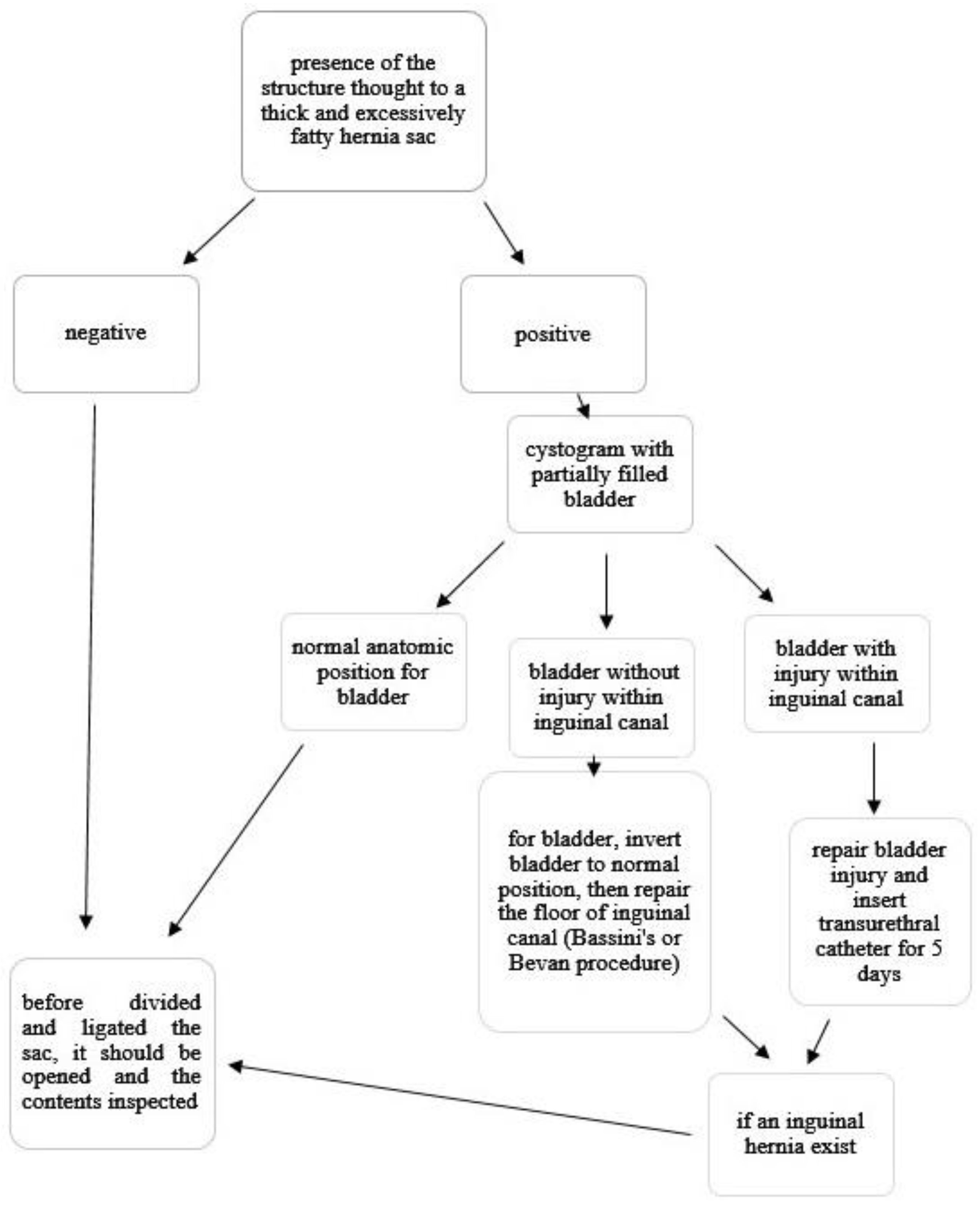
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lao, O.B.; Fitzgibbons, R.J., Jr.; Cusick, R.A. Pediatric inguinal hernias, hydroceles, and undescended testicles. Surg. Clin. N. Am. 2012, 92, 487–504. [Google Scholar] [CrossRef] [PubMed]
- Brooks, G.; Bisoffi, S.; Virgone, C.; Gamba, P. Inguinal Hernia Containing the Uterus in the Pediatric Patient: A Systematic Review. J. Pediatr. Adolesc. Gynecol. 2021, 26, 182–187. [Google Scholar] [CrossRef] [PubMed]
- Branchu, B.; Renard, Y.; Larre, S.; Leon, P. Diagnosis and treatment of inguinal hernia of the bladder: A systematic review of the past 10 years. Turk. J. Urol. 2018, 44, 384–388. [Google Scholar] [CrossRef] [PubMed]
- Ein, S.H.; Njere, I.; Ein, A. Six thousand three hundred sixty-one pediatric inguinal hernias: A 35-year review. J. Pediatr. Surg. 2006, 41, 980–986. [Google Scholar] [CrossRef]
- Foladi, N.; Farzam, F.; Tahir Aien, M. Massive inguino-scrotal herniation of urinary bladder in an infant (scrotal cystocele)-case report. Radiol. Case Rep. 2020, 15, 607–609. [Google Scholar] [CrossRef]
- Duess, J.W.; Schaller, M.C.; Lacher, M.; Sorge, I.; Puri, P.; Gosemann, J.H. Accidental bladder injury during elective inguinal hernia repair: A preventable complication with high morbidity. Pediatr. Surg. Int. 2020, 36, 235–239. [Google Scholar] [CrossRef]
- Allen, R.P.; Condon, V.R. Transitory extraperitoneal hernia of the bladder in infants (bladder ears). Radiology 1961, 77, 979–983. [Google Scholar] [CrossRef]
- Moe, D.C.; Parisi, M.T. Inguinal bladder herniation: An unexpected finding on Tc-99m MAG-3 renogram. Clin. Nucl. Med. 2008, 33, 150–152. [Google Scholar] [CrossRef]
- Bhullar, J.S.; Martin, M.; Dahman, B. Direct inguinal hernia containing a prolapsed bladder in an infant. Ann. Pediatr. Surg. 2013, 9, 157–158. [Google Scholar] [CrossRef]
- Okoro, I.; Anele, A. Scrotal cystocele in a 2-year-old Nigerian child. J. Pediatr. Surg. 2009, 44, e19–e20. [Google Scholar] [CrossRef]
- Kuyama, H.; Nii, A.; Takehara, H. A rare case of inguinal bladder hernia in a child. Asian J. Endosc. Surg. 2010, 3, 87–89. [Google Scholar] [CrossRef]
- Tiryaki, T.; Baskin, D.; Bulut, M. Operative complications of hernia repair in childhood. Pediatr. Surg. Int. 1998, 13, 160–161. [Google Scholar] [CrossRef]
- Aloi, I.P.; Lais, A.; Caione, P. Bladder injuries following inguinal canal surgery in infants. Pediatr. Surg. Int. 2010, 26, 1207–1210. [Google Scholar] [CrossRef]
- Shaw, A.; Santulli, T.V. Management of sliding hernias of the urinary bladder in infants. Surg. Gynecol. Obstetr. 1967, 124, 1314–1316. [Google Scholar]
- Miyano, G.; Yamataka, A.; Okada, Y.; Shimotakahara, A.; Kaneko, K.; Lane, G.J.; Yamashiro, Y.; Miyano, T. Sigmoidocolocystoplasty for augmentation of iatrogenic small capacity bladder caused by direct injury to the bladder during inguinal hernia repair: Long-term follow-up. Pediatr. Surg. Int. 2004, 20, 61–64. [Google Scholar] [CrossRef]
- Ko, P.J.; Lin, H.Y.; Lin, W.H.; Lai, H.S. Sliding inguinal hernia with incarceration of urinary bladder diverticulum in a child. Int. Surg. 2010, 95, 335–337. [Google Scholar]
- Zajaczkowski, T. Scrotal bladder hernia: Report of two cases. Int. Urol. Nephrol. 2007, 39, 479–484. [Google Scholar] [CrossRef]
- Chung, H.M.; Yu, T.J. Bladder rupture after inguinal herniotomy. Pediatr. Surg. Int. 1999, 15, 584–585. [Google Scholar] [CrossRef]
- Dann, A.; Shekherdimian, S. Potential pitfalls of laparoscopic inguinal hernia repair in children: Case report of an unrecognized sliding hernia and review of other rare complications. J. Pediatr. Surg. Case Rep. 2017, 18, 27–29. [Google Scholar] [CrossRef]
- Koot, V.C.; de Jong, J.R.; van der Zee, D.C.; Dik, P. Subtotal cystectomy as a complication of infant hernia repair. Eur. J. Surg. 1998, 164, 873–874. [Google Scholar] [CrossRef]
- Tröbs, R.B.; Yilmaz, B.; Roll, C.; Alrefai, M. Direct bladder hernia after indirect hernia repair in extremely low birth weight babies: Two case reports and a review of the literature. J. Med. Case Rep. 2017, 11, 15. [Google Scholar] [CrossRef] [PubMed]
- Colodny, A.H. Bladder injury during herniorrhaphy. Manifested by ascites and azotemia. Urology 1974, 3, 89–90. [Google Scholar] [CrossRef] [PubMed]
- Bakal, U.; Sarac, M.; Tartar, T.; Ersoz, F.; Kazez, A. Bladder perforations in children. Niger. J. Clin. Pract. 2015, 18, 483–488. [Google Scholar] [CrossRef]
- Wright, N. Baby’s bladder removed by mistake. J. Perioper. Pract. 2010, 20, 194. [Google Scholar] [PubMed]
- Redman, J.F.; Jacks, D.W.; O’Donnell, P.D. Cystectomy: A catastrophic complication of herniorrhaphy. J. Urol. 1985, 133, 97–98. [Google Scholar] [CrossRef]
- Oruç, M.T.; Akbulut, Z.; Ozozan, O.; Coşkun, F. Urological findings in inguinal hernias: A case report and review of the literature. Hernia 2004, 8, 76–79. [Google Scholar]
- Harper, R.G.; Garcia, A.; Sia, C. Inguinal hernia: A common problem of premature infants weighing 1000 g or less at birth. Pediatrics 1975, 56, 112–115. [Google Scholar] [CrossRef]
- Imamoglu, M.; Cay, A.; Sarihan, H.; Ahmetoglu, A.; Ozdemir, O. Paravesical abscess as an unusual late complication of inguinal hernia repair in children. J. Urol. 2004, 171, 1268–1270. [Google Scholar] [CrossRef]
- Wolfson, P.J. Inguinal hernia. In Surgical Directives: Pediatric Surgery, 1st ed.; Mattei, P., Ed.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2002; pp. 521–525. [Google Scholar]
- Gunduz, Y.; Tatli, L.A.; Asil, K.; Aksoy, Y.E. A Rare Cause of Inguinal Herniation: Bladder Herniation Two Cases Report. J. Med. Cases 2013, 4, 588–590. [Google Scholar] [CrossRef]
- Grosfeld, J.L.; Minnick, K.; Shedd, F.; West, K.W.; Rescorla, F.J.; Vane, D.W. Inguinal hernia in children: Factors affecting recurrence in 62 cases. J. Pediatr. Surg. 1991, 26, 283–287. [Google Scholar] [CrossRef]

| Age (Months) | Sex | Side | Surgery Type | Symptoms | Diagnosis | Other Information | Authors | |
|---|---|---|---|---|---|---|---|---|
| 1 | 12 | M | L | NA | Englarged scrotum | Intravenous urography for kidney evaluation | Scrotal cystocele | Foladi et al. [5] |
| 2 | 1 | NA | L | NA | Incidentally | Technetium-99m MAG-3 for evaluation of in utero hydronephrosis | Premature (24 weeks) | Moe et al. [8] |
| 3 | 6 | M | L | E | Bilateral reducible inguinal hernia | Voiding cystourethrogram | Premature (24 weeks), Bassini repair for left-sided hernia | Bhullar et al. [9] |
| 4 | 24 | M | R | E | Inguinoscrotal swelling | Intraoperative | Bassini repair | Okoro et al. [10] |
| 5 | 36 | M | R | E | Incarceration | Intraoperative | Bassini repair | Kuyuma et al. [11] |
| 6 | NA | M | NA | NA | Intraoperative | Bladder repair and cystostomy | Tiryaki et al. [12] | |
| 7 | 4 | M | NA | E | Intraoperative | Repair of bladder perforation and insertion of bladder catheter for 5 days | Aloi et al. [13] | |
| 8 | 3 | M | B | E | Intraoperative | Shaw et al. [14] | ||
| 9 | 12 | M | R | E | Intraoperative | Repair of bladder perforation and insertion of bladder catheter for 5 days | Our patient | |
| 10 | 9 | M | R | E | Intraoperative | Repair of bladder perforation and insertion of bladder catheter for 5 days | Our patient | |
| 11 | 9 | M | NA | E | Wound infection and seeping from the wound | Postoperative | Shaw et al. [14] | |
| 12 | 3 | M | B | E | Seeping from the right inguinal wound incision | Postoperative | Second bladder repair was performed at the age of 6 months. Sigmoidocoloplasty was performed at the age of 10 because of a small and contracted bladder. | Miyano et al. [15] |
| 13 | 24 | M | R | U | Peritonitis and ascites | Postoperative | Bladder repair | Ko et al. [16] |
| 14 | 84 | M | R | E | Seeping from the wound incision | Postoperative | Bladder repair and insertion of bladder catheter | Zajaczkowski [17] |
| 15 | 18 | M | R | E | Anuric with progressive abdominal distention | Postoperative | Laparotomy, closure of bladder almost completely resected with only base remaining | Chung et al. [18] |
| 16 | 5 | M | B | E | Postoperative elective cystourethrogram revealed bladder herniating into the right side day 2. | Premature (24 weeks), second operation Bassini repair | Dann et al. [19] | |
| 17 | 3 | F | L | E | Abdominal distension, left groin bulge, oliguric | Postoperative ultrasound showed a large amount of intra-abdominal free fluid. | Premature, laparotomy, closure of bladder almost completely resected with only base remaining | Koot et al. [20] |
| 18 | 4 | M | R | E | Recurrent bulging at right scar after bilateral scrotal hernia repair | Postoperative | Premature (25 weeks), widened deep inguinal ring closure snugly (Bassini’s procedure?) at the age of 11 m | Tröbs et al. [21] |
| 19 | 3 | M | R | E | Recurrent bulging at right scar after bilateral scrotal hernia repair | Postoperative | Premature (26 weeks), widened deep inguinal ring closure snugly (Bassini’s procedure?) at the age of 5 m | Tröbs et al. [21] |
| 20 | 3 | M | L | U | Abdominal distension, vomiting | Postoperative cystogram demonstrated extravasation. | Bladder repair and cystostomy | Colodny [22]. |
| 21 | 18 | M | R | E | Abdominal distension, anuria | Postoperative ultrasound showed intra-abdominal free fluid. Cystogram demonstrated extravasation and small capacity. | Bladder repair and cystostomy | Bakal et al. [23] |
| 22 | 3 | F | L | E | Abdominal distension | Postoperative | Laparotomy, closure of bladder almost completely resected with only base remaining | Wright [24] |
| 23 | NA | M | NA | NA | Seeping from inguinal wound incision | Postoperative | Suprapubic drainage and antibiotic treatment | Tiryaki et al. [12] |
| 24 | NA | M | NA | NA | Seeping from inguinal wound incision | Postoperative | Suprapubic drainage and antibiotic treatment | Tiryaki et al. [12] |
| 25 | 6 | M | NA | E | Peritonitis | Postoperative | Bladder repair | Aloi et al. [13] |
| 26 | 3 | M | NA | E | Retracted bladder with reflux and febrile urinary tract infection | Postoperative | Bladder augmentation and bilateral ureteral reimplantation | Aloi et al. [13] |
| 27 | 1 | M | R | E | Abdominal distention, seeping from the wound | Postoperative cystogram demonstrated extravasation. | Laparotomy, closure of bladder almost completely resected with only base remaining | Redman et al. [25] |
| 28 | 1 | M | B | E | Anuric | Postoperative cystogram demonstrated extravasation. | Bladder had been resected with both ureters. Bilateral ureteroileocecoplasty was performed. | Redman et al. [25] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kapisiz, A.; Karabulut, R.; Kaya, C.; Eryilmaz, S.; Turkyilmaz, Z.; Atan, A.; Sonmez, K. Our Cases and Literature Review for Presence of Bladder Hernias in the Inguinal Region in Children. Diagnostics 2023, 13, 1533. https://doi.org/10.3390/diagnostics13091533
Kapisiz A, Karabulut R, Kaya C, Eryilmaz S, Turkyilmaz Z, Atan A, Sonmez K. Our Cases and Literature Review for Presence of Bladder Hernias in the Inguinal Region in Children. Diagnostics. 2023; 13(9):1533. https://doi.org/10.3390/diagnostics13091533
Chicago/Turabian StyleKapisiz, Alparslan, Ramazan Karabulut, Cem Kaya, Sibel Eryilmaz, Zafer Turkyilmaz, Ali Atan, and Kaan Sonmez. 2023. "Our Cases and Literature Review for Presence of Bladder Hernias in the Inguinal Region in Children" Diagnostics 13, no. 9: 1533. https://doi.org/10.3390/diagnostics13091533
APA StyleKapisiz, A., Karabulut, R., Kaya, C., Eryilmaz, S., Turkyilmaz, Z., Atan, A., & Sonmez, K. (2023). Our Cases and Literature Review for Presence of Bladder Hernias in the Inguinal Region in Children. Diagnostics, 13(9), 1533. https://doi.org/10.3390/diagnostics13091533






