Acute Respiratory Distress Syndrome; A Review of Recent Updates and a Glance into the Future
Abstract
1. Introduction
- (1)
- Timing: “Within one week of a known clinical insult or new or worsening respiratory symptoms”
- (2)
- Chest Imaging (X-ray or Computed Tomography): “Bilateral opacities—not fully explained by effusions, lobar/lung collapse, or nodules”.
- (3)
- Origin of Edema: “Respiratory failure not fully explained by cardiac failure or fluid overload” with “objective assessment (e.g., echocardiography) to exclude hydrostatic edema if no risk factor present”.
- (4)
- Oxygenation:
- Mild: 200 mm Hg < PaO2/FIO2 ≤ 300 mm Hg with PEEP or CPAP ≥ 5 cm H2O
- Moderate: 100 mm Hg < PaO2/FIO2 ≤ 200 mm Hg with PEEP ≥ 5 cm H2O
- Severe: PaO2/FIO2 ≤ 100 mm Hg with PEEP ≥ 5 cm H2O
2. Pathophysiology
3. Current Management Strategies
4. Pharmacotherapy in ARDS; Recent Trials
4.1. Beta Agonists
4.2. Sivelestat
4.3. Simvastatin
4.4. Vitamin D
5. Mesenchymal Stromal Cells
6. Gut–Lung Interaction in ARDS
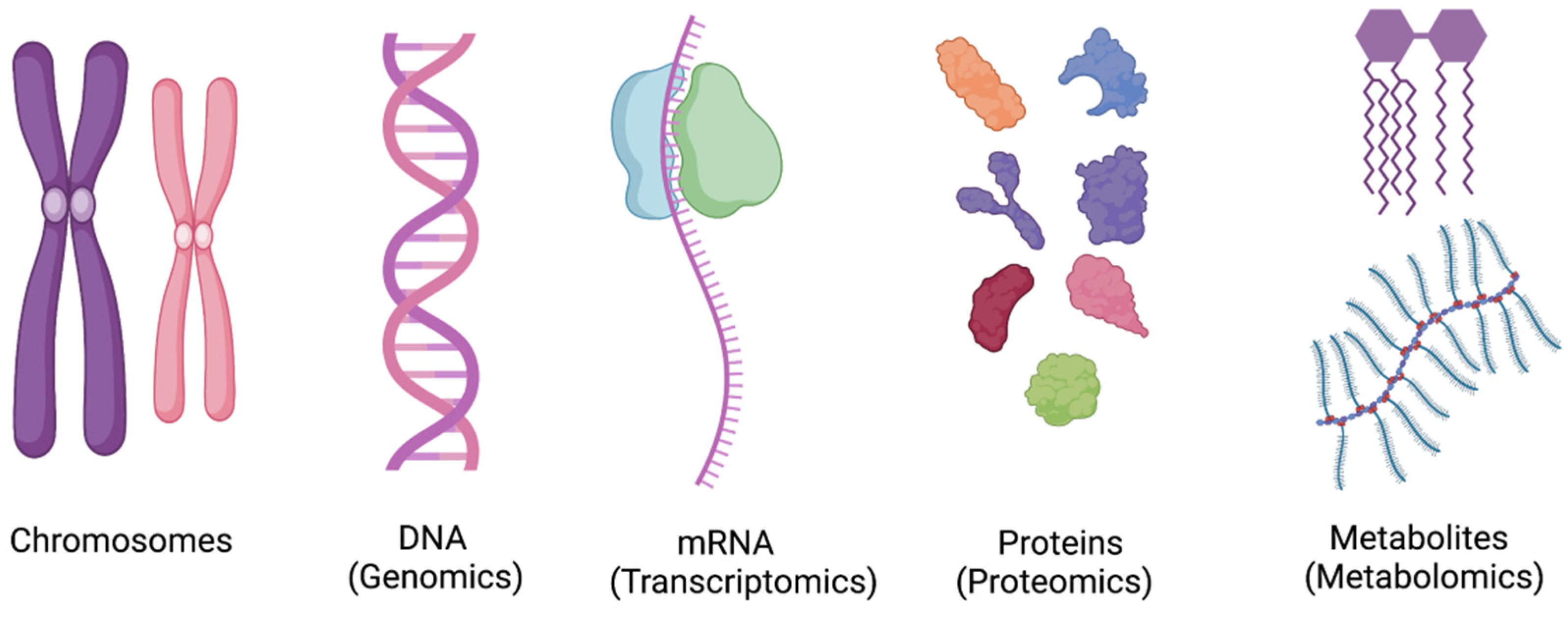
7. Metabolomics and Future Directions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Barry, J.M. The site of origin of the 1918 influenza pandemic and its public health implications. J. Transl. Med. 2004, 2, 3. [Google Scholar] [CrossRef] [PubMed]
- Oxford, J.S. The so-called Great Spanish Influenza Pandemic of 1918 may have originated in France in 1916. Philos. Trans. R. Soc. B Biol. Sci. 2001, 356, 1857–1859. [Google Scholar] [CrossRef] [PubMed]
- Rezoagli, E.; Fumagalli, R.; Bellani, G. Definition and epidemiology of acute respiratory distress syndrome. Ann. Transl. Med. 2017, 5, 282. [Google Scholar] [CrossRef] [PubMed]
- Diamond, M.; Peniston, H.L.; Sanghavi, D.; Mahapatra, S. Acute Respiratory Distress Syndrome; StatPearls Publishing: Tampa, FL, USA, 2022. [Google Scholar]
- Ashbaugh, D.; Bigelow, D.B.; Petty, T.; Levine, B.; Ashbaugh, D.; Bigelow, D.B.; Petty, T.; Levine, B. Acute Respiratory Distress in Adults. Lancet 1967, 2, 319–323. [Google Scholar] [CrossRef]
- ARDS Definition of Task Force; Ranieri, V.M.; Rubenfeld, G.D.; Thompson, B.T.; Ferguson, N.D.; Caldwell, E.; Fan, E.; Camporota, L.; Slutsky, A.S. Acute Respiratory Distress Syndrome: The Berlin Definition. JAMA 2010, 307, 2526–2533. [Google Scholar] [CrossRef]
- Bernard, G.R.; Artigas, A.; Brigham, K.L.; Carlet, J.; Falke, K.; Hudson, L.; Lamy, M.; Legall, J.R.; Morris, A.; Spragg, R. The American-European Consensus Conference on ARDS. Definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am. J. Respir. Crit. Care Med. 1994, 149 Pt 1, 818–824. [Google Scholar] [CrossRef]
- Bellani, G.; Laffey, J.G.; Pham, T.; Fan, E.; Brochard, L.; Esteban, A.; Gattinoni, L.; Van Haren, F.; Larsson, A.; McAuley, D.F.; et al. Epidemiology, Patterns of Care, and Mortality for Patients with Acute Respiratory Distress Syndrome in Intensive Care Units in 50 Countries. JAMA 2016, 315, 788–800. [Google Scholar] [CrossRef]
- Fan, E.; Beitler, J.R.; Brochard, L.; Calfee, C.S.; Ferguson, N.D.; Slutsky, A.S.; Brodie, D. COVID-19-associated acute respiratory distress syndrome: Is a different approach to management warranted? Lancet Respir. Med. 2020, 8, 816–821. [Google Scholar] [CrossRef] [PubMed]
- Kurihara, C.; Manerikar, A.; Querrey, M.; Felicelli, C.; Yeldandi, A.; Garza-Castillon, R.; Lung, K.; Kim, S.; Ho, B.; Tomic, R.; et al. Clinical Characteristics and Outcomes of Patients with COVID-19–Associated Acute Respiratory Distress Syndrome Who Underwent Lung Transplant. JAMA 2022, 327, 652–661. [Google Scholar] [CrossRef]
- Ramji, H.F.; Anderson, C.; Greer, K.; Baker, M.Z.; Brown, B.R. Management of the Hospitalized Patient with COVID Part Two. J. Okla. State Med. Assoc. 2023, 116, 34–43. Available online: https://www.bluetoad.com/publication/?i=783834 (accessed on 10 March 2023).
- Douin, D.J.; Ward, M.J.M.; Lindsell, C.J.; Howell, M.P.B.; Hough, C.L.M.; Exline, M.C.; Gong, M.N.; Aboodi, M.S.; Tenforde, M.W.M.; Feldstein, L.R.; et al. ICU Bed Utilization during the Coronavirus Disease 2019 Pandemic in a Multistate Analysis—March to June 2020. Crit. Care Explor. 2021, 3, e0361. [Google Scholar] [CrossRef] [PubMed]
- Tsai, T.C.; Jacobson, B.H.; Orav, E.J.; Jha, A.K. Association of community-level social vulnerability with US acute care hospital intensive care unit capacity during COVID-19. Healthcare 2022, 10, 100611. [Google Scholar] [CrossRef] [PubMed]
- Gattinoni, L.; Chiumello, D.; Rossi, S. COVID-19 pneumonia: ARDS or not? Crit. Care 2020, 24, 154. [Google Scholar] [CrossRef]
- Bos, L.D.J.; Ware, L.B. Acute respiratory distress syndrome: Causes, pathophysiology, and phenotypes. Lancet 2022, 400, 1145–1156. [Google Scholar] [CrossRef] [PubMed]
- Huppert, L.A.; Matthay, M.A.; Ware, L.B. Pathogenesis of Acute Respiratory Distress Syndrome. Semin. Respir. Crit. Care Med. 2019, 40, 31–39. [Google Scholar] [CrossRef] [PubMed]
- Kaku, S.; Nguyen, C.D.; Htet, N.N.; Tutera, D.; Barr, J.; Paintal, H.S.; Kuschner, W.G. Acute Respiratory Distress Syndrome: Etiology, Pathogenesis, and Summary on Management. J. Intensiv. Care Med. 2020, 35, 723–737. [Google Scholar] [CrossRef]
- Saguil, A.; Fargo, M.V. Acute Respiratory Distress Syndrome: Diagnosis and Management. Am. Fam. Physician 2020, 101, 730–738. [Google Scholar]
- Walkey, A.J.; Summer, R.; Ho, V.; Alkana, P. Acute respiratory distress syndrome: Epidemiology and management approaches. Clin. Epidemiol. 2012, 4, 159–169. [Google Scholar] [CrossRef]
- Swenson, K.E.; Swenson, E.R. Pathophysiology of Acute Respiratory Distress Syndrome and COVID-19 Lung Injury. Crit. Care Clin. 2021, 37, 749–776. [Google Scholar] [CrossRef]
- Matthay, M.A.; Zemans, R.L. The Acute Respiratory Distress Syndrome: Pathogenesis and Treatment. Annu. Rev. Pathol. Mech. Dis. 2011, 6, 147–163. [Google Scholar] [CrossRef]
- Matthay, M.A.; Zemans, R.L.; Zimmerman, G.A.; Arabi, Y.M.; Beitler, J.R.; Mercat, A.; Herridge, M.; Randolph, A.G.; Calfee, C.S. Acute respiratory distress syndrome. Nat. Rev. Dis. Prim. 2019, 5, 18. [Google Scholar] [CrossRef] [PubMed]
- Calfee, C.S.; Delucchi, K.; Parsons, P.E.; Thompson, B.T.; Ware, L.B.; Matthay, M.A. Subphenotypes in acute respiratory distress syndrome: Latent class analysis of data from two randomized controlled trials. Lancet Respir. Med. 2014, 2, 611–620. [Google Scholar] [CrossRef]
- Reilly, J.P.; Calfee, C.S.; Christie, J.D. Acute Respiratory Distress Syndrome Phenotypes. Semin. Respir. Crit. Care Med. 2019, 40, 19–30. [Google Scholar] [CrossRef] [PubMed]
- Feng, J.; Pang, J.; He, D.; Wu, Z.; Li, Q.; Ji, P.; He, C.; Zhong, Z.; Li, H.; Zhang, J. Identification of Genes with Altered Methylation and Its Role in Early Diagnosis of Sepsis-Induced Acute Respiratory Distress Syndrome. Int. J. Gen. Med. 2021, 14, 243–253. [Google Scholar] [CrossRef]
- Szilágyi, K.L.; Liu, C.; Zhang, X.; Wang, T.; Fortman, J.D.; Zhang, W.; Garcia, J.G. Epigenetic contribution of the myosin light chain kinase gene to the risk for acute respiratory distress syndrome. Transl. Res. 2017, 180, 12–21. [Google Scholar] [CrossRef] [PubMed]
- Radermacher, P.; Maggiore, S.M.; Mercat, A. Fifty Years of Research in ARDS.Gas Exchange in Acute Respiratory Distress Syndrome. Am. J. Respir. Crit. Care Med. 2017, 196, 964–984. [Google Scholar] [CrossRef]
- Fan, E.; Brodie, D.; Slutsky, A.S. Acute Respiratory Distress Syndrome: Advances in diagnosis and treatment. JAMA 2018, 319, 698–710. [Google Scholar] [CrossRef]
- Fan, E.; Needham, D.M.; Stewart, T.E. Ventilatory Management of Acute Lung Injury and Acute Respiratory Distress Syndrome. JAMA 2005, 294, 2889–2896. [Google Scholar] [CrossRef]
- Acute Respiratory Distress Syndrome Network; Brower, R.G.; Matthay, M.A.; Morris, A.; Schoenfeld, D.; Thompson, B.T.; Wheeler, A. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N. Engl. J. Med. 2000, 342, 1301–1308. [Google Scholar] [CrossRef]
- Briel, M.; Meade, M.; Mercat, A.; Brower, R.G.; Talmor, D.; Walter, S.D.; Slutsky, A.S.; Pullenayegum, E.; Zhou, Q.; Cook, D.; et al. Higher vs. Lower Positive End-Expiratory Pressure in Patients with Acute Lung Injury and Acute Respiratory Distress Syndrome: Systematic review and meta-analysis. JAMA 2010, 303, 865–873. [Google Scholar] [CrossRef]
- Grieco, D.L.; Maggiore, S.M.; Roca, O.; Spinelli, E.; Patel, B.K.; Thille, A.W.; Barbas, C.S.V.; de Acilu, M.G.; Cutuli, S.L.; Bongiovanni, F.; et al. Non-invasive ventilatory support and high-flow nasal oxygen as first-line treatment of acute hypoxemic respiratory failure and ARDS. Intensiv. Care Med. 2021, 47, 851–866. [Google Scholar] [CrossRef] [PubMed]
- Rittayamai, N.; Katsios, C.M.; Beloncle, F.; Friedrich, J.O.; Mancebo, J.; Brochard, L. Pressure-Controlled vs. Volume-Controlled Ventilation in Acute Respiratory Failure. Chest 2015, 148, 340–355. [Google Scholar] [CrossRef] [PubMed]
- González, M.; Arroliga, A.C.; Frutos-Vivar, F.; Raymondos, K.; Esteban, A.; Putensen, C.; Apezteguía, C.; Hurtado, J.; Desmery, P.; Tomicic, V.; et al. Airway pressure release ventilation versus assist-control ventilation: A comparative propensity score and international cohort study. Intensiv. Care Med. 2010, 36, 817–827. [Google Scholar] [CrossRef] [PubMed]
- Meade, M.O.; Young, D.; Hanna, S.; Zhou, Q.; Bachman, T.E.; Bollen, C.; Slutsky, A.S.; Lamb, S.; Adhikari, N.K.J.; Mentzelopoulos, S.D.; et al. Severity of Hypoxemia and Effect of High-Frequency Oscillatory Ventilation in Acute Respiratory Distress Syndrome. Am. J. Respir. Crit. Care Med. 2017, 196, 727–733. [Google Scholar] [CrossRef]
- Cornejo, R.A.; Díaz, J.C.; Tobar, E.A.; Bruhn, A.R.; Ramos, C.A.; González, R.A.; Repetto, C.A.; Romero, C.M.; Gálvez, L.R.; Llanos, O.; et al. Effects of Prone Positioning on Lung Protection in Patients with Acute Respiratory Distress Syndrome. Am. J. Respir. Crit. Care Med. 2013, 188, 440–448. [Google Scholar] [CrossRef] [PubMed]
- Caputo, N.D.; Strayer, R.J.; Levitan, R. Early Self-Proning in Awake, Non-intubated Patients in the Emergency Department: A Single ED’s Experience during the COVID-19 Pandemic. Acad. Emerg. Med. 2020, 27, 375–378. [Google Scholar] [CrossRef] [PubMed]
- Fan, E.; Del Sorbo, L.; Goligher, E.C.; Hodgson, C.L.; Munshi, L.; Walkey, A.J.; Adhikari, N.K.J.; Amato, M.B.P.; Branson, R.; Brower, R.G.; et al. An Official American Thoracic Society/European Society of Intensive Care Medicine/Society of Critical Care Medicine Clinical Practice Guideline: Mechanical Ventilation in Adult Patients with Acute Respiratory Distress Syndrome. Am. J. Respir. Crit. Care Med. 2017, 195, 1253–1263. [Google Scholar] [CrossRef] [PubMed]
- Chaves, R.C.D.F.; Filho, R.R.; Timenetsky, K.T.; Moreira, F.T.; Vilanova, L.C.D.S.; Bravim, B.D.A.; Neto, A.S.; Corrêa, T.D. Extracorporeal membrane oxygenation: A literature review. Rev. Bras. Ter. Intensiv. 2019, 31, 410–424. [Google Scholar] [CrossRef]
- Griffiths, M.J.D.; McAuley, D.F.; Perkins, G.D.; Barrett, N.; Blackwood, B.; Boyle, A.; Chee, N.; Connolly, B.; Dark, P.; Finney, S.; et al. Guidelines on the management of acute respiratory distress syndrome. BMJ Open Respir. Res. 2019, 6, e000420. [Google Scholar] [CrossRef]
- Wei, X.-B.; Wang, Z.-H.; Liao, X.-L.; Guo, W.-X.; Qin, T.-H.; Wang, S.-H. Role of Neuromuscular Blocking Agents in Acute Respiratory Distress Syndrome: An Updated Meta-Analysis of Randomized Controlled Trials. Front. Pharmacol. 2020, 10, 1637. [Google Scholar] [CrossRef]
- Papazian, L.; Forel, J.-M.; Gacouin, A.; Penot-Ragon, C.; Perrin, G.; Loundou, A.; Jaber, S.; Arnal, J.-M.; Perez, D.; Seghboyan, J.-M.; et al. Neuromuscular Blockers in Early Acute Respiratory Distress Syndrome. N. Engl. J. Med. 2010, 363, 1107–1116. [Google Scholar] [CrossRef] [PubMed]
- National Heart, Lung, and Blood Institute PETAL Clinical Trials Network; Moss, M.; Huang, D.T.; Brower, R.G.; Ferguson, N.D.; Ginde, A.A.; Gong, M.N.; Grissom, C.K.; Gundel, S.; Hayden, D.; et al. Early Neuromuscular Blockade in the Acute Respiratory Distress Syndrome. N. Engl. J. Med. 2019, 380, 1997–2008. [Google Scholar] [CrossRef] [PubMed]
- Adhikari, N.K.J.; Burns, K.E.A.; Friedrich, J.; Granton, J.T.; Cook, D.J.; Meade, M.O. Effect of nitric oxide on oxygenation and mortality in acute lung injury: Systematic review and meta-analysis. BMJ 2007, 334, 779. [Google Scholar] [CrossRef] [PubMed]
- Poonam, P.B.H.; Koscik, R.; Nguyen, T.; Rikhi, S.; Lin, H.-M. Nitric oxide versus epoprostenol for refractory hypoxemia in COVID-19. PLoS ONE 2022, 17, e0270646. [Google Scholar] [CrossRef]
- Hussain, S.T.; Jaliawala, H.A.; Zhao, D.; Ijaz, S.H.; Tsui, J.P.; Chasteen, B.R.; Brown, B.R.; Bernardo, R.J.M. Use of Aerosolized Prostacyclins in Critically Ill Patients and Association with Clinical Outcomes. Crit. Care Explor. 2023, 5, e0845. [Google Scholar] [CrossRef]
- Villar, J.; Ferrando, C.; Martínez, D.; Ambrós, A.; Muñoz, T.; Soler, J.A.; Aguilar, G.; Alba, F.; González-Higueras, E.; Conesa, L.A.; et al. Dexamethasone treatment for the acute respiratory distress syndrome: A multicentre, randomised controlled trial. Lancet Respir. Med. 2020, 8, 267–276. [Google Scholar] [CrossRef]
- Chaudhuri, D.; Sasaki, K.; Karkar, A.; Sharif, S.; Lewis, K.; Mammen, M.J.; Alexander, P.; Ye, Z.; Lozano, L.E.C.; Munch, M.W.; et al. Corticosteroids in COVID-19 and non-COVID-19 ARDS: A systematic review and meta-analysis. Intensiv. Care Med. 2021, 47, 521–537. [Google Scholar] [CrossRef]
- Luyt, C.-E.; Bouadma, L.; Morris, A.C.; Dhanani, J.A.; Kollef, M.; Lipman, J.; Martin-Loeches, I.; Nseir, S.; Ranzani, O.T.; Roquilly, A.; et al. Pulmonary infections complicating ARDS. Intensiv. Care Med. 2020, 46, 2168–2183. [Google Scholar] [CrossRef]
- Chien, J.-Y.; Hsueh, P.-R.; Yu, C.-J.; Yang, P.-C. The evolution of drug-resistant microorganisms in patients with prolonged me-chanical ventilation. Am. J. Infect. Control 2009, 37, 231–236. [Google Scholar] [CrossRef]
- Parker, C.M.; Kutsogiannis, J.; Muscedere, J.; Cook, D.; Dodek, P.; Day, A.G.; Heyland, D.K.; Canadian Critical Care Trials Group. Ventilator-associated pneumonia caused by multidrug-resistant organisms or Pseudomonas aeruginosa: Prevalence, incidence, risk factors, and outcomes. J. Crit. Care 2008, 23, 18–26. [Google Scholar] [CrossRef]
- Matthay, M.A.; Folkesson, H.G.; Clerici, C. Lung Epithelial Fluid Transport and the Resolution of Pulmonary Edema. Physiol. Rev. 2002, 82, 569–600. [Google Scholar] [CrossRef] [PubMed]
- Spindler, V.; Waschke, J. Beta-Adrenergic Stimulation Contributes to Maintenance of Endothelial Barrier Functions Under Baseline Conditions. Microcirculation 2011, 18, 118–127. [Google Scholar] [CrossRef] [PubMed]
- Morty, R.E.; Eickelberg, O.; Seeger, W. Alveolar fluid clearance in acute lung injury: What have we learned from animal models and clinical studies? Intensive Care Med. 2007, 33, 1229–1240. [Google Scholar] [CrossRef] [PubMed]
- Mutlu, G.M.; Factor, P. Alveolar epithelial β2-adrenergic receptors. Am. J. Respir. Cell Mol. Biol. 2008, 38, 127–134. [Google Scholar] [CrossRef]
- Manocha, S.; Gordon, A.C.; Salehifar, E.; Groshaus, H.; Walley, K.R.; Russell, J.A. Inhaled beta-2 agonist salbutamol and acute lung injury: An association with improvement in acute lung injury. Crit. Care 2006, 10, R12. [Google Scholar] [CrossRef]
- Di Marco, F.; Guazzi, M.; Sferrazza Papa, G.F.; Vicenzi, M.; Santus, P.; Busatto, P.; Piffer, F.; Blasi, F.; Centanni, S. Salmeterol improves fluid clearance from alveolar-capillary membrane in COPD patients: A pilot study. Pulm. Pharmacol. Ther. 2012, 25, 119–123. [Google Scholar] [CrossRef]
- Perkins, G.D.; McAuley, D.F.; Thickett, D.R.; Gao, F. The β-agonist lung injury trial (BALTI): A randomized placebo-controlled clinical trial. Am. J. Respir. Crit. Care Med. 2006, 173, 281–287. [Google Scholar] [CrossRef]
- Gates, S.; Perkins, G.; Lamb, S.; Kelly, C.; Thickett, D.R.; Young, J.; McAuley, D.; Snaith, C.; McCabe, C.; Hulme, C.; et al. Beta-Agonist Lung injury TrIal-2 (BALTI-2): A multicentre, randomised, double-blind, placebo-controlled trial and economic evaluation of intravenous infusion of salbutamol versus placebo in patients with acute respiratory distress syndrome. Health Technol. Assess. 2013, 17, 1–87. [Google Scholar] [CrossRef]
- Festic, E.; Carr, G.E.; Cartin–Ceba, R.; Hinds, R.F.; Banner–Goodspeed, V.; Bansal, V.; Asuni, A.T.; Talmor, D.; Rajagopalan, G.; Frank, R.D.; et al. Randomized Clinical Trial of a Combination of an Inhaled Corticosteroid and Beta Agonist in Patients at Risk of Developing the Acute Respiratory Distress Syndrome. Crit. Care Med. 2017, 45, 798. [Google Scholar] [CrossRef]
- Fouad, M.K.; Mohamed, M.H.; Ammar, M.A.M.; Ahmad, A.A.A.S. The Role of Inhaled Corticosteroids and B2 Agonist in Prevention of ARDS in High-Risk Patients Admitted to ICU. Qjm Int. J. Med. 2020, 113 (Suppl. S1), hcaa039.072. [Google Scholar] [CrossRef]
- Fujishima, S. Pathophysiology and biomarkers of acute respiratory distress syndrome. J. Intensiv. Care 2014, 2, 32. [Google Scholar] [CrossRef]
- Zeiher, B.G.; Matsuoka, S.; Kawabata, K.; Repine, J.E. Neutrophil elastase and acute lung injury: Prospects for sivelestat and other neutrophil elastase inhibitors as therapeutics. Crit. Care Med. 2002, 30, S281–S287. [Google Scholar] [CrossRef] [PubMed]
- Kawabata, K.; Suzuki, M.; Sugitani, M.; Imaki, K.; Toda, M.; Miyamoto, T. ONO-5046, a novel inhibitor of human neutrophil elastase. Biochem. Biophys. Res. Commun. 1991, 177, 814–820. [Google Scholar] [CrossRef]
- Tamakuma, S.; Ogawa, M.; Aikawa, N.; Kubota, T.; Hirasawa, H.; Ishizaka, A.; Taenaka, N.; Hamada, C.; Matsuoka, S.; Abiru, T. Relationship between neutrophil elastase and acute lung injury in humans. Pulm. Pharmacol. Ther. 2004, 17, 271–279. [Google Scholar] [CrossRef] [PubMed]
- Aikawa, N.; Ishizaka, A.; Hirasawa, H.; Shimazaki, S.; Yamamoto, Y.; Sugimoto, H.; Shinozaki, M.; Taenaka, N.; Endo, S.; Ikeda, T.; et al. Reevaluation of the efficacy and safety of the neutrophil elastase inhibitor, Sivelestat, for the treatment of acute lung injury associated with systemic inflammatory response syndrome; a phase IV study. Pulm. Pharmacol. Ther. 2011, 24, 549–554. [Google Scholar] [CrossRef]
- Kido, T.; Muramatsu, K.; Yatera, K.; Asakawa, T.; Otsubo, H.; Kubo, T.; Fujino, Y.; Matsuda, S.; Mayumi, T.; Mukae, H. Efficacy of early sivelestat administration on acute lung injury and acute respiratory distress syndrome published. Respirology 2017, 22, 708–713. [Google Scholar] [CrossRef] [PubMed]
- Zeiher, B.G.; Artigas, A.; Vincent, J.-L.; Dmitrienko, A.; Jackson, K.; Thompson, B.T.; Bernard, G. Neutrophil elastase inhibition in acute lung injury: Results of the STRIVE study. Crit. Care Med. 2004, 32, 1695–1702. [Google Scholar] [CrossRef]
- Miyoshi, S.; Hamada, H.; Ito, R.; Katayama, H.; Irifune, K.; Suwaki, T.; Nakanishi, N.; Kanematsu, T.; Dote, K.; Aibiki, M.; et al. Usefulness of a selective neutrophil elastase inhibitor, sivelestat, in acute lung injury patients with sepsis. Drug Des. Dev. Ther. 2013, 7, 305–316. [Google Scholar] [CrossRef]
- Ozawa, T.; Mihara, K.; Yasuno, N. Predictors of the therapeutic effect of sivelestat in patients with acute lung injury associated with systemic inflammatory response syndrome. J. Pharm. Health Care Sci. 2016, 2, 19. [Google Scholar] [CrossRef]
- Pu, S.; Wang, D.; Liu, D.; Zhao, Y.; Qi, D.; He, J.; Zhou, G. Effect of sivelestat sodium in patients with acute lung injury or acute respiratory distress syndrome: A meta-analysis of randomized controlled trials. BMC Pulm. Med. 2017, 17, 148. [Google Scholar] [CrossRef]
- Jacobson, J.R.; Dudek, S.M.; Birukov, K.G.; Ye, S.Q.; Grigoryev, D.N.; Girgis, R.E.; Garcia, J.G. Cytoskeletal activation and altered gene expression in endothelial barrier regulation by simvastatin. Am. J. Respir. Cell Mol. Biol. 2004, 30, 662–670. [Google Scholar] [CrossRef] [PubMed]
- Jacobson, J.R.; Barnard, J.W.; Grigoryev, D.N.; Ma, S.F.; Tuder, R.M.; Garcia, J.G. Simvastatin attenuates vascular leak and inflammation in murine inflammatory lung injury. Am. J. Physiol. Lung. Cell Mol. Physiol. 2005, 288, L1026–L1032. [Google Scholar] [CrossRef] [PubMed]
- Shyamsundar, M.; McKeown, S.T.W.; O’Kane, C.; Craig, T.R.; Brown, V.; Thickett, D.; Matthay, M.A.; Taggart, C.; Backman, J.T.; Elborn, J.; et al. Simvastatin Decreases Lipopolysaccharide-induced Pulmonary Inflammation in Healthy Volunteers. Am. J. Respir. Crit. Care Med. 2009, 179, 1107–1114. [Google Scholar] [CrossRef]
- McAuley, D.F.; Laffey, J.G.; O’Kane, C.M.; Perkins, G.D.; Mullan, B.; Trinder, T.J.; Johnston, P.; Hopkins, P.A.; Johnston, A.J.; McDowell, C.; et al. Simvastatin in the Acute Respiratory Distress Syndrome. N. Engl. J. Med. 2014, 371, 1695–1703. [Google Scholar] [CrossRef]
- Agus, A.; Hulme, C.; Verghis, R.M.; McDowell, C.; Jackson, C.; O’Kane, C.M.; Laffey, J.G.; McAuley, D.F. Simvastatin for patients with acute respiratory distress syndrome: Long-term outcomes and cost-effectiveness from a ran-domised controlled trial. Crit. Care 2017, 21, 108. [Google Scholar] [CrossRef]
- Calfee, C.S.; Delucchi, K.L.; Sinha, P.; Matthay, M.A.; Hackett, J.; Shankar-Hari, M.; McDowell, C.; Laffey, J.G.; O’Kane, C.M.; McAuley, D.F.; et al. Acute respiratory distress syndrome subphenotypes and differential response to simvastatin: Secondary analysis of a ran-domised controlled trial. Lancet 2018, 6, 691–698. [Google Scholar] [CrossRef]
- Boyle, A.J.; Ferris, P.; Bradbury, I.; Conlon, J.; Shankar-Hari, M.; Rogers, A.J.; O’kane, C.M.; McAuley, D.F. Baseline plasma IL-18 may predict simvastatin treatment response in patients with ARDS: A secondary analysis of the HARP-2 randomised clinical trial. Crit. Care 2022, 26, 68. [Google Scholar] [CrossRef]
- Remmelts, H.H.F.; Van De Garde, E.M.W.; Meijvis, S.C.A.; Peelen, E.L.G.C.A.; Damoiseaux, J.G.M.C.; Grutters, J.C.; Biesma, D.H.; Bos, W.J.W.; Rijkers, G.T. Addition of Vitamin D Status to Prognostic Scores Improves the Prediction of Outcome in Community-Acquired Pneumonia. Clin. Infect. Dis. 2012, 55, 1488–1494. [Google Scholar] [CrossRef]
- Parekh, D.; Thickett, D.; Turner, A. Vitamin D Deficiency and Acute Lung Injury. Inflamm. Allergy-Drug Targets 2013, 12, 253–261. [Google Scholar] [CrossRef]
- Zhang, Y.; Leung, D.Y.M.; Richers, B.N.; Liu, Y.; Remigio, L.K.; Riches, D.W.; Goleva, E. Vitamin D Inhibits Monocyte/Macrophage Proinflammatory Cytokine Production by Targeting MAPK Phosphatase-1. J. Immunol. 2012, 188, 2127–2135. [Google Scholar] [CrossRef]
- Kempker, J.A.; Tangpricha, V.; Ziegler, T.R.; Martin, G.S. Vitamin D in sepsis: From basic science to clinical impact. Crit. Care 2012, 16, 316. [Google Scholar] [CrossRef] [PubMed]
- Brockman-Schneider, R.A.; Pickles, R.J.; Gern, J.E. Effects of vitamin D on airway epithelial cell morphology and rhinovirus replication. PLoS ONE 2014, 9, e86755. [Google Scholar] [CrossRef] [PubMed]
- Quraishi, S.A.; McCarthy, C.; Blum, L.; Cobb, J.P.; Camargo, C.A. Plasma 25-Hydroxyvitamin D Levels at Initiation of Care and Duration of Mechanical Ventilation in Critically Ill Surgical Patients. J. Parenter. Enter. Nutr. 2015, 40, 273–278. [Google Scholar] [CrossRef] [PubMed]
- Brook, K.; Otero, T.M.; Yeh, D.D.; Canales, C.; Belcher, D.; Quraishi, S.A. Admission 25-Hydroxyvitamin D Levels Are Associated with Functional Status at Time of Discharge from Intensive Care Unit in Critically Ill Surgical Patients. Nutr. Clin. Pract. 2018, 34, 572–580. [Google Scholar] [CrossRef]
- Brook, K.; Camargo, C.A.; Christopher, K.B.; Quraishi, S.A. Admission vitamin D status is associated with discharge destination in critically ill surgical patients. Ann. Intensiv. Care 2015, 5, 23. [Google Scholar] [CrossRef]
- Quraishi, S.A.; Bittner, E.A.; Blum, L.; McCarthy, C.M.; Bhan, I.; Camargo, C.A., Jr. Prospective Study of Vitamin D Status at Initiation of Care in Critically Ill Surgical Patients and Risk of 90-Day Mortality. Crit. Care Med. 2014, 42, 1365–1371. [Google Scholar] [CrossRef]
- Amrein, K.; Schnedl, C.; Holl, A.; Riedl, R.; Christopher, K.B.; Pachler, C.; Purkart, T.U.; Waltensdorfer, A.; Münch, A.; Warnkross, H.; et al. Effect of high-dose vitamin D3 on hospital length of stay in critically ill patients with vitamin D deficiency: The VITdAL-ICU randomized clinical trial. JAMA 2014, 312, 1520–1530. [Google Scholar] [CrossRef]
- Quraishi, S.A.; Bhan, I.; Matthay, M.A.; Thompson, B.T.; Camargo, C.A., Jr.; Bajwa, E.K. Vitamin D Status and Clinical Outcomes in Acute Respiratory Distress Syndrome: A Secondary Analysis from the Assessment of Low Tidal Volume and Elevated End-Expiratory Volume to Obviate Lung Injury (ALVEOLI) Trial. J. Intensive Care Med. 2022, 37, 793–802. [Google Scholar] [CrossRef]
- Huss, R. Isolation of Primary and Immortalized CD34 − Hematopoietic and Mesenchymal Stem Cells from Various Sources. Stem Cells 2000, 18, 1–9. [Google Scholar] [CrossRef]
- Le Blanc, K.; Mougiakakos, D. Multipotent mesenchymal stromal cells and the innate immune system. Nat. Rev. Immunol. 2012, 12, 383–396. [Google Scholar] [CrossRef]
- Moll, G.; Hoogduijn, M.J.; Ankrum, J.A. Editorial: Safety, Efficacy and Mechanisms of Action of Mesenchymal Stem Cell Therapies. Front. Immunol. 2020, 11, 243. [Google Scholar] [CrossRef] [PubMed]
- Seetharaman, R.; Mahmood, A.; Kshatriya, P.; Patel, D.; Srivastava, A. Mesenchymal Stem Cell Conditioned Media Ameliorate Psoriasis Vulgaris: A Case Study. Case Rep. Dermatol. Med. 2019, 2019, 8309103. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.; Zhang, H.; Liang, J.; Wang, H.; Hua, B.; Feng, X.; Gilkeson, G.S.; Farge, D.; Shi, S.; Sun, L. A Long-Term Follow-Up Study of Allogeneic Mesenchymal Stem/Stromal Cell Transplantation in Patients with Drug-Resistant Systemic Lupus Erythematosus. Stem Cell Rep. 2018, 10, 933–941. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Fu, J.; Xu, X.; Wang, S.; Xu, R.; Zhao, M.; Nie, W.; Wang, X.; Zhang, J.; Li, T.; et al. Safety and immunological responses to human mesenchymal stem cell therapy in difficult-to-treat HIV-1-infected patients. Aids 2013, 27, 1283–1293. [Google Scholar] [CrossRef] [PubMed]
- Orozco, L.; Munar, A.; Soler, R.; Alberca, M.; Soler, F.; Huguet, M.; Sentís, J.; Sánchez, A.; García-Sancho, J. Treatment of Knee Osteoarthritis with Autologous Mesenchymal Stem Cells. Transplantation 2013, 95, 1535–1541. [Google Scholar] [CrossRef]
- Cahill, E.F.; Kennelly, H.; Carty, F.; Mahon, B.P.; English, K. Hepatocyte Growth Factor Is Required for Mesenchymal Stromal Cell Protection against Bleomycin-Induced Pulmonary Fibrosis. Stem Cells Transl. Med. 2016, 5, 1307–1318. [Google Scholar] [CrossRef]
- Rahbarghazi, R.; Keyhanmanesh, R.; Aslani, M.R.; Hassanpour, M.; Ahmadi, M. Bone marrow mesenchymal stem cells and condition media diminish inflammatory adhesion molecules of pulmonary endothelial cells in an ovalbumin-induced asthmatic rat model. Microvasc. Res. 2018, 121, 63–70. [Google Scholar] [CrossRef]
- Antunes, M.A.; Abreu, S.C.; Cruz, F.F.; Teixeira, A.C.; Lopes-Pacheco, M.; Bandeira, E.; Olsen, P.C.; Diaz, B.L.; Takyia, C.M.; Freitas, I.P.; et al. Effects of different mesenchymal stromal cell sources and delivery routes in experi-mental emphysema. Respir. Res. 2014, 15, 118. [Google Scholar] [CrossRef]
- Dyer, D.P.; Thomson, J.M.; Hermant, A.; Jowitt, T.A.; Handel, T.M.; Proudfoot, A.E.I.; Day, A.J.; Milner, C.M. TSG-6 Inhibits Neutrophil Migration via Direct Interaction with the Chemokine CXCL8. J. Immunol. 2014, 192, 2177–2185. [Google Scholar] [CrossRef]
- Güldner, A.; Maron-Gutierrez, T.; Abreu, S.C.; Xisto, D.G.; Senegaglia, A.C.; Barcelos, P.R.D.S.; Silva, J.D.; Brofman, P.; de Abreu, M.G.; Rocco, P.R.M. Expanded endothelial progenitor cells mitigate lung injury in septic mice. Stem Cell Res. Ther. 2015, 6, 230. [Google Scholar] [CrossRef]
- Gupta, N.; Su, X.; Popov, B.; Lee, J.W.; Serikov, V.; Matthay, M.A. Intrapulmonary Delivery of Bone Marrow-Derived Mesenchymal Stem Cells Improves Survival and Attenuates Endotoxin-Induced Acute Lung Injury in Mice. J. Immunol. 2007, 179, 1855–1863. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.S.; Chang, Y.S.; Choi, S.J.; Kim, J.K.; Yoo, H.S.; Ahn, S.Y.; Sung, D.K.; Kim, S.Y.; Park, Y.R.; Park, W.S. Intratracheal transplantation of human umbilical cord blood-derived mesenchymal stem cells attenuates Escherichia coli-induced acute lung injury in mice. Respir. Res. 2011, 12, 108. [Google Scholar] [CrossRef] [PubMed]
- Danchuk, S.; Ylostalo, J.H.; Hossain, F.; Sorge, R.; Ramsey, A.; Bonvillain, R.W.; Lasky, J.A.; Bunnell, B.A.; Welsh, D.A.; Prockop, D.J.; et al. Human multipotent stromal cells attenuate lipopolysaccharide-induced acute lung injury in mice via secretion of tumor necrosis factor-α-induced protein 6. Stem Cell Res. Ther. 2011, 2, 27. [Google Scholar] [CrossRef] [PubMed]
- McIntyre, L.A.; Moher, D.; Fergusson, D.A.; Sullivan, K.J.; Mei, S.H.J.; Lalu, M.; Marshall, J.; Mcleod, M.; Griffin, G.; Grimshaw, J.; et al. Efficacy of Mesenchymal Stromal Cell Therapy for Acute Lung Injury in Preclinical Animal Models: A Systematic Review. PLoS ONE 2016, 11, e0147170. [Google Scholar] [CrossRef]
- Wilson, J.G.; Liu, K.D.; Zhuo, H.; Caballero, L.; McMillan, M.; Fang, X.; Cosgrove, K.; Vojnik, R.; Calfee, C.S.; Lee, J.-W.; et al. Mesenchymal stem (stromal) cells for treatment of ARDS: A phase 1 clinical trial. Lancet Respir. Med. 2015, 3, 24–32. [Google Scholar] [CrossRef]
- Gorman, E.; Shankar-Hari, M.; Hopkins, P.; Tunnicliffe, W.S.; Perkins, G.D.; Silversides, J.; McGuigan, P.; Krasnodembskaya, A.; Jackson, C.; Boyle, R.; et al. Repair of acute respiratory distress syndrome by stromal cell administration (REALIST) trial: A phase 1 trial. Eclinicalmedicine 2021, 41, 101167. [Google Scholar] [CrossRef]
- Bellingan, G.; Jacono, F.; Bannard-Smith, J.; Brealey, D.; Meyer, N.; Thickett, D.; Young, D.; Bentley, A.; McVerry, B.J.; Wunderink, R.G.; et al. Safety and efficacy of multipotent adult progenitor cells in acute respiratory distress syndrome (MUST-ARDS): A multicentre, randomised, double-blind, placebo-controlled phase 1/2 trial. Intensiv. Care Med. 2022, 48, 36–44. [Google Scholar] [CrossRef]
- Mukherjee, S.; Hanidziar, D. More of the Gut in the Lung: How Two Microbiomes Meet in ARDS. Yale J. Biol. Med. 2018, 91, 143–149. [Google Scholar]
- Panzer, A.R.; Lynch, S.V.; Langelier, C.; Christie, J.D.; McCauley, K.; Nelson, M.; Cheung, C.K.; Benowitz, N.L.; Cohen, M.J.; Calfee, C.S. Lung Microbiota Is Related to Smoking Status and to Development of Acute Respiratory Distress Syndrome in Critically Ill Trauma Patients. Am. J. Respir. Crit. Care Med. 2018, 197, 621–631. [Google Scholar] [CrossRef]
- Dickson, R.P.; Singer, B.H.; Newstead, M.W.; Falkowski, N.R.; Erb-Downward, J.R.; Standiford, T.J.; Huffnagle, G.B. Enrichment of the lung mi-crobiome with gut bacteria in sepsis and the acute respiratory distress syndrome. Nat. Microbiol. 2016, 1, 16113. [Google Scholar] [CrossRef]
- Kyo, M.; Nishioka, K.; Nakaya, T.; Kida, Y.; Tanabe, Y.; Ohshimo, S.; Shime, N. Unique patterns of lower respiratory tract microbiota are associated with inflammation and hospital mortality in acute respiratory distress syndrome. Respir. Res. 2019, 20, 246. [Google Scholar] [CrossRef] [PubMed]
- Li, B.; Yin, G.-F.; Wang, Y.-L.; Tan, Y.-M.; Huang, C.-L.; Fan, X.-M. Impact of fecal microbiota transplantation on TGF-β1/Smads/ERK signaling pathway of endotoxic acute lung injury in rats. 3 Biotech 2020, 10, 52. [Google Scholar] [CrossRef] [PubMed]
- Nalbantoglu, S. Metabolomics: Basic Principles and Strategies. In Molecular Medicine; IntechOpen: London, UK, 2019. [Google Scholar] [CrossRef]
- Aderemi, A.V.; Ayeleso, A.O.; Oyedapo, O.O.; Mukwevho, E. Metabolomics: A Scoping Review of Its Role as a Tool for Disease Biomarker Discovery in Selected Non-Communicable Diseases. Metabolites 2021, 11, 418. [Google Scholar] [CrossRef] [PubMed]
- Saiki, S.; Hatano, T.; Fujimaki, M.; Ishikawa, K.I.; Mori, A.; Oji, Y.; Okuzumi, A.; Fukuhara, T.; Koinuma, T.; Imamichi, Y.; et al. Decreased long-chainacylcarnitines from insufficient be-ta-oxidation as potential early diagnostic markers for Parkinson’s disease. Sci. Rep. 2017, 7, 7328. [Google Scholar] [CrossRef]
- Mazumder, A.G.; Banerjee, S.; Zevictovich, F.; Ghosh, S.; Mukherjee, A.; Chatterjee, J. Fourier-transform-infrared-spectroscopy based metabolomic spectral biomarker selection towards optimal diagnostic differentiation of diabetes with and without reti-nopathy. Spectrosc. Lett. 2018, 51, 340–349. [Google Scholar] [CrossRef]
- Li, X.S.; Wang, Z.; Cajka, T.; Buffa, J.A.; Nemet, I.; Hurd, A.G.; Gu, X.; Skye, S.M.; Roberts, A.B.; Wu, Y.; et al. Untargeted metabolomics identifies trimethyllysine, a TMAO-producing nutrient precursor, as a predictor of incident cardiovascular disease risk. J. Clin. Investig. 2018, 3, e99096. [Google Scholar] [CrossRef]
- Rubenfeld, G.D.; Caldwell, E.; Granton, J.; Hudson, L.D.; Matthay, M.A. Interobserver Variability in Applying a Radiographic Definition for ARDS. Chest 1999, 116, 1347–1353. [Google Scholar] [CrossRef]
- Thille, A.W.; Esteban, A.; Fernández-Segoviano, P.; Rodriguez, J.-M.; Aramburu, J.-A.; Peñuelas, O.; Cortés-Puch, I.; Cardinal-Fernández, P.; Lorente, J.A.; Frutos-Vivar, F. Comparison of the Berlin Definition for Acute Respiratory Distress Syndrome with Autopsy. Am. J. Respir. Crit. Care Med. 2013, 187, 761–767. [Google Scholar] [CrossRef]
- Metwaly, S.M.; Winston, B.W. Systems Biology ARDS Research with a Focus on Metabolomics. Metabolites 2020, 10, 207. [Google Scholar] [CrossRef]
- Schubert, J.K.; Müller, W.P.E.; Benzing, A.; Geiger, K. Application of a new method for analysis of exhaled gas in critically ill patients. Intensiv. Care Med. 1998, 24, 415–421. [Google Scholar] [CrossRef]
- King, J.; Mochalski, P.; Unterkofler, K.; Teschl, G.; Klieber, M.; Stein, M.; Amann, A.; Baumann, M. Breath isoprene: Muscle dystrophy patients support the concept of a pool of isoprene in the periphery of the human body. Biochem. Biophys. Res. Commun. 2012, 423, 526–530. [Google Scholar] [CrossRef] [PubMed]
- Bos, L.D.J.; Weda, H.; Wang, Y.; Knobel, H.H.; Nijsen, T.M.E.; Vink, T.J.; Zwinderman, A.H.; Sterk, P.J.; Schultz, M.J. Exhaled breath metabolomics as a noninvasive diagnostic tool for acute respiratory distress syndrome. Eur. Respir. J. 2014, 44, 188–197. [Google Scholar] [CrossRef] [PubMed]
- Rai, R.K.; Azim, A.; Sinha, N.; Sahoo, J.N.; Singh, C.; Ahmed, A.; Saigal, S.; Baronia, A.K.; Gupta, D.; Gurjar, M.; et al. Metabolic profiling in human lung injuries by high-resolution nuclear magnetic resonance spectroscopy of bronchoalveolar lavage fluid (BALF). Metabolomics 2012, 9, 667–676. [Google Scholar] [CrossRef]
- Evans, C.; Karnovsky, A.; Kovach, M.A.; Standiford, T.J.; Burant, C.F.; Stringer, K.A. Untargeted LC–MS Metabolomics of Bronchoalveolar Lavage Fluid Differentiates Acute Respiratory Distress Syndrome from Health. J. Proteome Res. 2013, 13, 640–649. [Google Scholar] [CrossRef] [PubMed]
- Owens, R.L.; Stigler, W.S.; Hess, D.R. Do Newer Monitors of Exhaled Gases, Mechanics, and Esophageal Pressure Add Value? Clin. Chest Med. 2008, 29, 297–312. [Google Scholar] [CrossRef] [PubMed]
| Hyperinflammatory Phenotype Compared to Hypo-Inflammatory Phenotype |
|---|
| High levels of IL-6, IL-8, sTNFr-1 |
| Lower serum bicarbonate levels |
| Low protein C levels |
| More profound hypotension |
| Higher mortality |
| Less ventilator-free days |
| Lower mortality with higher PEEP |
| Improved mortality with fluid conservative strategy |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ramji, H.F.; Hafiz, M.; Altaq, H.H.; Hussain, S.T.; Chaudry, F. Acute Respiratory Distress Syndrome; A Review of Recent Updates and a Glance into the Future. Diagnostics 2023, 13, 1528. https://doi.org/10.3390/diagnostics13091528
Ramji HF, Hafiz M, Altaq HH, Hussain ST, Chaudry F. Acute Respiratory Distress Syndrome; A Review of Recent Updates and a Glance into the Future. Diagnostics. 2023; 13(9):1528. https://doi.org/10.3390/diagnostics13091528
Chicago/Turabian StyleRamji, Husayn F., Maida Hafiz, Hiba Hammad Altaq, Syed Talal Hussain, and Fawad Chaudry. 2023. "Acute Respiratory Distress Syndrome; A Review of Recent Updates and a Glance into the Future" Diagnostics 13, no. 9: 1528. https://doi.org/10.3390/diagnostics13091528
APA StyleRamji, H. F., Hafiz, M., Altaq, H. H., Hussain, S. T., & Chaudry, F. (2023). Acute Respiratory Distress Syndrome; A Review of Recent Updates and a Glance into the Future. Diagnostics, 13(9), 1528. https://doi.org/10.3390/diagnostics13091528







