The Role of Artificial Intelligence in Monitoring Inflammatory Bowel Disease—The Future Is Now
Abstract
1. Introduction
2. Understanding the Role of Artificial Intelligence in Gastroenterology
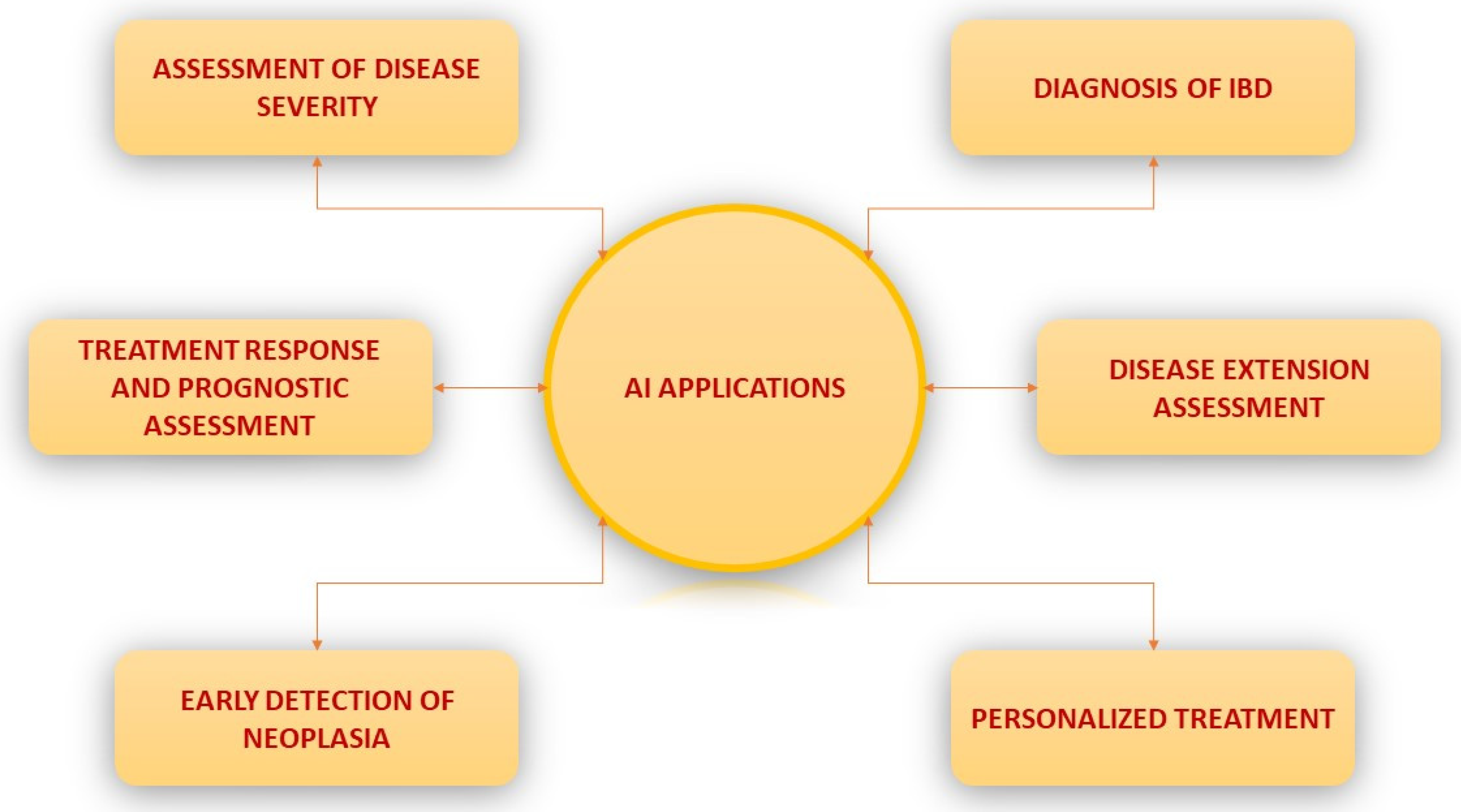
3. Potential Applications of AI in IBD
4. The Role of Artificial Intelligence in Assessing Disease Activity
| Study | Study Type | Modality | AI Classifier | Aim of AI Use | Training Set | Results | ||
|---|---|---|---|---|---|---|---|---|
| Accuracy | Sensitivity | Specificity | ||||||
| Quénéhervé L et al. [37] | Retrospective | CFLC | Automated analysis method | Discrimination between CD and UC | 12.900 images | 91.0 | 74.0 | 97.0 |
| Stidham R et al. [38] | Retrospective | WLI | CNN | Discriminating endoscopic remission from moderately-severe disease UC | 16.514 images | 83.0 | 96.0 | |
| Bossuyt P et al. [39] | Prospective | WLI | Integration of pixel color data | Assessment of disease activity in UC | 35 patients | R = 0.65 RD correlated with RHI | ||
| Ozawa T et al. [35] | Retrospective | WLI | CNN | Mucosal healing in UC | −26.304 images | AUROC 0.98 (Mayo 0–1) | ||
| Takenaka et al. [36] | Prospective | WLI | DNN | 40.758 images | 90.1 | 93.3 | 87.8 | |
| Maeda et al. [40] | Retrospective | EC | SVM | Prediction of persistent inflammation | 12.900 images | 91.0 | 74.0 | 97.0 |
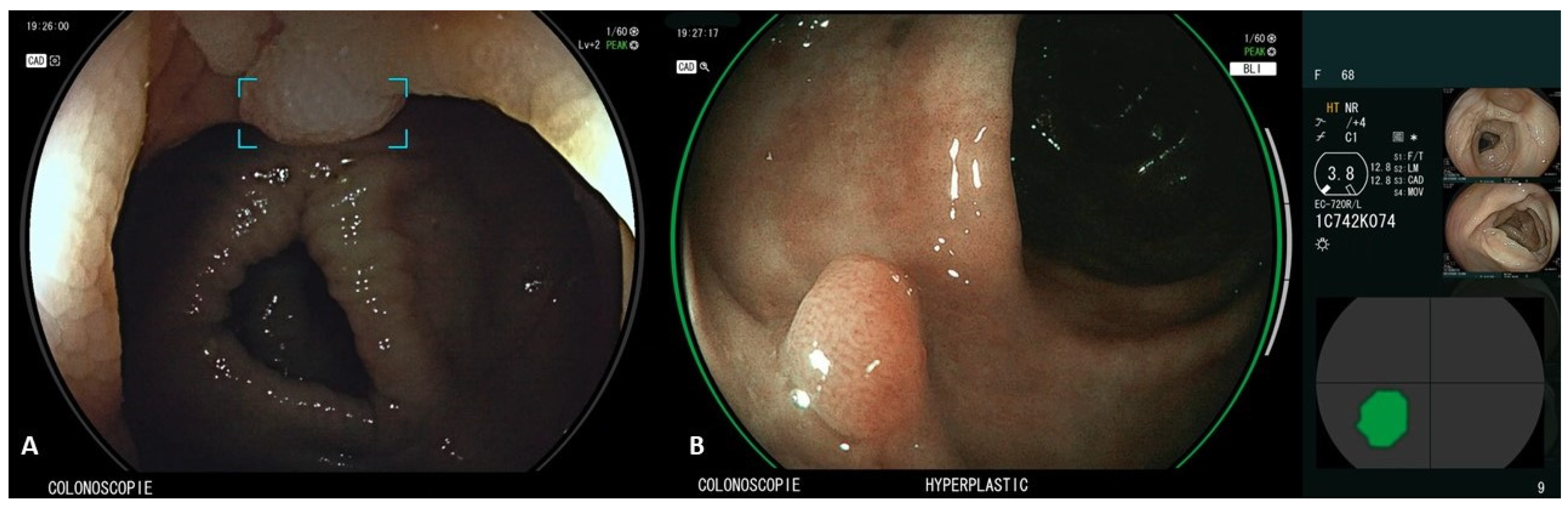
5. The Role of Artificial Intelligence in Screening for Early Neoplasia in IBD
6. AI in Aiding IBD Treatment—Disease Progression Prediction/Response to Treatment
7. Discussion
8. Future Directions
9. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Knowles, S.R.; Graff, L.; Wilding, H.; Hewitt, C.; Keefer, L.; Mikocka-Walus, A. Quality of Life in Inflammatory Bowel Disease: A Systematic Review and Meta-analyses—Part I. Inflamm. Bowel Dis. 2018, 24, 742–751. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.; Chowdhry, M.; Umar, S.; Bilal, M.; Clarke, K. Variations in the medical treatment of inflammatory bowel disease among gastroenterologists. Gastroenterol. Rep. 2017, 6, 61–64. [Google Scholar] [CrossRef]
- Rubin, D.T.; Rothe, J.A.; Hetzel, J.T.; Cohen, R.D.; Hanauer, S.B. Are dysplasia and colorectal cancer endoscopically visible in patients with ulcerative colitis? Gastrointest. Endosc. 2007, 65, 998–1004. [Google Scholar] [CrossRef] [PubMed]
- Sundaram, S.; Choden, T.; Mattar, M.C.; Desai, S.; Desai, M. Artificial intelligence in inflammatory bowel disease endoscopy: Current landscape and the road ahead. Ther. Adv. Gastrointest. Endosc. 2021, 14, 26317745211017809. [Google Scholar] [CrossRef]
- Davenport, T.; Kalakota, R. The potential for artificial intelligence in healthcare. Futur. Health J. 2019, 6, 94–98. [Google Scholar] [CrossRef] [PubMed]
- Sinonquel, P.; Eelbode, T.; Bossuyt, P.; Maes, F.; Bisschops, R. Artificial intelligence and its impact on quality improvement in upper and lower gastrointestinal endoscopy. Dig. Endosc. 2020, 33, 242–253. [Google Scholar] [CrossRef]
- Okagawa, Y.; Abe, S.; Yamada, M.; Oda, I.; Saito, Y. Artificial Intelligence in Endoscopy. Dig. Dis. Sci. 2022, 67, 1553–1572. [Google Scholar] [CrossRef] [PubMed]
- Choudhary, K.; DeCost, B.; Chen, C.; Jain, A.; Tavazza, F.; Cohn, R.; Park, C.W.; Choudhary, A.; Agrawal, A.; Billinge, S.J.K.; et al. Recent advances and applications of deep learning methods in materials science. npj Comput. Mater. 2022, 8, 59. [Google Scholar] [CrossRef]
- Pannala, R.; Krishnan, K.; Melson, J.; Parsi, M.A.; Schulman, A.R.; Sullivan, S.; Trikudanathan, G.; Trinidade, A.J.; Watson, R.R.; Maple, J.T.; et al. Emerging role of artificial intelligence in GI endoscopy. Gastrointest. Endosc. 2020, 92, 1151–1152. [Google Scholar] [CrossRef]
- Chen, G.; Shen, J. Artificial Intelligence Enhances Studies on Inflammatory Bowel Disease. Front. Bioeng. Biotechnol. 2021, 9, 635764. [Google Scholar] [CrossRef]
- Rex, D.K.; Mori, Y.; Sharma, P.; Lahr, R.E.; Vemulapalli, K.C.; Hassan, C. Strengths and Weaknesses of an Artificial Intelligence Polyp Detection Program as Assessed by a High-Detecting Endoscopist. Gastroenterology 2022, 163, 354–358. [Google Scholar] [CrossRef] [PubMed]
- Kamitani, Y.; Nonaka, K.; Isomoto, H. Current Status and Future Perspectives of Artificial Intelligence in Colonoscopy. J. Clin. Med. 2022, 11, 2923. [Google Scholar] [CrossRef]
- van der Sommen, F.; de Groof, J.; Struyvenberg, M.; van der Putten, J.; Boers, T.; Fockens, K.; Schoon, E.J.; Curvers, W.; de With, P.; Mori, Y.; et al. Machine learning in GI endoscopy: Practical guidance in how to interpret a novel field. Gut 2020, 69, 2035–2045. [Google Scholar] [CrossRef] [PubMed]
- Kudo, S.-E.; Ichimasa, K.; Villard, B.; Mori, Y.; Misawa, M.; Saito, S.; Hotta, K.; Saito, Y.; Matsuda, T.; Yamada, K.; et al. Artificial Intelligence System to Determine Risk of T1 Colorectal Cancer Metastasis to Lymph Node. Gastroenterology 2021, 160, 1075–1084.e2. [Google Scholar] [CrossRef] [PubMed]
- Maaser, C.; Sturm, A.; Vavricka, S.R.; Kucharzik, T.; Fiorino, G.; Annese, V.; Calabrese, E.; Baumgart, D.C.; Bettenworth, D.; Nunes, P.B.; et al. ECCO-ESGAR Guideline for Diagnostic Assessment in IBD Part 1: Initial diagnosis, monitoring of known IBD, detection of complications. J. Crohns Colitis 2019, 13, 144–164. [Google Scholar] [CrossRef]
- Sturm, A.; Maaser, C.; Calabrese, E.; Annese, V.; Fiorino, G.; Kucharzik, T.; Vavricka, S.R.; Verstockt, B.; van Rheenen, P.; Tolan, D.; et al. ECCO-ESGAR Guideline for Diagnostic Assessment in IBD Part 2: IBD scores and general principles and technical aspects. J. Crohns Colitis 2019, 13, 273–284. [Google Scholar] [CrossRef]
- Wei, Z.; Wang, W.; Bradfield, J.; Li, J.; Cardinale, C.; Frackelton, E.; Kim, C.; Mentch, F.; Van Steen, K.; Visscher, P.M.; et al. Large Sample Size, Wide Variant Spectrum, and Advanced Machine-Learning Technique Boost Risk Prediction for Inflammatory Bowel Disease. Am. J. Hum. Genet. 2013, 92, 1008–1012. [Google Scholar] [CrossRef] [PubMed]
- Chen, P.; Zhou, G.; Lin, J.; Li, L.; Zeng, Z.; Chen, M.; Zhang, S. Serum Biomarkers for Inflammatory Bowel Disease. Front. Med. 2020, 7, 123. [Google Scholar] [CrossRef] [PubMed]
- Isakov, O.; Dotan, I.; Ben-Shachar, S. Machine Learning-Based Gene Prioritization Identifies Novel Candidate Risk Genes for Inflammatory Bowel Disease. Inflamm. Bowel Dis. 2017, 23, 1516–1523. [Google Scholar] [CrossRef]
- Annese, V.; Daperno, M.; Rutter, M.D.; Amiot, A.; Bossuyt, P.; East, J.; Ferrante, M.; Gotz, M.; Katsanos, K.H.; Kießlich, R.; et al. European evidence based consensus for endoscopy in inflammatory bowel disease. J. Crohns Colitis 2013, 7, 982–1018. [Google Scholar] [CrossRef] [PubMed]
- Peyrin-Biroulet, L.; Sandborn, W.; Sands, B.E.; Reinjsch, W.; Bemelman, W.; Bryant, R.V.; D’Haens, G.; Dotan, I.; Dubinsky, M.; Faegan, B.; et al. Selecting Therapeutic Targets in Inflammatory Bowel Disease (STRIDE): Determining Therapeutic Goals for Treat-toTarget. Am. J. Gastroenterol. 2015, 110, 1324–1338. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, S.R.; Pinto, J.S.L.D.; Marques da Costa, P.; Correira, L. Disagreement Among Gastroenterologists Using the Mayo and Rutgeerts Endoscopic Scores. Inflamm. Bowel Dis. 2018, 24, 254–260. [Google Scholar] [CrossRef] [PubMed]
- Bhambhvani, H.P.; Zamora, A. Deep learning enabled classification of Mayo endoscopic subscore in patients with ulcerative colitis. Eur. J. Gastroenterol. Hepatol. 2021, 33, 645–649. [Google Scholar] [CrossRef] [PubMed]
- Becker, B.G.; Arcadu, F.; Thalhammer, A. Training and deploying a deep learning model for endoscopic severity grading in ulcerative colitis using multicenter clinical trial data. Ther. Adv. Gastrointest. Endosc. 2021, 14, 2631774521990623. [Google Scholar] [CrossRef]
- Takenaka, K.; Ohtsuka, K.; Fujii, T.; Oshima, S.; Okamoto, R.; Watanbe, M. Deep neural network accurately predicts prognosis of ulcerative colitis using endoscopic images. Gastroenterology 2021, 160, 2175–2177. [Google Scholar] [CrossRef] [PubMed]
- Yao, H.; Najarian, K.; Gryak, J.; Bishu, S.; Rice, M.D.; Waljee, A.K.; Wilkins, H.J.; Stidham, R.W. Fully automated endoscopic disease activity assessment in ulcerative colitis. Gastrointest. Endosc. 2020, 93, 728–736.e1. [Google Scholar] [CrossRef]
- Gottlieb, K.; Requa, J.; Karnes, W.; Gudivada, R.C.; Shen, J.; Rael, E.; Arora, V.; Dao, T.; Ninh, A.; McGill, J. Central reading of ulcerative colitis clinical trial videos using neural networks. Gastroenterology 2021, 160, 710–719. [Google Scholar] [CrossRef]
- Uttam, S.; Hashash, J.G.; LaFace, J.; Binion, D.; Regueiro, M.; Hartman, D.J.; Brand, R.E.; Liu, Y. Three-Dimensional Nanoscale Nuclear Architecture Mapping of Rectal Biopsies Detects Colorectal Neoplasia in Patients with Inflammatory Bowel Disease. Cancer Prev. Res. 2019, 12, 527–538. [Google Scholar] [CrossRef]
- Klang, E.; Barash, Y.; Margalit, R.Y.; Soffer, S.; Shimon, O.; Albshesh, A.; Ben-Horin, S.; Amitai, M.M.; Eliakim, R.; Kopylov, U. Deep learning algorithms for automated detection of Crohn’s disease ulcers by video capsule endoscopy. Gastrointest. Endosc. 2019, 91, 606–613. [Google Scholar] [CrossRef]
- Klenske, E.; Bojarski, C.; Waldner, M.; Rath, T.; Neurath, M.F.; Atreya, R. Targeting mucosal healing in Crohn’s disease: What the clinician needs to know. Ther. Adv. Gastroenterol. 2019, 12, 1756284819856865. [Google Scholar] [CrossRef]
- Colombel, J.F.; Rutgeerts, P.; Reinisch, W.; Esser, D.; Wang, Y.; Lang, Y.; Marano, C.W.; Strauss, R.; Oddens, B.J.; Feagan, B.G.; et al. Early mucosal healing with infliximab is associated with improved long-term clinical outcomes in ulcerative colitis. Gastroenterology 2011, 141, 1194–1201. [Google Scholar] [CrossRef] [PubMed]
- Turner, D.; Ricciuto, A.; Lewis, A.; D’Amico, F.; Dhaliwal, J.; Griffiths, A.M.; Bettenworth, D.; Sandborn, W.J.; Sands, B.E.; Reinisch, W.; et al. STRIDE-II: An Update on the Selecting Therapeutic Targets in Inflammatory Bowel Disease (STRIDE) Initiative of the International Organization for the Study of IBD (IOIBD): Determining Therapeutic Goals for Treat-to-Target strategies in IBD. Gastroenterology 2021, 160, 1570–1583. [Google Scholar] [CrossRef] [PubMed]
- Daperno, M.; Comberlato, M.; Bossa, F.; Biancone, L.; Bonanomi, A.G.; Cassinotti, A.; Cosintino, R.; Lombardi, G.; Mangiarotti, R.; Papa, A.; et al. Inter-observer agreement in endoscopic scoring systems: Preliminary report of an ongoing study from the Italian Group for Inflammatory Bowel Disease (IG-IBD). Dig. Liver Dis. 2014, 46, 969–973. [Google Scholar] [CrossRef] [PubMed]
- Yang, L.S.; Perry, E.; Shan, L.; Wilding, H.; Connell, W.; Thompson, A.J.; Taylor, A.C.F.; Desmond, P.V.; Holt, B.A. Clinical application and diagnostic accuracy of artificial intelligence in colonoscopy for inflammatory bowel disease: Systematic review. Endosc. Int. Open 2022, 10, E1004–E1013. [Google Scholar] [CrossRef]
- Ozawa, T.; Ishihara, S.; Fujishiro, M.; Saito, H.; Kumagai, Y.; Shichijo, S.; Aoyama, K.; Tada, T. Novel computer-assisted diagnosis system for endoscopic disease activity in patients with ulcerative colitis. Gastrointest. Endosc. 2018, 89, 416–421. [Google Scholar] [CrossRef]
- Takenaka, K.; Ohtsuka, K.; Fujii, T.; Negi, M.; Suzuki, K.; Shimizu, H.; Oshima, S.; Akiyama, S.; Motobayashi, M.; Nagahori, M.; et al. Development and validation of a deep neural network for accurate evaluation of endoscopic images from patients with ulcerative colitis. Gastroenterology 2020, 158, 2150–2157. [Google Scholar] [CrossRef]
- Quénéhervé, L.; David, G.; Bourreille, A.; Hardouin, J.B.; Rahmi, G.; Neunlist, M.; Bregeon, J.; Coron, E. Quantitative assessment of mucosal architecture using computer-based analysis of confocal laser endomicroscopy in infammatory bowel diseases. Gastrointest. Endosc. 2019, 89, 626–636. [Google Scholar] [CrossRef]
- Stidham, R.W.; Liu, W.; Bishu, S.; Rice, M.D.; Higgins, P.D.R.; Zhu, J.; Nallamothu, B.K.; Waljee, A.K. Performance of a deep learning model vs. human reviewers in grading endoscopic disease severity of patients with ulcerative colitis. JAMA Netw. Open 2019, 2, 193963. [Google Scholar] [CrossRef]
- Bossuyt, P.; Nakase, H.; Vermeire, S.; de Hertogh, G.; Eelbode, T.; Ferrante, M.; Hasegawa, T.; Willekens, H.; Ikemoto, Y.; Makino, T.; et al. Automatic, computeraided determination of endoscopic and histological infammation in patients with mild to moderate ulcerative colitis based on red density. Gut 2020, 69, 1778–1786. [Google Scholar] [CrossRef]
- Maeda, Y.; Kudo, S.E.; Mori, Y.; Misawa, M.; Ogata, N.; Sesanuma, S.; Wakamura, K.; Oda, M.; Mori, K.; Ohtsuka, K. Fully automated diagnostic system with artificial intelligence using endocytoscopy to identify the presence of histologic inflammation associated with ulcerative colitis (with video). Gastrointest. Endosc. 2019, 89, 408–415. [Google Scholar] [CrossRef]
- Gui, X.; Bazarova, A.; del Amor, R.; Vieth, M.; de Hertogh, G.; Villanacci, V.; Zardo, D.; Parigi, T.L.; Røyset, E.S.; Shivaji, U.N.; et al. PICaSSO Histologic Remission Index (PHRI) in ulcerative colitis: Development of a novel simplified histological score for monitoring mucosal healing and predicting clinical outcomes and its applicability in an artificial intelligence system. Gut 2022, 71, 889–898. [Google Scholar] [CrossRef]
- Kim, S.H.; Lim, Y.J. Artificial Intelligence in Capsule Endoscopy: A Practical Guide to Its Past and Future Challenges. Diagnostics 2021, 11, 1722. [Google Scholar] [CrossRef]
- Barash, Y.; Azaria, L.; Soffer, S.; Yehuda, R.M.; Shlomi, O.; Ben-Horin, S.; Eliakim, R.; Klang, E.; Kopylov, U. Ulcer severity grading in video capsule images of patients with Crohn’s disease: An ordinal neural network solution. Gastrointest. Endosc. 2020, 93, 187–192. [Google Scholar] [CrossRef]
- Kamiya, K.J.L.; Hosoe, N.; Hayashi, Y.; Kawaguchi, T.; Takabayashi, K.; Ogata, H.; Kanai, T. Video capsule endoscopy in inflammatory bowel disease. DEN Open 2021, 2, e26. [Google Scholar] [CrossRef]
- Fan, S.; Xu, L.; Fan, Y.; Wei, K.; Li, L. Computer-aided detection of small intestinal ulcer and erosion in wireless capsule endoscopy images. Phys. Med. Biol. 2018, 63, 165001. [Google Scholar] [CrossRef] [PubMed]
- Aoki, T.; Yamada, A.; Aoyama, K.; Saito, H.; Fujisawa, G.; Odawara, N.; Kondo, R.; Tsuboi, A.; Ishibashi, R.; Nakada, A.; et al. Clinical usefulness of a deep learning-based system as the first screening on small-bowel capsule endoscopy reading. Dig. Endosc. 2019, 32, 585–591. [Google Scholar] [CrossRef] [PubMed]
- Yashiro, M. Ulcerative colitis-associated colorectal cancer. World J. Gastroenterol. 2014, 20, 16389–16397. [Google Scholar] [CrossRef] [PubMed]
- Herszenyi, L.; Miheller, P.; Tulassay, Z. Carcinogenesis in inflammatory bowel disease. Dig. Dis. 2007, 25, 267–269. [Google Scholar] [CrossRef] [PubMed]
- Marabotto, E.; Kayali, S.; Buccilli, S.; Levo, F.; Bodini, G.; Giannini, E.G.; Savarino, V.; Savarino, E.V. Colorectal Cancer in Inflammatory Bowel Diseases: Epidemiology and Prevention: A Review. Cancers 2022, 14, 4254. [Google Scholar] [CrossRef]
- Scarpa, M.; Castagliuolo, I.; Castoro, C.; Pozza, A.; Scarpa, M.; Kotsafti, A.; Angriman, I. Inflammatory colonic carcinogenesis: A review on pathogenesis and immunosurveillance mechanisms in ulcerative colitis. World J. Gastroenterol. 2014, 20, 6774–6785. [Google Scholar] [CrossRef]
- Ang, T.L.; Wang, L.M. Artificial intelligence for the diagnosis of dysplasia in inflammatory bowel diseases. J. Gastroenterol. Hepatol. 2022, 37, 1469–1470. [Google Scholar] [CrossRef] [PubMed]
- Wallace, M.B.; Sharma, P.; Bhandari, P.; East, J.; Antonelli, G.; Lorenzetii, R.; Vieth, M.; Speranza, I.; Spadaccini, M.; Desai, M.; et al. Impact of Artificial Intelligence on Miss Rate of Colorectal Neoplasia. Gastroenterology 2022, 163, 295–304. [Google Scholar] [CrossRef] [PubMed]
- Magro, F.; Gionchetti, P.; Eliakim, R.; Ardizzone, S.; Armuzzi, A.; Barreiro-de Acosta, M.; Burisch, J.; Gecse, K.B.; Hart, A.L.; Hindryckx, P.; et al. Third European Evidence-based Consensus on Diagnosis and Management of Ulcerative Colitis. Part 1: Definitions, Diagnosis, Extra-intestinal Manifestations, Pregnancy, Cancer Surveillance, Surgery, and Ileo-anal Pouch Disorders. J. Crohns Colitis 2017, 11, 649–670. [Google Scholar] [CrossRef] [PubMed]
- Rubin, D.T.; Ananthakrishnan, A.N.; Siegel, C.A.; Sauer, B.G.; Long, M.D. ACG Clinical Guideline: Ulcerative Colitis in Adults. Am. J. Gastroenterol. 2019, 114, 384–413. [Google Scholar] [CrossRef]
- Lamb, C.A.; Kennedy, N.A.; Raine, T.; Hendy, P.A.; Smith, P.J.; Limdi, J.K.; Hayee, B.; Lomer, M.C.E.; Parkes, G.C.; Selinger, C.; et al. British Society of Gastroenterology consensus guidelines on the management of inflammatory bowel disease in adults. Gut 2019, 68 (Suppl. 3), s1–s106. [Google Scholar] [CrossRef]
- Shah, S.C.; Itzkowitz, S.H. Colorectal Cancer in Inflammatory Bowel Disease: Mechanisms and Management. Gastroenterology 2022, 162, 715–730. [Google Scholar] [CrossRef]
- Marques, K.F.; Marques, A.F.; Lopes, M.A.; Beraldo, R.F.; Lima, T.B.; Sassaki, L.Y. Artificial intelligence in colorectal cancer screening in patients with inflammatory bowel disease. Artif. Intell. Gastrointest. Endosc. 2022, 3, 1–8. [Google Scholar] [CrossRef]
- Laine, L.; Kaltenbach, T.; Barkun, A.; McQuaid, K.R.; Subramanian, V.; Soetikno, R. SCENIC Guideline Development Panel. SCENIC international consensus statement on surveillance and management of dysplasia in inflammatory bowel disease. Gastroenterology 2015, 148, 639–651. [Google Scholar] [CrossRef]
- Murthy, S.K.; Feuerstein, J.D.; Nguyen, G.C.; Velayos, F.S. AGA clinical practice update on endoscopic surveillance and management of colorectal dysplasia in inflammatory bowel disease: Expert review. Gastroenterology 2021, 161, 1043–1051. [Google Scholar] [CrossRef]
- Bisschops, R.; Bessissow, T.; Joseph, J.A.; Baert, F.; Ferrante, M.; Ballet, V.; Willekens, H.; Demedts, I.; Geboes, K.; De Hertogh, G.; et al. Chromoendoscopy versus narrow band imaging in UC: A prospective randomised controlled trial. Gut 2018, 67, 1087–1094. [Google Scholar] [CrossRef]
- Shukla, R.; Salem, M.; Hou, J.K. Use and barriers to chromoendoscopy for dysplasia surveillance in inflammatory bowel disease. World J. Gastrointest. Endosc. 2017, 9, 359–367. [Google Scholar] [CrossRef] [PubMed]
- Jess, T.; Rungoe, C.; Peyrin-Biroulet, L. Risk of colorectal cancer in patients with ulcerative colitis: A meta-analysis of population-based cohort studies. Clin. Gastroenterol. Hepatol. 2012, 10, 639–645. [Google Scholar] [CrossRef] [PubMed]
- Farraye, F.; Odze, R.D.; Eaden, J.; Itzkowitz, S.H.; McCabe, R.P.; Dassopoulos, T.; Lewis, J.D.; Ullman, T.A.; James, T.; McLeod, R.; et al. AGA medical position statement on the diagnosis and management of colorectal neoplasia in inflammatory bowel disease. Gastroenterology 2010, 138, 738–745. [Google Scholar] [CrossRef] [PubMed]
- Kohli, A.; Holzwanger, E.A.; Levy, A.N. Emerging use of artificial intelligence in inflammatory bowel disease. World J. Gastroenterol. 2020, 26, 6923–6928. [Google Scholar] [CrossRef]
- Alagappan, M.; Brown, J.R.G.; Mori, Y.; Berzin, T.M. Artificial intelligence in gastrointestinal endoscopy: The future is almost here. World J. Gastrointest. Endosc. 2018, 10, 239–249. [Google Scholar] [CrossRef] [PubMed]
- Hassan, C.; Wallace, M.B.; Sharma, P.; Maselli, R.; Craviotto, V.; Spadaccini, M.; Repici, A. New artificial intelligence system: First validation study versus experienced endoscopists for colorectal polyp detection. Gut 2020, 69, 799–800. [Google Scholar] [CrossRef] [PubMed]
- Misawa, M.; Kudo, S.-E.; Mori, Y.; Hotta, K.; Ohtsuka, K.; Matsuda, T.; Saito, S.; Kudo, T.; Baba, T.; Ishida, F.; et al. Development of a computer-aided detection system for colonoscopy and a publicly accessible large colonoscopy video database (with video). Gastrointest. Endosc. 2020, 93, 960–967. [Google Scholar] [CrossRef] [PubMed]
- Maeda, Y.; Kudo, S.E.; Ogata, N.; Misawa, M.; Mori, Y.; Mori, K.; Ohtsuka, K. Can artificial intelligence help to detect dysplasia in patients with ulcerative colitis? Endoscopy 2021, 53, E273–E274. [Google Scholar] [CrossRef]
- Leifeld, L.; Rogler, G.; Stallmach, A.; Schmidt, C.; Zuber-Jerger, I.; Hartmann, F.; Plauth, M.; Drabik, A.; Hofstadter, F.; Dienes, H.P.; et al. Detect Dysplasia Study Group. White-light or narrow-band imaging colonoscopy in surveillance of ulcerative colitis: A prospective multicenter study. Clin. Gastroenterol. Hepatol. 2015, 13, 1776–1781. [Google Scholar] [CrossRef]
- Solitano, V.; Zilli, A.; Franchellucci, G.; Allocca, M.; Fiorino, G.; Furfaro, F.; D’amico, F.; Danese, S.; Al Awadhi, S. Artificial Endoscopy and Inflammatory Bowel Disease: Welcome to the Future. J. Clin. Med. 2022, 11, 569. [Google Scholar] [CrossRef]
- Panaccione, R.; Colombel, J.-F.; Louis, E.; Peyrin-Biroulet, L.; Sandborn, W.J. Evolving definitions of remission in Crohn’s disease. Inflamm. Bowel Dis. 2013, 19, 1645–1653. [Google Scholar] [CrossRef] [PubMed]
- Sandborn, W.J.; Hanauer, S.; Van Assche, G.; Panes, J.; Wilson, S.; Petersson, J.; Panaccione, R. Treating beyond symptoms with a view to improving patient outcomes in inflammatory bowel diseases. J. Crohns Colitis 2014, 8, 927–935. [Google Scholar] [CrossRef] [PubMed]
- Neurath, M.F.; Travis, S.P. Mucosal healing in inflammatory bowel diseases: A systematic review. Gut 2012, 61, 1619–1635. [Google Scholar] [CrossRef] [PubMed]
- Neurath, M.F. Current and emerging therapeutic targets for IBD. Nat. Rev. Gastroenterol. Hepatol. 2017, 14, 269–278. [Google Scholar] [CrossRef] [PubMed]
- Weisshof, R.; El Jurdi, K.; Zmeter, N.; Rubin, D.T. Emerging Therapies for Inflammatory Bowel Disease. Adv. Ther. 2018, 35, 1746–1762. [Google Scholar] [CrossRef]
- Yu, H.; MacIsaac, D.; Wong, J.J.; Sellers, Z.M.; Wren, A.A.; Bensen, R.; Kin, C.; Park, K.T. Market share and costs of biologic therapies for inflammatory bowel disease in the USA. Aliment. Pharmacol. Ther. 2018, 47, 364–370. [Google Scholar] [CrossRef]
- Breiman, L. Random forests. Mach. Learn. 2001, 45, 5–32. [Google Scholar] [CrossRef]
- Waljee, A.K.; Joyce, J.C.; Wang, S.; Saxena, A.; Hart, M.; Zhu, J.; Higgins, P.D. Algorithms outperform metabolite tests in predicting response of patients with inflammatory bowel disease to thiopurines. Clin. Gastroenterol. Hepatol. 2010, 8, 143–150. [Google Scholar] [CrossRef] [PubMed]
- Waljee, A.K.; Sauder, K.; Patel, A.; Segar, S.; Liu, B.; Zhang, Y.; Zhu, J.; Stidham, R.W.; Balis, U.; Higgins, P.D. Machine Learning Algorithms for Objective Remission and Clinical Outcomes with Thiopurines. J. Crohns Colitis 2017, 11, 801–810. [Google Scholar] [CrossRef]
- Sandborn, W.J.; Feagan, B.G.; Rutgeerts, P.; Hanauer, S.; Colombel, J.F.; Sands, B.E.; Lukas, M.; Fedorak, R.N.; Lee, S.; Bressler, B.; et al. Vedolizumab as induction and maintenance therapy for Crohn’s disease. N. Engl. J. Med. 2013, 369, 711–721. [Google Scholar] [CrossRef] [PubMed]
- Waljee, A.K.; Liu, B.; Sauder, K.; Zhu, J.; Govani, S.M.; Stidham, R.W.; Higgins, P.D. Predicting Corticosteroid-Free Biologic Remission with Vedolizumab in Crohn’s Disease. Inflamm. Bowel Dis. 2018, 24, 1185–1192. [Google Scholar] [CrossRef] [PubMed]
- Waljee, A.K.; Liu, B.; Sauder, K.; Zhu, J.; Govani, S.M.; Stidham, R.W.; Higgins, P.D. Predicting corticosteroid-free endoscopic remission with vedolizumab in ulcerative colitis. Aliment. Pharmacol. Ther. 2018, 47, 763–772. [Google Scholar] [CrossRef] [PubMed]
- Waljee, A.K.; Wallace, B.I.; Cohen-Mekelburg, S.; Liu, Y.; Liu, B.; Sauder, K.; Stidham, R.W.; Zhu, J.; Higgins, P.D.R. Development and Validation of Machine Learning Models in Prediction of Remission in Patients With Moderate to Severe Crohn Disease. JAMA Netw. Open 2019, 2, e197386. [Google Scholar] [CrossRef] [PubMed]
- Denson, L.A.; Curran, M.; McGovern, D.P.B.; Koltun, Q.A.; Duerr, R.H.; Kim, S.C.; Sartor, R.B.; Silvester, F.A.; Abraham, C.; Zoeten, E.F. Challenges in IBD Research: Precision Medicine. Inflamm. Bowel Dis. 2019, 25, S31–S39. [Google Scholar] [CrossRef] [PubMed]
- England, J.R.; Cheng, P.M. Artificial intelligence for medical image analysis: A guide for authors and reviewers. Am. J. Roentgenol. 2019, 212, 513–519. [Google Scholar] [CrossRef]
- Khorasani, H.M.; Usefi, H.; Peña-Castillo, L. Detecting ulcerative colitis from colon samples using efficient feature selection and machine learning. Sci. Rep. 2020, 10, 13744. [Google Scholar] [CrossRef]
- Liu, X.; Rivera, S.C.; Moher, D.; Calvert, M.J.; Denniston, A.K. Reporting guidelines for clinical trial reports for interventions involving artificial intelligence: The CONSORT-AI extension. BJM 2020, 370, m3210. [Google Scholar]
- Cruz Rivera, S.; Liu, X.; Chan, A.W.; Calvert, M.J. Guidelines for clinical trial protocols for interventions involving artificial intelligence: The SPIRIT-AI extension. Nat. Med. 2020, 26, 1351–1363. [Google Scholar] [CrossRef]
- Cohen-Mekelburg, S.; Berry, S.; Stidham, R.W.; Zhu, J.; Waljee, A.K. Clinical applications of artificial intelligence and machine learning-based methods in inflammatory bowel disease. J. Gastroenterol. Hepatol. 2021, 36, 279–285. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Diaconu, C.; State, M.; Birligea, M.; Ifrim, M.; Bajdechi, G.; Georgescu, T.; Mateescu, B.; Voiosu, T. The Role of Artificial Intelligence in Monitoring Inflammatory Bowel Disease—The Future Is Now. Diagnostics 2023, 13, 735. https://doi.org/10.3390/diagnostics13040735
Diaconu C, State M, Birligea M, Ifrim M, Bajdechi G, Georgescu T, Mateescu B, Voiosu T. The Role of Artificial Intelligence in Monitoring Inflammatory Bowel Disease—The Future Is Now. Diagnostics. 2023; 13(4):735. https://doi.org/10.3390/diagnostics13040735
Chicago/Turabian StyleDiaconu, Claudia, Monica State, Mihaela Birligea, Madalina Ifrim, Georgiana Bajdechi, Teodora Georgescu, Bogdan Mateescu, and Theodor Voiosu. 2023. "The Role of Artificial Intelligence in Monitoring Inflammatory Bowel Disease—The Future Is Now" Diagnostics 13, no. 4: 735. https://doi.org/10.3390/diagnostics13040735
APA StyleDiaconu, C., State, M., Birligea, M., Ifrim, M., Bajdechi, G., Georgescu, T., Mateescu, B., & Voiosu, T. (2023). The Role of Artificial Intelligence in Monitoring Inflammatory Bowel Disease—The Future Is Now. Diagnostics, 13(4), 735. https://doi.org/10.3390/diagnostics13040735








