Control Level of Type 2 Diabetes Mellitus in the Elderly Is Associated with Polypharmacy, Accompanied Comorbidities, and Various Increased Risks According to the Beers Criteria
Abstract
:1. Introduction
2. Materials and Methods
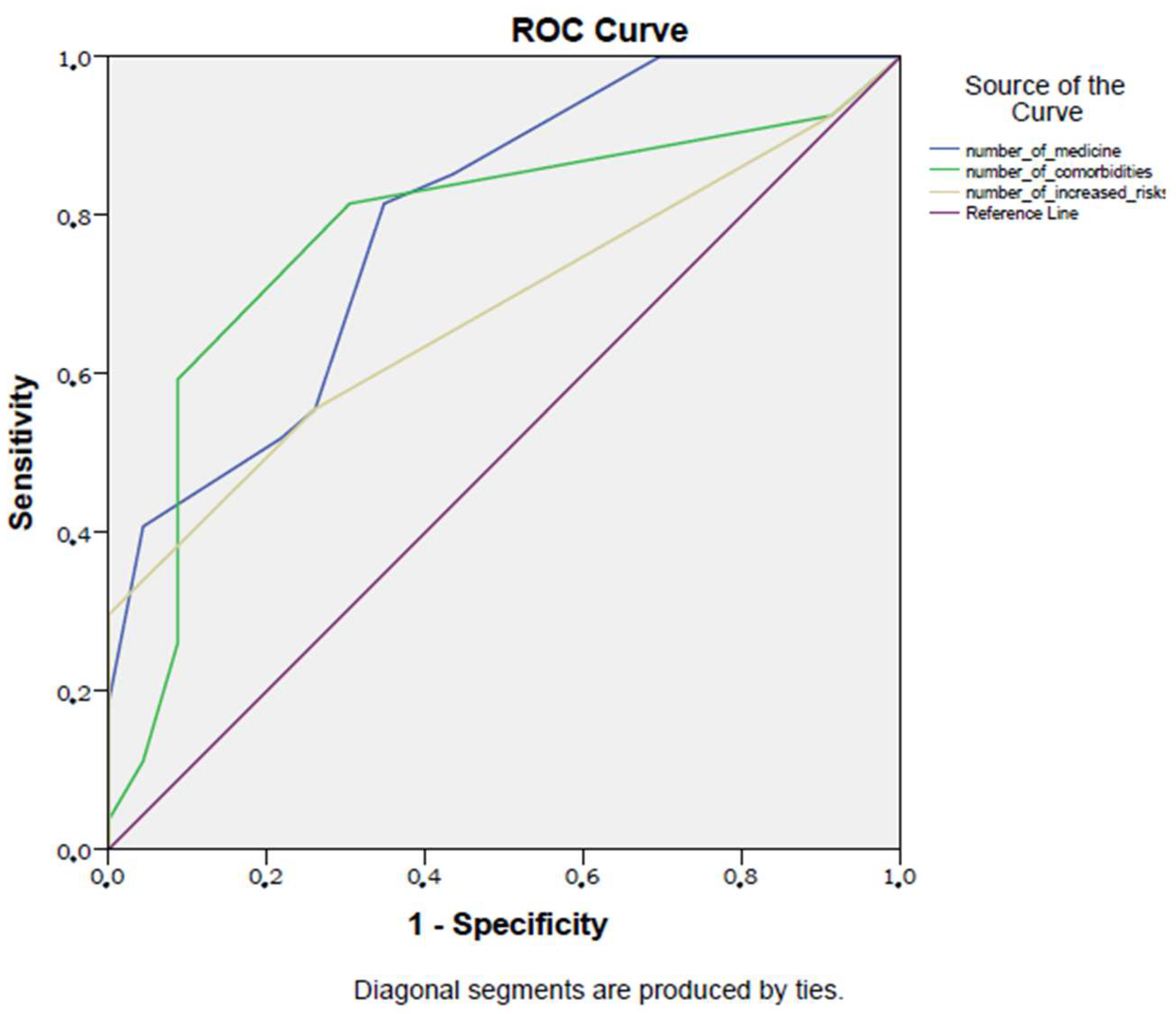
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kocak, M.Z.; Aktas, G.; Atak, B.M.; Duman, T.T.; Yis, O.M.; Erkus, E.; Savli, H. Is Neuregulin-4 a predictive marker of microvascular complications in type 2 diabetes mellitus? Eur. J. Clin. Investig. 2020, 50, e13206. [Google Scholar] [CrossRef] [PubMed]
- Fick, D.M.; Semla, T.P.; Steinman, M.; Beizer, J.; Brandt, N.; Dombrowski, R. American Geriatrics Society 2019 Updated AGS Beers Criteria® for Potentially Inappropriate Medication Use in Older Adults. J. Am. Geriatr. Soc. 2019, 67, 674–694. [Google Scholar] [CrossRef]
- Atak, B.M.; Aktas, G.; Duman, T.T.; Kurtkulagi, O.; Bilgin, S.; Kahveci, G.; Demirkol, M.E. Inappropriate medication use in older adults according to Beers Criteria in a Tertiary Referral Hospital, in Bolu, Turkey. Russ. Open Med. J. 2021, 10, e0211. [Google Scholar] [CrossRef]
- Horodinschi, R.N.; Stanescu, A.M.A.; Bratu, O.G.; Pantea Stoian, A.; Radavoi, D.G.; Diaconu, C.C. Treatment with Statins in Elderly Patients. Medicina 2019, 55, 721. [Google Scholar] [CrossRef] [PubMed]
- Borsheski, R.; Johnson, Q.L. Pain management in the geriatric population. Mo. Med. 2014, 111, 508–511. [Google Scholar]
- Chovatiya, R.; Silverberg, J.I. Iatrogenic Burden of Atopic Dermatitis. Dermatitis 2022, 33, S17–S23. [Google Scholar] [CrossRef] [PubMed]
- Vrdoljak, D.; Borovac, J.A. Medication in the elderly-considerations and therapy prescription guidelines. Acta Med. Acad. 2015, 44, 159–168. [Google Scholar] [CrossRef]
- Xu, X.; Mishra, G.D.; Jones, M. Evidence on multimorbidity from definition to intervention: An overview of systematic reviews. Ageing Res. Rev. 2017, 37, 53–68. [Google Scholar] [CrossRef]
- Lavan, A.H.; Gallagher, P.F.; O’Mahony, D. Methods to reduce prescribing errors in elderly patients with multimorbidity. Clin. Interv. Aging 2016, 11, 857–866. [Google Scholar] [CrossRef]
- Bowling, C.B.; Sloane, R.; Pieper, C.; Luciano, A.; Davis, B.R.; Simpson, L.M.; Einhorn, P.T.; Oparil, S.; Muntner, P. Association of Sustained Blood Pressure Control with Multimorbidity Progression Among Older Adults. J. Am. Geriatr. Soc. 2020, 68, 2059–2066. [Google Scholar] [CrossRef]
- Kurtkulagi, O.; Aktas, G.; Bilgin, S.; Meryem Atak, B.; Taslamacioglu Duman, T.; Emin Demirkol, M. Combined antihypertensive treatment is better than mono-therapy in hypertensive patients. Neth. J. Med. 2020, 78, 239–243. [Google Scholar] [PubMed]
- Perpétuo, C.; Plácido, A.I.; Rodrigues, D.; Aperta, J.; Piñeiro-Lamas, M.; Figueiras, A.; Herdeiro, M.T.; Roque, F. Prescription of Potentially Inappropriate Medication in Older Inpatients of an Internal Medicine Ward: Concordance and Overlap Among the EU(7)-PIM List and Beers and STOPP Criteria. Front. Pharm. 2021, 12, 676020. [Google Scholar] [CrossRef]
- Komiya, H.; Umegaki, H.; Asai, A.; Kanda, S.; Maeda, K.; Shimojima, T.; Nomura, H.; Kuzuya, M. Factors associated with polypharmacy in elderly home-care patients. Geriatr. Gerontol. Int. 2018, 18, 33–41. [Google Scholar] [CrossRef] [PubMed]
- Zaninotto, P.; Huang, Y.T.; Di Gessa, G.; Abell, J.; Lassale, C.; Steptoe, A. Polypharmacy is a risk factor for hospital admission due to a fall: Evidence from the English Longitudinal Study of Ageing. BMC Public Health 2020, 20, 1804. [Google Scholar] [CrossRef]
- McCracken, R.; McCormack, J.; McGregor, M.J.; Wong, S.T.; Garrison, S. Associations between polypharmacy and treatment intensity for hypertension and diabetes: A cross-sectional study of nursing home patients in British Columbia, Canada. BMJ Open 2017, 7, e017430. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.T.; Steptoe, A.; Wei, L.; Zaninotto, P. Polypharmacy difference between older people with and without diabetes: Evidence from the English longitudinal study of ageing. Diabetes Res. Clin. Pr. 2021, 176, 108842. [Google Scholar] [CrossRef]
- Coutinho, D.F.; de Figueiredo, R.C.; Duncan, B.B.; Schmidt, M.I.; Barreto, S.M.; Diniz, M. Association between control of diabetes mellitus and polypharmacy at the Brazilian Longitudinal Study of Adult Health (ELSA-Brasil). Pharmacoepidemiol. Drug Saf. 2021, 30, 749–757. [Google Scholar] [CrossRef]
- Remelli, F.; Ceresini, M.G.; Trevisan, C.; Noale, M.; Volpato, S. Prevalence and impact of polypharmacy in older patients with type 2 diabetes. Aging Clin. Exp. Res. 2022, 34, 1969–1983. [Google Scholar] [CrossRef]
- Alexandre, K.; Campbell, J.; Bugnon, M.; Henry, C.; Schaub, C.; Serex, M.; Elmers, J.; Desrichard, O.; Peytremann-Bridevaux, I. Factors influencing diabetes self-management in adults: An umbrella review of systematic reviews. JBI Evid. Synth. 2021, 19, 1003–1118. [Google Scholar] [CrossRef]
- Dobrică, E.C.; Găman, M.A.; Cozma, M.A.; Bratu, O.G.; Pantea Stoian, A.; Diaconu, C.C. Polypharmacy in Type 2 Diabetes Mellitus: Insights from an Internal Medicine Department. Medicina 2019, 55, 436. [Google Scholar] [CrossRef]
- Al-Musawe, L.; Torre, C.; Guerreiro, J.P.; Rodrigues, A.T.; Raposo, J.F.; Mota-Filipe, H.; Martins, A.P. Polypharmacy, potentially serious clinically relevant drug-drug interactions, and inappropriate medicines in elderly people with type 2 diabetes and their impact on quality of life. Pharm. Res. Perspect. 2020, 8, e00621. [Google Scholar] [CrossRef]
- Maher, R.L.; Hanlon, J.; Hajjar, E.R. Clinical consequences of polypharmacy in elderly. Expert Opin. Drug Saf. 2014, 13, 57–65. [Google Scholar] [CrossRef]
- Ikäheimo, I.; Karjalainen, M.; Tiihonen, M.; Haanpää, M.; Kautiainen, H.; Saltevo, J.; Mäntyselkä, P. Clinically relevant drug-drug interactions and the risk for drug adverse effects among home-dwelling older persons with and without type 2 diabetes. J. Clin. Pharm. 2019, 44, 735–741. [Google Scholar] [CrossRef]
- Curkendall, S.M.; Thomas, N.; Bell, K.F.; Juneau, P.L.; Weiss, A.J. Predictors of medication adherence in patients with type 2 diabetes mellitus. Curr. Med. Res. Opin. 2013, 29, 1275–1286. [Google Scholar] [CrossRef]
- Grant, R.W.; Devita, N.G.; Singer, D.E.; Meigs, J.B. Polypharmacy and medication adherence in patients with type 2 diabetes. Diabetes Care 2003, 26, 1408–1412. [Google Scholar] [CrossRef] [PubMed]
- García, A.L.; Villarreal, R.E.; Galicia, R.L.; Martínez, G.L.; Vargas, D.E. The cost of polypharmacy in patients with type 2 diabetes mellitus. Rev. Med. Chil. 2015, 143, 606–611. [Google Scholar] [CrossRef] [PubMed]
- Horii, T.; Atsuda, K. Effects of pharmacist intervention on polypharmacy in patients with type 2 diabetes in Japan. BMC Res. Notes 2020, 13, 183. [Google Scholar] [CrossRef] [PubMed]
- Srikanth, V.; Sinclair, A.J.; Hill-Briggs, F.; Moran, C.; Biessels, G.J. Type 2 diabetes and cognitive dysfunction-towards effective management of both comorbidities. Lancet Diabetes Endocrinol. 2020, 8, 535–545. [Google Scholar] [CrossRef] [PubMed]
- Bellary, S.; Kyrou, I.; Brown, J.E.; Bailey, C.J. Type 2 diabetes mellitus in older adults: Clinical considerations and management. Nat. Rev. Endocrinol. 2021, 17, 534–548. [Google Scholar] [CrossRef]
- Urina-Jassir, M.; Herrera-Parra, L.J.; Hernández Vargas, J.A.; Valbuena-García, A.M.; Acuña-Merchán, L.; Urina-Triana, M. The effect of comorbidities on glycemic control among Colombian adults with diabetes mellitus: A longitudinal approach with real-world data. BMC Endocr. Disord. 2021, 21, 128. [Google Scholar] [CrossRef]
- Fina Lubaki, J.P.; Omole, O.B.; Francis, J.M. Glycaemic control among type 2 diabetes patients in sub-Saharan Africa from 2012 to 2022: A systematic review and meta-analysis. Diabetol. Metab. Syndr. 2022, 14, 134. [Google Scholar] [CrossRef]
- Malecki, M.T. Genetics of type 2 diabetes mellitus. Diabetes Res. Clin. Pr. 2005, 68 (Suppl. S1), S10–S21. [Google Scholar] [CrossRef]
- Defronzo, R.A. From the triumvirate to the ominous octet: A new paradigm for the treatment of type 2 diabetes mellitus. Diabetes 2009, 58, 773–795. [Google Scholar] [CrossRef] [PubMed]
- Reach, G.; Pechtner, V.; Gentilella, R.; Corcos, A.; Ceriello, A. Clinical inertia and its impact on treatment intensification in people with type 2 diabetes mellitus. Diabetes Metab. 2017, 43, 501–511. [Google Scholar] [CrossRef] [PubMed]
- Halpern, A.; Mancini, M.C.; Magalhães, M.E.; Fisberg, M.; Radominski, R.; Bertolami, M.C.; Bertolami, A.; de Melo, M.E.; Zanella, M.T.; Queiroz, M.S.; et al. Metabolic syndrome, dyslipidemia, hypertension and type 2 diabetes in youth: From diagnosis to treatment. Diabetol. Metab. Syndr. 2010, 2, 55. [Google Scholar] [CrossRef] [PubMed]
- Szmuilowicz, E.D.; Aleppo, G. Stepwise approach to continuous glucose monitoring interpretation for internists and family physicians. Postgrad. Med. 2022, 134, 743–751. [Google Scholar] [CrossRef]
- Aktas, G.; Atak Tel, B.M.; Tel, R.; Balci, B. Treatment of type 2 diabetes patients with heart conditions. Expert Rev. Endocrinol. Metab. 2023, 18, 255–265. [Google Scholar] [CrossRef]
- Powell, P.W.; Corathers, S.D.; Raymond, J.; Streisand, R. New approaches to providing individualized diabetes care in the 21st century. Curr. Diabetes Rev. 2015, 11, 222–230. [Google Scholar] [CrossRef]
- Faselis, C.; Katsimardou, A.; Imprialos, K.; Deligkaris, P.; Kallistratos, M.; Dimitriadis, K. Microvascular Complications of Type 2 Diabetes Mellitus. Curr. Vasc. Pharm. 2020, 18, 117–124. [Google Scholar] [CrossRef]
- Velázquez-López, L.; Segura Cid Del Prado, P.; Colín-Ramírez, E.; Muñoz-Torres, A.V.; Escobedo-de la Peña, J. Adherence to non-pharmacological treatment is associated with the goals of cardiovascular control and better eating habits in Mexican patients with type 2 diabetes mellitus. Clin. Investig. Arter. 2022, 34, 88–96. [Google Scholar] [CrossRef]
- Shymko, G.; Grace, T.; Jolly, N.; Dobson, L.; Hacking, D.; Parmar, A.; Kapi, P.; Waters, F. Weight gain and metabolic screening in young people with early psychosis on long acting injectable antipsychotic medication (aripiprazole vs. paliperidone). Early Interv. Psychiatry 2021, 15, 787–793. [Google Scholar] [CrossRef] [PubMed]
- Lipska, K.J.; Huang, E.S.; Liu, J.Y.; Parker, M.M.; Laiteerapong, N.; Grant, R.W.; Moffet, H.H.; Karter, A.J. Glycemic control and diabetes complications across health status categories in older adults treated with insulin or insulin secretagogues: The Diabetes & Aging Study. J. Am. Geriatr. Soc. 2023. [Google Scholar] [CrossRef]
- Xu, H.; Garcia-Ptacek, S.; Trevisan, M.; Evans, M.; Lindholm, B.; Eriksdotter, M.; Carrero Pharm, J.J. Kidney Function, Kidney Function Decline, and the Risk of Dementia in Older Adults: A Registry-Based Study. Neurology 2021, 96, e2956–e2965. [Google Scholar] [CrossRef]
- Verhulst, C.E.M.; Fabricius, T.W.; Nefs, G.; Kessels, R.P.C.; Pouwer, F.; Teerenstra, S.; Tack, C.J.; Broadley, M.M.; Kristensen, P.L.; McCrimmon, R.J.; et al. Consistent Effects of Hypoglycemia on Cognitive Function in People With or Without Diabetes. Diabetes Care 2022, 45, 2103–2110. [Google Scholar] [CrossRef] [PubMed]
- Cuspidi, C.; Gherbesi, E.; Tadic, M. Diabetes and orthostatic hypotension: Are all patients created equal? J. Hypertens. 2023, 41, 1217–1218. [Google Scholar] [CrossRef]
- McCreight, L.J.; Bailey, C.J.; Pearson, E.R. Metformin and the gastrointestinal tract. Diabetologia 2016, 59, 426–435. [Google Scholar] [CrossRef]

| Well-Controlled T2DM (n = 23) | Poorly Controlled T2DM (n = 27) | p | ||
|---|---|---|---|---|
| Sex | Female (n, (%)) | 12 (52) | 15 (56) | 0.81 |
| Male (n, (%)) | 11 (48) | 12 (44) | ||
| Mean ± SD | ||||
| Age (years) | 78 ± 6 | 78 ± 6 | 0.23 | |
| WBC (k/mm3) | 7.9 ± 2.3 | 7.7 ± 1.9 | 0.76 | |
| Hb (g/dL) | 12.2 ± 1.9 | 12.4 ± 1.5 | 0.58 | |
| Plt (k/mm3) | 283 ± 98 | 271 ± 93 | 0.67 | |
| Median (min.-max.) | ||||
| AST (U/L) | 16 (8–40) | 15 (7–38) | 0.3 | |
| ALT (U/L | 14 (8–30) | 13 (7–34) | 0.37 | |
| HbA1c (%) | 6.9 (5.8–7.45) | 8.9 (7.67–13) | <0.001 | |
| Creatinine (mg/dL) | 1 (0.74–2.7) | 0.99 (0.69–2.3) | 0.42 | |
| eGFR (%) | 67 (15–88) | 64 (26–91) | 0.5 | |
| Fasting glucose (mg/dL) | 119 (96–168) | 121 (91–234) | 0.52 | |
| Well-Controlled T2DM (n = 23) | Poorly Controlled T2DM (n = 27) | p | |
|---|---|---|---|
| Number of daily medicines (n) | 4 (2–9) | 8 (4–13) | <0.001 |
| Number of comorbidities (n) | 2 (1–6) | 4 (1–7) | 0.001 |
| Number of increased risks according to the Beers Criteria (n) | 1 (0–2) | 2 (0–6) | 0.02 |
| Well-Controlled T2DM (n = 23) | Poorly Controlled T2DM (n = 27) | p | |
|---|---|---|---|
| Comorbidity (n (%)) | 1 (4.7%) | 2 (7.4%) | 0.65 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Atak Tel, B.M.; Aktas, G.; Bilgin, S.; Baltaci, S.B.; Taslamacioglu Duman, T. Control Level of Type 2 Diabetes Mellitus in the Elderly Is Associated with Polypharmacy, Accompanied Comorbidities, and Various Increased Risks According to the Beers Criteria. Diagnostics 2023, 13, 3433. https://doi.org/10.3390/diagnostics13223433
Atak Tel BM, Aktas G, Bilgin S, Baltaci SB, Taslamacioglu Duman T. Control Level of Type 2 Diabetes Mellitus in the Elderly Is Associated with Polypharmacy, Accompanied Comorbidities, and Various Increased Risks According to the Beers Criteria. Diagnostics. 2023; 13(22):3433. https://doi.org/10.3390/diagnostics13223433
Chicago/Turabian StyleAtak Tel, Burcin Meryem, Gulali Aktas, Satilmis Bilgin, Sumeyye Buse Baltaci, and Tuba Taslamacioglu Duman. 2023. "Control Level of Type 2 Diabetes Mellitus in the Elderly Is Associated with Polypharmacy, Accompanied Comorbidities, and Various Increased Risks According to the Beers Criteria" Diagnostics 13, no. 22: 3433. https://doi.org/10.3390/diagnostics13223433
APA StyleAtak Tel, B. M., Aktas, G., Bilgin, S., Baltaci, S. B., & Taslamacioglu Duman, T. (2023). Control Level of Type 2 Diabetes Mellitus in the Elderly Is Associated with Polypharmacy, Accompanied Comorbidities, and Various Increased Risks According to the Beers Criteria. Diagnostics, 13(22), 3433. https://doi.org/10.3390/diagnostics13223433








