Measuring Impairments of Mentalization with the 15-Item Mentalization Questionnaire (MZQ) and Introducing the MZQ-6 Short Scale: Reliability, Validity and Norm Values Based on a Representative Sample of the German Population
Abstract
1. Introduction
2. Materials and Methods
2.1. Sample and Setting
2.2. Measures
2.2.1. Mentalization Questionnaire (MZQ)
2.2.2. Personality Functioning—Operationalized Psychodynamic Diagnosis Structure Questionnaire-Short Form (OPD-SQS)
2.2.3. Symptoms of Depression and Anxiety (PHQ-4)
2.2.4. Profile of Mood States—POMS
2.3. Statistical Analyses
3. Results
3.1. Sample Characteristics
3.2. Acceptance
3.3. Psychometric Properties and Reliability
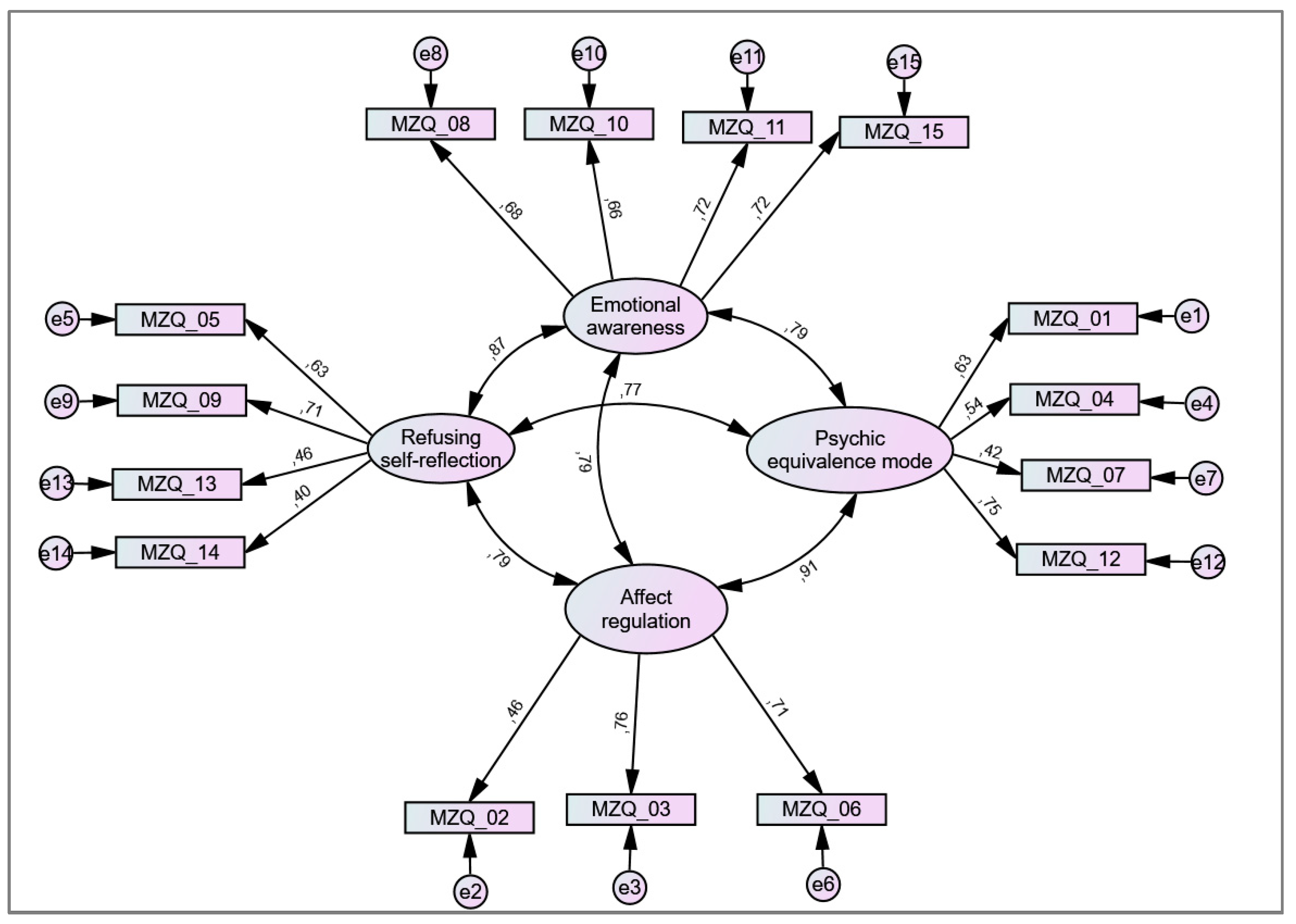
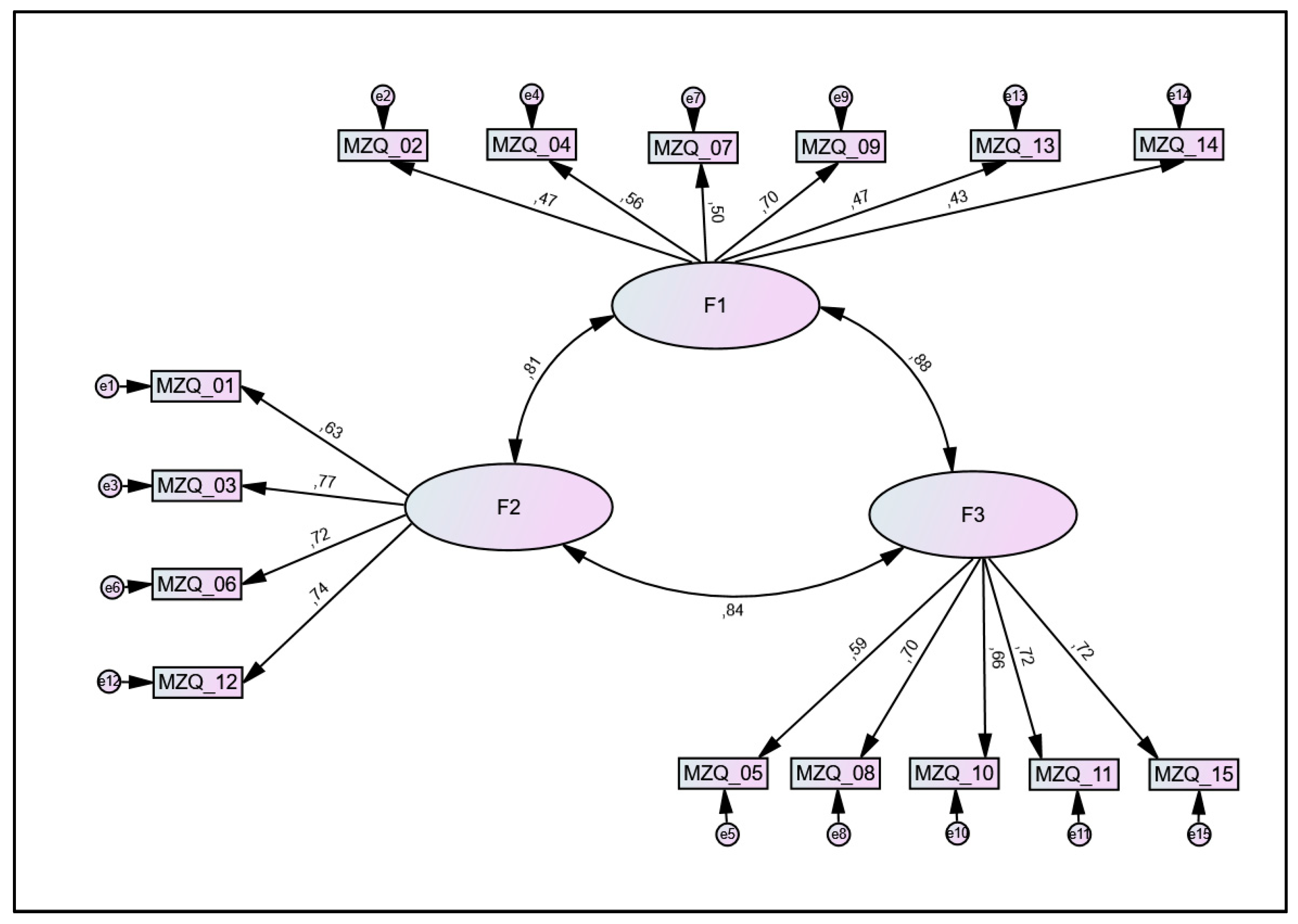
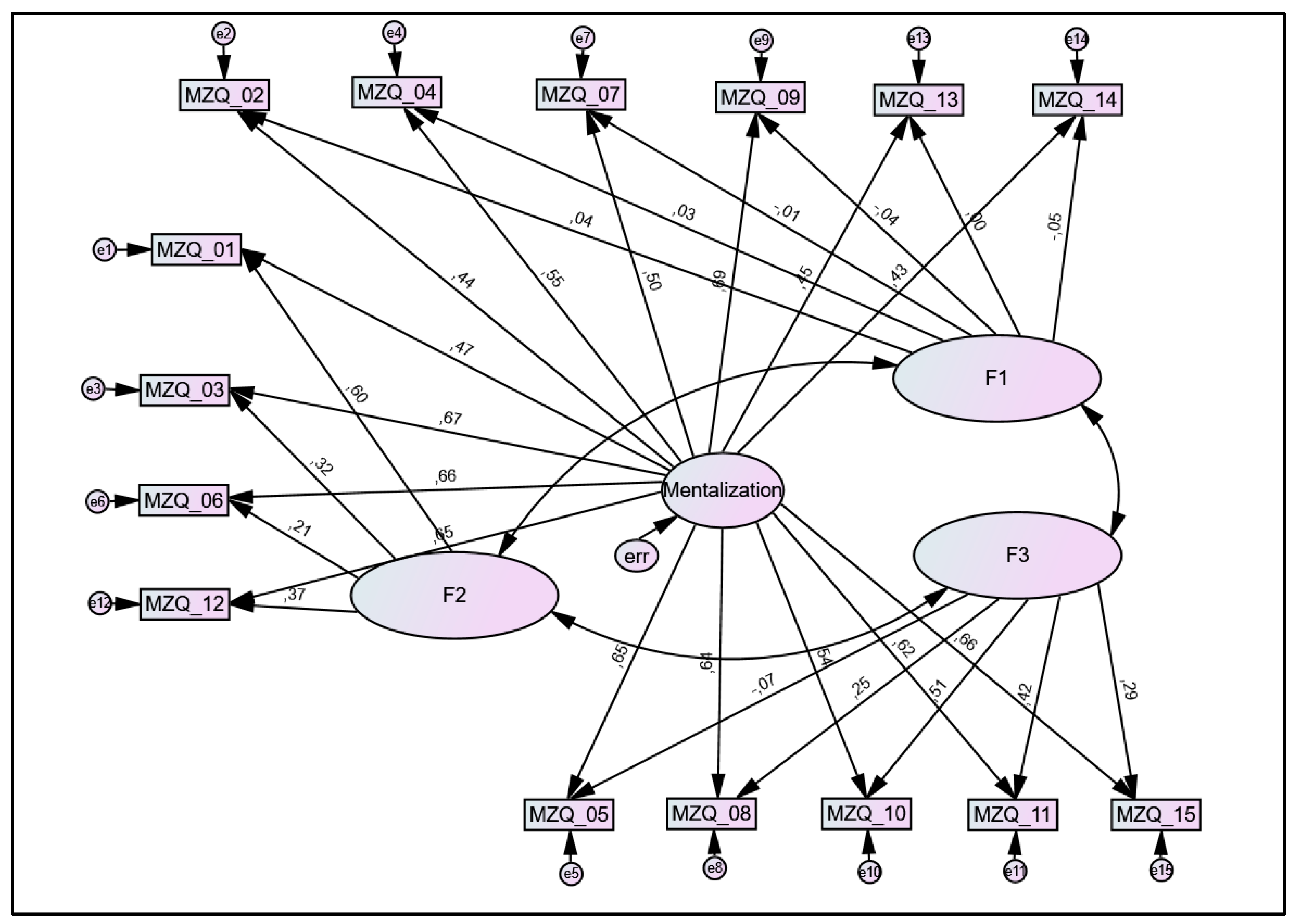
3.4. Factorial Validity
3.5. Dimensionality
3.6. Convergent Validity
3.7. Norm Values—Normed Means for Different Age Groups and Gender
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bateman, A.W.; Fonagy, P. The development of an attachment-based treatment program for borderline personality disorder. Bull. Menn. Clin. 2003, 67, 187–211. [Google Scholar] [CrossRef] [PubMed]
- Fonagy, P.; Bateman, A. The development of borderline personality disorder—A mentalizing model. J. Pers. Disord. 2008, 22, 4–21. [Google Scholar] [CrossRef]
- Fonagy, P.; Target, M.; Gergely, G.; Allen, J.G.; Bateman, A.W. The Developmental Roots of Borderline Personality Disorder in Early Attachment Relationships: A Theory and Some Evidence. Psychoanal. Inq. 2003, 23, 412–459. [Google Scholar] [CrossRef]
- Juul, S.; Simonsen, S.; Poulsen, S.; Lunn, S.; Sørensen, P.; Bateman, A.; Jakobsen, J.C. Detailed statistical analysis plan for the short-term versus long-term mentalisation-based therapy for outpatients with subthreshold or diagnosed borderline personality disorder randomised clinical trial (MBT-RCT). Trials 2021, 22, 497. [Google Scholar] [CrossRef] [PubMed]
- Weijers, J.; Ten Kate, C.; Viechtbauer, W.; Rampaart, L.J.A.; Eurelings, E.H.M.; Selten, J.P. Mentalization-based treatment for psychotic disorder: A rater-blinded, multi-center, randomized controlled trial. Psychol. Med. 2020, 51, 2846–2855. [Google Scholar] [CrossRef]
- Rossouw, T.I.; Fonagy, P. Mentalization-based treatment for self-harm in adolescents: A randomized controlled trial. J. Am. Acad. Child. Adolesc. Psychiatry 2012, 51, 1304–1313. [Google Scholar] [CrossRef]
- Hausberg, M.C.; Schulz, H.; Piegler, T.; Happach, C.G.; Klopper, M.; Brutt, A.L.; Sammet, I.; Andreas, S. Is a self-rated instrument appropriate to assess mentalization in patients with mental disorders? Development and first validation of the mentalization questionnaire (MZQ). Psychother. Res. J. Soc. Psychother. Res. 2012, 22, 699–709. [Google Scholar] [CrossRef]
- Fischer-Kern, M.; Fonagy, P.; Kapusta, N.D.; Luyten, P.; Boss, S.; Naderer, A.; Blüml, V.; Leithner, K. Mentalizing in female inpatients with major depressive disorder. J. Nerv. Ment. Dis. 2013, 201, 202–207. [Google Scholar] [CrossRef] [PubMed]
- Taubner, S.; Kessler, H.; Buchheim, A.; Kächele, H.; Staun, L. The role of mentalization in the psychoanalytic treatment of chronic depression. Psychiatry 2011, 74, 49–57. [Google Scholar] [CrossRef]
- Fischer-Kern, M.; Tmej, A. Mentalization and Depression: Theoretical Concepts, Treatment Approaches and Empirical Studies—An Overview. Z. Psychosom. Med. Psychother. 2019, 65, 162–177. [Google Scholar] [CrossRef]
- Huang, Y.L.; Fonagy, P.; Feigenbaum, J.; Montague, P.R.; Nolte, T. Multidirectional Pathways between Attachment, Mentalizing, and Posttraumatic Stress Symptomatology in the Context of Childhood Trauma. Psychopathology 2020, 53, 48–58. [Google Scholar] [CrossRef] [PubMed]
- Brent, B. Mentalization-based psychodynamic psychotherapy for psychosis. J. Clin. Psychol. 2009, 65, 803–814. [Google Scholar] [CrossRef]
- MaBeth, A.; Gumley, A.; Schwannauer, M.; Fisher, R. Attachment states of mind, mentalization, and their correlates in a first-episode psychosis sample. Psychol. Psychother. 2011, 84, 42–57, discussion 98–110. [Google Scholar] [CrossRef] [PubMed]
- Fekete, K.; Torok, E.; Kelemen, O.; Makkos, Z.; Csigo, K.; Keri, S. Dimensions of mentalization in psychotic disorders. Neuropsychopharmacol. Hung. 2019, 21, 5–11. [Google Scholar] [PubMed]
- Savov, S.; Atanassov, N. Deficits of affect mentalization in patients with drug addiction: Theoretical and clinical aspects. ISRN Addict. 2013, 2013, 250751. [Google Scholar] [CrossRef] [PubMed]
- Innamorati, M.; Imperatori, C.; Harnic, D.; Erbuto, D.; Patitucci, E.; Janiri, L.; Lamis, D.A.; Pompili, M.; Tamburello, S.; Fabbricatore, M. Emotion Regulation and Mentalization in People at Risk for Food Addiction. Behav. Med. 2017, 43, 21–30. [Google Scholar] [CrossRef]
- Cate, R.; Khademi, M.; Judd, P.; Miller, H. Deficits in mentalization: A risk factor for future development of eating disorders among pre-adolescent girls. Adv. Eat. Disord. 2013, 1, 187–194. [Google Scholar] [CrossRef]
- Skårderud, F. Eating one’s words, part I: ‘Concretised metaphors’ and reflective function in anorexia nervosa—An interview study. Eur. Eat. Disord. Rev. 2007, 15, 163–174. [Google Scholar] [CrossRef]
- Dimaggio, G.; Carcione, A.; Salvatore, G.; Nicolò, G.; Sisto, A.; Semerari, A. Progressively promoting metacognition in a case of obsessive-compulsive personality disorder treated with metacognitive interpersonal therapy. Psychol. Psychother. 2011, 84, 70–83. [Google Scholar] [CrossRef]
- Fonagy, P.; Target, M. Playing with reality: I. Theory of mind and the normal development of psychic reality. Int. J. Psychoanal. 1996, 77 Pt 2, 217–233. [Google Scholar]
- Fonagy, P.; Gergely, G.; Jurist, E.L. Affect Regulation, Mentalization and the Development of the Self, 1st ed.; Fonagy, P., Gergely, G., Jurist, E.L., Eds.; Routledge: London, UK, 2019. [Google Scholar]
- Fonagy, P.; Target, M. Early Intervention and the Development of Self-Regulation. Psychoanal. Inq. 2002, 22, 307–335. [Google Scholar] [CrossRef]
- Probst, T.; Dehoust, M.; Brütt, A.L.; Schulz, H.; Pieh, C.; Andreas, S. Mentalization and Self-Efficacy as Mediators between Psychological Symptom Severity and Disabilities in Activities and Participation in Psychotherapy Patients. Psychopathology 2018, 51, 38–46. [Google Scholar] [CrossRef] [PubMed]
- Wagner-Skacel, J.; Riedl, D.; Kampling, H.; Lampe, A. Mentalization and dissociation after adverse childhood experiences. Sci. Rep. 2022, 12, 6809. [Google Scholar] [CrossRef]
- Freier, A.; Kruse, J.; Schmalbach, B.; Zara, S.; Werner, S.; Brähler, E.; Fegert, J.M.; Kampling, H. The mediation effect of personality functioning between different types of child maltreatment and the development of depression/anxiety symptoms—A German representative study. J. Affect. Disord. 2022, 299, 408–415. [Google Scholar] [CrossRef]
- Li, M.; D’Arcy, C.; Meng, X. Maltreatment in childhood substantially increases the risk of adult depression and anxiety in prospective cohort studies: Systematic review, meta-analysis, and proportional attributable fractions. Psychol. Med. 2016, 46, 717–730. [Google Scholar] [CrossRef] [PubMed]
- Fonagy, P.; Target, M.; Steele, M.; Steele, H. The Reflective-Functioning Manual, Version 4.1 for Application to Adult Attachment Interviews; University of London: London, UK, 1997; Unpublished Manuscript. [Google Scholar]
- Ehrenthal, J.C.; Dinger, U.; Schauenburg, H.; Horsch, L.; Dahlbender, R.W.; Gierk, B. Development of a 12-item version of the OPD-Structure Questionnaire (OPD-SQS). Z. Psychosom. Med. Psychother. 2015, 61, 262–274. [Google Scholar] [CrossRef] [PubMed]
- Ehrenthal, J.; Kruse, J.; Schmalbach, B.; Dinger, U.; Werner, S.; Schauenburg, H. Measuring personality functioning with the 12-item version of the OPD-Structure Questionnaire (OPD-SQS): Reliability, factor structure, validity, and measurement invariance in the general population. under review.
- Ehrenthal, J.C.; Dinger, U.; Horsch, L.; Komo-Lang, M.; Klinkerfuss, M.; Grande, T.; Schauenburg, H. The OPD Structure Questionnaire (OPD-SQ): First results on reliability and validity. Psychother. Psychosom. Med. Psychol. 2012, 62, 25–32. [Google Scholar] [CrossRef] [PubMed]
- Obbarius, A.; Obbarius, N.; Fischer, F.; Liegl, G.; Rose, M. Evaluation of Factor Structure and Construct Validity of the 12-Item Short Version of the OPD Structure Questionnaire (OPD-SQS) in Psychosomatic Patients. Psychother. Psychosom. Med. Psychol. 2019, 69, 38–48. [Google Scholar] [CrossRef]
- Löwe, B.; Wahl, I.; Rose, M.; Spitzer, C.; Glaesmer, H.; Wingenfeld, K.; Schneider, A.; Brähler, E. A 4-item measure of depression and anxiety: Validation and standardization of the Patient Health Questionnaire-4 (PHQ-4) in the general population. J. Affect. Disord. 2010, 122, 86–95. [Google Scholar] [CrossRef]
- Wicke, F.S.; Krakau, L.; Löwe, B.; Beutel, M.E.; Brähler, E. Update of the standardization of the Patient Health Questionnaire-4 (PHQ-4) in the general population. J. Affect. Disord. 2022, 312, 310–314. [Google Scholar] [CrossRef]
- McNair, D.; Lorr, M.; Droppleman, L. Manual for the Profile of Mood States; Educational and Industrial Testing Services: San Diego, CA, USA, 1971. [Google Scholar]
- Petrowski, K.; Albani, C.; Zenger, M.; Brähler, E.; Schmalbach, B. Revised Short Screening Version of the Profile of Mood States (POMS) From the German General Population. Front. Psychol. 2021, 12, 631668. [Google Scholar] [CrossRef] [PubMed]
- DeVellis, R.F. Scale Development: Theory and Applications; Sage: Los Angeles, CA, USA, 2012. [Google Scholar]
- O’Connor, B.P. SPSS and SAS programs for determining the number of components using parallel analysis and velicer’s MAP test. Behav. Res. Methods Instrum. Comput. 2000, 32, 396–402. [Google Scholar] [CrossRef]
- Dueber, D.M. Bifactor Indices Calculator: A Microsoft Excel-Based Tool to Calculate Various Indices Relevant to Bifactor CFA Models. Available online: http://sites.education.uky.edu/apslab/resources/ (accessed on 28 July 2021).
- Luyten, P.; Campbell, C.; Allison, E.; Fonagy, P. The Mentalizing Approach to Psychopathology: State of the Art and Future Directions. Annu. Rev. Clin. Psychol. 2020, 16, 297–325. [Google Scholar] [CrossRef] [PubMed]
- Zettl, M.; Volkert, J.; Vögele, C.; Herpertz, S.C.; Kubera, K.M.; Taubner, S. Mentalization and criterion a of the alternative model for personality disorders: Results from a clinical and nonclinical sample. Personal. Disord. 2020, 11, 191–201. [Google Scholar] [CrossRef] [PubMed]
- Nazzaro, M.P.; Boldrini, T.; Tanzilli, A.; Muzi, L.; Giovanardi, G.; Lingiardi, V. Does reflective functioning mediate the relationship between attachment and personality? Psychiatry Res. 2017, 256, 169–175. [Google Scholar] [CrossRef] [PubMed]
- Antonsen, B.T.; Johansen, M.S.; Rø, F.G.; Kvarstein, E.H.; Wilberg, T. Is reflective functioning associated with clinical symptoms and long-term course in patients with personality disorders? Compr. Psychiatry 2016, 64, 46–58. [Google Scholar] [CrossRef] [PubMed]
- Fischer-Kern, M.; Buchheim, A.; Hörz, S.; Schuster, P.; Doering, S.; Kapusta, N.D.; Taubner, S.; Tmej, A.; Rentrop, M.; Buchheim, P.; et al. The relationship between personality organization, reflective functioning, and psychiatric classification in borderline personality disorder. Psychoanal. Psychol. 2010, 27, 395–409. [Google Scholar] [CrossRef]
- Müller, C.; Kaufhold, J.; Overbeck, G.; Grabhorn, R. The importance of reflective functioning to the diagnosis of psychic structure. Psychol. Psychother. 2006, 79, 485–494. [Google Scholar] [CrossRef]
- Beebe, B.; Jaffe, J.; Markese, S.; Buck, K.; Chen, H.; Cohen, P.; Bahrick, L.; Andrews, H.; Feldstein, S. The origins of 12-month attachment: A microanalysis of 4-month mother-infant interaction. Attach. Hum. Dev. 2010, 12, 3–141. [Google Scholar] [CrossRef]
- Kernberg, O. Severe Personality Disorders: Psychotherapeutic Strategies; Yale University Press: New Haven, CT, USA, 1986. [Google Scholar]
- Kernberg, O.F. A psychoanalytic classification of character pathology. J. Am. Psychoanal. Assoc. 1970, 18, 800–822. [Google Scholar] [CrossRef]
- Krakau, L.; Tibubos, A.N.; Beutel, M.E.; Ehrenthal, J.C.; Gieler, U.; Brähler, E. Personality functioning as a mediator of adult mental health following child maltreatment. J. Affect. Disord. 2021, 291, 126–134. [Google Scholar] [CrossRef] [PubMed]
- Ernst, M.; Brähler, E.; Kampling, H.; Kruse, J.; Fegert, J.M.; Plener, P.L.; Beutel, M.E. Is the end in the beginning? Child maltreatment increases the risk of non-suicidal self-injury and suicide attempts through impaired personality functioning. Child Abus. Negl. 2022, 133, 105870. [Google Scholar] [CrossRef]
- Nolte, T.; Guiney, J.; Fonagy, P.; Mayes, L.C.; Luyten, P. Interpersonal stress regulation and the development of anxiety disorders: An attachment-based developmental framework. Front. Behav. Neurosci. 2011, 5, 55. [Google Scholar] [CrossRef] [PubMed]
- Luyten, P.; Fonagy, P. The stress-reward-mentalizing model of depression: An integrative developmental cascade approach to child and adolescent depressive disorder based on the Research Domain Criteria (RDoC) approach. Clin. Psychol. Rev. 2018, 64, 87–98. [Google Scholar] [CrossRef] [PubMed]
- Fonagy, P.; Luyten, P.; Allison, E. Epistemic Petrification and the Restoration of Epistemic Trust: A New Conceptualization of Borderline Personality Disorder and Its Psychosocial Treatment. J. Pers. Disord. 2015, 29, 575–609. [Google Scholar] [CrossRef]
- Fonagy, P.; Luyten, P.; Allison, E.; Campbell, C. What we have changed our minds about: Part 2. Borderline personality disorder, epistemic trust and the developmental significance of social communication. Bord. Personal. Disord. Emot. Dysregul. 2017, 4, 9. [Google Scholar] [CrossRef]
- Müller, S.; Wendt, L.P.; Zimmermann, J. Development and Validation of the Certainty About Mental States Questionnaire (CAMSQ): A Self-Report Measure of Mentalizing Oneself and Others. Assessment 2021, 10731911211061280. [Google Scholar] [CrossRef]
| n | (%) | |
|---|---|---|
| Sex | ||
| male | 1165 | (46.8) |
| female | 1321 | (53.1) |
| diverse | 1 | (0.04) |
| Age | (M = 46.0; SD = 17.8) | |
| <30 | 613 | (24.6) |
| 30–39 | 358 | (14.4) |
| 40–49 | 369 | (14.8) |
| 50–59 | 527 | (21.2) |
| 60–69 | 381 | (15.3) |
| ≥70 | 239 | (9.6) |
| Education | ||
| no qualification | 58 | (2.3) |
| general school | 505 | (20.3) |
| secondary school | 1005 | (40.4) |
| technical college/high school | 476 | (19.1) |
| university education | 360 | (14.5) |
| other | 76 | (3.1) |
| missing | 7 | (0.3) |
| Relationship | ||
| married | 1041 | (41.9) |
| single | 988 | (39.7) |
| divorced | 293 | (11.8) |
| widowed | 149 | (6.0) |
| missing | 16 | (0.6) |
| Employment status | ||
| full time | 1063 | (42.7) |
| part time | 407 | (16.4) |
| unemployed | 219 | (8.8) |
| in training | 249 | (10.0) |
| retired | 503 | (20.2) |
| missing | 46 | (1.8) |
| Monthly net household income | ||
| <1500 EUR | 699 | (28.1) |
| 1500–2499 EUR | 584 | (23.5) |
| 2500–3499 EUR | 534 | (21.5) |
| ≥3500 EUR | 670 | (26.9) |
| Reliability | Factor Loading | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| No | Item | M | SD | ITC | ω | EFA | CFA b | CFA c | IECV |
| Factor 1: Mental states in oneself regarding others— cognition and communication | 2.4 | 0.7 | - | 0.69 | |||||
| 2 | Explanations from others are of little assistance in understanding my feelings. | 2.6 | 1.1 | 0.44 | 0.43 | 0.47 | 0.45 | 0.96 | |
| 4 a | I only believe that someone really likes me a lot if I have enough realistic proof for it (e.g., a date, a gift or a hug). | 2.5 | 1.3 | 0.52 | 0.55 | 0.56 | 0.52 | 0.96 | |
| 7 | It’s difficult for me to believe that relationships can change. | 2.4 | 1.1 | 0.45 | 0.54 | 0.51 | 0.44 | 0.99 | |
| 9 a | Talking about feelings would mean that they become more and more powerful | 2.1 | 1.1 | 0.62 | 0.64 | 0.70 | 0.65 | 1.00 | |
| 13 | If someone yawns in my presence, that’s a reliable sign that he is bored in my company | 2.0 | 1.1 | 0.41 | 0.47 | 0.47 | 0.43 | 1.00 | |
| 14 | Most of the time I don’t feel like talking about my thoughts and feelings with others | 2.8 | 1.2 | 0.38 | 0.46 | 0.44 | 0.35 | 0.93 | |
| Factor 2: Mental states regarding oneself— affect-regulation | 2.2 | 0.9 | 0.80 | ||||||
| 1 | If I expect to be criticized or offended, my fear increases more and more | 2.5 | 1.2 | 0.51 | 0.74 | 0.58 | 0.55 | 0.49 | |
| 3 | Sometimes feelings are dangerous for me | 2.1 | 1.1 | 0.66 | 0.71 | 0.77 | 0.68 | 0.55 | |
| 6 a | Often, I can’t control my feelings | 2.1 | 1.1 | 0.62 | 0.61 | 0.74 | 0.66 | 0.67 | |
| 12 a | Often, I feel threatened by the idea that someone could criticize or offend me | 2.2 | 1.1 | 0.66 | 0.71 | 0.71 | 0.68 | 0.78 | |
| Factor 3: Mental states regarding oneself— affect-perception and -differentiation | 2.3 | 0.8 | 0.79 | ||||||
| 5 | Most of the time it is better not to feel anything | 2.2 | 1.1 | 0.57 | 0.47 | 0.61 | 0.59 | 1.00 | |
| 8 | I tend to ignore feelings of physical tension or of discomfort until they compel my full attention | 2.3 | 1.1 | 0.62 | 0.66 | 0.69 | 0.64 | 0.95 | |
| 10 | Sometimes I only become aware of my feelings in retrospect | 2.7 | 1.1 | 0.56 | 0.74 | 0.62 | 0.60 | 0.85 | |
| 11 a | Frequently it’s difficult for me to perceive my feelings at their full intensity | 2.3 | 1.1 | 0.62 | 0.76 | 0.68 | 0.66 | 0.90 | |
| 15 a | Often, I don’t even know what is happening inside of me | 2.0 | 1.0 | 0.65 | 0.68 | 0.72 | 0.70 | 0.48 | |
| OPD SQS Total Score | OPD SQS Self-Perception | OPD SQS Contact | OPD SQS Relationship | |
|---|---|---|---|---|
| MZQ-6 | 0.71 *** | 0.69 *** | 0.60 *** | 0.54 *** |
| MZQ-15 | 0.73 *** | 0.67 *** | 0.60 *** | 0.60 *** |
| POMS Dejection | POMS Vigor | POMS Fatigue | POMS Anger | PHQ-4 | |
|---|---|---|---|---|---|
| MZQ-6 total score | 0.46 *** | −0.11 *** | 0.35 *** | 0.36 *** | 0.45 *** |
| MZQ-15 total score | 0.46 *** | −0.22 *** | 0.35 *** | 0.36 *** | 0.45 *** |
| MZQ-15 Total Score | MZQ-6 Total Score | |||||
|---|---|---|---|---|---|---|
| Age | Sex | n | Mean | (SD) | Mean | (SD) |
| <30 | M | 306 | 34.5 | (9.55) | 14.0 | (4.29) |
| F | 306 | 37.8 | (10.39) | 14.8 | (5.13) | |
| 30–39 | M | 163 | 34.9 | (10.69) | 13.1 | (4.62) |
| F | 196 | 35.6 | (10.89) | 13.9 | (5.14) | |
| 40–49 | M | 181 | 34.5 | (10.41) | 12.9 | (4.54) |
| F | 188 | 34.4 | (10.70) | 12.8 | (4.81) | |
| 50–59 | M | 242 | 34.6 | (9.56) | 12.9 | (4.24) |
| F | 286 | 33.0 | (10.18) | 12.1 | (4.50) | |
| 60–69 | M | 175 | 31.8 | (8.57) | 12.0 | (3.96) |
| F | 206 | 33.6 | (9.94) | 12.5 | (4.50) | |
| ≥70 | M | 98 | 33.6 | (9.64) | 12.6 | (4.38) |
| F | 140 | 35.2 | (9.76) | 13.0 | (4.65) | |
| Total sample | M | 1165 | 34.6 | (9.8) | 13.1 | (4.37) |
| F | 1322 | 35.0 | (10.46) | 13.3 | (4.90) | |
| total | 2488 | 34.8 | (10.17) | 13.2 | (4.66) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Riedl, D.; Kampling, H.; Nolte, T.; Lampe, A.; Beutel, M.E.; Brähler, E.; Kruse, J. Measuring Impairments of Mentalization with the 15-Item Mentalization Questionnaire (MZQ) and Introducing the MZQ-6 Short Scale: Reliability, Validity and Norm Values Based on a Representative Sample of the German Population. Diagnostics 2023, 13, 135. https://doi.org/10.3390/diagnostics13010135
Riedl D, Kampling H, Nolte T, Lampe A, Beutel ME, Brähler E, Kruse J. Measuring Impairments of Mentalization with the 15-Item Mentalization Questionnaire (MZQ) and Introducing the MZQ-6 Short Scale: Reliability, Validity and Norm Values Based on a Representative Sample of the German Population. Diagnostics. 2023; 13(1):135. https://doi.org/10.3390/diagnostics13010135
Chicago/Turabian StyleRiedl, David, Hanna Kampling, Tobias Nolte, Astrid Lampe, Manfred E. Beutel, Elmar Brähler, and Johannes Kruse. 2023. "Measuring Impairments of Mentalization with the 15-Item Mentalization Questionnaire (MZQ) and Introducing the MZQ-6 Short Scale: Reliability, Validity and Norm Values Based on a Representative Sample of the German Population" Diagnostics 13, no. 1: 135. https://doi.org/10.3390/diagnostics13010135
APA StyleRiedl, D., Kampling, H., Nolte, T., Lampe, A., Beutel, M. E., Brähler, E., & Kruse, J. (2023). Measuring Impairments of Mentalization with the 15-Item Mentalization Questionnaire (MZQ) and Introducing the MZQ-6 Short Scale: Reliability, Validity and Norm Values Based on a Representative Sample of the German Population. Diagnostics, 13(1), 135. https://doi.org/10.3390/diagnostics13010135







