Balance Remains Impaired after Hip Arthroplasty: A Systematic Review and Best Evidence Synthesis
Abstract
1. Introduction
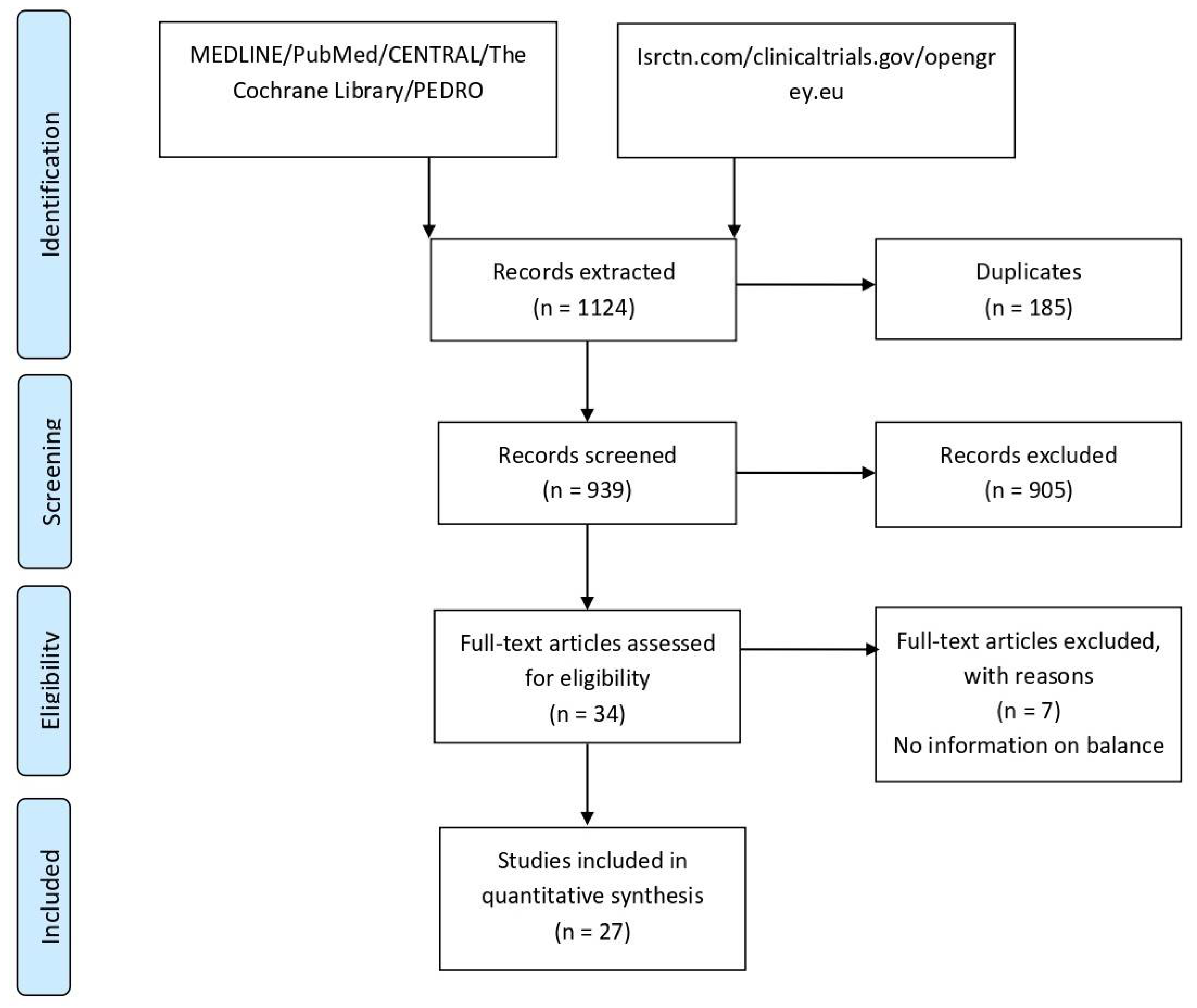
2. Methods
2.1. Source of Data and Data Extraction
2.2. Risk of Bias Assessment and Best-Evidence Synthesis
- Strong evidence, if a result was reported by two or more studies with low risk of bias and with findings that were, overall, at least 75% consistent across studies.
- Moderate evidence, if a result was reported by one study with low risk of bias and by two or more studies with moderate/high risk of bias, or if it was reported by two or more studies with moderate/high risk of bias and with findings that were, overall, at least 75% consistent across papers.
- Limited evidence, if a result was reported by one or more studies with moderate/high risk of bias, or if it was reported by one study with low risk of bias study and with findings that were, overall, at least 75% consistent across papers.
- Conflicting evidence, with conflicting findings (<75% of the studies reporting consistent findings).
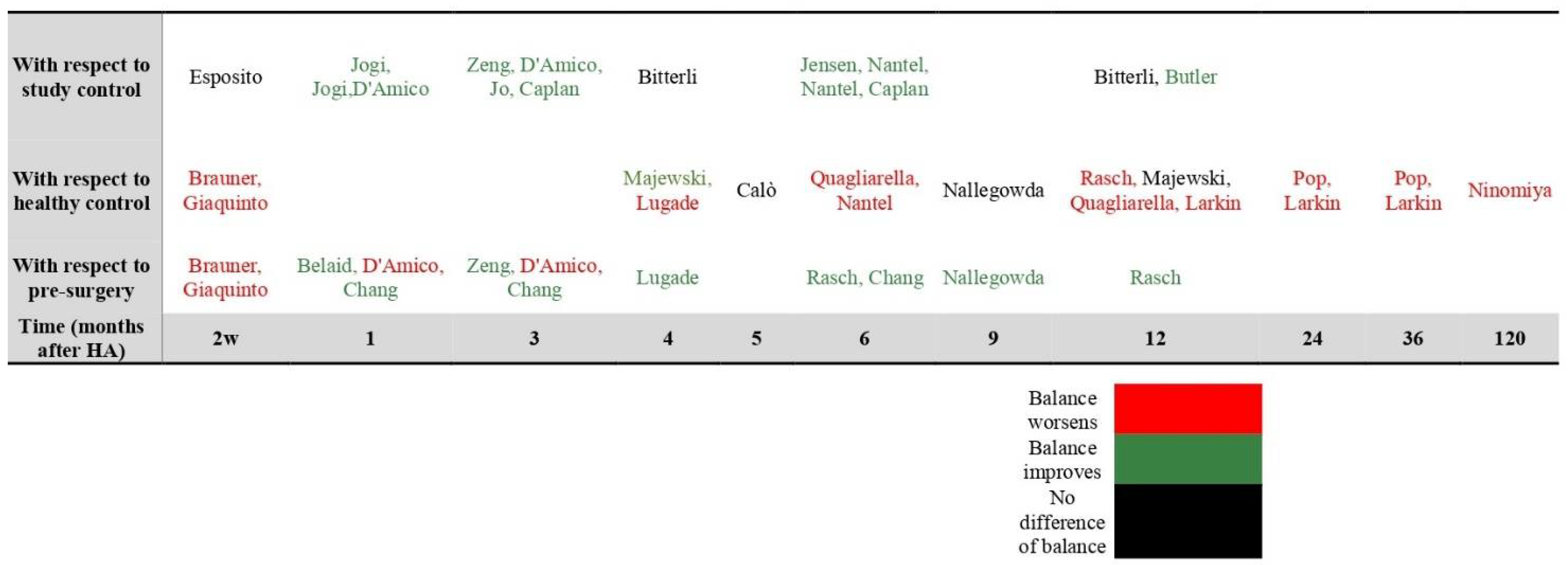
3. Results
3.1. Characteristics of the Included Studies
3.2. Risk of Bias and Best-Evidence Assessment
3.2.1. Treatment-Related Changes
3.2.2. Pre-Operative Risk Factors
3.2.3. Surgical Risk Factors
3.2.4. Post-Operative Risk Factors
4. Discussion
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Learmonth, I.D.; Young, C.; Rorabeck, C. The operation of the century: Total hip replacement. Lancet 2007, 370, 1508–1519. [Google Scholar] [CrossRef]
- Courpied, J.-P.; Caton, J.H. Total Hip Arthroplasty, State of the Art for the 21st Century; Springer: Berlin/Heidelberg, Germany, 2011. [Google Scholar]
- Fuller, G.F. Falls in the elderly. Am. Fam. Physician 2000, 61, 2159–2168. [Google Scholar] [PubMed]
- Bergen, G.; Stevens, M.R.; Burns, E.R. Falls and Fall Injuries Among Adults Aged ≥65 Years-United States, 2014. MMWR Morb. Mortal. Wkly. Rep. 2016, 65, 993–998. [Google Scholar] [CrossRef] [PubMed]
- Spaniolas, K.; Cheng, J.D.; Gestring, M.L.; Sangosanya, A.; Stassen, N.A.; Bankey, P.E. Ground level falls are associated with significant mortality in elderly patients. J. Trauma 2010, 69, 821–825. [Google Scholar] [CrossRef] [PubMed]
- MacKinnon, C.D. Sensorimotor anatomy of gait, balance, and falls. Handb. Clin. Neurol. 2018, 159, 3–26. [Google Scholar] [CrossRef]
- Hurley, M.V.; Scott, D.L.; Rees, J.; Newham, D.J. Sensorimotor changes and functional performance in patients with knee osteoarthritis. Ann. Rheum. Dis. 1997, 56, 641–648. [Google Scholar] [CrossRef]
- Marks, R. Osteoarthritis and Proprioception: What Does the Literature Reveal? Int. J. Orthop. 2017, 4, 826–836. [Google Scholar] [CrossRef]
- Mahomed, N.N.; Barrett, J.A.; Katz, J.N.; Phillips, C.B.; Losina, E.; Lew, R.A.; Guadagnoli, E.; Harris, W.H.; Poss, R.; Baron, J.A. Rates and outcomes of primary and revision total hip replacement in the United States medicare population. JBJS 2003, 85, 27–32. [Google Scholar] [CrossRef]
- Nallegowda, M.; Singh, U.; Bhan, S.; Wadhwa, S.; Handa, G.; Dwivedi, S. Balance and gait in total hip replacement: A pilot study. Am. J. Phys. Med. Rehabil. 2003, 82, 669–677. [Google Scholar] [CrossRef]
- Majewski, M.; Bischoff-Ferrari, H.; Grüneberg, C.; Dick, W.; Allum, J. Improvements in balance after total hip replacement. J. Bone Jt. Surg. Bre. 2005, 87, 1337–1343. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Ann. Intern. Med. 2009, 151, 264–269. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.; Altman, D.G.; Gøtzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D.; Savović, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef] [PubMed]
- Eijgenraam, S.M.; Reijman, M.; Bierma-Zeinstra, S.M.; Van Yperen, D.T.; Meuffels, D.E. Can we predict the clinical outcome of arthroscopic partial meniscectomy? A systematic review. Br. J. Sports Med. 2018, 52, 514–521. [Google Scholar] [CrossRef] [PubMed]
- Furlan, A.D.; Malmivaara, A.; Chou, R.; Maher, C.G.; Deyo, R.A.; Schoene, M.; Bronfort, G.; Van Tulder, M.W. 2015 updated method guideline for systematic reviews in the Cochrane Back and Neck Group. Spine 2015, 40, 1660–1673. [Google Scholar] [CrossRef] [PubMed]
- Kiss, R.M.; Illyes, A. Comparison of gait parameters in patients following total hip arthroplasty with a direct-lateral or antero-lateral surgical approach. Hum. Mov. Sci. 2012, 31, 1302–1316. [Google Scholar] [CrossRef] [PubMed]
- Butler, R.J.; Ruberte Thiele, R.A.; Barnes, C.L.; Bolognesi, M.P.; Queen, R.M. Unipedal balance is affected by lower extremity joint arthroplasty procedure 1 year following surgery. J. Arthroplast. 2015, 30, 286–289. [Google Scholar] [CrossRef]
- Pop, T.; Szymczyk, D.; Majewska, J.; Bejer, A.; Baran, J.; Bielecki, A.; Rusek, W. The Assessment of Static Balance in Patients after Total Hip Replacement in the Period of 2-3 Years after Surgery. BioMed Res. Int. 2018, 2018, 3707254. [Google Scholar] [CrossRef] [PubMed]
- Bitterli, R.; Sieben, J.M.; Hartmann, M.; de Bruin, E.D. Pre-surgical sensorimotor training for patients undergoing total hip replacement: A randomised controlled trial. Int. J. Sports Med. 2011, 32, 725–732. [Google Scholar] [CrossRef]
- Nantel, J.; Termoz, N.; Ganapathi, M.; Vendittoli, P.A.; Lavigne, M.; Prince, F. Postural balance during quiet standing in patients with total hip arthroplasty with large diameter femoral head and surface replacement arthroplasty. Arch. Phys. Med. Rehabil. 2009, 90, 1607–1612. [Google Scholar] [CrossRef]
- Nantel, J.; Termoz, N.; Vendittoli, P.A.; Lavigne, M.; Prince, F. Gait patterns after total hip arthroplasty and surface replacement arthroplasty. Arch. Phys. Med. Rehabil. 2009, 90, 463–469. [Google Scholar] [CrossRef]
- Larkin, B.; Nyazee, H.; Motley, J.; Nunley, R.M.; Clohisy, J.C.; Barrack, R.L. Hip resurfacing does not improve proprioception compared with THA. Clin. Orthop. Relat. Res. 2014, 472, 555–561. [Google Scholar] [CrossRef] [PubMed]
- Caplan, N.; Stewart, S.; Kashyap, S.; Banaszkiewicz, P.; St Clair Gibson, A.; Kader, D.; Ewen, A. The effect of total hip and hip resurfacing arthroplasty on vertical ground reaction force and impulse symmetry during a sit-to-stand task. Clin. Biomech. 2014, 29, 1164–1169. [Google Scholar] [CrossRef] [PubMed]
- Jensen, C.; Rosenlund, S.; Nielsen, D.B.; Overgaard, S.; Holsgaard-Larsen, A. The use of the Gait Deviation Index for the evaluation of participants following total hip arthroplasty: An explorative randomized trial. Gait Posture 2015, 42, 36–41. [Google Scholar] [CrossRef] [PubMed]
- Holnapy, G.; Kiss, R.M. Impact of the method of exposure in total hip arthroplasty on balancing ability in response to sudden unidirectional perturbation in the first six months of the postoperative period. J. Electromyogr. Kinesiol. Off. J. Int. Soc. Electrophysiol. Kinesiol. 2013, 23, 727–733. [Google Scholar] [CrossRef][Green Version]
- Chang, C.J.; Lin, N.L.; Lee, M.S.; Chern, J.S. Recovery of Posture Stability at Different Foot Placements in Patients Who Underwent Minimally Invasive Total Hip Arthroplasty: A One-Year Follow-Up Study. BioMed Res. Int. 2015, 2015, 463792. [Google Scholar] [CrossRef]
- Esposito, F.; Freddolini, M.; Latella, L.; Braccio, P.; Marcucci, M.; Corvi, A. The influence of the crutch setup on stability and weight-bearing parameters in post total hip replacement surgery patients during quiet standing. Disabil. Rehabil. Assist. Technol. 2018, 13, 373–378. [Google Scholar] [CrossRef]
- D’Amico, M.; Ciarrocca, F.; Liscio, G.; Serafini, P.; Tommasini, M.; Vallasciani, M. Balance lower limb loads and 3D spine modifications after total hip joint replacement: Effects of leg length discrepancy correction. Stud. Health Technol. Inform. 2006, 123, 409–414. [Google Scholar]
- John, S.; Weizel, D.; Heumann, A.S.; Fischer, A.; Orlowski, K.; Mrkor, K.U.; Edelmann-Nusser, J.; Witte, K. Persisting inter-limb differences in patients following total hip arthroplasty four to five years after surgery? A preliminary cross-sectional study. BMC Musculoskelet. Disord. 2021, 22, 230. [Google Scholar] [CrossRef]
- Kannus, P.; Parkkari, J.; Koskinen, S.; Niemi, S.; Palvanen, M.; Järvinen, M.; Vuori, I. Fall-induced injuries and deaths among older adults. JAMA 1999, 281, 1895–1899. [Google Scholar] [CrossRef]
- Arnold, C.M.; Faulkner, R.A. The history of falls and the association of the timed up and go test to falls and near-falls in older adults with hip osteoarthritis. BMC Geriatr. 2007, 7, 17. [Google Scholar] [CrossRef]
- Ikutomo, H.; Nagai, K.; Nakagawa, N.; Masuhara, K. Falls in patients after total hip arthroplasty in Japan. J. Orthop. Sci. 2015, 20, 663–668. [Google Scholar] [CrossRef] [PubMed]
- Ikutomo, H.; Nagai, K.; Tagomori, K.; Miura, N.; Nakagawa, N.; Masuhara, K. Gait abnormality predicts falls in women after total hip arthroplasty. J. Arthroplast. 2018, 33, 3215–3219. [Google Scholar] [CrossRef] [PubMed]
- Jørgensen, C.C.; Kehlet, H.; Hip, L.F.C.f.F.-t.; Group, K.R.C. Fall-related admissions after fast-track total hip and knee arthroplasty–cause of concern or consequence of success? Clin. Interv. Aging 2013, 8, 1569. [Google Scholar] [CrossRef] [PubMed]
- Girard, J.; Lavigne, M.; Vendittoli, P.-A.; Roy, A. Biomechanical reconstruction of the hip: A randomised study comparing total hip resurfacing and total hip arthroplasty. J. Bone Jt. Surg. Br. 2006, 88, 721–726. [Google Scholar] [CrossRef] [PubMed]
- Loughead, J.; Chesney, D.; Holland, J.; McCaskie, A. Comparison of offset in Birmingham hip resurfacing and hybrid total hip arthroplasty. J. Bone Jt. Surg. Br. Vol. 2005, 87, 163–166. [Google Scholar] [CrossRef] [PubMed]
- Amstutz, H.C.; Grigoris, P.; Dorey, F.J. Evolution and future of surface replacement of the hip. J. Orthop. Sci. 1998, 3, 169–186. [Google Scholar] [CrossRef] [PubMed]
- Mont, M.A.; Seyler, T.M.; Ulrich, S.D.; Beaule, P.E.; Boyd, H.S.; Grecula, M.J.; Goldberg, V.M.; Kennedy, W.R.; Marker, D.R.; Schmalzried, T.P.; et al. Effect of changing indications and techniques on total hip resurfacing. Clin. Orthop. Relat. Res. 2007, 465, 63–70. [Google Scholar] [CrossRef] [PubMed]
- Amstutz, H.C.; Le Duff, M.J.; Johnson, A.J. Socket position determines hip resurfacing 10-year survivorship. Clin. Orthop. Relat. Res. 2012, 470, 3127–3133. [Google Scholar] [CrossRef]
- Amstutz, H.C.; Le Duff, M.J.; Campbell, P.A.; Wisk, L.E.; Takamura, K.M. Complications after metal-on-metal hip resurfacing arthroplasty. Orthop. Clin. N. Am. 2011, 42, 207–230. [Google Scholar] [CrossRef]
- Calo, L.; Rabini, A.; Picciotti, P.M.; Laurino, S.; Passali, G.C.; Ferrara, P.E.; Maggi, L.; Piazzini, D.B.; Specchia, A.; Frasca, G.; et al. Postural control in patients with total hip replacement. Eur. J. Phys. Rehabil. Med. 2009, 45, 327–334. [Google Scholar]
- Zeng, R.; Lin, J.; Wu, S.; Chen, L.; Chen, S.; Gao, H.; Zheng, Y.; Ma, H. A randomized controlled trial: Preoperative home-based combined Tai Chi and Strength Training (TCST) to improve balance and aerobic capacity in patients with total hip arthroplasty (THA). Arch. Gerontol. Geriatr. 2015, 60, 265–271. [Google Scholar] [CrossRef] [PubMed]
- Rasch, A.; Dalen, N.; Berg, H.E. Muscle strength, gait, and balance in 20 patients with hip osteoarthritis followed for 2 years after THA. Acta Orthop. 2010, 81, 183–188. [Google Scholar] [CrossRef] [PubMed]
- Jogi, P.; Overend, T.J.; Spaulding, S.J.; Zecevic, A.; Kramer, J.F. Effectiveness of balance exercises in the acute post-operative phase following total hip and knee arthroplasty: A randomized clinical trial. SAGE Open Med. 2015, 3, 2050312115570769. [Google Scholar] [CrossRef] [PubMed]
- Jogi, P.; Zecevic, A.; Overend, T.J.; Spaulding, S.J.; Kramer, J.F. Force-plate analyses of balance following a balance exercise program during acute post-operative phase in individuals with total hip and knee arthroplasty: A randomized clinical trial. SAGE Open Med. 2016, 4, 2050312116675097. [Google Scholar] [CrossRef] [PubMed]
- Masui, T.; Hasegawa, Y.; Matsuyama, Y.; Sakano, S.; Kawasaki, M.; Suzuki, S. Gender differences in platform measures of balance in rural community-dwelling elders. Arch. Gerontol. Geriatr. 2005, 41, 201–209. [Google Scholar] [CrossRef] [PubMed]

| Predictor | Significant Association (Level of Evidence) | No Significant Association | Level of Evidence |
|---|---|---|---|
| Exercise before THA | Bitterli (L) | limited | |
| Strength and ROM exercise post THA | Nantel (L), Calò (M), Nantel (M), Rasch (L), Brauner (M), Joji (M), Joji (M), Zeng (M), Pop (L) | strong | |
| BMI | Kiss (L), Butler (M) | limited | |
| Balance exercise post surgery | Joji (M), Joji (M) | moderate | |
| Set-up crutch | Esposito (L) | limited | |
| Surgical approach | Kiss(L) Holnapy (L) Chang (L) | conflictual | |
| Female | Pop (L) | limited | |
| Type of intervention | Natel (M), Natel (L), Larkin (L), Caplan (L), Jensen (L) | strong | |
| Proprioception | Nallegowda (M), Jo (M), Larkin (L) | conflictual |
| Author | Year | Risk of Bias |
|---|---|---|
| Nallegowda | 2003 | moderate |
| Majewski | 2005 | low |
| D’Amico | 2006 | moderate |
| Giaquinto | 2006 | moderate |
| Belaid | 2007 | moderate |
| Nantel | 2007 | low |
| Lugade | 2008 | moderate |
| Calò | 2009 | low |
| Nantel | 2009 | moderate |
| Quagliarella | 2010 | low |
| Rasch | 2010 | low |
| Bitterli | 2011 | low |
| Kiss | 2012 | low |
| Holnapy | 2013 | low |
| Larkin | 2013 | low |
| Brauner | 2014 | moderate |
| Caplan | 2014 | low |
| Jogi | 2014 | moderate |
| Butler | 2015 | moderate |
| Chang | 2015 | low |
| Jensen | 2015 | low |
| Jogi | 2015 | moderate |
| Zeng | 2015 | moderate |
| Jo | 2016 | moderate |
| Esposito | 2017 | moderate |
| Ninomiya | 2017 | low |
| Pop | 2018 | low |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Di Laura Frattura, G.; Bordoni, V.; Feltri, P.; Fusco, A.; Candrian, C.; Filardo, G. Balance Remains Impaired after Hip Arthroplasty: A Systematic Review and Best Evidence Synthesis. Diagnostics 2022, 12, 684. https://doi.org/10.3390/diagnostics12030684
Di Laura Frattura G, Bordoni V, Feltri P, Fusco A, Candrian C, Filardo G. Balance Remains Impaired after Hip Arthroplasty: A Systematic Review and Best Evidence Synthesis. Diagnostics. 2022; 12(3):684. https://doi.org/10.3390/diagnostics12030684
Chicago/Turabian StyleDi Laura Frattura, Giorgio, Vittorio Bordoni, Pietro Feltri, Augusto Fusco, Christian Candrian, and Giuseppe Filardo. 2022. "Balance Remains Impaired after Hip Arthroplasty: A Systematic Review and Best Evidence Synthesis" Diagnostics 12, no. 3: 684. https://doi.org/10.3390/diagnostics12030684
APA StyleDi Laura Frattura, G., Bordoni, V., Feltri, P., Fusco, A., Candrian, C., & Filardo, G. (2022). Balance Remains Impaired after Hip Arthroplasty: A Systematic Review and Best Evidence Synthesis. Diagnostics, 12(3), 684. https://doi.org/10.3390/diagnostics12030684







