Osteo-Proliferative Lesions of the Phalanges on Radiography: Associations with Sex, Age, and Osteoarthritis
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients and Sample Size Estimation
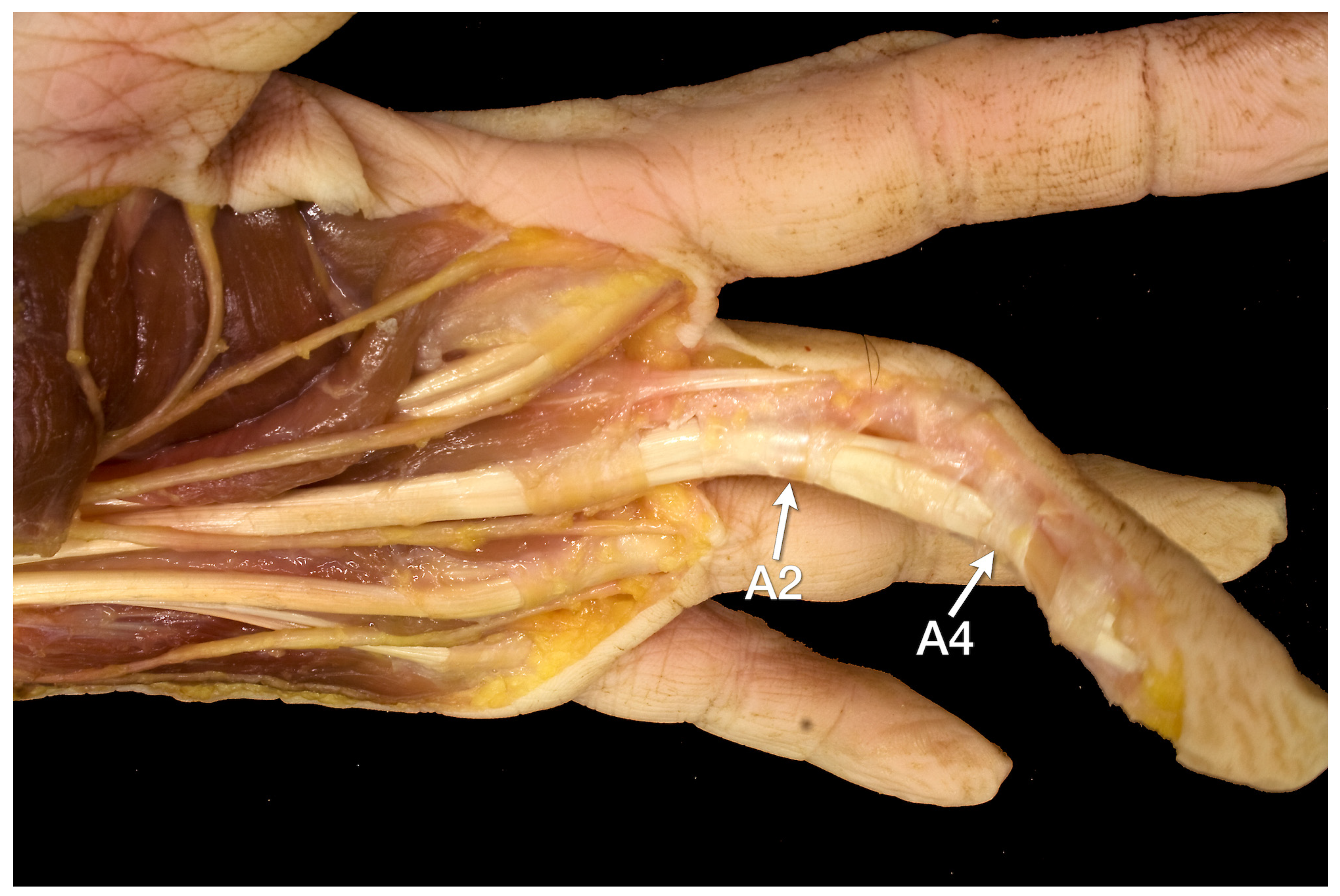
2.2. Anatomical Studies
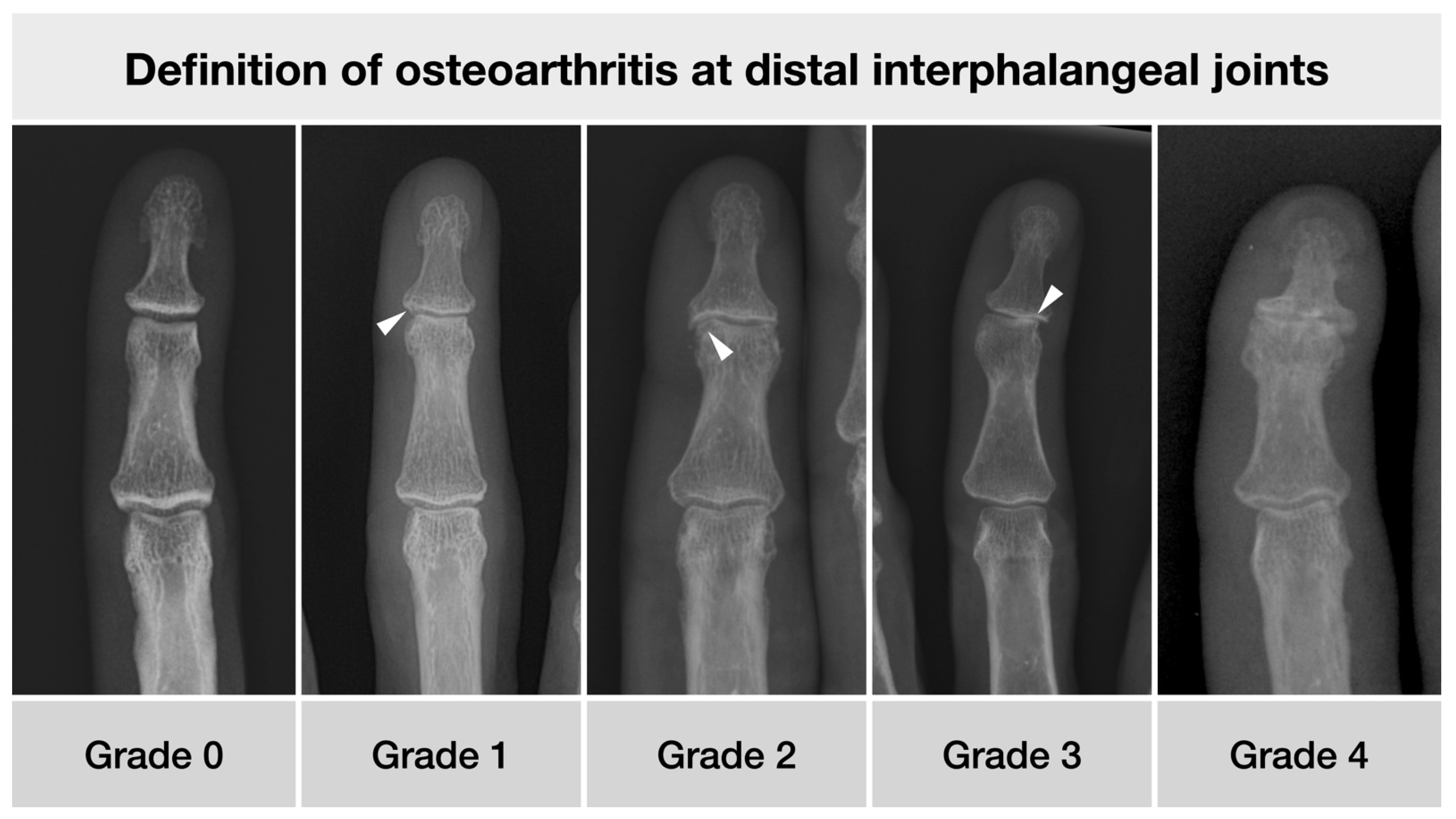
2.3. Imaging and Scoring System
2.4. Statistical Analysis
3. Results
3.1. Patients
3.2. Osteoarthritis
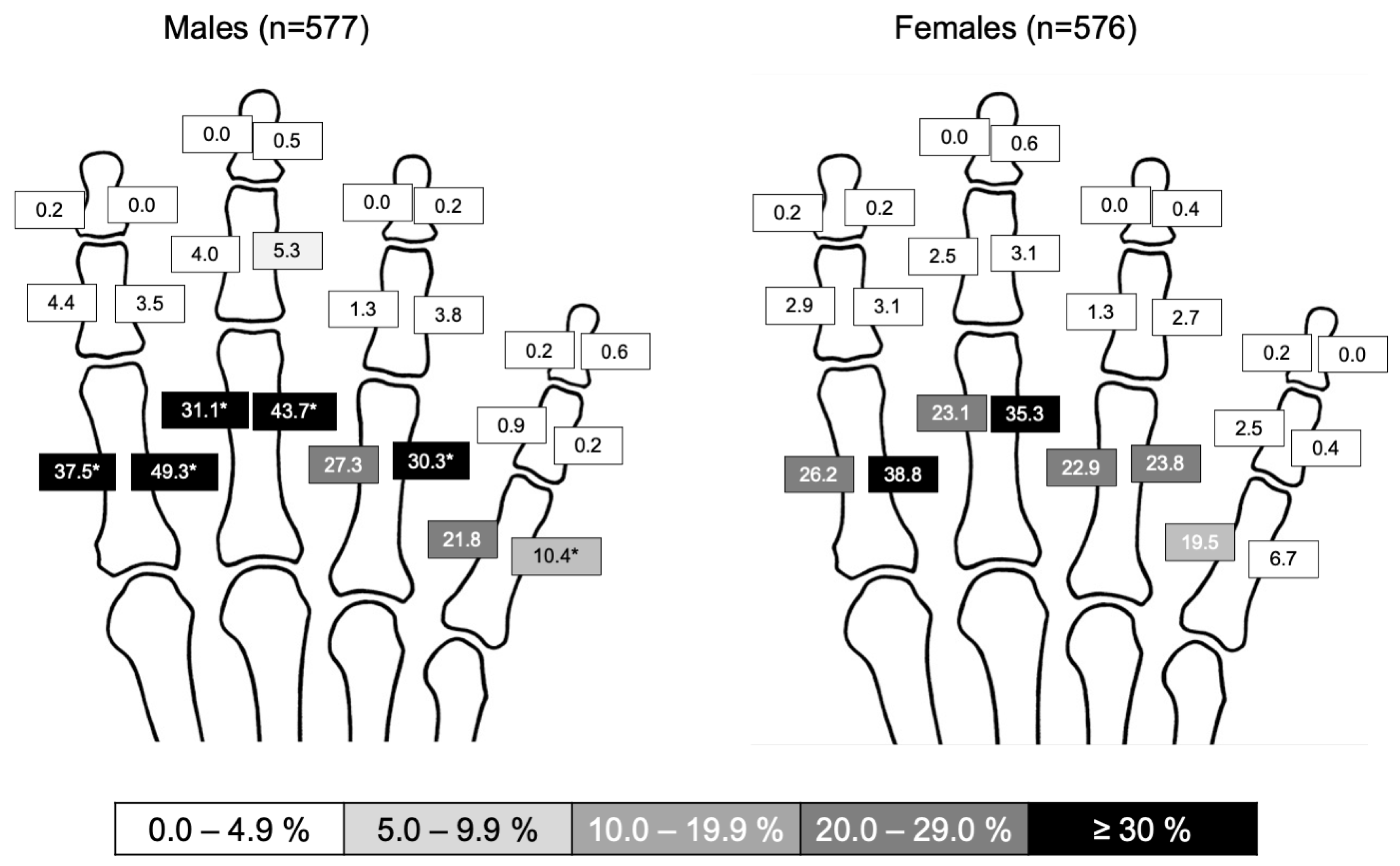
3.3. Periosteal Lesions
3.4. Inter-Reader Agreement
4. Discussion
4.1. Anatomical Considerations
4.2. Psoriatic Arthritis
4.3. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Murphy, W.A., Jr. Introduction to the history of musculoskeletal radiology. Radiographics 1990, 10, 915–943. [Google Scholar] [CrossRef]
- Spinnato, P. Imaging in Musculoskeletal Oncology. Curr. Med. Imaging 2021, 17, 155–156. [Google Scholar] [CrossRef] [PubMed]
- Ritchlin, C.T.; Colbert, R.A.; Gladman, D.D. Psoriatic Arthritis. N. Engl. J. Med. 2017, 376, 957–970. [Google Scholar] [CrossRef]
- Baraliakos, X.; Kleyer, A.; Simon, D.; Kohm, M.; Ohrndorf, S.; Sewerin, P. Imaging of psoriatic arthritis and aspects of radiographic progression. Z. Rheumatol. 2020, 79, 40–52. [Google Scholar] [CrossRef] [PubMed]
- Felbo, S.K.; Terslev, L.; Ostergaard, M. Imaging in peripheral and axial psoriatic arthritis: Contributions to diagnosis, follow-up, prognosis and knowledge of pathogenesis. Clin. Exp. Rheumatol. 2018, 36 (Suppl. 114), 24–34. [Google Scholar] [PubMed]
- Taylor, W.; Gladman, D.; Helliwell, P.; Marchesoni, A.; Mease, P.; Mielants, H.; Group, C.S. Classification criteria for psoriatic arthritis: Development of new criteria from a large international study. Arthritis Rheum. 2006, 54, 2665–2673. [Google Scholar] [CrossRef] [PubMed]
- Eshed, I.; Bollow, M.; McGonagle, D.G.; Tan, A.L.; Althoff, C.E.; Asbach, P.; Hermann, K.G. MRI of enthesitis of the appendicular skeleton in spondyloarthritis. Ann. Rheum. Dis. 2007, 66, 1553–1559. [Google Scholar] [CrossRef] [PubMed]
- Simon, D.; Faustini, F.; Kleyer, A.; Haschka, J.; Englbrecht, M.; Kraus, S.; Hueber, A.J.; Kocijan, R.; Sticherling, M.; Schett, G.; et al. Analysis of periarticular bone changes in patients with cutaneous psoriasis without associated psoriatic arthritis. Ann. Rheum. Dis. 2016, 75, 660–666. [Google Scholar] [CrossRef] [PubMed]
- Salaffi, F.; Carotti, M.; Beci, G.; Di Carlo, M.; Giovagnoni, A. Radiographic scoring methods in rheumatoid arthritis and psoriatic arthritis. Radiol. Med. 2019, 124, 1071–1086. [Google Scholar] [CrossRef] [PubMed]
- Pavlovsky, O.; Kobyliansky, E. Population Biology of Human Aging; Angelo Pontecorboli Press: Florence, Italy, 1999. [Google Scholar]
- Kalichman, L.; Malkin, I.; Kobyliansky, E. Osseographic Score as a Biomarker of Biological Aging. In Biennal Book of EAA ‘Ageing Related Problems in Past and Present Populations’; European Anthropological Association: Castel Gandolfo, Italy, 2008; Volume 5, pp. 103–117. [Google Scholar]
- Karasik, D.; Hannan, M.T.; Cupples, L.A.; Felson, D.T.; Kiel, D.P. Genetic contribution to biological aging: The Framingham Study. J. Gerontol. A Biol. Sci. Med. Sci. 2004, 59, 218–226. [Google Scholar] [CrossRef] [PubMed]
- Kellgren, J.H.; Lawrence, J.S. Radiological assessment of osteo-arthrosis. Ann. Rheum. Dis. 1957, 16, 494–502. [Google Scholar] [CrossRef]
- Kalichman, L.; Malkin, I.; Kobyliansky, E. Hand bone midshaft enthesophytes: The influence of age, sex, and heritability. Osteoarthr. Cartil. 2007, 15, 1113–1119. [Google Scholar] [CrossRef][Green Version]
- Leyk, D.; Gorges, W.; Ridder, D.; Wunderlich, M.; Ruther, T.; Sievert, A.; Essfeld, D. Hand-grip strength of young men, women and highly trained female athletes. Eur. J. Appl. Physiol. 2007, 99, 415–421. [Google Scholar] [CrossRef]
- Valenzuela, M.; Varacallo, M. Anatomy, Shoulder and Upper Limb, Hand Lumbrical Muscles; StatPearls Publishing LLC: Treasure Island, FL, USA, 2020. [Google Scholar]
- Meng, J.; Willekens, I.; Cattrysse, E.; Vereecke, E.; Geers, C.; Van Cauteren, T.; de Mey, J.; De Maeseneer, M. Bony palmar ridges of the phalanges of the human fingers. Surg. Radiol. Anat. 2014, 36, 587–593. [Google Scholar] [CrossRef] [PubMed]
- Benjamin, M.; McGonagle, D. Entheses: Tendon and ligament attachment sites. Scand. J. Med. Sci. Sports 2009, 19, 520–527. [Google Scholar] [CrossRef] [PubMed]
- Eshed, I.; Hermann, K.A.; Zejden, A.; Sudol-Szopinska, I. Imaging to Differentiate the Various Forms of Seronegative Arthritis. Semin. Musculoskelet. Radiol. 2018, 22, 189–196. [Google Scholar] [CrossRef] [PubMed]
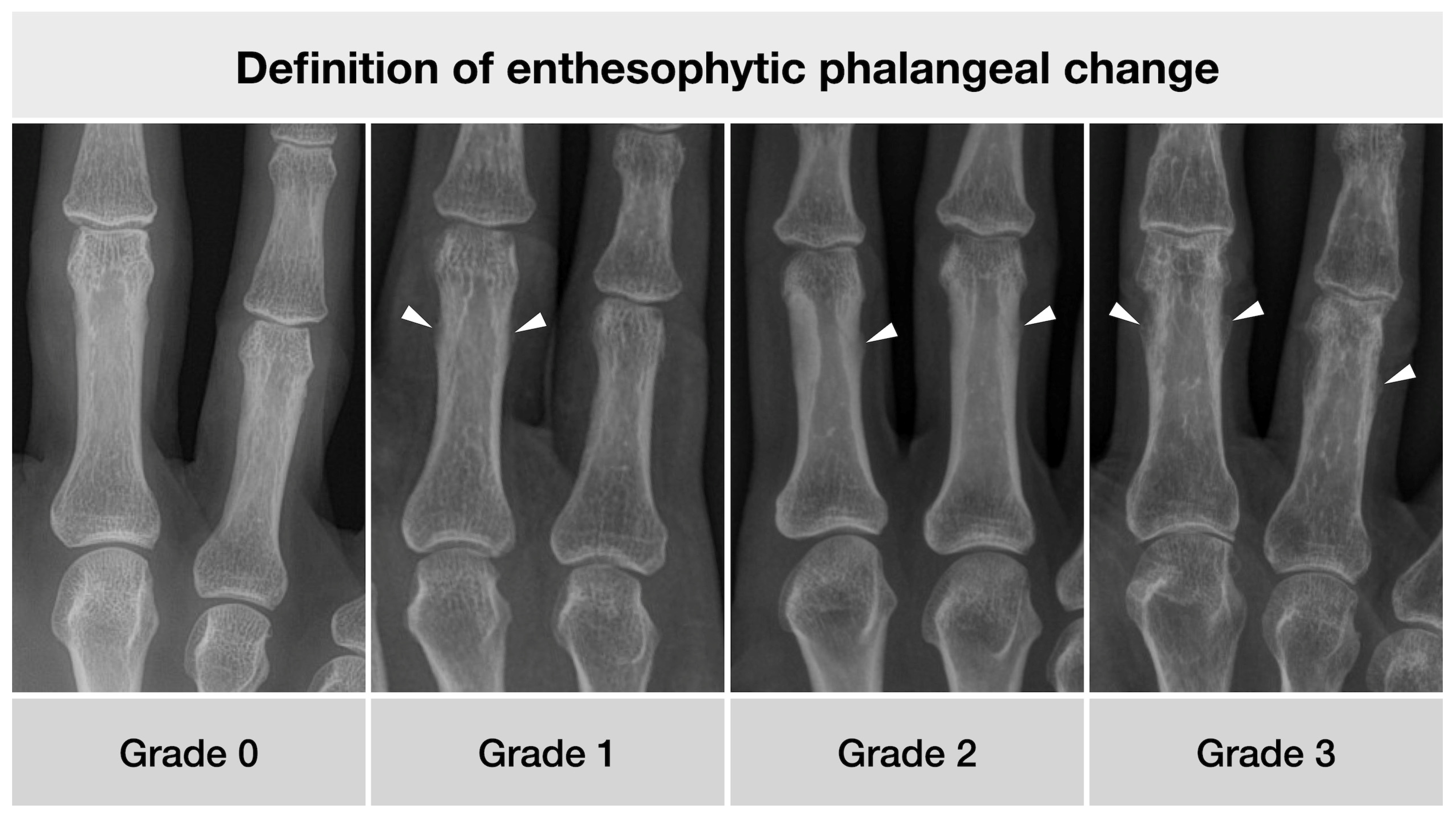
| Grade | Definition of Enthesophytic Phalangeal Change |
|---|---|
| 0 | Cortical bone smooth without prominences |
| 1 | Irregular cortical bone, possibly with fluffing, possibly with smallest, flattened periosteal proliferations |
| 2 | Cortical bone with well-defined enthesophytic protuberance, not more than 1 mm of substance increase |
| 3 | Cortical bone with clearly recognizable enthesophytic proliferation of 1 mm or more |
| <30 Years (%, n) | 30–39 Years (%, n) | 40–49 Years (%, n) | 50–59 Years (%, n) | 60–69 Years (%, n) | 70–79 Years (%, n) | ≥80 Years (%, n) | |
|---|---|---|---|---|---|---|---|
| DIP-II | 2.0 (5/252) | 2.4 (4/168) | 10.6 (18/170) | 16.4 (26/159) | 34.1 (60/176) | 50.3 (75/149) | 49.4 (39/79) |
| PIP-II | 0.0 (0/252) | 1.2 (2/168) | 0.0 (0/170) | 4.4 (7/159) | 7.4 (13/176) | 16.8 (25/149) | 21.5 (17/79) |
| MCP-II | 0.0 (0/252) | 0.0 (0/168) | 0.6 (1/170) | 2.5 (4/159) | 2.8 (5/176) | 4.7 (7/149) | 12.7 (10/79) |
| DIP-III | 1.6 (4/252) | 4.3 (7/168) | 5.9 (10/170) | 16.4 (26/159) | 31.8 (56/176) | 55.7 (83/149) | 48.1 (38/79) |
| PIP-III | 0.4 (1/252) | 0.0 (0/168) | 1.8 (3/170) | 3.8 (6/159) | 6.3 (11/176) | 14.8 (22/149) | 20.3 (16/79) |
| MCP-III | 0.0 (0/252) | 0.0 (0/168) | 1.2 (2/170) | 1.9 (3/159) | 2.3 (4/176) | 6.7 (10/149) | 13.9 (11/79) |
| DIP-IV | 0.4 (1/252) | 4.2 (7/168) | 6.5 (11/170) | 13.2 (21/159) | 22.7 (40/176) | 39.6 (59/149) | 36.7 (29/79) |
| PIP-IV | 0.0 (0/252) | 1.2 (2/168) | 2.9 (5/170) | 5.7 (9/159) | 7.4 (13/176) | 22.8 (34/149) | 22.8 (18/79) |
| MCP-IV | 0.0 (0/252) | 0.0 (0/168) | 0.0 (0/170) | 0.0 (0/159) | 0.0 (0/176) | 2.7 (4/149) | 1.3 (1/79) |
| DIP-V | 0.4 (1/252) | 3.0 (5/168) | 5.9 (10/170) | 8.2 (13/159) | 21.0 (37/176) | 34.2 (51/149) | 43.0 (34/79) |
| PIP-V | 0.0 (0/252) | 0.6 (1/168) | 0.0 (0/170) | 3.1 (5/159) | 10.8 (19/176) | 20.1 (30/149) | 24.1 (19/79) |
| MCP-V | 0.0 (0/252) | 0.0 (0/168) | 0.0 (0/170) | 0.0 (0/159) | 0.6 (1/176) | 1.3 (2/149) | 3.8 (3/79) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hermann, S.; Eshed, I.; Sáenz, I.; Doepner, N.; Ziegeler, K.; Hermann, K.G.A. Osteo-Proliferative Lesions of the Phalanges on Radiography: Associations with Sex, Age, and Osteoarthritis. Diagnostics 2022, 12, 618. https://doi.org/10.3390/diagnostics12030618
Hermann S, Eshed I, Sáenz I, Doepner N, Ziegeler K, Hermann KGA. Osteo-Proliferative Lesions of the Phalanges on Radiography: Associations with Sex, Age, and Osteoarthritis. Diagnostics. 2022; 12(3):618. https://doi.org/10.3390/diagnostics12030618
Chicago/Turabian StyleHermann, Sandra, Iris Eshed, Iván Sáenz, Niclas Doepner, Katharina Ziegeler, and Kay Geert A. Hermann. 2022. "Osteo-Proliferative Lesions of the Phalanges on Radiography: Associations with Sex, Age, and Osteoarthritis" Diagnostics 12, no. 3: 618. https://doi.org/10.3390/diagnostics12030618
APA StyleHermann, S., Eshed, I., Sáenz, I., Doepner, N., Ziegeler, K., & Hermann, K. G. A. (2022). Osteo-Proliferative Lesions of the Phalanges on Radiography: Associations with Sex, Age, and Osteoarthritis. Diagnostics, 12(3), 618. https://doi.org/10.3390/diagnostics12030618







