The Influence of Surgical Realignment Procedures on Dynamic Patellar Tracking: A Dynamic Magnetic Resonance Imaging-Controlled Feasibility Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
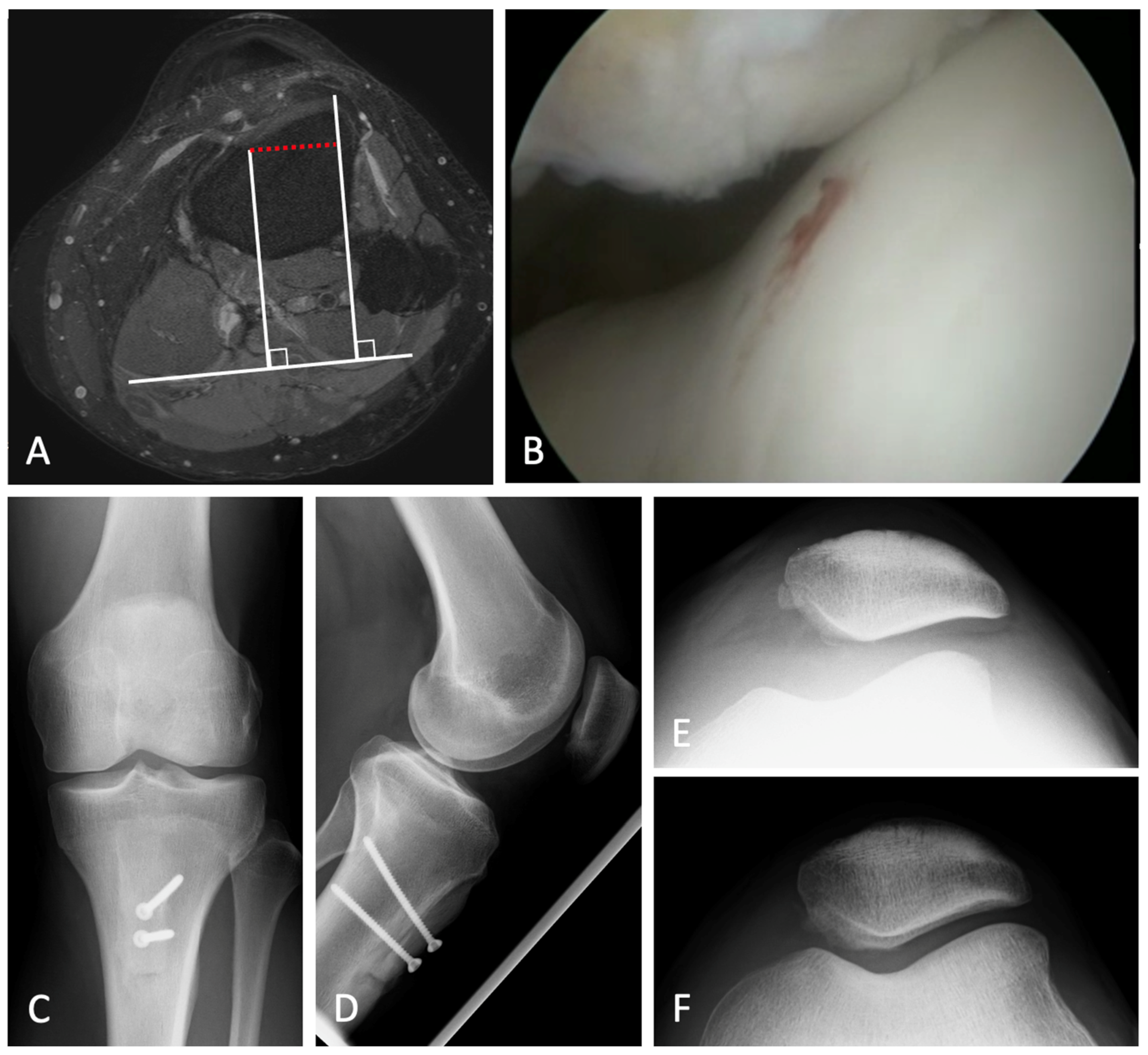
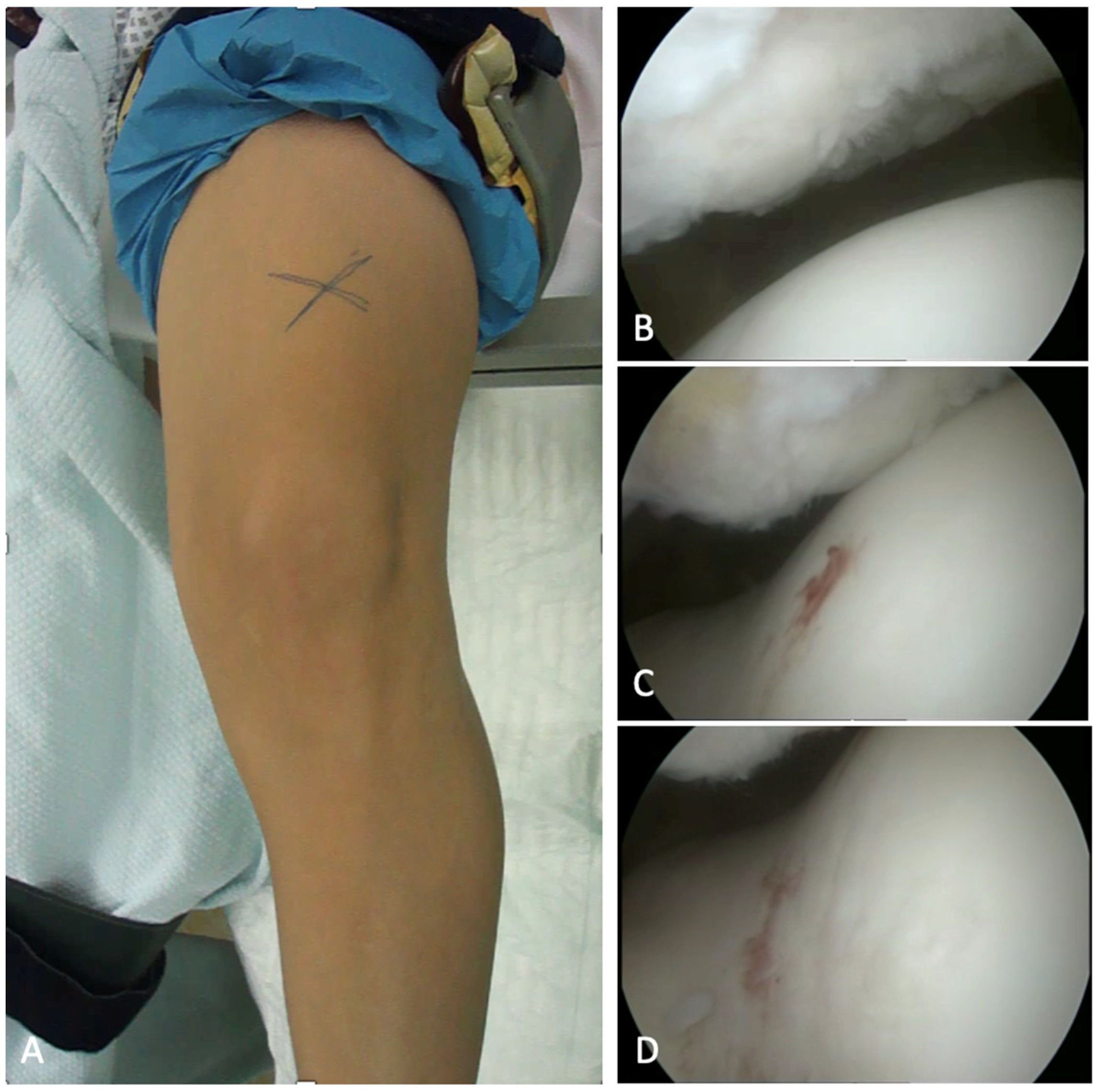
2.2. Surgical Techniques
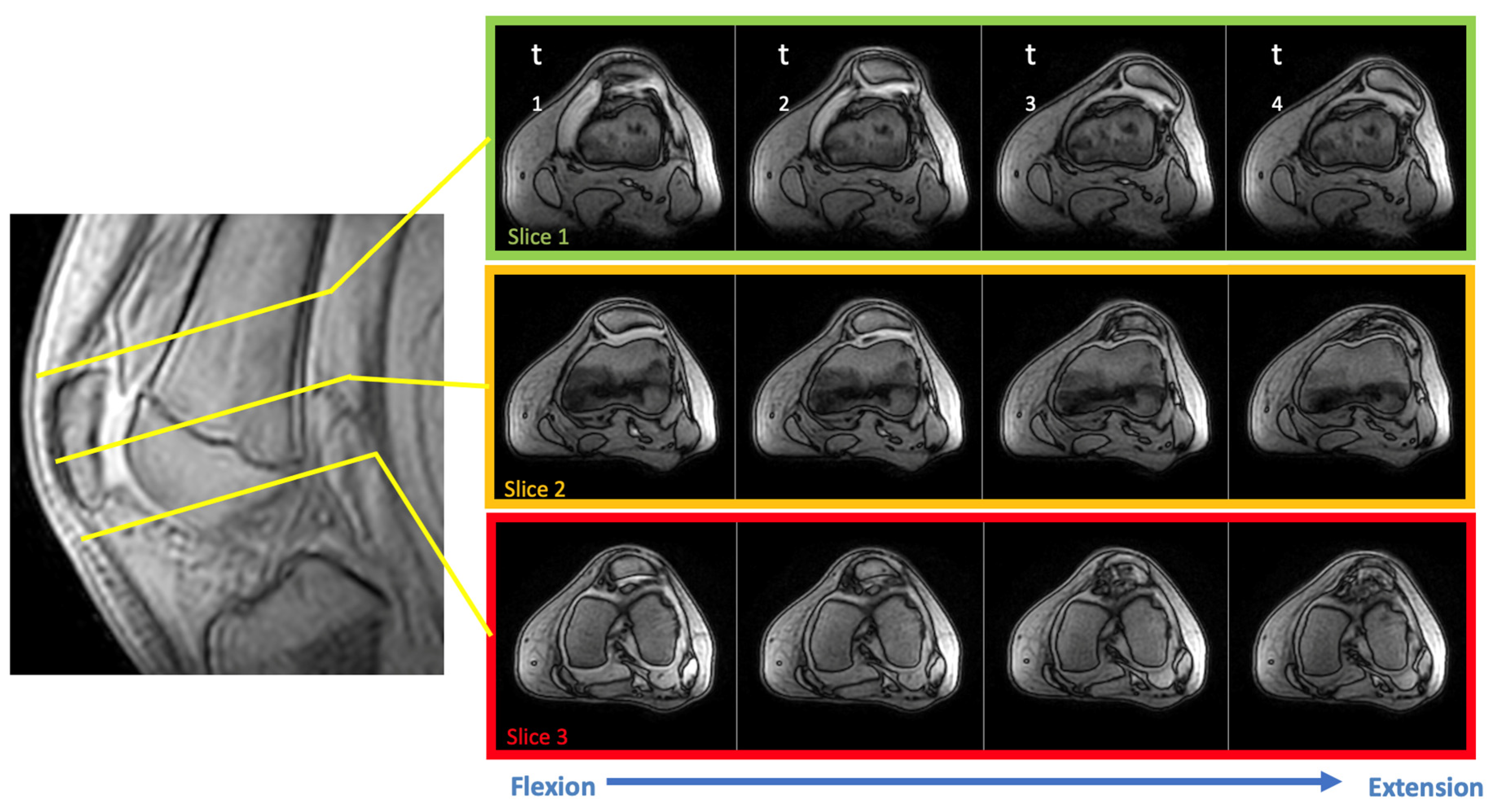
2.3. Examination Setup
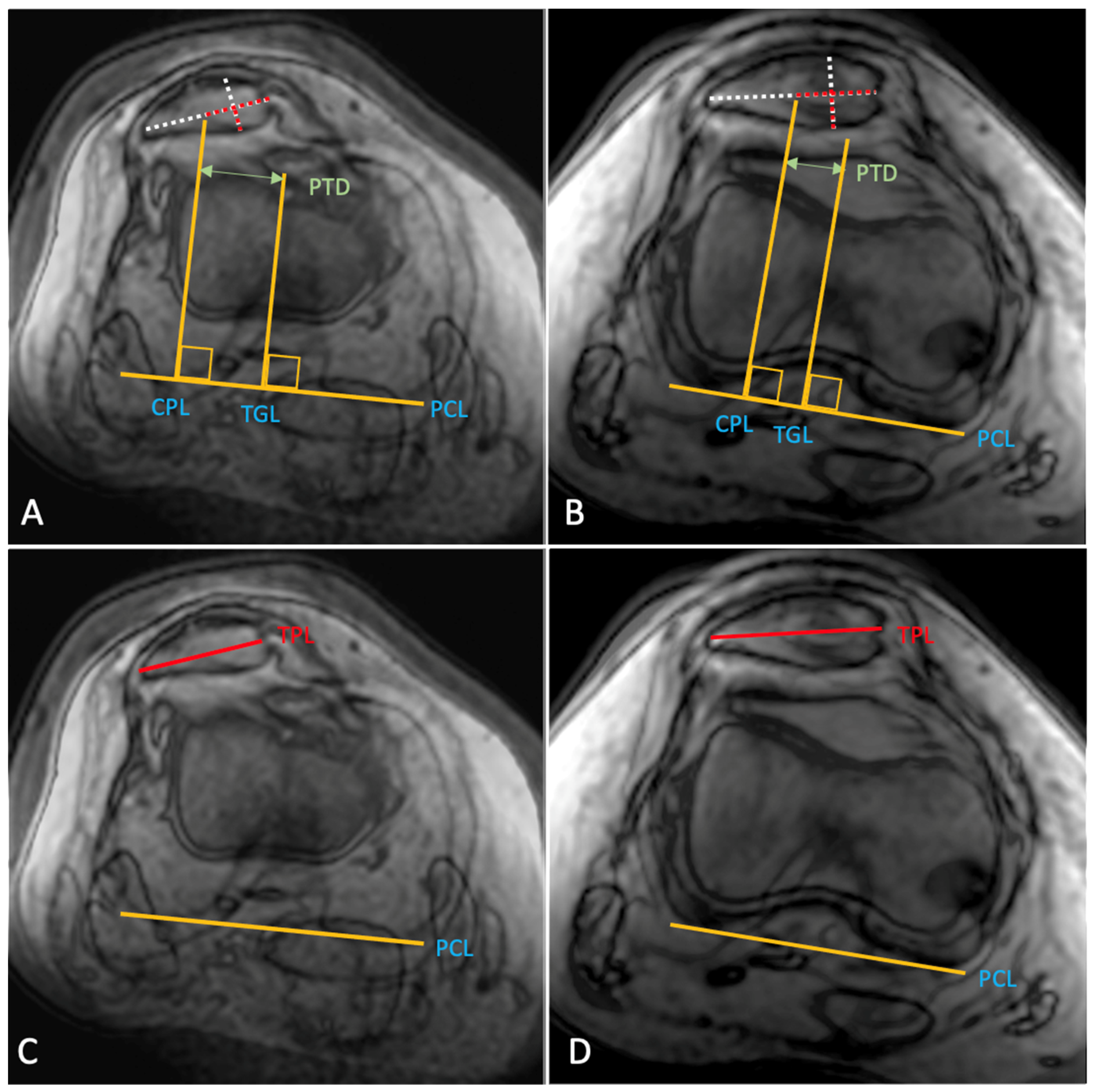
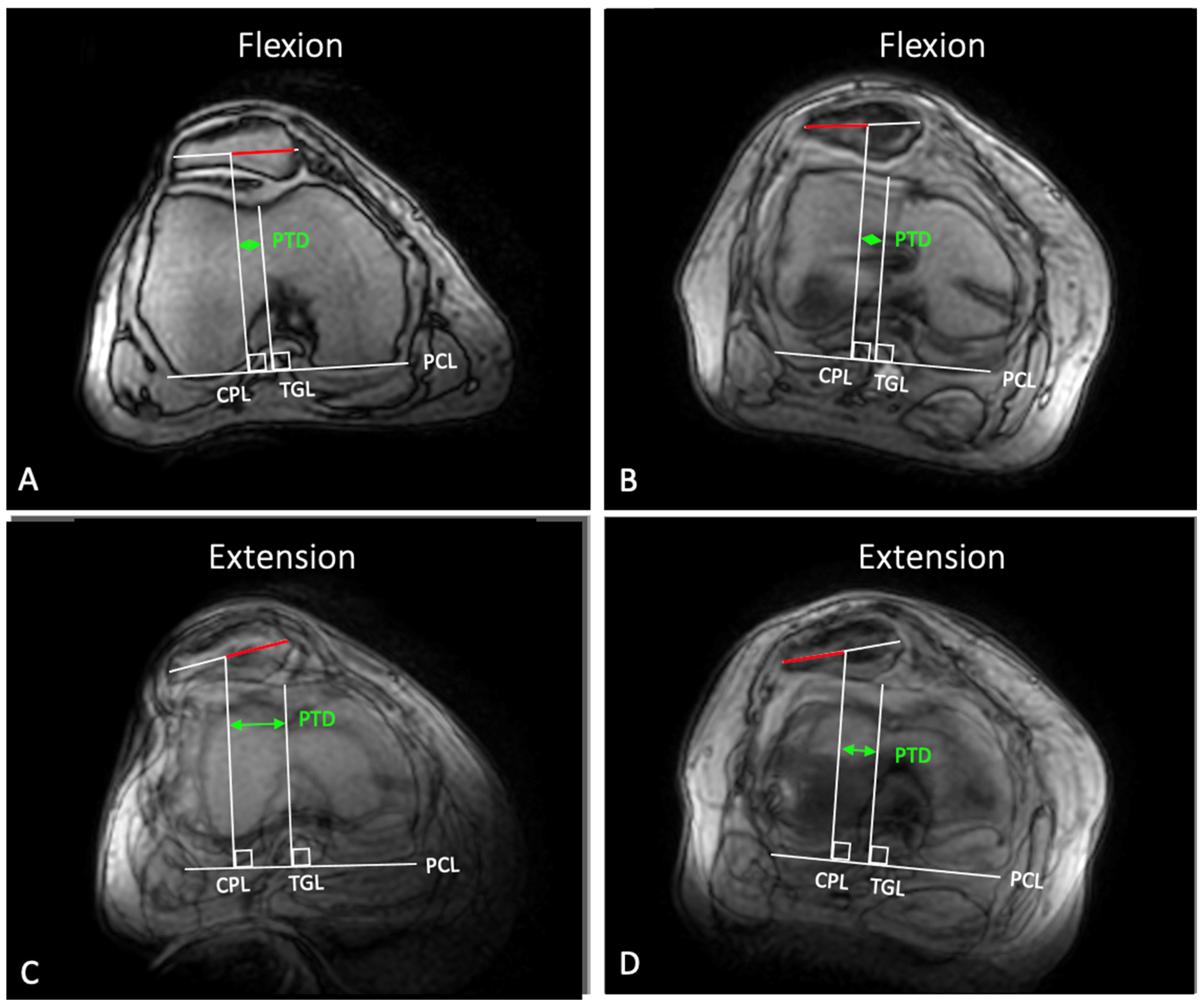
3. Measurement and Analysis
Statistical Calculations
4. Results
5. Discussion and Conclusions
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Arendt, E.A.; Askenberger, M.; Agel, J.; Tompkins, M.A. Risk of Redislocation After Primary Patellar Dislocation: A Clinical Prediction Model Based on Magnetic Resonance Imaging Variables. Am. J. Sports Med. 2018, 46, 3385–3390. [Google Scholar] [CrossRef] [PubMed]
- Previtali, D.; Milev, S.R.; Pagliazzi, G.; Filardo, G.; Zaffagnini, S.; Candrian, C. Recurrent Patellar Dislocations Without Untreated Predisposing Factors: Medial Patellofemoral Ligament Reconstruction Versus Other Medial Soft-Tissue Surgical Techniques-A Meta-analysis. Arthroscopy 2020, 36, 1725–1734. [Google Scholar] [CrossRef] [PubMed]
- Hevesi, M.; Heidenreich, M.J.; Camp, C.L.; Hewett, T.E.; Stuart, M.J.; Dahm, D.L.; Krych, A.J. The Recurrent Instability of the Patella Score: A Statistically Based Model for Prediction of Long-Term Recurrence Risk After First-Time Dislocation. Arthroscopy 2019, 35, 537–543. [Google Scholar] [CrossRef] [PubMed]
- Balcarek, P.; Oberthur, S.; Hopfensitz, S.; Frosch, S.; Walde, T.A.; Wachowski, M.M.; Schuttrumpf, J.P.; Sturmer, K.M. Which patellae are likely to redislocate? Knee Surg. Sports Traumatol. Arthrosc. 2014, 22, 2308–2314. [Google Scholar] [CrossRef] [PubMed]
- Frings, J.; Balcarek, P.; Tscholl, P.M.; Liebensteiner, M.; Dirisamer, F.; Koenen, P. Conservative versus surgical treatment for primary patellar dislocation—A systematic review to guide risk stratification. Deutsch Arztebl. Int. 2020, 117, 279–286. [Google Scholar]
- Kaiser, P.; Schmoelz, W.; Schoettle, P.; Zwierzina, M.; Heinrichs, C.; Attal, R. Increased internal femoral torsion can be regarded as a risk factor for patellar instability—A biomechanical study. Clin. Biomech. 2017, 47, 103–109. [Google Scholar] [CrossRef]
- Stephen, J.M.; Lumpaopong, P.; Dodds, A.L.; Williams, A.; Amis, A.A. The effect of tibial tuberosity medialization and lateralization on patellofemoral joint kinematics, contact mechanics, and stability. Am. J. Sports Med. 2015, 43, 186–194. [Google Scholar] [CrossRef]
- Tanaka, M.J.; Elias, J.J.; Williams, A.A.; Carrino, J.A.; Cosgarea, A.J. Correlation Between Changes in Tibial Tuberosity-Trochlear Groove Distance and Patellar Position During Active Knee Extension on Dynamic Kinematic Computed Tomographic Imaging. Arthroscopy 2015, 31, 1748–1755. [Google Scholar] [CrossRef]
- Tischer, T.; Geier, A.; Lenz, R.; Woernle, C.; Bader, R. Impact of the patella height on the strain pattern of the medial patellofemoral ligament after reconstruction: A computer model-based study. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 3123–3133. [Google Scholar] [CrossRef]
- Van Haver, A.; De Roo, K.; De Beule, M.; Labey, L.; De Baets, P.; Dejour, D.; Claessens, T.; Verdonk, P. The effect of trochlear dysplasia on patellofemoral biomechanics: A cadaveric study with simulated trochlear deformities. Am. J. Sports Med. 2015, 43, 1354–1361. [Google Scholar] [CrossRef]
- Liebensteiner, M.; Keiler, A.; El Attal, R.; Balcarek, P.; Dirisamer, F.; Giesinger, J.; Seitlinger, G.; Nelitz, M.; Keshmiri, A.; Frings, J.; et al. Conservative versus tailored surgical treatment in patients with first time lateral patella dislocation: A randomized-controlled trial. J. Orthop. Surg. Res. 2021, 16, 378. [Google Scholar] [CrossRef]
- Frosch, K.H.; Schmeling, A. A new classification system of patellar instability and patellar maltracking. Arch. Orthop. Trauma. Surg. 2016, 136, 485–497. [Google Scholar] [CrossRef]
- Bartsch, A.; Lubberts, B.; Mumme, M.; Egloff, C.; Pagenstert, G. Does patella alta lead to worse clinical outcome in patients who undergo isolated medial patellofemoral ligament reconstruction? A systematic review. Arch. Orthop. Trauma. Surg. 2018, 138, 1563–1573. [Google Scholar] [CrossRef]
- Frings, J.; Krause, M.; Wohlmuth, P.; Akoto, R.; Frosch, K.H. Influence of patient-related factors on clinical outcome of tibial tubercle transfer combined with medial patellofemoral ligament reconstruction. Knee 2018, 25, 1157–1164. [Google Scholar] [CrossRef]
- Laidlaw, M.S.; Feeley, S.M.; Ruland, J.R.; Diduch, D.R. Sulcus-Deepening Trochleoplasty and Medial Patellofemoral Ligament Reconstruction for Recurrent Patellar Instability. Arthrosc. Tech. 2018, 7, e113–e123. [Google Scholar] [CrossRef]
- Frings, J.; Krause, M.; Akoto, R.; Frosch, K.H. Clinical Results after Combined Distal Femoral Osteotomy in Patients with Patellar Maltracking and Recurrent Dislocations. J. Knee Surg. 2019, 32, 924–933. [Google Scholar] [CrossRef]
- Tscholl, P.M.; Wanivenhaus, F.; Centmaier-Molnar, V.; Camenzind, R.S.; Fucentese, S.F. Clinical and radiological results after one hundred fifteen MPFL reconstructions with or without tibial tubercle transfer in patients with recurrent patellar dislocation-a mean follow-up of 5.4 years. Int. Orthop. 2020, 44, 301–308. [Google Scholar] [CrossRef]
- Zimmermann, F.; Bortlein, J.; Milinkovic, D.D.; Balcarek, P. Patient-Reported Outcomes After Revision Surgery for Failed Medial Patellofemoral Ligament Reconstruction: A Matched-Pair Analysis Including Correction of Predisposing Factors. Am. J. Sports Med. 2020, 48, 3566–3572. [Google Scholar] [CrossRef]
- Gorbaty, J.D.; Varkey, D.T.; Hong, I.S.; Trofa, D.P.; Odum, S.M.; Piasecki, D.P.; Saltzman, B.M.; Fleischli, J.E. Outcomes and reoperation rates after tibial tubercle transfer and medial patellofemoral ligament reconstruction: Higher revision stabilization in patients with trochlear dysplasia and patella alta. Knee Surg. Sports Traumatol. Arthrosc. 2021, 30, 2227–2234. [Google Scholar] [CrossRef]
- Leite, C.B.G.; Santos, T.P.; Giglio, P.N.; Pecora, J.R.; Camanho, G.L.; Gobbi, R.G. Tibial Tubercle Osteotomy With Distalization Is a Safe and Effective Procedure for Patients With Patella Alta and Patellar Instability. Orthop. J. Sports Med. 2021, 9, 2325967120975101. [Google Scholar] [CrossRef]
- Tan, S.H.S.; Ngiam, E.H.K.; Lim, J.Y.; Lim, A.K.S.; Hui, J.H. Surgical Management of Patella Alta in Patellofemoral Instability: A Systematic Review and Meta-analysis. Orthop. J. Sports Med. 2021, 9, 2325967121999642. [Google Scholar] [CrossRef] [PubMed]
- Hiemstra, L.A.; O’Brien, C.L.; Lafave, M.R.; Kerslake, S. Common Physical Examination Tests for Patellofemoral Instability Demonstrate Weak Inter-Rater Reliability. Arthrosc. Sports Med. Rehabil. 2021, 3, e673–e677. [Google Scholar] [CrossRef] [PubMed]
- Frings, J.; Dust, T.; Krause, M.; Ohlmeier, M.; Frosch, K.H.; Adam, G.; Warncke, M.; Maas, K.J.; Henes, F.O. Objective assessment of patellar maltracking with 3 T dynamic magnetic resonance imaging: Feasibility of a robust and reliable measuring technique. Sci. Rep. 2020, 10, 16770. [Google Scholar] [CrossRef] [PubMed]
- Burke, C.J.; Kaplan, D.; Block, T.; Chang, G.; Jazrawi, L.; Campbell, K.; Alaia, M. Clinical Utility of Continuous Radial Magnetic Resonance Imaging Acquisition at 3 T in Real-time Patellofemoral Kinematic Assessment: A Feasibility Study. Arthroscopy 2018, 34, 726–733. [Google Scholar] [CrossRef]
- Frings, J.; Dust, T.; Krause, M.; Frosch, K.H.; Adam, G.; Warncke, M.; Welsch, G.; Henes, F.O.; Maas, K.J. Dynamic Mediolateral Patellar Translation Is a Sex- and Size-Independent Parameter of Adult Proximal Patellar Tracking Using Dynamic 3 Tesla Magnetic Resonance Imaging. Arthroscopy 2022, 38, 1571–1580. [Google Scholar] [CrossRef]
- Frings, J.; Krause, M.; Akoto, R.; Wohlmuth, P.; Frosch, K.H. Combined distal femoral osteotomy (DFO) in genu valgum leads to reliable patellar stabilization and an improvement in knee function. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 3572–3581. [Google Scholar] [CrossRef]
- Kraus, T.; Lidder, S.; Svehlik, M.; Rippel, K.; Schneider, F.; Eberl, R.; Linhart, W. Patella re-alignment in children with a modified Grammont technique. Acta Orthop. 2012, 83, 504–510. [Google Scholar] [CrossRef]
- Bereiter, H.; Gautier, E. Die Trochleaplastik als chirurgische Therapie der rezidivierenden Patellaluxation bei Trochleadysplasie des Femurs. Arthroskopie 1994, 7, 281–286. [Google Scholar]
- Biedert, R.M. Laterale Retinakulumverlängerung bei arthroskopischen Eingriffen. Arthroskopie 2010, 23, 191–194. [Google Scholar] [CrossRef]
- Ren, B.; Zhang, X.; Zhang, L.; Zhang, M.; Liu, Y.; Tian, B.; Zhang, B.; Zheng, J. Isolated trochleoplasty for recurrent patellar dislocation has lower outcome and higher residual instability compared with combined MPFL and trochleoplasty: A systematic review. Arch. Orthop. Trauma Surg. 2019, 139, 1617–1624. [Google Scholar] [CrossRef]
- Schottle, P.B.; Romero, J.; Schmeling, A.; Weiler, A. anatomical reconstruction of the medial patellofemoral ligament using a free gracilis autograft. Arch. Orthop. Trauma. Surg. 2008, 128, 479–484. [Google Scholar] [CrossRef] [PubMed]
- Caton, J.; Deschamps, G.; Chambat, P.; Lerat, J.L.; Dejour, H. Patella infera. Apropos of 128 cases. Rev. Chir. Orthop. Reparatrice Appar. Mot. 1982, 68, 317–325. [Google Scholar]
- Yue, R.A.; Arendt, E.A.; Tompkins, M.A. Patellar Height Measurements on Radiograph and Magnetic Resonance Imaging in Patellar Instability and Control Patients. J. Knee Surg. 2017, 30, 943–950. [Google Scholar] [CrossRef]
- Seitlinger, G.; Scheurecker, G.; Högler, R.; Labey, L.; Innocenti, B.; Hofmann, S. Tibial tubercle-posterior cruciate ligament distance: A new measurement to define the position of the tibial tubercle in patients with patellar dislocation. Am. J. Sports Med. 2012, 40, 1119–1125. [Google Scholar] [CrossRef]
- Schoettle, P.B.; Zanetti, M.; Seifert, B.; Pfirrmann, C.W.; Fucentese, S.F.; Romero, J. The tibial tuberosity-trochlear groove distance; a comparative study between CT and MRI scanning. Knee 2006, 13, 26–31. [Google Scholar] [CrossRef]
- Biedert, R.M.; Bachmann, M. Anterior-posterior trochlear measurements of normal and dysplastic trochlea by axial magnetic resonance imaging. Knee Surg. Sports Traumatol. Arthrosc. 2009, 17, 1225–1230. [Google Scholar] [CrossRef]
- Nacey, N.C.; Fox, M.G.; Luce, B.N.; Boatman, D.M.; Diduch, D.R. Assessing Femoral Trochlear Morphologic Features on Cross-Sectional Imaging Before Trochleoplasty: Dejour Classification Versus Quantitative Measurement. AJR Am. J. Roentgenol. 2020, 215, 458–464. [Google Scholar] [CrossRef]
- Paiva, M.; Blønd, L.; Hölmich, P.; Steensen, R.N.; Diederichs, G.; Feller, J.A.; Barfod, K.W. Quality assessment of radiological measurements of trochlear dysplasia; a literature review. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 746–755. [Google Scholar] [CrossRef]
- Stefanik, J.J.; Zumwalt, A.C.; Segal, N.A.; Lynch, J.A.; Powers, C.M. Association between measures of patella height, morphologic features of the trochlea, and patellofemoral joint alignment: The MOST study. Clin. Orthop. Relat. Res. 2013, 471, 2641–2648. [Google Scholar] [CrossRef]
- Koo, T.K.; Li, M.Y. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef]
- Waidelich, H.; Strecker, W.; Schneider, E. Computed tomographic torsion-angle and length measurement of the lower extremity. The methods, normal values and radiation load. RoFo 1992, 157, 245–251. [Google Scholar] [CrossRef] [PubMed]
- Hiemstra, L.A.; Peterson, D.; Youssef, M.; Soliman, J.; Banfield, L.; Ayeni, O.R. Trochleoplasty provides good clinical outcomes and an acceptable complication profile in both short and long-term follow-up. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 2967–2983. [Google Scholar] [CrossRef] [PubMed]
- Zaffagnini, S.; Previtali, D.; Tamborini, S.; Pagliazzi, G.; Filardo, G.; Candrian, C. Recurrent patellar dislocations: Trochleoplasty improves the results of medial patellofemoral ligament surgery only in severe trochlear dysplasia. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 3599–3613. [Google Scholar] [CrossRef] [PubMed]
- Dickschas, J.; Tassika, A.; Lutter, C.; Harrer, J.; Strecker, W. Torsional osteotomies of the tibia in patellofemoral dysbalance. Arch. Orthop. Trauma. Surg. 2017, 137, 179–185. [Google Scholar] [CrossRef] [PubMed]
- Dickschas, J.; Ferner, F.; Lutter, C.; Gelse, K.; Harrer, J.; Strecker, W. Patellofemoral dysbalance and genua valga: Outcome after femoral varisation osteotomies. Arch. Orthop. Trauma. Surg. 2018, 138, 19–25. [Google Scholar] [CrossRef]
- Mulliez, A.; Lambrecht, D.; Verbruggen, D.; Van Der Straeten, C.; Verdonk, P.; Victor, J. Clinical outcome in MPFL reconstruction with and without tuberositas transposition. Knee Surg. Sports Traumatol. Arthrosc. 2015, 25, 2708–2714. [Google Scholar] [CrossRef]
- Chen, H.; Zhao, D.; Xie, J.; Duan, Q.; Zhang, J.; Wu, Z.; Jiang, J. The outcomes of the modified Fulkerson osteotomy procedure to treat habitual patellar dislocation associated with high-grade trochlear dysplasia. BMC Musculoskelet. Disord. 2017, 18, 73. [Google Scholar] [CrossRef]
- Clark, D.; Stevens, J.M.; Tortonese, D.; Whitehouse, M.R.; Simpson, D.; Eldridge, J. Mapping the contact area of the patellofemoral joint: The relationship between stability and joint congruence. Bone Jt. J. 2019, 101, 552–558. [Google Scholar] [CrossRef]
- Vollnberg, B.; Koehlitz, T.; Jung, T.; Scheffler, S.; Hoburg, A.; Khandker, D.; Hamm, B.; Wiener, E.; Diederichs, G. Prevalence of cartilage lesions and early osteoarthritis in patients with patellar dislocation. Europ. Radiol. 2012, 22, 2347–2356. [Google Scholar] [CrossRef]
- Salonen, E.E.; Magga, T.; Sillanpaa, P.J.; Kiekara, T.; Maenpaa, H.; Mattila, V.M. Traumatic Patellar Dislocation and Cartilage Injury: A Follow-up Study of Long-Term Cartilage Deterioration. Am. J. Sports Med. 2017, 45, 1376–1382. [Google Scholar] [CrossRef]
- Fick, C.N.; Grant, C.; Sheehan, F.T. Patellofemoral Pain in Adolescents: Understanding Patellofemoral Morphology and Its Relationship to Maltracking. Am. J. Sports Med. 2020, 48, 341–350. [Google Scholar] [CrossRef]
- Gobbi, R.G.; Demange, M.K.; de Avila, L.F.R.; Araujo Filho, J.A.B.; Moreno, R.A.; Gutierrez, M.A.; de Sa Rebelo, M.; Tirico, L.E.P.; Pecora, J.R.; Camanho, G.L. Patellar tracking after isolated medial patellofemoral ligament reconstruction: Dynamic evaluation using computed tomography. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 3197–3205. [Google Scholar] [CrossRef]
- Rezvanifar, S.C.; Flesher, B.L.; Jones, K.C.; Elias, J.J. Lateral patellar maltracking due to trochlear dysplasia: A computational study. Knee 2019, 26, 1234–1242. [Google Scholar] [CrossRef]
- Elias, J.J.; Rezvanifar, S.C.; Koh, J.L. Groove-deepening trochleoplasty reduces lateral patellar maltracking and increases patellofemoral contact pressures: Dynamic simulation. J. Orthop. Res. 2021, 40, 1529–1537. [Google Scholar] [CrossRef]
- Balcarek, P.; Zimmermann, F. Deepening trochleoplasty and medial patellofemoral ligament reconstruction normalize patellotrochlear congruence in severe trochlear dysplasia. Bone Jt. J. 2019, 101, 325–330. [Google Scholar] [CrossRef]
- Lorenz, A.; Muller, O.; Kohler, P.; Wunschel, M.; Wulker, N.; Leichtle, U.G. The influence of asymmetric quadriceps loading on patellar tracking--an in vitro study. Knee 2012, 19, 818–822. [Google Scholar] [CrossRef]
- Stephen, J.; Alva, A.; Lumpaopong, P.; Williams, A.; Amis, A.A. A cadaveric model to evaluate the effect of unloading the medial quadriceps on patellar tracking and patellofemoral joint pressure and stability. J. Exp. Orthop. 2018, 5, 34. [Google Scholar] [CrossRef]
- Thomeer, L.; Guan, S.; Gray, H.; Schache, A.; de Steiger, R.; Pandy, M. Six-Degree-of-Freedom Tibiofemoral and Patellofemoral Joint Motion During Activities of Daily Living. Ann. Biomed. Eng. 2021, 49, 1183–1198. [Google Scholar] [CrossRef]
- Sherman, S.L.; DiPaolo, Z.J.; Ray, T.E.; Sachs, B.M.; Oladeji, L.O. Meniscus Injuries: A Review of Rehabilitation and Return to Play. Clin. Sports Med. 2020, 39, 165–183. [Google Scholar] [CrossRef]
- Hauger, A.V.; Reiman, M.P.; Bjordal, J.M.; Sheets, C.; Ledbetter, L.; Goode, A.P. Neuromuscular electrical stimulation is effective in strengthening the quadriceps muscle after anterior cruciate ligament surgery. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 399–410. [Google Scholar] [CrossRef]
- Balcarek, P.; Oberthur, S.; Frosch, S.; Schuttrumpf, J.P.; Sturmer, K.M. Vastus medialis obliquus muscle morphology in primary and recurrent lateral patellar instability. BioMed Res. Int. 2014, 2014, 326586. [Google Scholar] [CrossRef] [PubMed]
- Pal, S.; Besier, T.F.; Draper, C.E.; Fredericson, M.; Gold, G.E.; Beaupre, G.S.; Delp, S.L. Patellar tilt correlates with vastus lateralis: Vastus medialis activation ratio in maltracking patellofemoral pain patients. J. Orthop. Res. 2012, 30, 927–933. [Google Scholar] [CrossRef] [PubMed]
- Sawatsky, A.; Bourne, D.; Horisberger, M.; Jinha, A.; Herzog, W. Changes in patellofemoral joint contact pressures caused by vastus medialis muscle weakness. Clin. Biomech. 2012, 27, 595–601. [Google Scholar] [CrossRef] [PubMed]
- Amis, A.A.; Senavongse, W.; Bull, A.M. Patellofemoral kinematics during knee flexion-extension: An in vitro study. J. Orthop. Res. 2006, 24, 2201–2211. [Google Scholar] [CrossRef]
- Kita, K.; Tanaka, Y.; Toritsuka, Y.; Amano, H.; Uchida, R.; Takao, R.; Horibe, S. Factors Affecting the Outcomes of Double-Bundle Medial Patellofemoral Ligament Reconstruction for Recurrent Patellar Dislocations Evaluated by Multivariate Analysis. Am. J. Sports Med. 2015, 43, 2988–2996. [Google Scholar] [CrossRef]


| Inclusion Criteria | Exclusion Criteria |
|---|---|
| recurring patellar dislocations | limited range of motion |
| clinical signs for patellar maltracking | absence of patellar maltracking (absence of patellar maltracking) |
| planned surgical realignment | concomitant knee injuries |
| written consent to participate | acute joint effusion |
| Parameter | Preoperative (n = 24) | Postoperative (n = 24) | p |
|---|---|---|---|
| Side | |||
| Left knee | 12 | ||
| Right knee | 12 | ||
| Sex | |||
| Male | 7 | ||
| Female | 17 | ||
| Age (range) Years | 23.0 (12–45) | ||
| TT-TG (±SD), mm | 15.35 ± 5.18 | 10.17 ± 4.11 | 0.008 |
| TT-PCL (±SD), mm | 23.03 ± 4.50 | 16.30 ± 5.16 | <0.001 |
| Trochlear sulcus angle (±SD), degrees | 143.80 ± 12.65 | 139.35 ± 8.80 | 0.678 |
| Trochlear sulcus depth (±SD), mm | 4.84 ± 1.49 | 5.29 ± 1.52 | 0.217 |
| Lateral inclination angle (±SD), degrees | 19.58 ± 7.08 | 19.41 ± 5.99 | 0.482 |
| Canton Deschamps Index (±SD) | 1.33 ± 0.20 | 1.29 ± 0.18 | 0.158 |
| Patellar position in flexion (±SD), mm | 5.75 ± 3.86 | 5.68 ± 4.20 | 0.661 |
| Patellar position in extension (±SD), mm | 16.74 ± 6.32 | 10.83 ± 5.59 | <0.001 |
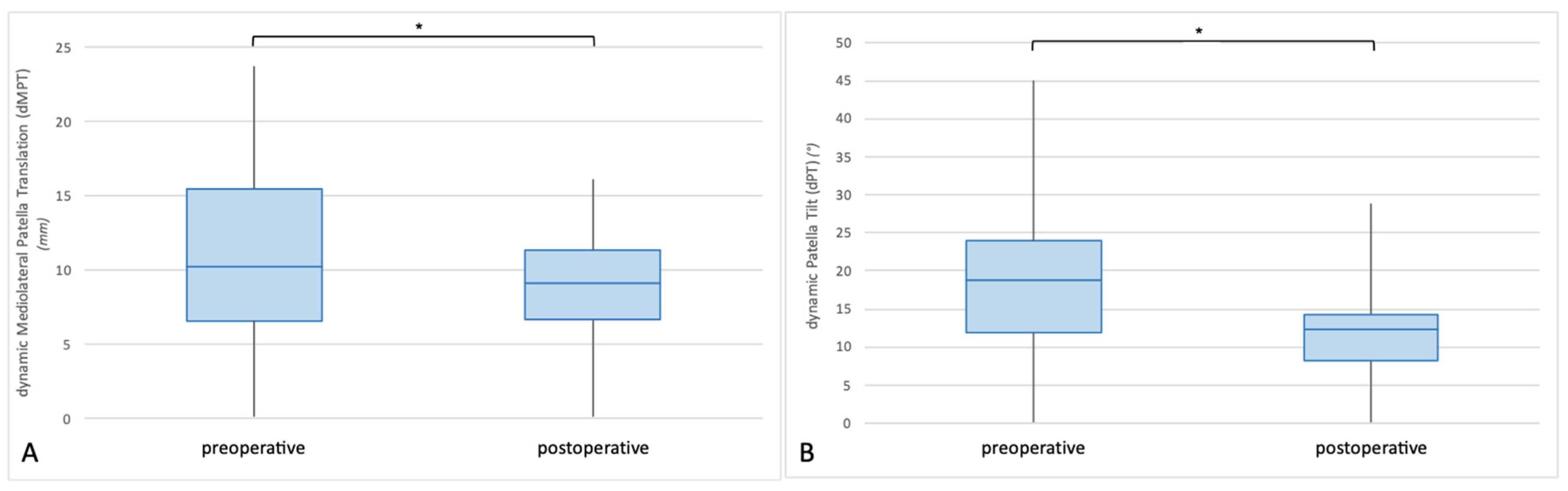
| Dynamic mediolateral translation (±SD), mm | 10.95 ± 5.93 | 4.89 ± 0.40 | <0.001 |
| Patellar tilt in flexion (±SD), degrees | 8.65 ± 6.80 | 7.67 ± 4.19 | 0.719 |
| Patellar tilt in extension (±SD), degrees | 23.15 ± 11.03 | 16.11 ± 7.29 | 0.007 |
| Dynamic patellar tilt (±SD), degrees | 14.50 ± 10.33 to lateral | 8.44 ± 7.46 to lateral | 0.026 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Frings, J.; Dust, T.; Meyer, J.; Krause, M.; Frosch, K.-H.; Adam, G.; Henes, F.O.; Spink, C.; Maas, K.-J. The Influence of Surgical Realignment Procedures on Dynamic Patellar Tracking: A Dynamic Magnetic Resonance Imaging-Controlled Feasibility Study. Diagnostics 2022, 12, 2761. https://doi.org/10.3390/diagnostics12112761
Frings J, Dust T, Meyer J, Krause M, Frosch K-H, Adam G, Henes FO, Spink C, Maas K-J. The Influence of Surgical Realignment Procedures on Dynamic Patellar Tracking: A Dynamic Magnetic Resonance Imaging-Controlled Feasibility Study. Diagnostics. 2022; 12(11):2761. https://doi.org/10.3390/diagnostics12112761
Chicago/Turabian StyleFrings, Jannik, Tobias Dust, Jennifer Meyer, Matthias Krause, Karl-Heinz Frosch, Gerhard Adam, Frank Oliver Henes, Clemens Spink, and Kai-Jonathan Maas. 2022. "The Influence of Surgical Realignment Procedures on Dynamic Patellar Tracking: A Dynamic Magnetic Resonance Imaging-Controlled Feasibility Study" Diagnostics 12, no. 11: 2761. https://doi.org/10.3390/diagnostics12112761
APA StyleFrings, J., Dust, T., Meyer, J., Krause, M., Frosch, K.-H., Adam, G., Henes, F. O., Spink, C., & Maas, K.-J. (2022). The Influence of Surgical Realignment Procedures on Dynamic Patellar Tracking: A Dynamic Magnetic Resonance Imaging-Controlled Feasibility Study. Diagnostics, 12(11), 2761. https://doi.org/10.3390/diagnostics12112761






