A Novel Combination of Blood Biomarkers and Clinical Stroke Scales Facilitates Detection of Large Vessel Occlusion Ischemic Strokes
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Sample Collection
2.2. Clinical Data Collection
2.3. Assigning a Diagnostic Category
- -
- non-LVO if CTA had been undertaken and LVO was not present or if a CTA had not been undertaken upon admission, but the NIHSS score was <5. The latter was a pragmatic threshold reflecting a low likelihood of LVO [15];
- -
- not classifiable if CTA had not been undertaken and NIHSS score on admission was >4.
2.4. Derivation of Stroke Scales from NIHSS Score
2.5. Measurement of Blood Biomarkers
2.6. Statistical Analyses
3. Results
3.1. Derivation Cohort
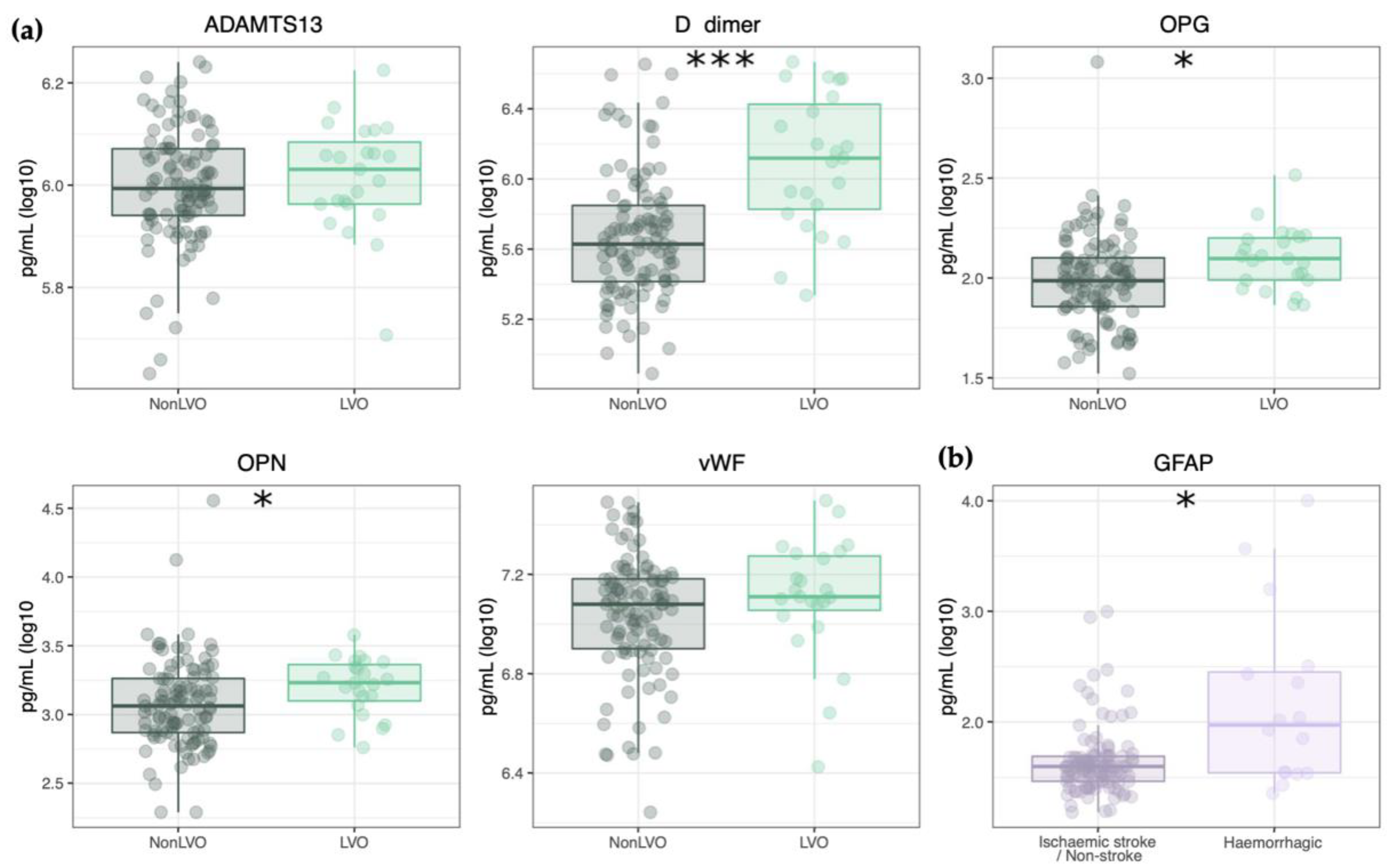
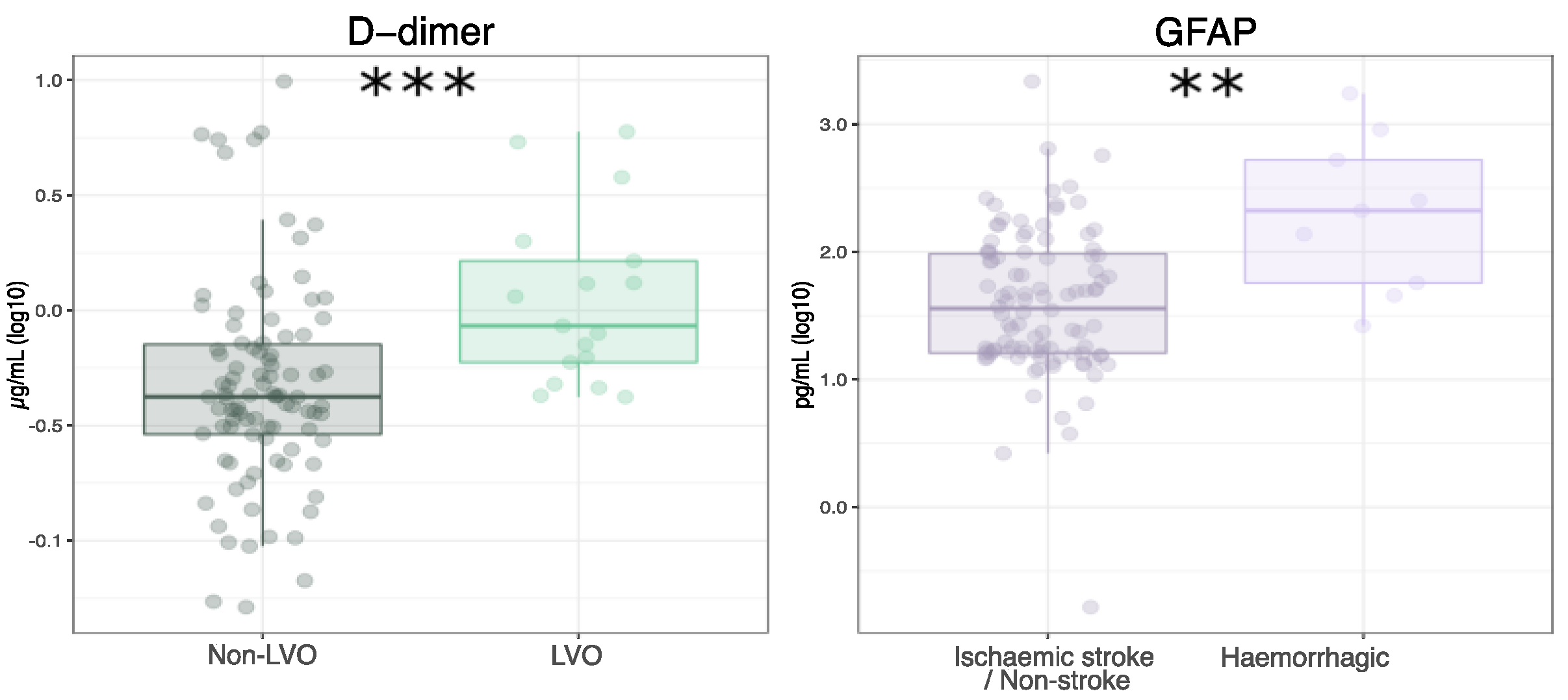
3.2. Blood Biomarker Panel
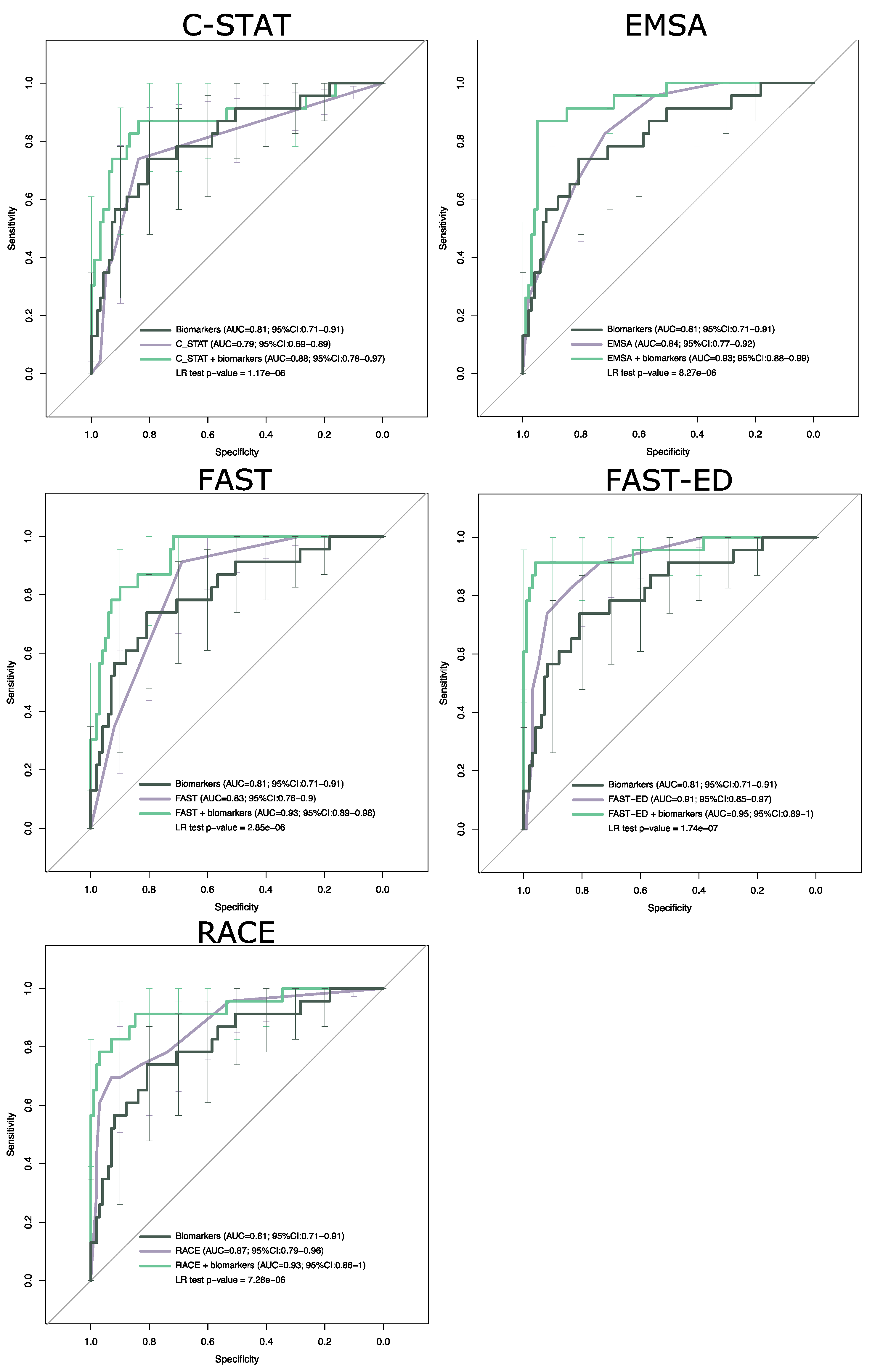
3.3. Combination of Blood Biomarkers and Clinical Stroke Scales
3.4. Validation Cohort
3.5. Validation of Diagnostic Accuracy
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Malhotra, K. Ischemic Strokes Due to Large-Vessel Occlusions Contribute Disproportionately to Stroke-Related Dependence and Death: A Review. Front. Neurol. 2017, 8, 651. [Google Scholar] [CrossRef] [Green Version]
- Goyal, M.; Menon, B.K.; Van Zwam, W.H.; Dippel, D.W.J.; Mitchell, P.J.; Demchuk, A.M.; Dávalos, A.; Majoie, C.B.L.M.; Van Der Lugt, A.; De Miquel, M.A.; et al. Endovascular thrombectomy after large-vessel ischaemic stroke: A meta-analysis of individual patient data from five randomised trials. Lancet 2016, 387, 1723–1731. [Google Scholar] [CrossRef]
- Romoli, M.; Paciaroni, M.; Tsivgoulis, G.; Agostoni, E.C.; Vidale, S. Mothership versus drip-and-ship model for mechanical thrombectomy in acute stroke: A systematic review and meta-analysis for clinical and radiological outcomes. J. Stroke 2020, 22, 317–323. [Google Scholar] [CrossRef]
- American Heart Association Severity-Based Stroke Triage Algorithm for EMS. Mission: Lifeline® Stroke. Available online: https://www.heart.org/en/professional/quality-improvement/mission-lifeline/mission-lifeline-stroke (accessed on 28 May 2021).
- Smith, E.E.; Kent, D.M.; Bulsara, K.R.; Leung, L.Y.; Lichtman, J.H.; Reeves, M.J.; Towfighi, A.; Whiteley, W.N.; Zahuranec, D.B. Accuracy of Prediction Instruments for Diagnosing Large Vessel Occlusion in Individuals With Suspected Stroke: A Systematic Review for the 2018 Guidelines for the Early Management of Patients With Acute Ischemic Stroke. Stroke 2018, 49, e111–e122. [Google Scholar] [CrossRef]
- Turc, G.; Maïer, B.; Naggara, O.; Seners, P.; Isabel, C.; Tisserand, M.; Raynouard, I.; Edjlali, M.; Calvet, D.; Baron, J.C.; et al. Clinical Scales Do Not Reliably Identify Acute Ischemic Stroke Patients with Large-Artery Occlusion. Stroke 2016, 47, 1466–1472. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Monbailliu, T.; Goossens, J.; Hachimi-Idrissi, S. Blood protein biomarkers as diagnostic tool for ischemic stroke: A systematic review. Biomark. Med. 2017, 11, 503–512. [Google Scholar] [CrossRef]
- Montaner, J.; Perea-Gainza, M.; Delgado, P.; Ribó, M.; Chacón, P.; Rosell, A.; Quintana, M.; Palacios, M.E.; Molina, C.A.; Alvarez-Sabín, J. Etiologic diagnosis of ischemic stroke subtypes with plasma biomarkers. Stroke 2008, 39, 2280–2287. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chang, A.; Ricci, B.; Mac Grory, B.; Cutting, S.; Burton, T.; Dakay, K.; Jayaraman, M.; Merkler, A.; Reznik, M.; Lerario, M.P.; et al. Cardiac Biomarkers Predict Large Vessel Occlusion in Patients with Ischemic Stroke. J. Stroke Cerebrovasc. Dis. 2019, 28, 1726–1731. [Google Scholar] [CrossRef]
- Qin, C.; Zhao, X.L.; Ma, X.T.; Zhou, L.Q.; Wu, L.J.; Shang, K.; Wang, W.; Tian, D.S. Proteomic profiling of plasma biomarkers in acute ischemic stroke due to large vessel occlusion. J. Transl. Med. 2019, 17, 214. [Google Scholar] [CrossRef] [PubMed]
- López-Cancio, E.; Bustamante, A.; García-Berrocoso, T.; Millán, M.; Cardona, P.; Rubiera, M.; Serena, J.; Garcè, S.M.; Ustrell, X.; Baldrich, E.; et al. D-dimer as a predictor of large vessel occlusion in acute ischemic stroke. Eur. Stroke J. 2021, 2, 245. [Google Scholar] [CrossRef]
- Ozaki, S.; Kurata, M.; Kumon, Y.; Matsumoto, S.; Tagawa, M.; Watanabe, H.; Ohue, S.; Higaki, J.; Ohnishi, T. Plasma thrombin-cleaved osteopontin as a potential biomarker of acute atherothrombotic ischemic stroke. Hypertens. Res. 2017, 40, 61–66. [Google Scholar] [CrossRef] [PubMed]
- Qu, L.; Jiang, M.; Qiu, W.; Lu, S.; Zhao, Y.; Xia, L.; Ruan, C.; Zhao, Y. Assessment of the Diagnostic Value of Plasma Levels, Activities, and Their Ratios of von Willebrand Factor and ADAMTS13 in Patients with Cerebral Infarction. Clin. Appl. Thromb. 2016, 22, 252–259. [Google Scholar] [CrossRef] [PubMed]
- Bossuyt, P.M.; Reitsma, J.B.; Bruns, D.E.; Gatsonis, C.A.; Glasziou, P.P.; Irwig, L.; Lijmer, J.G.; Moher, D.; Rennie, D.; De Vet, H.C.W.; et al. STARD 2015: An updated list of essential items for reporting diagnostic accuracy studies. BMJ 2015, 351, h5527. [Google Scholar] [CrossRef] [Green Version]
- Scheitz, J.F.; Abdul-Rahim, A.H.; Macisaac, R.L.; Cooray, C.; Sucharew, H.; Kleindorfer, D.; Khatri, P.; Broderick, J.P.; Audebert, H.J.; Ahmed, N.; et al. Clinical Selection Strategies to Identify Ischemic Stroke Patients with Large Anterior Vessel Occlusion: Results from SITS-ISTR (Safe Implementation of Thrombolysis in Stroke International Stroke Thrombolysis Registry). Stroke 2017, 48, 290–297. [Google Scholar] [CrossRef] [Green Version]
- Lima, F.O.; Silva, G.S.; Furie, K.L.; Frankel, M.R.; Lev, M.H.; Camargo, É.C.S.; Haussen, D.C.; Singhal, A.B.; Koroshetz, W.J.; Smith, W.S.; et al. Field Assessment Stroke Triage for Emergency Destination. Stroke 2016, 47, 1997–2002. [Google Scholar] [CrossRef] [PubMed]
- Pérez de la Ossa, N.; Carrera, D.; Gorchs, M.; Querol, M.; Millán, M.; Gomis, M.; Dorado, L.; López-Cancio, E.; Hernández-Pérez, M.; Chicharro, V.; et al. Design and Validation of a Prehospital Stroke Scale to Predict Large Arterial Occlusion. Stroke 2014, 45, 87–91. [Google Scholar] [CrossRef] [Green Version]
- Katz, B.S.; McMullan, J.T.; Sucharew, H.; Adeoye, O.; Broderick, J.P. Design and Validation of a Prehospital Scale to Predict Stroke Severity: Cincinnati Prehospital Stroke Severity Scale. Stroke 2015, 46, 1508–1512. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gropen, T.I.; Boehme, A.; Martin-Schild, S.; Albright, K.; Samai, A.; Pishanidar, S.; Janjua, N.; Brandler, E.S.; Levine, S.R. Derivation and Validation of the Emergency Medical Stroke Assessment and Comparison of Large Vessel Occlusion Scales. J. Stroke Cerebrovasc. Dis. 2018, 27, 806–815. [Google Scholar] [CrossRef]
- Llombart, V.; García-Berrocoso, T.; Bustamante, A.; Giralt, D.; Rodriguez-Luna, D.; Muchada, M.; Penalba, A.; Boada, C.; Hernández-Guillamon, M.; Montaner, J. Plasmatic retinol-binding protein 4 and glial fibrillary acidic protein as biomarkers to differentiate ischemic stroke and intracerebral hemorrhage. J. Neurochem. 2016, 136, 416–424. [Google Scholar] [CrossRef]
- Foerch, C.; Curdt, I.; Yan, B.; Dvorak, F.; Hermans, M.; Berkefeld, J.; Raabe, A.; Neumann-Haefelin, T.; Steinmetz, H.; Sitzer, M. Serum glial fibrillary acidic protein as a biomarker for intracerebral haemorrhage in patients with acute stroke. J. Neurol. Neurosurg. Psychiatry 2006, 77, 181–184. [Google Scholar] [CrossRef] [Green Version]
- Morgenstern, L.B.; Hemphill, J.C.; Anderson, C.; Becker, K.; Broderick, J.P.; Connolly, E.S.; Greenberg, S.M.; Huang, J.N.; MacDonald, R.L.; Messé, S.R.; et al. Guidelines for the management of spontaneous intracerebral hemorrhage: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2010, 41, 2108–2129. [Google Scholar] [CrossRef] [Green Version]
- Taqi, M.A.; Sodhi, A.; Suriya, S.; Quadri, S.; Farooqui, M.; Salvucci, A.; Stefansen, A.; Mortazavi, M.; Shepherd, D. Application and In field Validation of a Pre-Hospital Emergent Large Vessel Occlusion Screening Tool: Ventura Emergent Large Vessel Occlusion Score. J. Stroke Cerebrovasc. Dis. 2019, 28, 728–734. [Google Scholar] [CrossRef] [PubMed]
- Gropen, T.I.; Gazi, M.; Minor, M.; Fadairo, A.; Acker, J. Centrally Guided Identification of Patients With Large Vessel Occlusion: Lessons From Trauma Systems. J. Stroke Cerebrovasc. Dis. 2019, 28, 2388–2397. [Google Scholar] [CrossRef]
- Brouns, R.; Van Den Bossche, J.; De Surgeloose, D.; Sheorajpanday, R.; De Deyn, P.P. Clinical and biochemical diagnosis of small-vessel disease in acute ischemic stroke. J. Neurol. Sci. 2009, 285, 185–190. [Google Scholar] [CrossRef] [PubMed]
- Allen, M.; Pearn, K.; James, M.; Ford, G.A.; White, P.; Rudd, A.G.; McMeekin, P.; Stein, K. Maximising access to thrombectomy services for stroke in England: A modelling study. Eur. Stroke J. 2019, 4, 39–49. [Google Scholar] [CrossRef] [PubMed]
- Glickman, S.W.; Phillips, S.; Anstrom, K.J.; Laskowitz, D.T.; Cairns, C.B. Discriminative capacity of biomarkers for acute stroke in the emergency department. J. Emerg. Med. 2011, 41, 333–339. [Google Scholar] [CrossRef]
- Sibon, I.; Rouanet, F.; Meissner, W.; Orgogozo, J.M. Use of the Triage Stroke Panel in a neurologic emergency service. Am. J. Emerg. Med. 2009, 27, 558–562. [Google Scholar] [CrossRef]
- Karakece, E.; Ciftci, I.H.; Koroglu, M.; Ozbek, A. Evaluation of The Effect of Storage Temperature on D-dimer Stability, Using Two Different Techniques. J. Microbiol. Exp. 2016, 3, 3–5. [Google Scholar] [CrossRef]
- Hondow, J.A.; Russell, W.J.; Tunbridge, L.J.; Lloyd, J.V. Stability of Von Willebrand Factor in Blood Stored at 4 °C. Thromb. Res. 1982, 125–130. [Google Scholar] [CrossRef]
- Saleem, Y.; Nogueira, R.G.; Rodrigues, G.M.; Kim, S.; Sharashidze, V.; Frankel, M.; Al-Bayati, A.; Bianchi, N.; Haussen, D.C. Acute Neurological Deterioration in Large Vessel Occlusions and Mild Symptoms Managed Medically. Stroke 2020, 51, 1428–1434. [Google Scholar] [CrossRef]
- Woodward, M.; Lowe, G.D.O.; Francis, L.M.A.; Rumley, A.; Cobbe, S.M.; Bain, R.; Dean, J.; Fulcher, R.; Gershlick, A.; Haywood, G.; et al. A randomized comparison of the effects of aspirin and clopidogrel on thrombotic risk factors and C-reactive protein following myocardial infarction: The CADET trial. J. Thromb. Haemost. 2004, 2, 1934–1940. [Google Scholar] [CrossRef] [PubMed]
- Legnani, C.; Martinelli, I.; Palareti, G.; Ciavarella, A.; Poli, D.; Ageno, W.; Testa, S.; Mastroiacovo, D.; Ciammaichella, M.; Bucherini, E.; et al. D-dimer levels during and after anticoagulation withdrawal in patients with venous thromboembolism treated with non-Vitamin K anticoagulants. PLoS ONE 2019, 14, e0219751. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Clinical Characteristics | LVO Mean (SD 1) | Non-LVO Mean (SD 1) | p-Value |
|---|---|---|---|
| Sex (F/M) | 11/12 | 60/45 | 0.90 |
| Age | 75 (13) | 77 (21) | 1 |
| Atrial fibrillation (% yes) | 52 | 10 | <0.001 |
| Systolic blood pressure | 140 (22) | 157 (29) | 0.03 |
| Diastolic blood pressure | 80 (24) | 83 (18) | 0.85 |
| Hypertension (% yes) | 70 | 58 | 0.85 |
| APTT | 29 (5) | 30 (6) | 0.87 |
| Hematocrit | 0.38 (0.07) | 0.41 (0.06) | 0.78 |
| Prothrombin time | 12 (0) | 12 (1) | 0.81 |
| Fibrinogen | 4.9 (1.3) | 4.7 (1.1) | 0.87 |
| Platelet count | 227 (76) | 247 (85) | 0.85 |
| Glucose | 6.8 (2.8) | 6.0 (2.1) | 0.21 |
| NIHSS score | 18 (9) | 3 (5) | <0.001 |
| OBT (min) 2 | 155 (179) | 161 (154) | 1 |
| Model | AIC 1 | AUC 2 | LR 3 (df), p-Value |
|---|---|---|---|
| C-STAT | 102.36 | 79 (72–86) | - |
| C-STAT + D-dimer + GFAP | 79.29 | 88 (81–94) | 27.3 (4), <0.001 |
| EMSA | 89.75 | 84 (79–89) | - |
| EMSA + D-dimer + GFAP | 70.34 | 93 (89–97) | 23.4 (4), <0.001 |
| FAST | 93.35 | 83 (78–88) | - |
| FAST + D-dimer + GFAP | 71.82 | 93 (90–97) | 25.5 (4), <0.001 |
| FAST-ED | 78.25 | 91 (86–95) | - |
| FAST-ED + D-dimer + GFAP | 51.12 | 95 (91–100) | 31.1 (4), <0.001 |
| RACE | 78.87 | 87 (82–93) | - |
| RACE + D-dimer + GFAP | 59.21 | 93 (89–98) | 23.7 (4), <0.001 |
| Model | Accuracy | Sensitivity | Specificity | LR+ | LR− |
|---|---|---|---|---|---|
| C-STAT | 84 (79–88) | 35 (19–49) | 95 (92–98) | 8 (3–20) | 0.69 (0.54–0.85) |
| C-STAT + D-dimer + GFAP | 89 (79–96) | 74 (52–90) | 93 (86–97) | 10 (5–22) | 0.28 (0.14–0.56) |
| EMSA | 79 (73–84) | 65 (50–80) | 82 (76–87) | 3.7 (2.5–5.3) | 0.42 (0.24–0.6) |
| EMSA + D-dimer + GFAP | 93 (84–98) | 87 (66–97) | 95 (89–98) | 17 (7–41) | 0.14 (0.05–0.39) |
| FAST | 73 (67–78) | 91 (83–96) | 69 (62–75) | 2.9 (2.3–3.7) | 0.13 (0.06–0.25) |
| FAST + D-dimer + GFAP | 90 (80–96) | 78 (56–93) | 93 (86–97) | 11 (5–23) | 0.23 (0.11–0.51) |
| FAST-ED | 84 (78–88) | 83 (71–95) | 84 (79–89) | 5.3 (3.6–7.6) | 0.21 (0.06–0.35) |
| FAST-ED + D-dimer + GFAP | 95 (87–99) | 91 (72–99) | 96 (90–99) | 23 (9–60) | 0.09 (0.02–0.34) |
| RACE | 86 (82–91) | 70 (56–85) | 90 (86–94) | 7.3 (4.6–12.4) | 0.33 (0.17–0.49) |
| RACE + D-dimer + GFAP | 91 (81–97) | 83 (61–95) | 93 (86–97) | 12 (6–24) | 0.19 (0.08–0.46) |
| Model | Accuracy | Sensitivity | Specificity | LR+ | LR− |
|---|---|---|---|---|---|
| C-STAT | 89 (85–93) | 65 (47–82) | 93 (90–97) | 11 (6–20) | 0.38 (0.2–0.57) |
| C-STAT + D-dimer + GFAP | 89 (78–96) | 71 (44–90) | 92 (85–97) | 9 (4–20) | 0.32 (0.15–0.67) |
| EMSA | 69 (63–75) | 100 (100–100) | 63 (56–70) | 3 (2–3) | 0 (0–0) |
| EMSA + D-dimer + GFAP | 90 (79–96) | 88 (64–99) | 90 (82–95) | 9 (5–17) | 0.13 (0.04–0.48) |
| FAST | 89 (85–93) | 65 (47–81) | 93 (90–97) | 11 (6–23) | 0.38 (0.2–0.56) |
| FAST + D-dimer + GFAP | 88 (77–95) | 71 (44–90) | 91 (83–96) | 8 (4–16) | 0.32 (0.15–0.68) |
| FAST-ED | 89 (85–93) | 88 (77–100) | 89 (84–93) | 8 (6–14) | 0.13 (0–0.26) |
| FAST-ED + D-dimer + GFAP | 95 (87–99) | 82 (57–96) | 98 (92–100) | 37 (9–148) | 0.18 (0.06–0.5) |
| RACE | 87 (82–92) | 88 (77–100) | 87 (81–92) | 7 (5–11) | 0.14 (0–0.26) |
| RACE + D-dimer + GFAP | 91 (80–97) | 82 (57–96) | 92 (85–97) | 11 (5–22) | 0.19 (0.07–0.54) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gaude, E.; Nogueira, B.; Ladreda Mochales, M.; Graham, S.; Smith, S.; Shaw, L.; Graziadio, S.; Ladreda Mochales, G.; Sloan, P.; Bernstock, J.D.; et al. A Novel Combination of Blood Biomarkers and Clinical Stroke Scales Facilitates Detection of Large Vessel Occlusion Ischemic Strokes. Diagnostics 2021, 11, 1137. https://doi.org/10.3390/diagnostics11071137
Gaude E, Nogueira B, Ladreda Mochales M, Graham S, Smith S, Shaw L, Graziadio S, Ladreda Mochales G, Sloan P, Bernstock JD, et al. A Novel Combination of Blood Biomarkers and Clinical Stroke Scales Facilitates Detection of Large Vessel Occlusion Ischemic Strokes. Diagnostics. 2021; 11(7):1137. https://doi.org/10.3390/diagnostics11071137
Chicago/Turabian StyleGaude, Edoardo, Barbara Nogueira, Marcos Ladreda Mochales, Sheila Graham, Sarah Smith, Lisa Shaw, Sara Graziadio, Gonzalo Ladreda Mochales, Philip Sloan, Joshua D. Bernstock, and et al. 2021. "A Novel Combination of Blood Biomarkers and Clinical Stroke Scales Facilitates Detection of Large Vessel Occlusion Ischemic Strokes" Diagnostics 11, no. 7: 1137. https://doi.org/10.3390/diagnostics11071137
APA StyleGaude, E., Nogueira, B., Ladreda Mochales, M., Graham, S., Smith, S., Shaw, L., Graziadio, S., Ladreda Mochales, G., Sloan, P., Bernstock, J. D., Shekhar, S., Gropen, T. I., & Price, C. I. (2021). A Novel Combination of Blood Biomarkers and Clinical Stroke Scales Facilitates Detection of Large Vessel Occlusion Ischemic Strokes. Diagnostics, 11(7), 1137. https://doi.org/10.3390/diagnostics11071137






