Pediatric Abusive Head Trauma: A Systematic Review
Abstract
1. Introduction
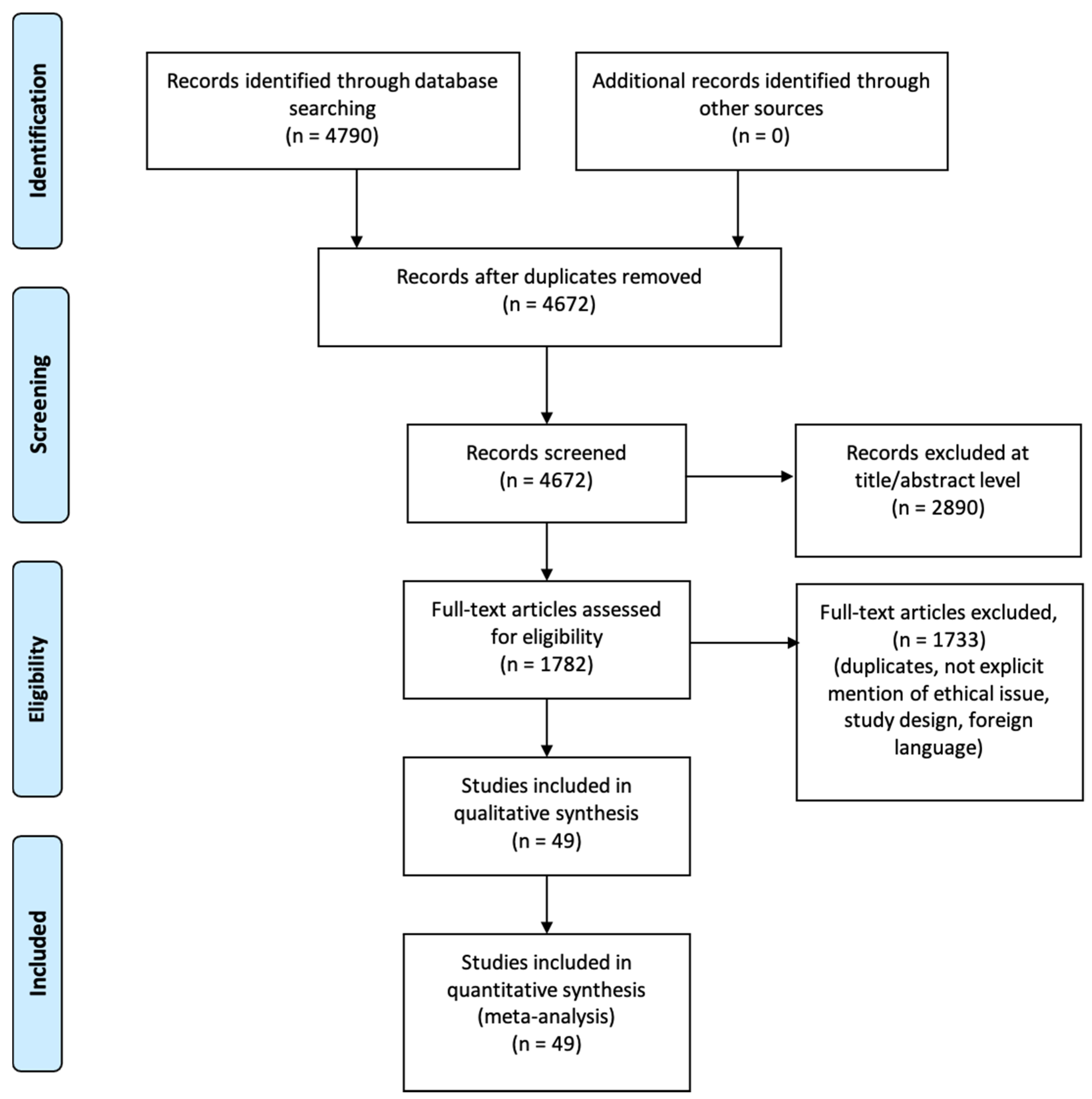
2. Materials and Methods
2.1. Eligibility Criteria
2.2. Search Criteria and Critical Appraisal
3. Results
3.1. Search Results and Included Studies
- Estimate diagnosis process;
- Clinical features analyzed;
- Circumstantial data evaluation;
- Post-mortem evaluation;
- Study design.
3.2. Risk of Bias
4. Discussion
4.1. Clinical Findings
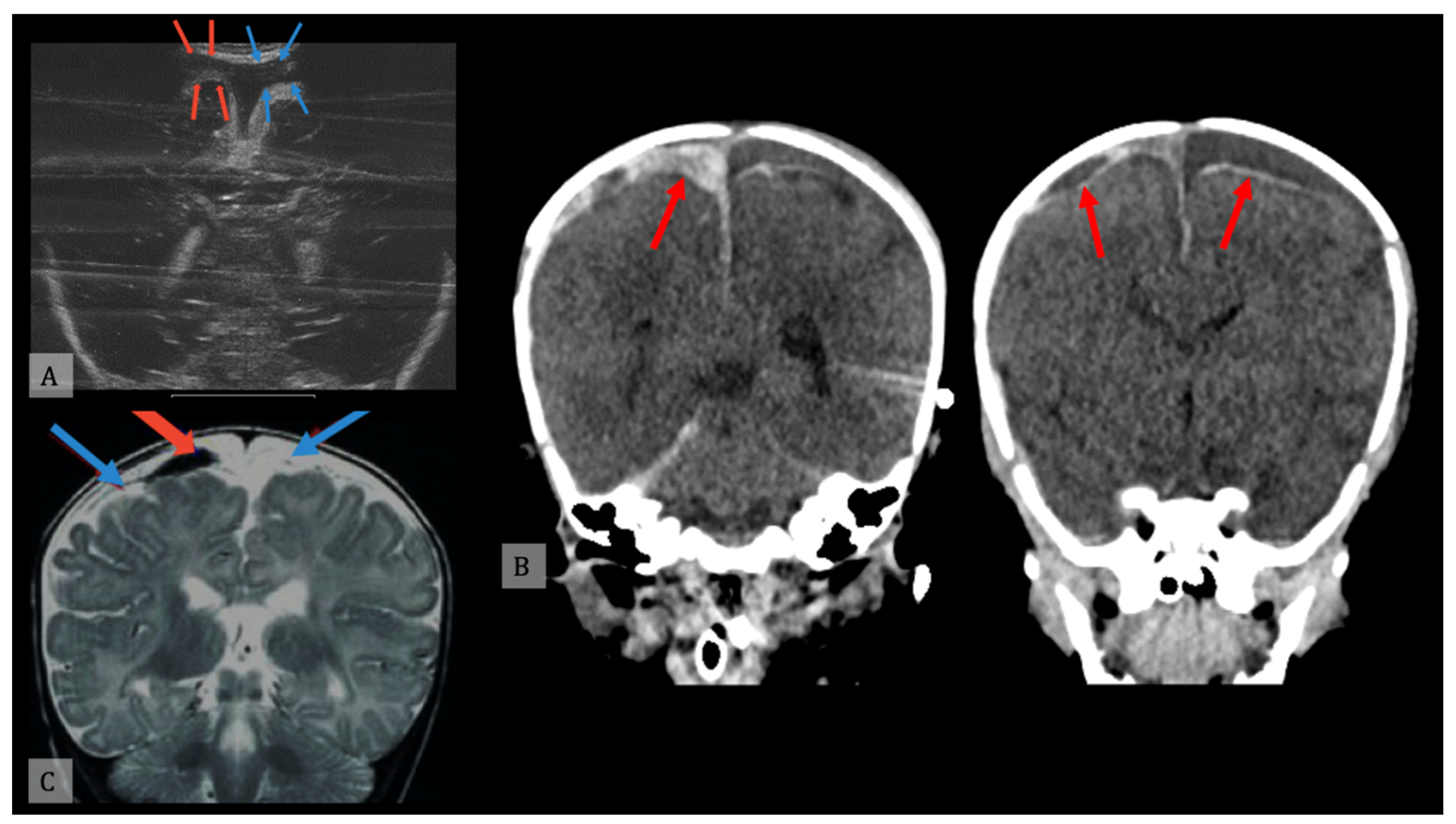
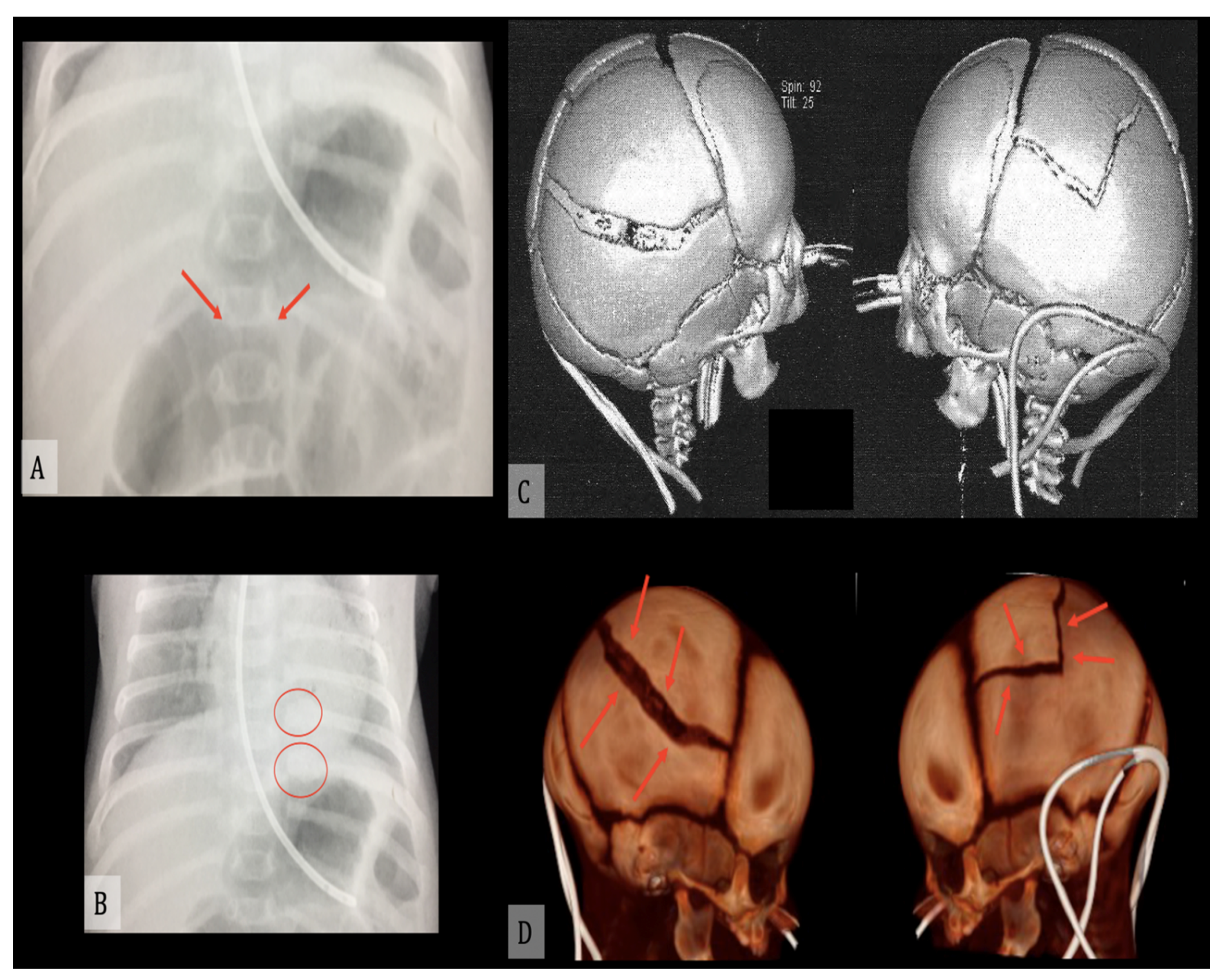
4.1.1. Radiology
4.1.2. Ophthalmological Examination
4.2. Forensic Pathology
4.2.1. Post-Mortem CT
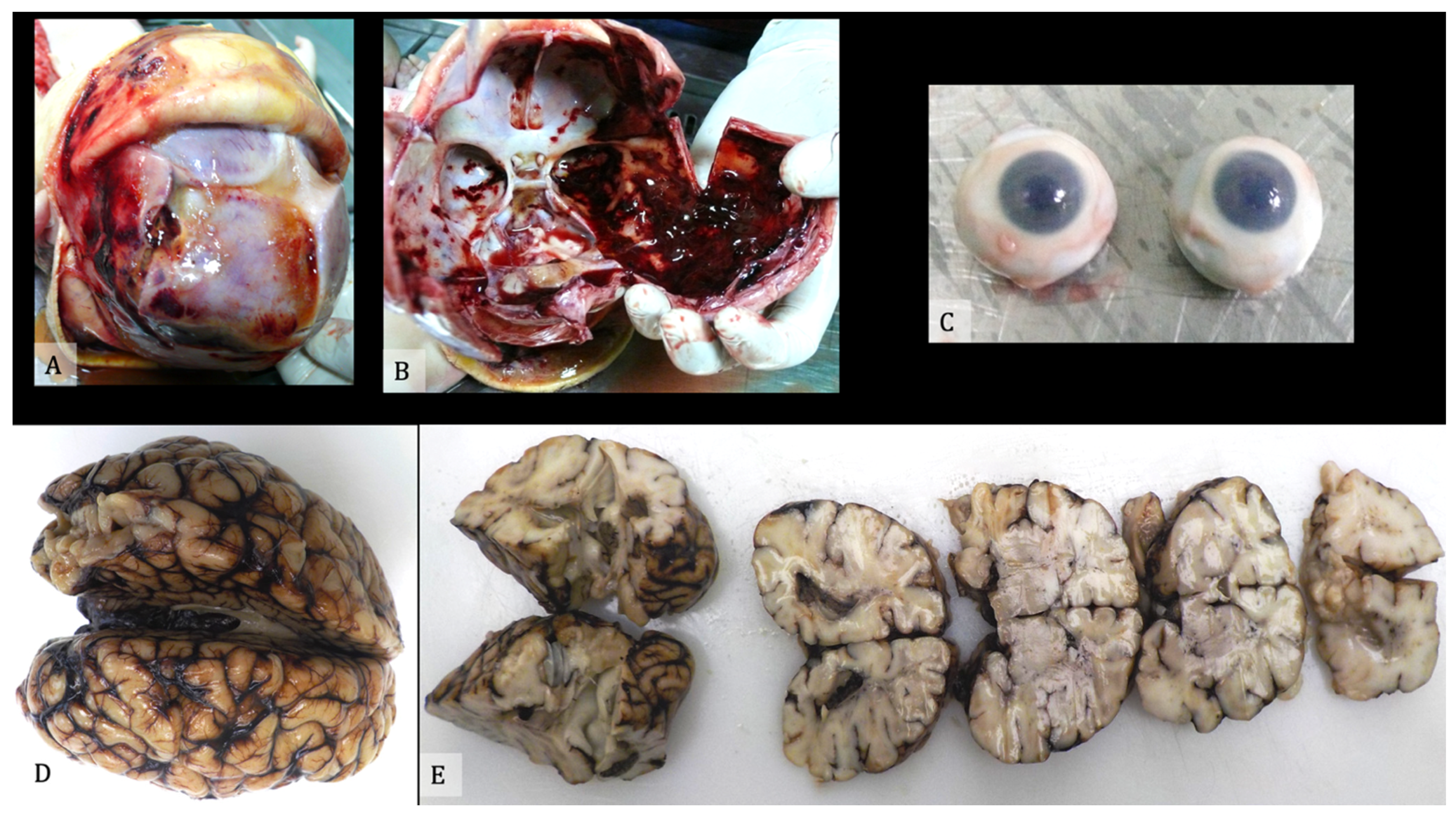
4.2.2. Autopsy
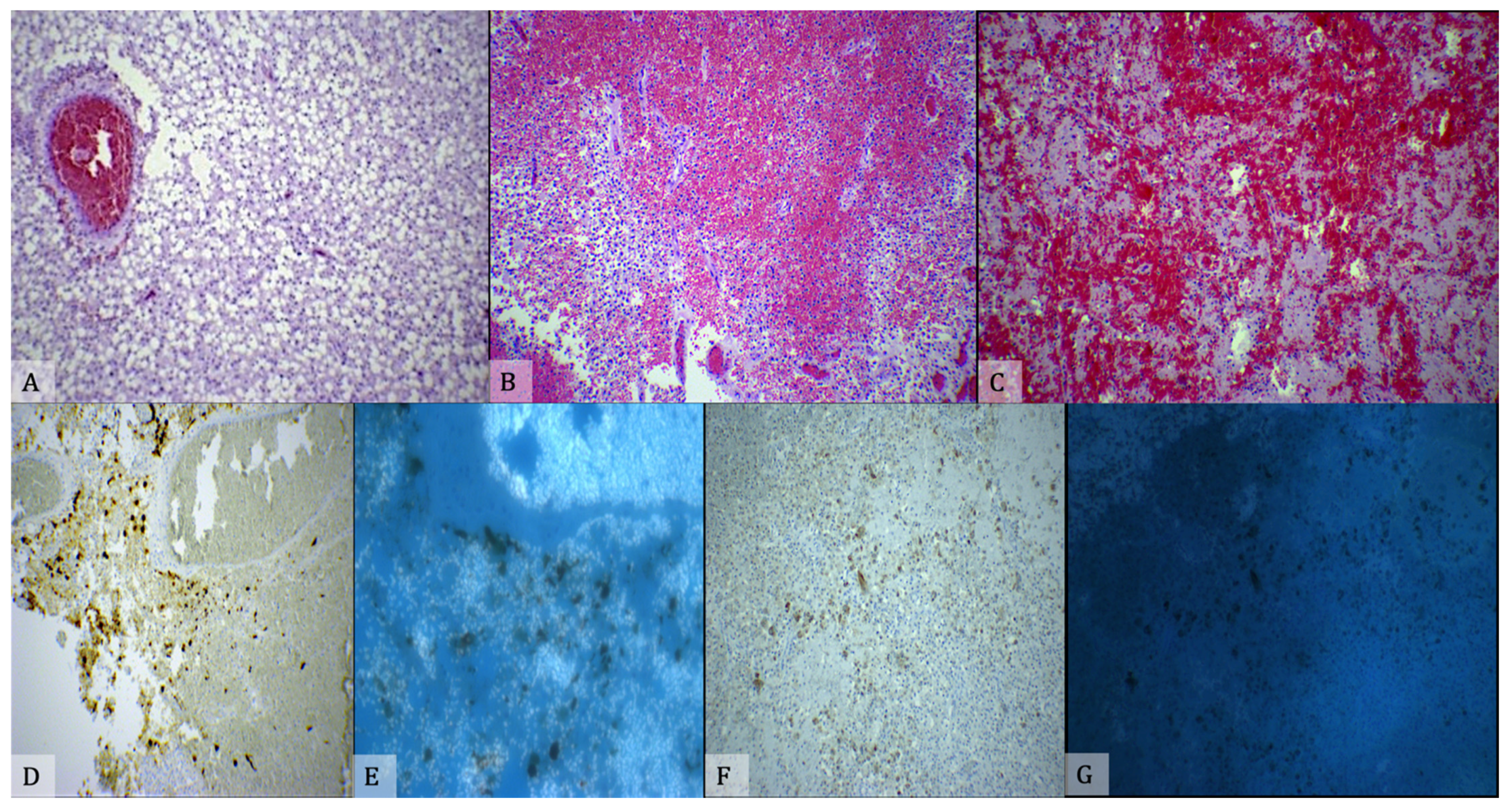
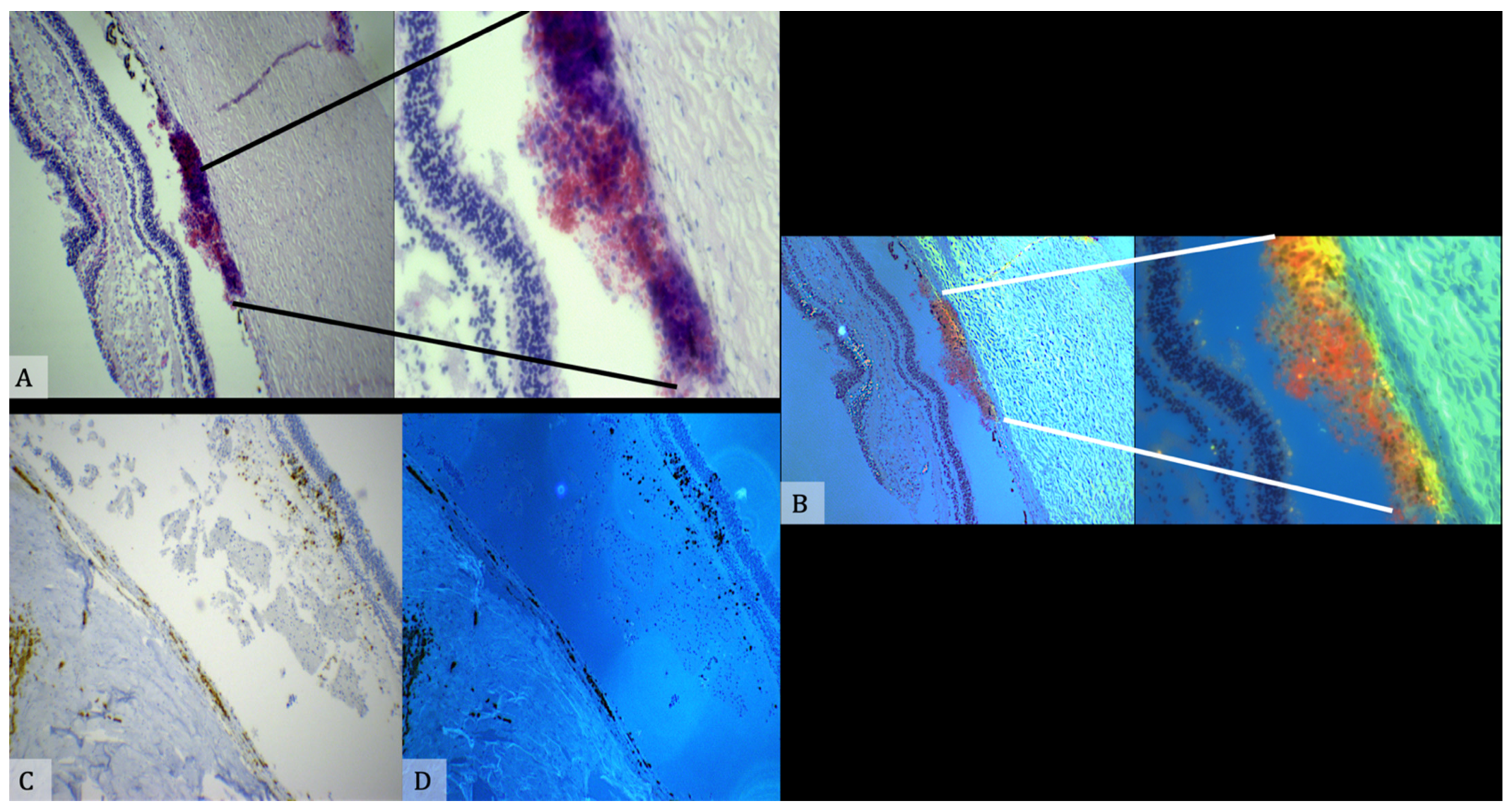
4.2.3. Histology
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Christian, C.W.; Block, R. Abusive head trauma in infants and children. Pediatrics 2009, 123, 1409–1411. [Google Scholar] [CrossRef]
- Parks, S.E.; Annest, J.L.; Hill, H.A.; Karch, D.L. Pediatric Abusive Head Trauma: Recommended Definitions for Public Health Surveillance and Research; National Center for Injury Prevention and Control (U.S.), Division of Violence Prevention: Atlanta, GA, USA, 2012.
- Babl, F.E.; Pfeiffer, H.; Kelly, P.; Dalziel, S.R.; Oakley, E.; Borland, M.L.; Kochar, A.; Dalton, S.; Cheek, J.A.; Gilhotra, Y.; et al. Paediatric abusive head trauma in the emergency department: A multicentre prospective cohort study. J. Paediatr. Child Health 2020, 56, 615–621. [Google Scholar] [CrossRef] [PubMed]
- Greeley, C.S. Abusive head trauma: A review of the evidence base. AJR. Am. J. Roentgenol. 2015, 204, 967–973. [Google Scholar] [CrossRef] [PubMed]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ 2009, 339, b2700. [Google Scholar] [CrossRef] [PubMed]
- Minns, R.A.; Jones, P.A.; Tandon, A.; Fleck, B.W.; Mulvihill, A.O.; Elton, R.A. Prediction of inflicted brain injury in infants and children using retinal imaging. Pediatrics 2012, 130, e1227–e1234. [Google Scholar] [CrossRef]
- Squier, W. The “Shaken Baby” syndrome: Pathology and mechanisms. Acta Neuropathol. 2011, 122, 519–542. [Google Scholar] [CrossRef] [PubMed]
- Parks, S.; Sugerman, D.; Xu, L.; Coronado, V. Characteristics of non-fatal abusive head trauma among children in the USA, 2003–2008: Application of the CDC operational case definition to national hospital inpatient data. Inj. Prev. 2012, 18, 392–398. [Google Scholar] [CrossRef] [PubMed]
- Levin, A.V.; Christian, C.W.; Committee on Child Abuse and Neglect; Section on Ophthalmology. The eye examination in the evaluation of child abuse. Pediatrics 2010, 126, 376–380. [Google Scholar] [CrossRef] [PubMed]
- Bartschat, S.; Richter, C.; Stiller, D.; Banschak, S. Long-term outcome in a case of shaken baby syndrome. Med. Sci. Law 2016, 56, 147–149. [Google Scholar] [CrossRef]
- Hung, K.L. Pediatric abusive head trauma. Biomed. J. 2020, 43, 240–250. [Google Scholar] [CrossRef]
- Yu, Y.R.; DeMello, A.S.; Greeley, C.S.; Cox, C.S.; Naik-Mathuria, B.J.; Wesson, D.E. Injury patterns of child abuse: Experience of two Level 1 pediatric trauma centers. J. Pediatr. Surg. 2018, 53, 1028–1032. [Google Scholar] [CrossRef]
- Mian, M.; Shah, J.; Dalpiaz, A.; Schwamb, R.; Miao, Y.; Warren, K.; Khan, S. Shaken Baby Syndrome: A review. Fetal Pediatr. Pathol. 2015, 34, 169–175. [Google Scholar] [CrossRef] [PubMed]
- Schelhorn, J.; Gramsch, C.; Deuschl, C.; Quick, H.H.; Nensa, F.; Moenninghoff, C.; Schlamann, M. Intracranial hemorrhage detection over time using susceptibility-weighted magnetic resonance imaging. Acta Radiol. 2015, 56, 1501–1507. [Google Scholar] [CrossRef]
- Adamsbaum, C.; Morel, B.; Ducot, B.; Antoni, G.; Rey-Salmon, C. Dating the abusive head trauma episode and perpetrator statements: Key points for imaging. Pediatr. Radiol. 2014, 44, S578–S588. [Google Scholar] [CrossRef]
- Wootton-Gorges, S.L.; Soares, B.P.; Alazraki, A.L.; Anupindi, S.A.; Blount, J.P.; Booth, T.N.; Dempsey, M.E.; Falcone, R.A.; Hayes, L.L.; Kulkarni, A.V.; et al. ACR appropriateness criteria® suspected physical abuse-child. J. Am. Coll. Radiol. 2017, 14, S338–S349. [Google Scholar] [CrossRef]
- Maguire, S.A.; Watts, P.O.; Shaw, A.D.; Holden, S.; Taylor, R.H.; Watkins, W.J.; Mann, M.K.; Tempest, V.; Kemp, A.M. Retinal haemorrhages and related findings in abusive and non-abusive head trauma: A systematic review. Eye 2013, 27, 28–36. [Google Scholar] [CrossRef]
- Vinchon, M.; de Foort-Dhellemmes, S.; Desurmont, M.; Delestret, I. Confessed abuse versus witnessed accidents in infants: Comparison of clinical, radiological, and ophthalmological data in corroborated cases. Childs Nerv. Syst. 2010, 26, 637–645. [Google Scholar] [CrossRef]
- Binenbaum, G.; Christian, C.W.; Ichord, R.N.; Ying, G.S.; Simon, M.A.; Romero, K.; Pollock, A.N.; Forbes, B.J. Retinal hemorrhage and brain injury patterns on diffusion-weighted magnetic resonance imaging in children with head trauma. J. AAPOS 2013, 17, 603–608. [Google Scholar] [CrossRef] [PubMed]
- Christian, C.W.; Levin, A.V.; Council on Child Abuse and Neglect; Section on Ophthalmology; American Association of Certified Orthoptists; American Association for Pediatric Ophthalmology and Strabismus; American Academy of Ophthalmology. The eye examination in the evaluation of child abuse. Pediatrics 2018, 142, e20181411. [Google Scholar] [CrossRef] [PubMed]
- Binenbaum, G.; Rogers, D.L.; Forbes, B.J.; Levin, A.V.; Clark, S.A.; Christian, C.W.; Liu, G.T.; Avery, R. Patterns of retinal hemorrhage associated with increased intracranial pressure in children. Pediatrics 2013, 132, e430–e434. [Google Scholar] [CrossRef]
- Bhardwaj, G.; Chowdhury, V.; Jacobs, M.B.; Moran, K.T.; Martin, F.J.; Coroneo, M.T. A systematic review of the diagnostic accuracy of ocular signs in pediatric abusive head trauma. Ophthalmology 2010, 117, 983–992. [Google Scholar] [CrossRef]
- Choudhary, A.K.; Servaes, S.; Slovis, T.L.; Palusci, V.J.; Hedlund, G.L.; Narang, S.K.; Moreno, J.A.; Dias, M.S.; Christian, C.W.; Nelson, M.D., Jr.; et al. Consensus statement on abusive head trauma in infants and young children. Pediatr Radiol. 2018, 48, 1048–1065. [Google Scholar] [CrossRef]
- Elinder, G.; Eriksson, A.; Hallberg, B.; Lynøe, N.; Sundgren, P.M.; Rosén, M.; Engström, I.; Erlandsson, B.E. Traumatic shaking: The role of the triad in medical investigations of suspected traumatic shaking. Acta Paediatr. 2018, 107, 3–23. [Google Scholar] [CrossRef]
- Bradford, R.; Choudhary, A.K.; Dias, M.S. Serial neuroimaging in infants with abusive head trauma: Timing abusive injuries. J. Neurosurg. Pediatr. 2013, 12, 110–119. [Google Scholar] [CrossRef]
- Agrawal, S.; Peters, M.J.; Adams, G.G.W.; Pierce, C.M. Prevalence of retinal hemorrhages in critically ill children. Pediatrics 2012, 129, e1388–e1396. [Google Scholar] [CrossRef]
- Gekat, W.; Binder, S.; Wetzel, C.; Rothschild, M.A.; Banaschak, S. SDH and EDH in children up to 18 years of age—A clinical collective in the view of forensic considerations. Int. J. Legal Med. 2018, 132, 1719–1727. [Google Scholar] [CrossRef] [PubMed]
- Zuccoli, G.; Panigrahy, A.; Haldipur, A.; Willaman, D.; Squires, J.; Wolford, J.; Sylvester, C.; Mitchell, E.; Lope, L.A.; Nischal, K.K.; et al. Susceptibility weighted imaging depicts retinal hemorrhages in abusive head trauma. Neuroradiology 2013, 55, 889–893. [Google Scholar] [CrossRef]
- Mulvihill, A.O.; Jones, P.; Tandon, A.; Fleck, B.W.; Minns, R.A. An inter-observer and intra-observer study of a classification of RetCam images of retinal haemorrhages in children. Br. J. Ophthalmol. 2011, 95, 99–104. [Google Scholar] [CrossRef]
- Barnes, P.D.; Galaznik, J.; Gardner, H.; Shuman, M. Infant acute life-threatening event—Dysphagic choking versus nonaccidental injury. Semin. Pediatr. Neurol. 2010, 17, 7–11. [Google Scholar] [CrossRef] [PubMed]
- Miller, D.; Barnes, P.; Miller, M. The significance of macrocephaly or enlarging head circumference in infants with the triad: Further evidence of mimics of shaken baby syndrome. Am. J. Forensic Med. Pathol. 2015, 36, 111–120. [Google Scholar] [CrossRef] [PubMed]
- Carrim, Z.I.; Arbabi, E.M.; Long, V.W. Presumed non-accidental injury with retinal haemorrhages—Findings from a tertiary referral centre in the United Kingdom. Brain Inj. 2010, 26, 1716–1722. [Google Scholar] [CrossRef]
- Adamsbaum, C.; Grabar, S.; Mejean, N.; Rey-Salmon, C. Abusive head trauma: Judicial admissions highlight violent and repetitive shaking. Pediatrics 2010, 126, 546–555. [Google Scholar] [CrossRef]
- Kemp, A.M.; Jaspan, T.; Griffiths, J.; Stoodley, N.; Mann, M.K.; Tempest, V.; Maguire, S.A. Neuroimaging: What neuroradiological features distinguish abusive from non-abusive head trauma? A systematic review. Arch. Dis. Child. 2011, 96, 1103–1112. [Google Scholar] [CrossRef]
- Maguire, S.A.; Kemp, A.M.; Lumb, R.C.; Farewell, D.M. Estimating the probability of abusive head trauma: A pooled analysis. Pediatrics 2011, 128, e550–e564. [Google Scholar] [CrossRef]
- Wu, A.L.; See, L.C.; Hsia, S.H.; Tu, H.T.; Wang, N.K.; Huang, J.L.; Hwang, Y.S.; Lai, C.C.; Wu, W.C. Pediatric abusive head trauma in Taiwan: Clinical characteristics and risk factors associated with mortality. Graefes. Arch. Clin. Exp. Ophthalmol. 2018, 256, 997–1003. [Google Scholar] [CrossRef]
- Fraser, J.A.; Flemington, T.; Doan, T.N.D.; Hoang, M.T.V.; Doan, T.L.B.; Ha, M.T. Prevention and recognition of abusive head trauma: Training for healthcare professionals in Vietnam. Acta Paediatr. 2017, 106, 1608–1616. [Google Scholar] [CrossRef] [PubMed]
- Loredo-Abdalá, A.; Casas-Muñoz, A.; Villanueva-Clift, H.J.; Aguilar-Ceniceros, A.; González-Garay, A.G.; Gutiérrez-Leyva, C.J.; Juarez Olguin, H. Pediatric abusive head trauma: Multicentric experience in Mexico. J. Interpers. Violence 2020, 20, 886260520916283. [Google Scholar] [CrossRef] [PubMed]
- Miller Ferguson, N.; Sarnaik, A.; Miles, D.; Shafi, N.; Peters, M.J.; Truemper, E.; Vavilala, M.S.; Bell, M.J.; Wisniewski, S.R.; Luther, J.F.; et al. Investigators of the approaches and decisions in acute pediatric traumatic brain injury (ADAPT) trial. Abusive head trauma and mortality-an analysis from an international comparative effectiveness study of children with severe traumatic brain injury. Crit. Care Med. 2017, 45, 1398–1407. [Google Scholar] [CrossRef] [PubMed]
- Thamburaj, K.; Soni, A.; Frasier, L.D.; Tun, K.N.; Weber, S.R.; Dias, M.S. Susceptibility-weighted imaging of retinal hemorrhages in abusive head trauma. Pediatr Radiol. 2019, 49, 210–216. [Google Scholar] [CrossRef]
- Andersson, J.; Thiblin, I. National study shows that abusive head trauma mortality in Sweden was at least 10 times lower than in other Western countries. Acta Paediatr. 2018, 107, 477–483. [Google Scholar] [CrossRef]
- Morgan, L.A.; Jain, S.F.; Svec, A.; Svec, C.; Haney, S.B.; Allbery, S.; High, R.; Suh, D.W. Clinical comparison of ocular and systemic findings in diagnosed cases of abusive and non-abusive head trauma. Clin. Ophthalmol. 2018, 12, 1505–1510. [Google Scholar] [CrossRef]
- Gencturk, M.; Tore, H.G.; Nascene, D.R.; Zhang, L.; Koksel, Y.; McKinney, A.M. Various cranial and orbital imaging findings in pediatric abusive and non-abusive head trauma, and relation to outcomes. Clin. Neuroradiol. 2019, 29, 253–261. [Google Scholar] [CrossRef]
- Sidpra, J.; Jeelani, N.U.O.; Ong, J.; Birch, W.; Mankad, K. Skull fractures in abusive head trauma: A single centre experience and review of the literature. Childs Nerv. Syst. 2021, 37, 919–929. [Google Scholar] [CrossRef] [PubMed]
- Wright, J.; Painter, S.; Kodagali, S.S.; Jones, N.R.; Roalfe, A.; Jayawant, S.; Elston, J.; Anand, G. Disability and visual outcomes following suspected abusive head trauma in children under 2 years. Arch. Dis. Child. 2020, 14, 2019–318638. [Google Scholar] [CrossRef] [PubMed]
- Donaldson, L.; Isaza, G.; Baird, B.; Chaudhary, V. Ophthalmology referral as part of a multidisciplinary approach to suspected abusive head trauma. Can. J. Ophthalmol. 2020, 55, 172–178. [Google Scholar] [CrossRef] [PubMed]
- Payne, F.L.; Fernandez, D.N.; Jenner, L.; Paul, S.P. Recognition and nursing management of abusive head trauma in children. Br. J. Nurs. 2017, 26, 974–981. [Google Scholar] [CrossRef] [PubMed]
- Levin, A.V. Retinal hemorrhage in abusive head trauma. Pediatrics 2010, 126, 961–970. [Google Scholar] [CrossRef]
- Drubach, L.A.; Johnston, P.R.; Newton, A.W.; Perez-Rossello, J.M.; Grant, F.D.; Kleinman, P.K. Skeletal trauma in child abuse: Detection with 18F-NaF PET. Radiology 2010, 255, 173–181. [Google Scholar] [CrossRef]
- Laghmari, M.; Skiker, H.; Handor, H.; Mansouri, B.; Chahdi, K.O.; Lachkar, R.; Salhi, Y.; Cherkaoui, O.; Ouazzani Tnacheri, B.; Ibrahimy, W.; et al. Birth-related retinal hemorrhages in the newborn: Incidence and relationship with maternal, obstetric and neonatal factors. Prospective study of 2,031 cases. J. Fr. Ophtalmol. 2014, 37, 313–319. [Google Scholar] [CrossRef]
- Breazzano, M.P.; Unkrich, K.H.; Barker-Griffith, A.E. Clinicopathological findings in abusive head trauma: Analysis of 110 infant autopsy eyes. Am. J. Ophthalmol. 2014, 158, 1146–1154.e2. [Google Scholar] [CrossRef]
- Piteau, S.J.; Ward, M.G.K.; Barrowman, N.J.; Plint, A.C. Clinical and radiographic characteristics associated with abusive and nonabusive head trauma: A systematic review. Pediatrics 2012, 130, 315–323. [Google Scholar] [CrossRef] [PubMed]
- Feld, K.; Feld, D.; Karger, B.; Helmus, J.; Schwimmer-Okike, N.; Pfeiffer, H.; Banaschak, S.; Wittschieber, D. Abusive head trauma in Court: A multi-center study on criminal proceedings in Germany. Int. J. Legal Med. 2021, 135, 235. [Google Scholar] [CrossRef]
- Cartocci, G.; Fineschi, V.; Padovano, M.; Scopetti, M.; Rossi-Espagnet, M.C.; Giannì, C. Shaken baby syndrome: Magnetic resonance imaging features in abusive head trauma. Brain Sci. 2021, 11, 179. [Google Scholar] [CrossRef]
- Verdijk, R.M.; Herwig-Carl, M.C. Fetal and Neonatal Eye Pathology; Springer: Cham, Switzerland, 2020. [Google Scholar]
- Rambaud, C. Bridging veins and autopsy findings in abusive head trauma. Pediatr. Radiol. 2015, 45, 1126–1131. [Google Scholar] [CrossRef]
- Suvarna, S.K. Atlas of Adult Autopsy: A Guide to Modern Practice; Springer International Publishing: Cham, Switzerland, 2016; pp. 292–294. [Google Scholar]
- Case, M.E. Distinguishing accidental from inflicted head trauma at autopsy. Pediatr. Radiol. 2014, 44, S632–S640. [Google Scholar] [CrossRef] [PubMed]
- Pinchi, E.; Frati, A.; Cantatore, S.; D’Errico, S.; La Russa, R.; Maiese, A.; Palmieri, M.; Pesce, A.; Viola, R.V.; Frati, P.; et al. Acute spinal cord injury: A systematic review investigating miRNA families involved. Int. J. Mol. Sci. 2019, 20, 1841. [Google Scholar] [CrossRef]
- dell’Aquila, M.; Maiese, A.; De Matteis, A.; Viola, R.V.; Arcangeli, M.; La Russa, R.; Fineschi, V. Traumatic brain injury: Estimate of the age of the injury based on neuroinflammation, endothelial activation markers and adhesion molecules. Histol. Histopathol. 2021, 18319. [Google Scholar] [CrossRef]
- La Russa, R.; Maiese, A.; Di Fazio, N.; Morano, A.; Di Bonaventura, C.; De Matteis, A.; Fazio, V.; Frati, P.; Fineschi, V. Post-traumatic meningitis is a diagnostic challenging time: A systematic review focusing on clinical and pathological features. Int. J. Mol. Sci. 2020, 21, 4148. [Google Scholar] [CrossRef] [PubMed]
| Author | Title | Clinical History | Radiological Evaluation of the Brain and/or CNS | Ophthalmologic Evaluation | All Items |
|---|---|---|---|---|---|
| Minns et al. [6] | Prediction of inflicted brain injury in infants and children using retinal imaging | X | |||
| Squier [7] | The “Shaken Baby” syndrome: Pathology and mechanisms | X | |||
| Parks et al. [8] | Characteristics of non-fatal abusive head trauma among children in the USA, 2003–2008: Application of the CDC operational case definition to national hospital inpatient data | X | |||
| Levin and Christian [9] | The eye examination in the evaluation of child abuse | X | |||
| Bartschat et al. [10] | Long-term outcome in a case of shaken baby syndrome | X | |||
| Hung [11] | Pediatric abusive head trauma | X | |||
| Yu et al. [12] | Injury patterns of child abuse: experience of two level 1 pediatric trauma centers | X | |||
| Mian et al. [13] | Shaken baby syndrome: A review | X | |||
| Schelhorn et al. [14] | Intracranial hemorrhage detection over time using susceptibility-weighted magnetic resonance imaging | X | |||
| Adamsbaum et al. [15] | Dating the abusive head trauma episode and perpetrator statements: Key points for imaging | X | X | ||
| Wootton-Gorges et al. [16] | ACR appropriateness criteria® suspected physical abuse-child | X | X | ||
| Maguire et al. [17] | Retinal haemorrhages and related findings in abusive and non-abusive head trauma: A systematic review | X | X | ||
| Vinchon et al. [18] | Confessed abuse versus witnessed accidents in infants: Comparison of clinical, radiological, and ophthalmological data in corroborated cases | X | |||
| Binenbaum et al. [19] | Retinal hemorrhage and brain injury patterns on diffusion-weighted magnetic resonance imaging in children with head trauma | X | X | ||
| Christian et al. [20] | The eye examination in the evaluation of child abuse | X | |||
| Binenbaum et al. [21] | Patterns of retinal hemorrhage associated with increased intracranial pressure in children | X | |||
| Bhardwaj et al. [22] | A systematic review of the diagnostic accuracy of ocular signs in pediatric abusive head trauma | X | |||
| Choudhary et al. [23] | Consensus statement on abusive head trauma in infants and young children | X | |||
| Elinder et al. [24] | Traumatic shaking: The role of the triad in medical investigations of suspected traumatic shaking | X | |||
| Bradford et al. [25] | Serial neuroimaging in infants with abusive head trauma: Timing abusive injuries | X | X | ||
| Agrawal et al. [26] | Prevalence of retinal hemorrhages in critically ill children | X | |||
| Gekat et al. [27] | SDH and EDH in children up to 18 years of age—A clinical collective in the view of forensic consideration | X | X | ||
| Zuccoli et al. [28] | Susceptibility weighted imaging depicts retinal hemorrhages in abusive head trauma | X | |||
| Mulvihil et al. [29] | An inter-observer and intra-observer study of a classification of RetCam images of retinal haemorrhages in children | x | |||
| Barnes et al. [30] | Infant acute life-threatening event—Dysphagic choking versus nonaccidental injury | X | X | ||
| Miller et al. [31] | The significance of macrocephaly or enlarging head circumference in infants with the triad: Further evidence of mimics of shaken baby syndrome | X | |||
| Carrim et al. [32] | Presumed non-accidental injury with retinal haemorrhages—Findings from a tertiary referral centre in the United Kingdom | X | |||
| Adamsbaum et al. [33] | Abusive head trauma: Judicial admissions highlight violent and repetitive shaking | X | X | ||
| Kemp et al. [34] | Neuroimaging: What neuroradiological features distinguish abusive from non-abusive head trauma? A systematic review | X | |||
| Maguire et al. [35] | Estimating the probability of abusive head trauma: A pooled analysis | X | |||
| Wu et al. [36] | Pediatric abusive head trauma in Taiwan: Clinical characteristics and risk factors associated with mortality | X | |||
| Babl et al. [3] | Pediatric abusive head trauma in the emergency department: A multicentre prospective cohort study | X | |||
| Fraser et al. [37] | Prevention and recognition of abusive head trauma: Training for healthcare professionals in Vietnam | X | |||
| Loredo-Abdalá et al. [38] | Pediatric abusive trauma: Multicentric experience in Mexico | X | |||
| Ferguson et al. [39] | Abusive head trauma and mortality: An analysis from an international comparative effectiveness study of children with severe traumatic brain injury | X | |||
| Thamburaj et al. [40] | Susceptibility-weighted imaging of retinal hemorrhages in abusive head trauma | X | |||
| Andersson and Thiblin [41] | National study shows that abusive head trauma mortality in Sweden was at least 10 times lower than in other Western countries | X | X | ||
| Morgan et al. [42] | Clinical comparison of ocular and systemic findings in diagnosed cases of abusive and non-abusive head trauma | X | X | ||
| Gencturk et al. [43] | Various cranial and orbital imaging findings in pediatric abusive and non-abusive head trauma, and relation to outcomes | X | X | ||
| Sidpra et al. [44] | Skull fractures in abusive head trauma: A single centre experience and review of the literature | X | |||
| Wright et al. [45] | Disability and visual outcomes following suspected abusive head trauma in children under 2 years | X | |||
| Donaldson et al. [46] | Ophthalmology referral as part of a multidisciplinary approach to suspected abusive head trauma | X | |||
| Payne et al. [47] | Recognition and nursing management of abusive head trauma in children | X | X | ||
| Levin [48] | Retinal hemorrhage in abusive head trauma | X | |||
| Drubach et al. [49] | Skeletal trauma in child abuse: Detection with 18F-NaF PET | X | |||
| Laghmari et al. [50] | Birth-related retinal hemorrhages in the newborn: incidence and relationship with maternal, obstetric and neonatal factors. Prospective study of 2,031 cases | ||||
| Breazzano et al. [51] | Clinicopathological findings in abusive head trauma: analysis of 110 infant autopsy eyes | X | |||
| Piteau et al. [52] | Clinical and radiographic characteristics associated with abusive and nonabusive head trauma: A systematic review | X | X |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maiese, A.; Iannaccone, F.; Scatena, A.; Del Fante, Z.; Oliva, A.; Frati, P.; Fineschi, V. Pediatric Abusive Head Trauma: A Systematic Review. Diagnostics 2021, 11, 734. https://doi.org/10.3390/diagnostics11040734
Maiese A, Iannaccone F, Scatena A, Del Fante Z, Oliva A, Frati P, Fineschi V. Pediatric Abusive Head Trauma: A Systematic Review. Diagnostics. 2021; 11(4):734. https://doi.org/10.3390/diagnostics11040734
Chicago/Turabian StyleMaiese, Aniello, Francesca Iannaccone, Andrea Scatena, Zoe Del Fante, Antonio Oliva, Paola Frati, and Vittorio Fineschi. 2021. "Pediatric Abusive Head Trauma: A Systematic Review" Diagnostics 11, no. 4: 734. https://doi.org/10.3390/diagnostics11040734
APA StyleMaiese, A., Iannaccone, F., Scatena, A., Del Fante, Z., Oliva, A., Frati, P., & Fineschi, V. (2021). Pediatric Abusive Head Trauma: A Systematic Review. Diagnostics, 11(4), 734. https://doi.org/10.3390/diagnostics11040734








