The Prognostic Impact of HER2 Genetic and Protein Expression in Pancreatic Carcinoma—HER2 Protein and Gene in Pancreatic Cancer
Abstract
1. Introduction
2. Material and Methods
2.1. Study Design and Case Selection
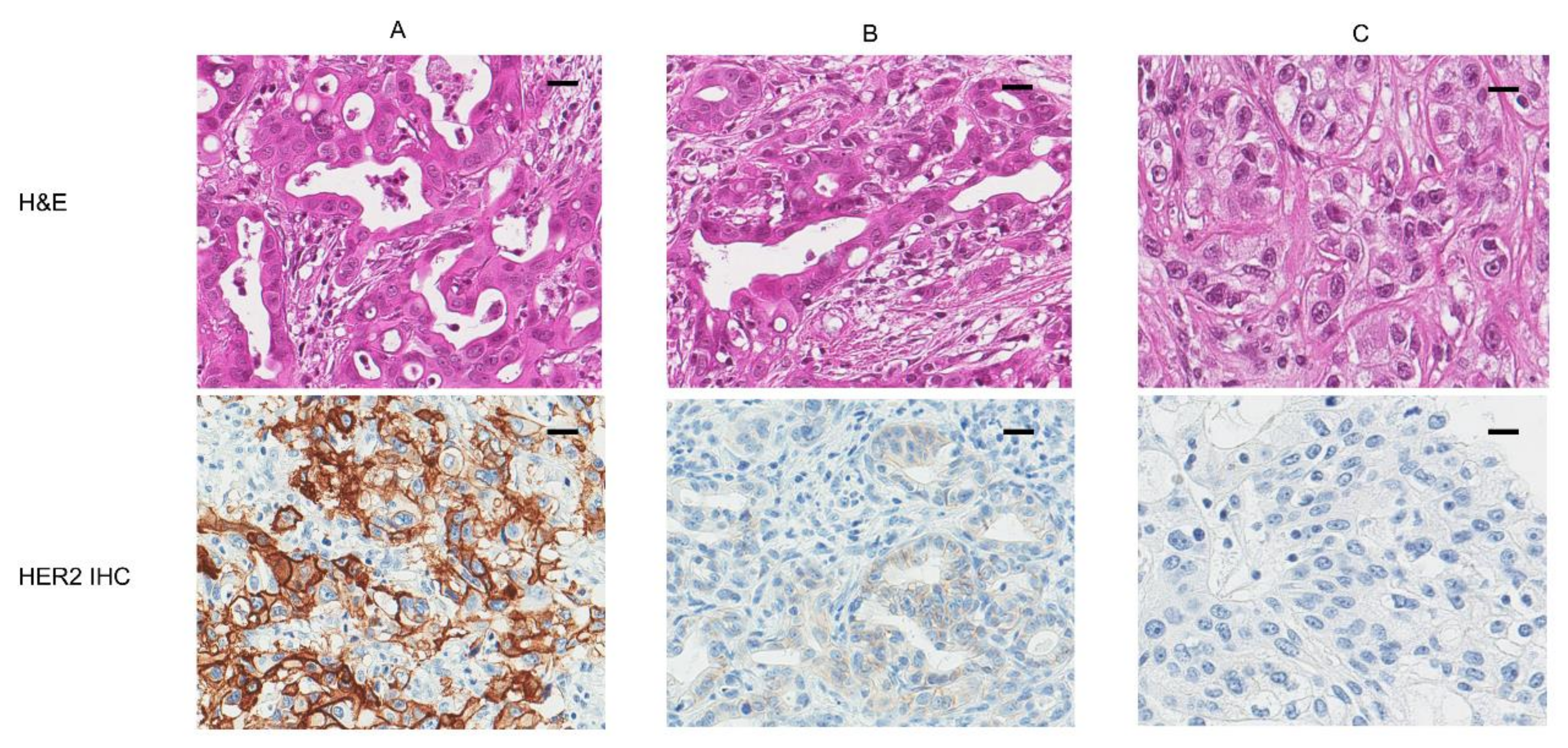
2.2. Tissue Microarray Construction, HER2 Immunohistochemistry, and Silver-Enhanced In Situ Hybridization
2.3. Evaluation of HER2 Status Using HER2 Immunohistochemistry and Silver-Enhanced In Situ Hybridization
2.4. Statistical Analysis
3. Results
3.1. Analyses of the HER2 Protein and Encoding Gene Using IHC and SISH
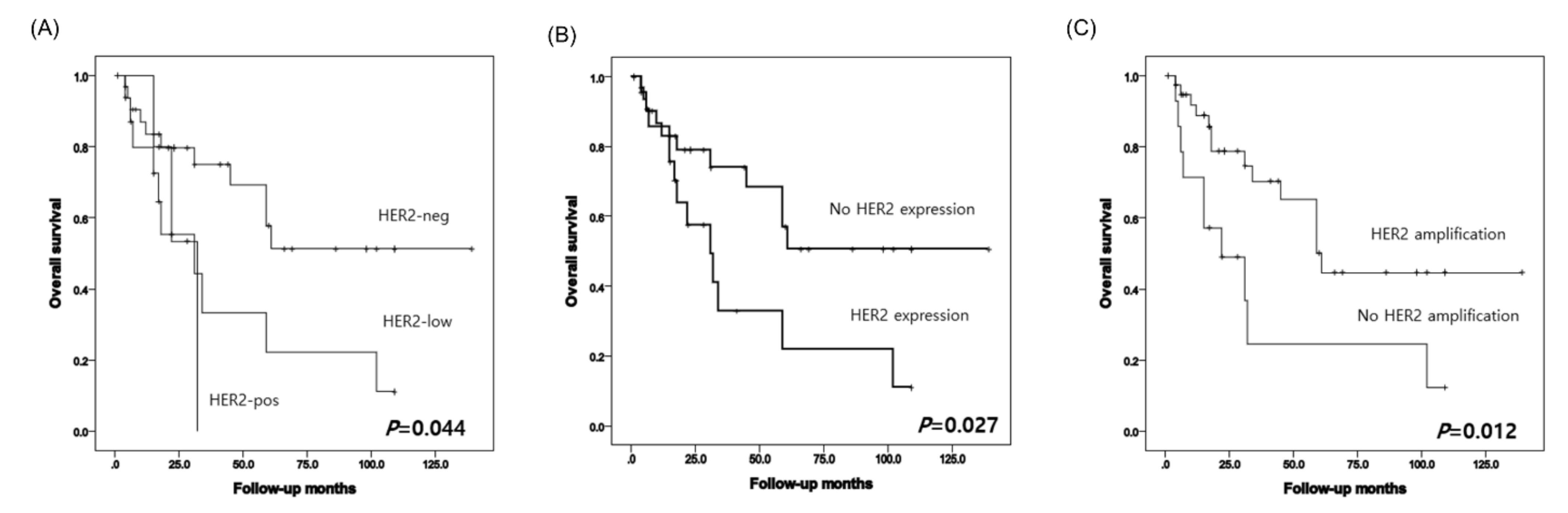
3.2. Survival Analyses According to HER2 Protein and Gene Status in PDAC
3.3. Association of Clinicopathological Characteristics and HER2 Genetic Heterogeneity in HER2-Neg and HER2-Low Groups
3.4. Survival Analyses in HER2-Neg and HER2-Low Groups
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Jung, K.W.; Won, Y.J.; Kong, H.J.; Lee, E.S. Prediction of cancer incidence and mortality in Korea, 2019. Cancer Res. Treat. 2019, 51, 431–437. [Google Scholar] [CrossRef]
- Ross, J.S.; Fletcher, J.A.; Linette, G.P.; Stec, J.; Clark, E.; Ayers, M.; Symmans, W.F.; Pusztai, L.; Bloom, K.J. The Her-2/neu gene and protein in breast cancer 2003: Biomarker and target of therapy. Oncologist 2003, 8, 307–325. [Google Scholar] [CrossRef] [PubMed]
- Alroy, I.; Yarden, Y. The ErbB signaling network in embryogenesis and oncogenesis: Signal diversification through combinatorial ligand-receptor interactions. FEBS Lett. 1997, 410, 83–86. [Google Scholar] [CrossRef]
- Moasser, M.M. The oncogene HER2: Its signaling and transforming functions and its role in human cancer pathogenesis. Oncogene 2007, 26, 6469–6487. [Google Scholar] [CrossRef]
- Tzahar, E.; Waterman, H.; Chen, X.; Levkowitz, G.; Karunagaran, D.; Lavi, S.; Ratzkin, B.J.; Yarden, Y. A hierarchical network of interreceptor interactions determines signal transduction by Neu differentiation factor/neuregulin and epidermal growth factor. Mol. Cell. Biol. 1996, 16, 5276–5287. [Google Scholar] [CrossRef]
- Gutierrez, C.; Schiff, R. HER2: Biology, detection, and clinical implications. Arch. Pathol. Lab. Med. 2011, 135, 55–62. [Google Scholar] [CrossRef] [PubMed]
- Menard, S.; Fortis, S.; Castiglioni, F.; Agresti, R.; Balsari, A. HER2 as a prognostic factor in breast cancer. Oncology 2001, 61, 67–72. [Google Scholar] [CrossRef]
- Jorgensen, J.T.; Nielsen, K.B.; Kjaersgaard, G.; Jepsen, A.; Mollerup, J. Gene signal distribution and HER2 amplification in gastroesophageal cancer. J. Cancer 2017, 8, 1517–1524. [Google Scholar] [CrossRef]
- Roskoski, R. The ErbB/HER family of protein-tyrosine kinases and cancer. Pharmacol. Res. 2014, 79, 34–74. [Google Scholar] [CrossRef]
- Piccart-Gebhart, M.J.; Procter, M.; Leyland-Jones, B.; Goldhirsch, A.; Untch, M.; Smith, I.; Gianni, L.; Baselga, J.; Bell, R.; Jackisch, C.; et al. Trastuzumab after adjuvant chemotherapy in HER2-positive breast cancer. N. Engl. J. Med. 2005, 353, 1659–1672. [Google Scholar] [CrossRef] [PubMed]
- Early Breast Cancer Trialists’ Collaborative Group. Tamoxifen for early breast cancer: An overview of the randomised trials. Lancet 1998, 351, 1451–1467. [Google Scholar] [CrossRef]
- Bang, Y.J.; Van Cutsem, E.; Feyereislova, A.; Chung, H.C.; Shen, L.; Sawaki, A.; Lordick, F.; Ohtsu, A.; Omuro, Y.; Satoh, T.; et al. Trastuzumab in combination with chemotherapy versus chemotherapy alone for treatment of HER2-positive advanced gastric or gastro-oesophageal junction cancer (ToGA): A phase 3, open-label, randomised controlled trial. Lancet 2010, 376, 687–697. [Google Scholar] [CrossRef]
- Potti, A.; Ganti, A.K.; Tendulkar, K.; Chitajallu, S.; Sholes, K.; Koch, M.; Kargas, S. HER-2/neu and CD117 (C-kit) overexpression in hepatocellular and pancreatic carcinoma. Anticancer Res. 2003, 23, 2671–2674. [Google Scholar]
- Dergham, S.T.; Dugan, M.C.; Arlauskas, P.; Du, W.; Vaitkevicius, V.K.; Crissman, J.D.; Sarkar, F.H. Relationship of family cancer history to the expression of p53, p21WAF-1, HER-2/neu, and K-ras mutation in pancreatic adenocarcinoma. Int. J. Pancreatol. 1997, 21, 225–234. [Google Scholar] [CrossRef]
- Hall, P.A.; Hughes, C.M.; Staddon, S.L.; Richman, P.I.; Gullick, W.J.; Lemoine, N.R. The c-erb B-2 proto-oncogene in human pancreatic cancer. J. Pathol. 1990, 161, 195–200. [Google Scholar] [CrossRef]
- Nordstrom, J.L.; Gorlatov, S.; Zhang, W.; Yang, Y.; Huang, L.; Burke, S.; Li, H.; Ciccarone, V.; Zhang, T.; Stavenhagen, J.; et al. Anti-tumor activity and toxicokinetics analysis of MGAH22, an anti-HER2 monoclonal antibody with enhanced Fcgamma receptor binding properties. Breast Cancer Res. 2011, 13, R123. [Google Scholar] [CrossRef]
- Agus, D.B.; Akita, R.W.; Fox, W.D.; Lewis, G.D.; Higgins, B.; Pisacane, P.I.; Lofgren, J.A.; Tindell, C.; Evans, D.P.; Maiese, K.; et al. Targeting ligand-activated ErbB2 signaling inhibits breast and prostate tumor growth. Cancer Cell 2002, 2, 127–137. [Google Scholar] [CrossRef]
- Modi, S.; Park, H.; Murthy, R.K.; Iwata, H.; Tamura, K.; Tsurutani, J.; Moreno-Aspitia, A.; Doi, T.; Sagara, Y.; Redfern, C.; et al. Antitumor activity and safety of trastuzumab deruxtecan in patients with HER2-low-expressing advanced breast cancer: Results from a phase Ib study. J. Clin. Oncol. 2020, 38, 1887–1896. [Google Scholar] [CrossRef]
- Nakada, T.; Sugihara, K.; Jikoh, T.; Abe, Y.; Agatsuma, T. The latest research and development into the antibody-drug conjugate, [fam-] trastuzumab deruxtecan (DS-8201a), for HER2 cancer therapy. Chem. Pharm. Bull. 2019, 67, 173–185. [Google Scholar] [CrossRef]
- Banerji, U.; van Herpen, C.M.L.; Saura, C.; Thistlethwaite, F.; Lord, S.; Moreno, V.; Macpherson, I.R.; Boni, V.; Rolfo, C.; de Vries, E.G.E.; et al. Trastuzumab duocarmazine in locally advanced and metastatic solid tumours and HER2-expressing breast cancer: A phase 1 dose-escalation and dose-expansion study. Lancet Oncol. 2019, 20, 1124–1135. [Google Scholar] [CrossRef]
- Gibbons-Fideler, I.S.; Nitta, H.; Murillo, A.; Tozbikian, G.; Banks, P.; Parwani, A.V.; Li, Z. Identification of HER2 immunohistochemistry-negative, FISH-amplified breast cancers and their response to anti-HER2 neoadjuvant chemotherapy. Am. J. Clin. Pathol. 2019, 151, 176–184. [Google Scholar] [CrossRef]
- Hofmann, M.; Stoss, O.; Shi, D.; Buttner, R.; van de Vijver, M.; Kim, W.; Ochiai, A.; Ruschoff, J.; Henkel, T. Assessment of a HER2 scoring system for gastric cancer: Results from a validation study. Histopathology 2008, 52, 797–805. [Google Scholar] [CrossRef] [PubMed]
- Ogitani, Y.; Aida, T.; Hagihara, K.; Yamaguchi, J.; Ishii, C.; Harada, N.; Soma, M.; Okamoto, H.; Oitate, M.; Arakawa, S.; et al. DS-8201a, A Novel HER2-Targeting ADC with a Novel DNA topoisomerase I inhibitor, demonstrates a promising antitumor efficacy with differentiation from T-DM1. Clin. Cancer Res. 2016, 22, 5097–5108. [Google Scholar] [CrossRef] [PubMed]
- Doi, T.; Shitara, K.; Naito, Y.; Shimomura, A.; Fujiwara, Y.; Yonemori, K.; Shimizu, C.; Shimoi, T.; Kuboki, Y.; Matsubara, N.; et al. Safety, pharmacokinetics, and antitumour activity of trastuzumab deruxtecan (DS-8201), a HER2-targeting antibody-drug conjugate, in patients with advanced breast and gastric or gastro-oesophageal tumours: A phase 1 dose-escalation study. Lancet Oncol. 2017, 18, 1512–1522. [Google Scholar] [CrossRef]
- Hausman, D.F.; Hamilton, E.P.; Beeram, M.; Thimmarayappa, J.; Ng, G.; Meric-Bernstam, F. Phase 1 study of ZW25, a bispecific anti-HER2 antibody, in patients with advanced HER2-expressing cancers. J. Clin. Oncol. 2017, 35, TPS215. [Google Scholar] [CrossRef]
- Zellmer, V.R.; Zhang, S. Evolving concepts of tumor heterogeneity. Cell Biosci. 2014, 4, 69. [Google Scholar] [CrossRef]
- Allison, K.H.; Dintzis, S.M.; Schmidt, R.A. Frequency of HER2 heterogeneity by fluorescence in situ hybridization according to CAP expert panel recommendations: Time for a new look at how to report heterogeneity. Am. J. Clin. Pathol. 2011, 136, 864–871. [Google Scholar] [CrossRef]
- Lee, H.J.; Kim, J.Y.; Park, S.Y.; Park, I.A.; Song, I.H.; Yu, J.H.; Ahn, J.H.; Gong, G. Clinicopathologic significance of the intratumoral heterogeneity of HER2 gene amplification in HER2-positive breast cancer patients treated with adjuvant trastuzumab. Am. J. Clin. Pathol. 2015, 144, 570–578. [Google Scholar] [CrossRef]
- Seol, H.; Lee, H.J.; Choi, Y.; Lee, H.E.; Kim, Y.J.; Kim, J.H.; Kang, E.; Kim, S.W.; Park, S.Y. Intratumoral heterogeneity of HER2 gene amplification in breast cancer: Its clinicopathological significance. Mod. Pathol. 2012, 25, 938–948. [Google Scholar] [CrossRef]
- Bartlett, A.I.; Starcyznski, J.; Robson, T.; Maclellan, A.; Campbell, F.M.; van de Velde, C.J.; Hasenburg, A.; Markopoulos, C.; Seynaeve, C.; Rea, D.; et al. Heterogeneous HER2 gene amplification: Impact on patient outcome and a clinically relevant definition. Am. J. Clin. Pathol. 2011, 136, 266–274. [Google Scholar] [CrossRef]
- Li, A.; Yang, J.J.; Zhang, X.C.; Zhang, Z.; Su, J.; Gou, L.Y.; Bai, Y.; Zhou, Q.; Yang, Z.; Han-Zhang, H.; et al. Acquired MET Y1248H and D1246N mutations mediate resistance to MET inhibitors in non-small cell lung cancer. Clin. Cancer Res. 2017, 23, 4929–4937. [Google Scholar] [CrossRef]
- Arcila, M.E.; Oxnard, G.R.; Nafa, K.; Riely, G.J.; Solomon, S.B.; Zakowski, M.F.; Kris, M.G.; Pao, W.; Miller, V.A.; Ladanyi, M. Rebiopsy of lung cancer patients with acquired resistance to EGFR inhibitors and enhanced detection of the T790M mutation using a locked nucleic acid-based assay. Clin. Cancer Res. 2011, 17, 1169–1180. [Google Scholar] [CrossRef]
- Turner, N.C.; Reis-Filho, J.S. Genetic heterogeneity and cancer drug resistance. Lancet Oncol. 2012, 13, e178–e185. [Google Scholar] [CrossRef]
- Ayala, F.J. Darwin’s greatest discovery: Design without designer. Proc. Natl. Acad. Sci. USA 2007, 104, 8567–8573. [Google Scholar] [CrossRef]
- Jackson, A.L.; Loeb, L.A. The mutation rate and cancer. Genetics 1998, 148, 1483–1490. [Google Scholar] [CrossRef] [PubMed]
- Turajlic, S.; Swanton, C. Metastasis as an evolutionary process. Science 2016, 352, 169–175. [Google Scholar] [CrossRef] [PubMed]
- Dagogo-Jack, I.; Shaw, A.T. Tumour heterogeneity and resistance to cancer therapies. Nat. Rev. Clin. Oncol. 2018, 15, 81–94. [Google Scholar] [CrossRef] [PubMed]
- Cleary, A.S.; Leonard, T.L.; Gestl, S.A.; Gunther, E.J. Tumour cell heterogeneity maintained by cooperating subclones in Wnt-driven mammary cancers. Nature 2014, 508, 113–117. [Google Scholar] [CrossRef] [PubMed]
- Polyak, K.; Marusyk, A. Cancer: Clonal cooperation. Nature 2014, 508, 52–53. [Google Scholar] [CrossRef]
- Hudis, C.A. Trastuzumab--mechanism of action and use in clinical practice. N. Engl. J. Med. 2007, 357, 39–51. [Google Scholar] [CrossRef]
- Collins, D.M.; O’Donovan, N.; McGowan, P.M.; O’Sullivan, F.; Duffy, M.J.; Crown, J. Trastuzumab induces antibody-dependent cell-mediated cytotoxicity (ADCC) in HER-2-non-amplified breast cancer cell lines. Ann. Oncol. 2012, 23, 1788–1795. [Google Scholar] [CrossRef]
- Collins, D.M.; Madden, S.F.; Gaynor, N.; AlSultan, D.; Le Gal, M.; Eustace, A.J.; Gately, K.A.; Hughes, C.; Davies, A.M.; Mahgoub, T.; et al. Effects of HER family-targeting tyrosine kinase inhibitors on antibody-dependent cell-mediated cytotoxicity in HER2-expressing breast cancer. Clin. Cancer Res. 2021, 27, 807–818. [Google Scholar] [CrossRef] [PubMed]
| Main Cohort | Validation Cohort | |
|---|---|---|
| Characteristic | Number of patients (%) | Number of patients (%) |
| Cohort size | 55 (100) | 19 (100) |
| Sex | ||
| Male | 27 (49.1) | 8 (42.1) |
| Female | 28 (50.9) | 11 (57.9) |
| Location | ||
| Head | 33 (60.0) | 15 (78.9) |
| Tail | 15 (27.3) | 4 (21.1) |
| Body | 6 (10.9) | 0 |
| Uncinate process | 1 (1.8) | 0 |
| Tumor stage | ||
| pT1 | 6 (10.9) | 2 (10.5) |
| pT2 | 33 (60.0) | 14 (737.7) |
| pT3 | 16 (29.1) | 3 (15.8) |
| Node stage | ||
| pN0 | 20 (35.7) | 12 (63.2) |
| pN1 | 25 (44.6) | 7 (36.8) |
| pN2 | 10 (17.9) | 0 |
| Clinical stage | ||
| IA | 4 (7.3) | 1 (5.3) |
| IB | 7 (12.7) | 8 (42.1) |
| IIA | 3 (5.5) | 3 (15.8) |
| IIB | 20 (36.3) | 7 (36.8) |
| III | 9 (16.4) | 0 |
| IV | 12 (21.8) | 0 |
| HER2 Status | Main Cohort | HER2 Status | Validation Cohort | ||||
|---|---|---|---|---|---|---|---|
| IHC Score | SISH Result | IHC Score | SISH Result | ||||
| 0 | 32 (58.2) | Ratio of ≥2.0 | 2 (6.3) | 0 | 7 (36.8) | Ratio of ≥2.0 | 1 (14.2) |
| Ratio of <2.0 | 30 (93.8) | Ratio of <2.0 | 6 (85.8) | ||||
| 1 | 14 (25.4) | Ratio of ≥2.0 | 7 (50.0) | 1 | 5 (26.3) | Ratio of ≥2.0 | 1 (20.0) |
| Ratio of <2.0 | 7 (50.0) | Ratio of <2.0 | 4 (80.0) | ||||
| 2 | 5 (9.1) | Ratio of ≥2.0 | 1 (20.0) | 2 | 6 (31.6) | Ratio of ≥2.0 | 2 (33.3) |
| Ratio of <2.0 | 4 (80.0) | Ratio of <2.0 | 4 (66.7) | ||||
| 3 | 4 (7.3) | Ratio of ≥2.0 | 4 (100.0) | 3 | 1 (5.3) | Ratio of ≥2.0 | 1 (100.0) |
| Total (n, %) | 55 (100) | Total (n, %) | 19 (100) |
| Characteristics | HER2 Heterogeneity (n = 36) | HER2 Non-Heterogeneity (N = 14) | p |
|---|---|---|---|
| Age (year) | 62.3 ± 8.6 | 59.8 ± 9.3 | |
| Tumor size (cm) | 3.6 ± 1.7 | 3.9 ± 1.9 | |
| Tumor stage | 0.129 | ||
| pT1 | 2 (5.6) | 3 (21.4) | |
| pT2 | 25 (69.4) | 6 (42.9) | |
| pT3 | 9 (25.0) | 5 (35.7) | |
| Node stage | 0.753 | ||
| pN0 | 15 (41.7) | 5 (35.7) | |
| pN1-2 | 21 (58.3) | 9 (64.3) | |
| HER2/CEP17 ratio | 1.8 ± 0.55 | 1.7 ± 0.12 | |
| HER2 gene amplification | 0.039 | ||
| Negative | 27 (75.0) | 14 (100.0) | |
| Positive | 9 (25.0) | 0 (0) | |
| HER2 IHC score | 0.005 | ||
| 0 | 20 (55.6) | 12 (85.7) | |
| 1 | 12 (33.3) | 2 (14.3) | |
| 2 | 4 (11.1) | 0 (0) | |
| Discordance of IHC and SISH | 0.045 | ||
| No | 26 (72.2) | 14 (100.0) | |
| Yes | 10 (27.8) | 0 (0) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Han, S.-H.; Ryu, K.H.; Kwon, A.-Y. The Prognostic Impact of HER2 Genetic and Protein Expression in Pancreatic Carcinoma—HER2 Protein and Gene in Pancreatic Cancer. Diagnostics 2021, 11, 653. https://doi.org/10.3390/diagnostics11040653
Han S-H, Ryu KH, Kwon A-Y. The Prognostic Impact of HER2 Genetic and Protein Expression in Pancreatic Carcinoma—HER2 Protein and Gene in Pancreatic Cancer. Diagnostics. 2021; 11(4):653. https://doi.org/10.3390/diagnostics11040653
Chicago/Turabian StyleHan, Song-Hee, Ki Hyun Ryu, and Ah-Young Kwon. 2021. "The Prognostic Impact of HER2 Genetic and Protein Expression in Pancreatic Carcinoma—HER2 Protein and Gene in Pancreatic Cancer" Diagnostics 11, no. 4: 653. https://doi.org/10.3390/diagnostics11040653
APA StyleHan, S.-H., Ryu, K. H., & Kwon, A.-Y. (2021). The Prognostic Impact of HER2 Genetic and Protein Expression in Pancreatic Carcinoma—HER2 Protein and Gene in Pancreatic Cancer. Diagnostics, 11(4), 653. https://doi.org/10.3390/diagnostics11040653






