Complications of Outpatient and Inpatient Renal Biopsy: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Methods
2.1. Study Inclusion Criteria
2.1.1. Types of Studies and Study Participants
2.1.2. Types of Intervention
2.1.3. Types of Outcome Measures
2.1.4. Data Source
2.2. Data Extraction
2.3. Statistical Analysis
3. Results
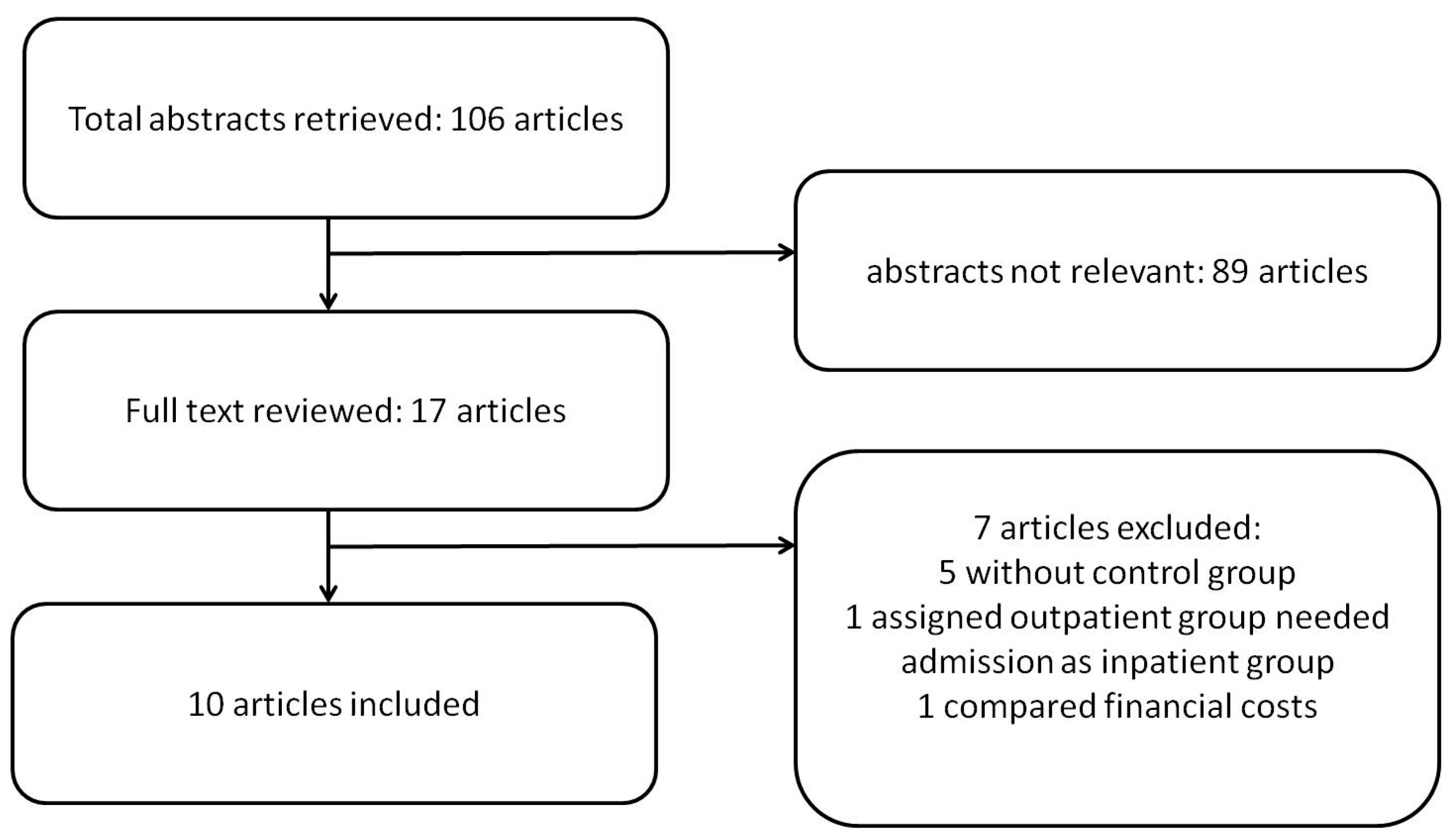
3.1. Literature Search and Characteristics of Included Studies
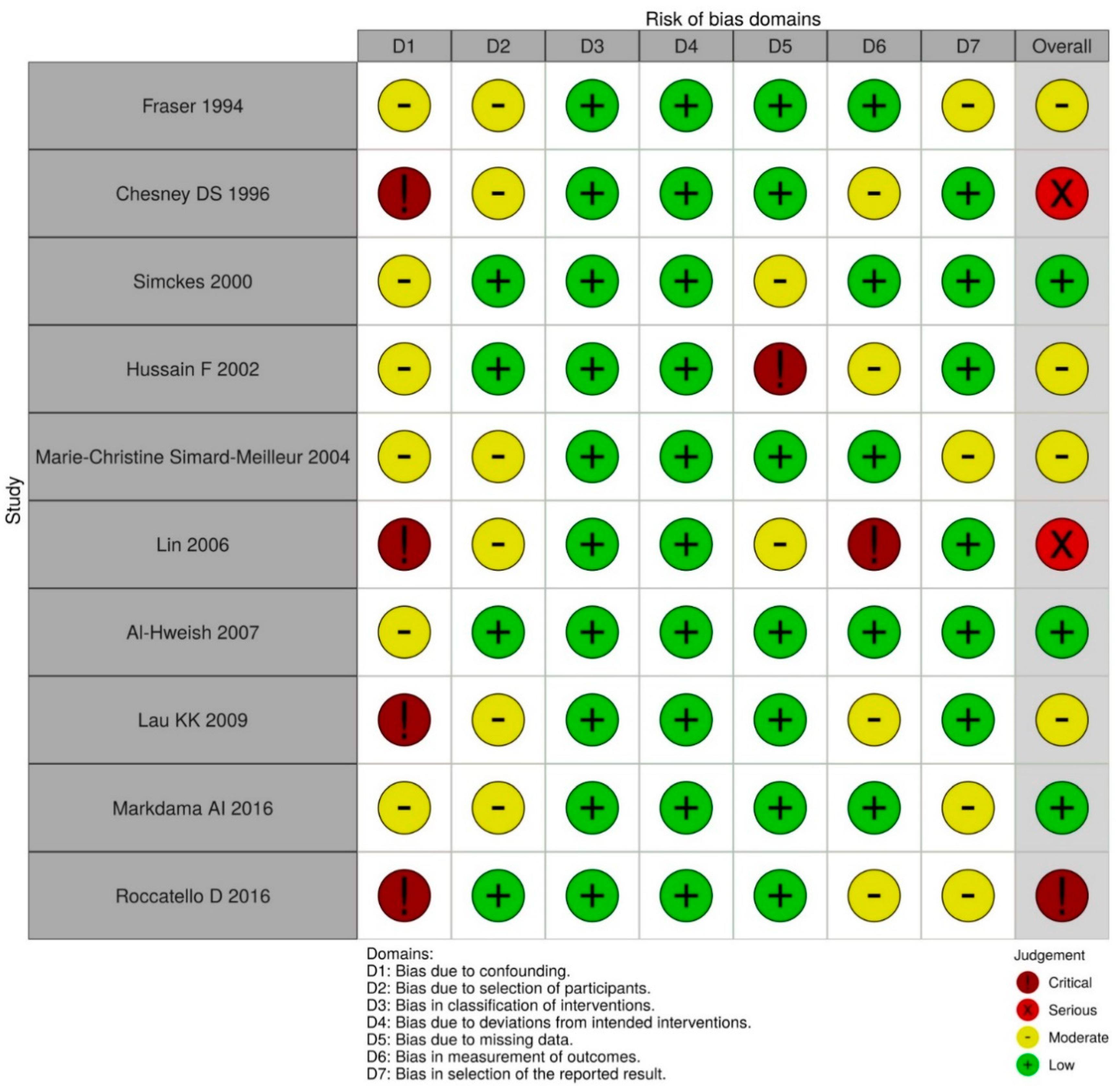
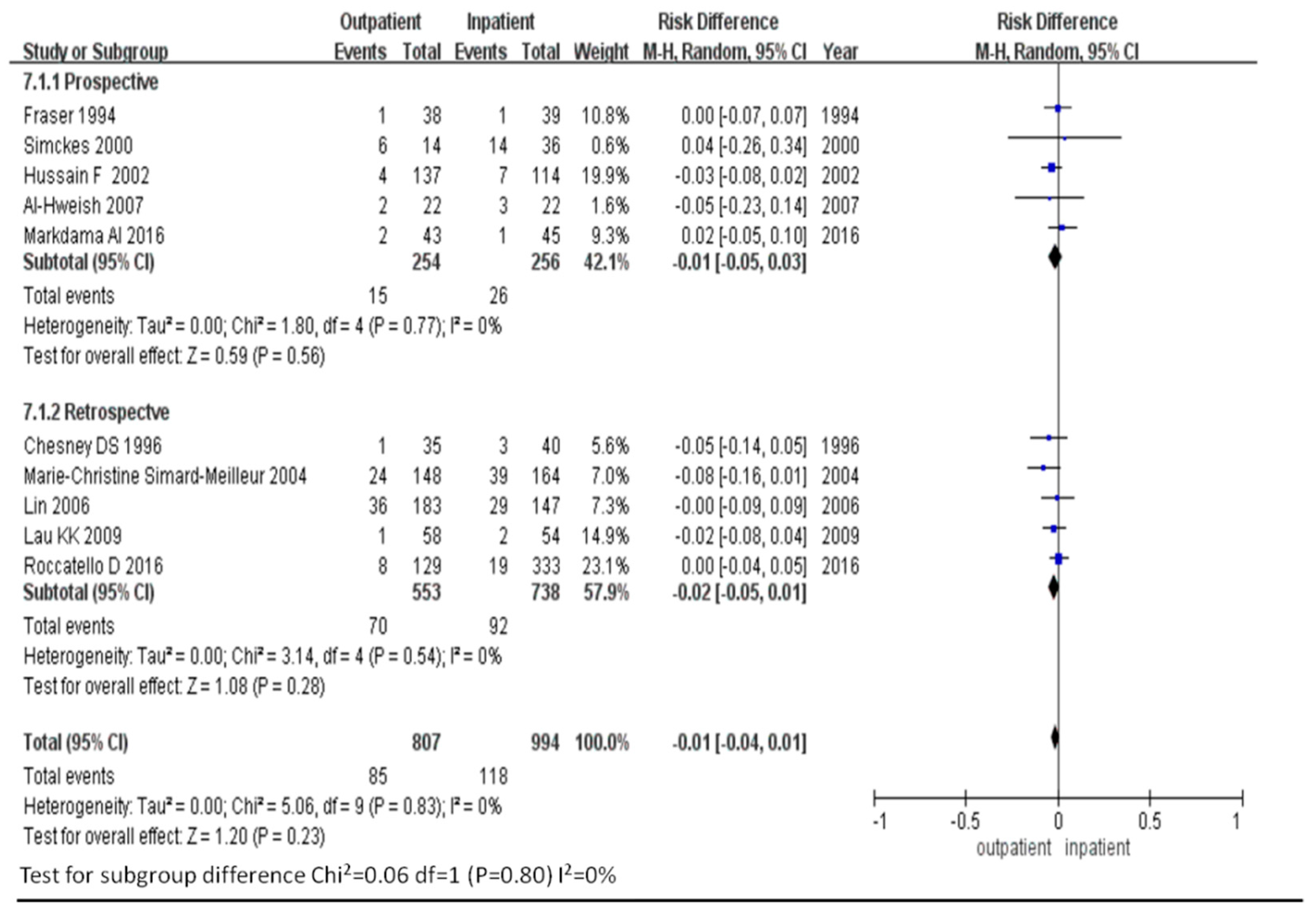
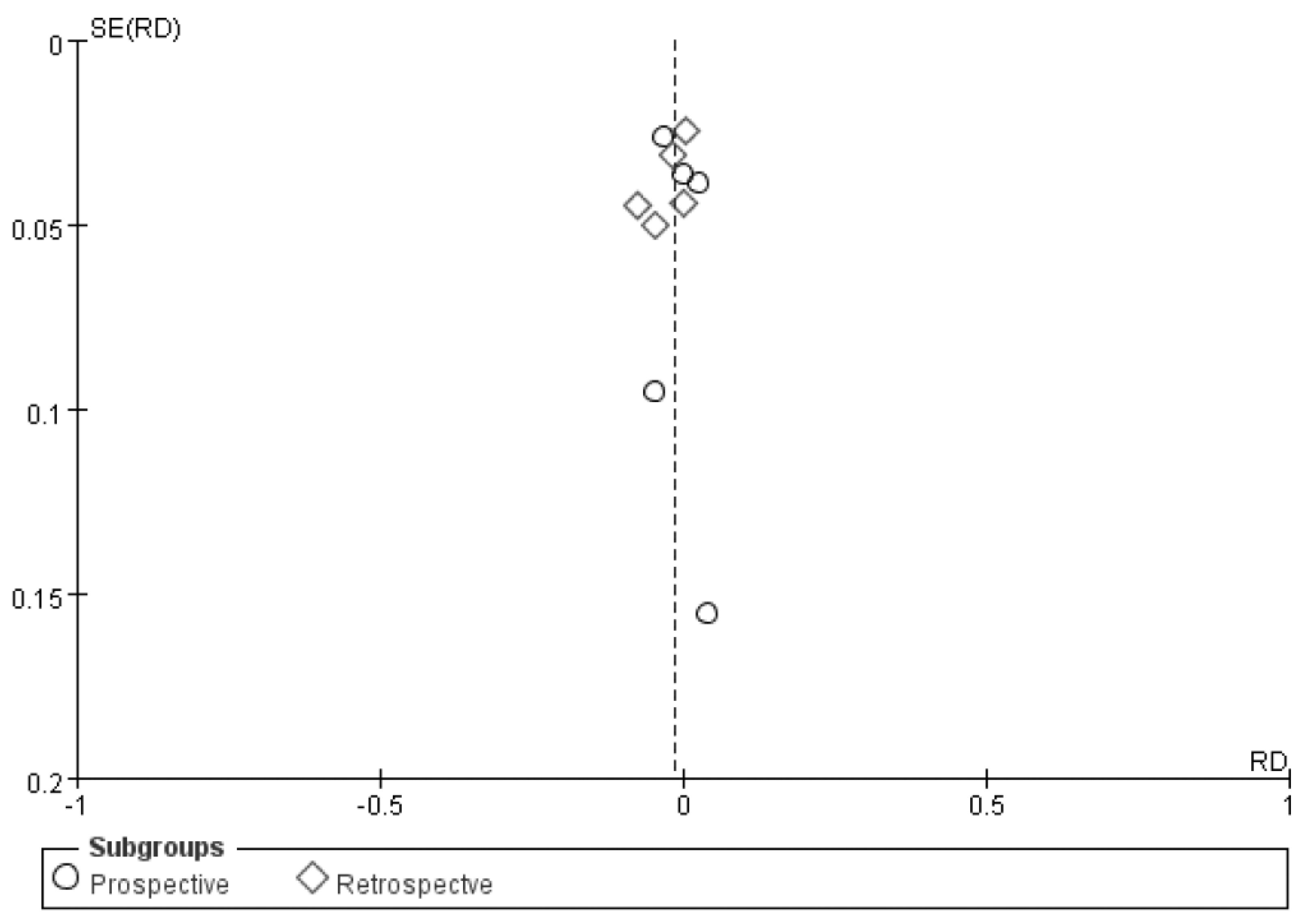
3.2. Risk of Bleeding
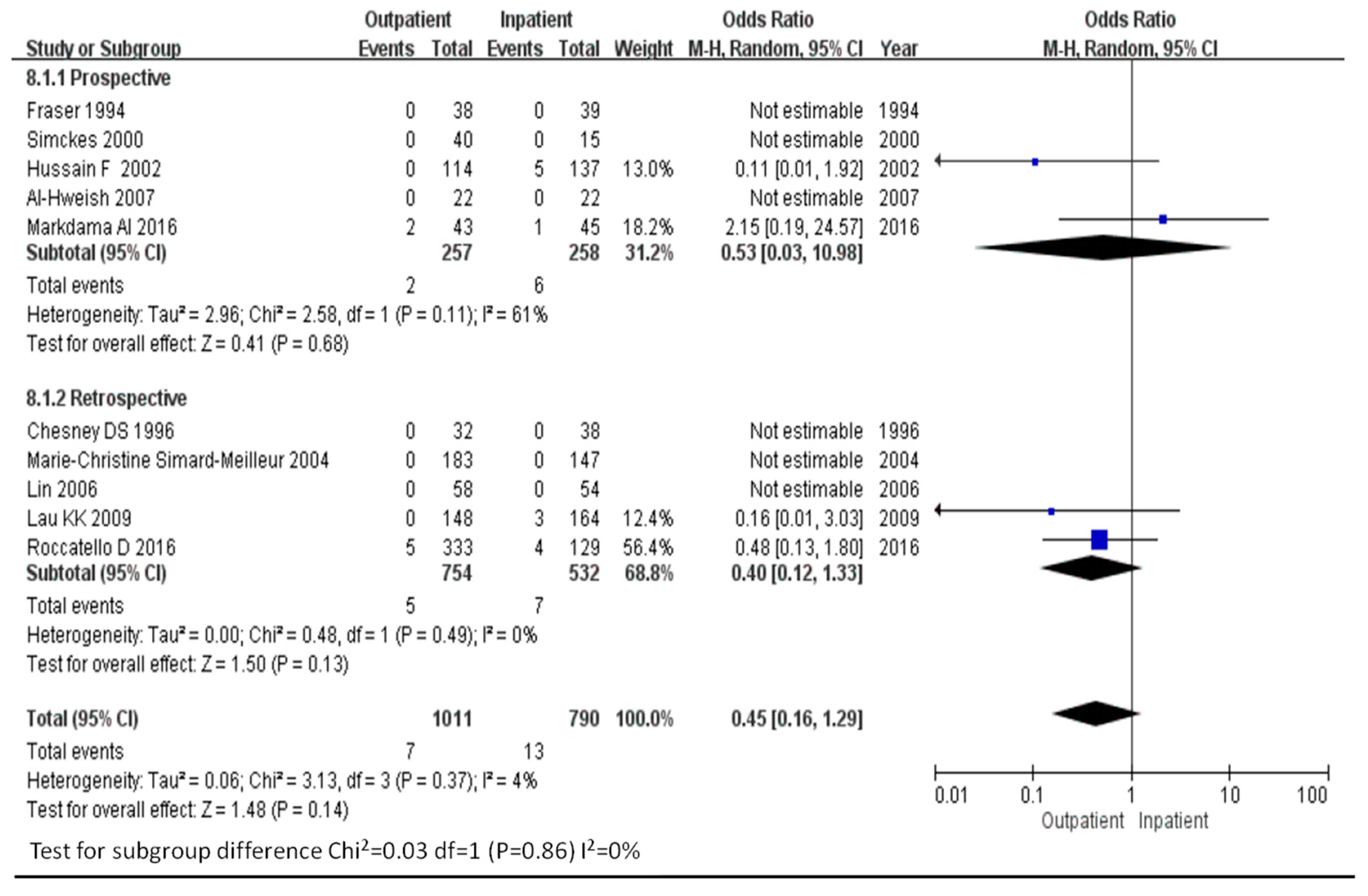
3.3. Rates of Major Events
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Walker, P.D. The renal biopsy. Arch. Pathol. Lab. Med. 2009, 133, 181–188. [Google Scholar] [CrossRef] [PubMed]
- Fuiano, G.; Mazza, G.; Comi, N.; Caglioti, A.; De Nicola, L.; Iodice, C.; Andreucci, M.; Andreucci, V.E. Current indications for renal biopsy: A questionnaire-based survey. Am. J. Kidney Dis. 2000, 35, 448–457. [Google Scholar] [CrossRef]
- Korbet, S.M. Percutaneous renal biopsy. Semin. Nephrol. 2002, 22, 254–267. [Google Scholar] [CrossRef] [PubMed]
- Wiseman, D.A.; Hawkins, R.; Numerow, L.M.; Taub, K.J. Percutaneous renal biopsy utilizing real time, ultrasonic guidance and a semiautomated biopsy device. Kidney Int. 1990, 38, 347–349. [Google Scholar] [CrossRef] [PubMed]
- Hergesell, O.; Felten, H.; Andrassy, K.; Kühn, K.; Ritz, E. Safety of ultrasound-guided percutaneous renal biopsy-retrospective analysis of 1090 consecutive cases. Nephrol. Dial. Transplant. 1998, 13, 975–977. [Google Scholar] [CrossRef]
- Parrish, A. Complications of percutaneous renal biopsy: A review of 37 years’ experience. Clin. Nephrol. 1992, 38, 135–141. [Google Scholar]
- Eiro, M.; Katoh, T.; Watanabe, T. Risk factors for bleeding complications in percutaneous renal biopsy. Clin. Exp. Nephrol. 2005, 9, 40–45. [Google Scholar] [CrossRef]
- Muñoz, A.T.; Valdez-Ortiz, R.; Gonzalez-Parra, C.; Espinoza-Dávila, E.; Morales-Buenrostro, L.E.; Correa-Rotter, R. Percutaneous renal biopsy of native kidneys: Efficiency, safety and risk factors associated with major complications. Arch. Med Sci. AMS 2011, 7, 823. [Google Scholar] [CrossRef]
- Shidham, G.B.; Siddiqi, N.; Beres, J.A.; Logan, B.; Nagaraja, H.; Shidham, S.G.; Piering, W.F. Clinical risk factors associated with bleeding after native kidney biopsy. Nephrology 2005, 10, 305–310. [Google Scholar] [CrossRef] [PubMed]
- Lees, J.S.; McQuarrie, E.P.; Mordi, N.; Geddes, C.C.; Fox, J.G.; Mackinnon, B. Risk factors for bleeding complications after nephrologist-performed native renal biopsy. Clin. Kidney J. 2017, 10, 573–577. [Google Scholar] [CrossRef]
- Whittier, W.L.; Korbet, S.M. Timing of complications in percutaneous renal biopsy. J. Am. Soc. Nephrol. 2004, 15, 142–147. [Google Scholar] [CrossRef] [PubMed]
- ZHANG, P.P.; GE, Y.C.; LI, S.J.; XIE, H.L.; LI, L.S.; LIU, Z.H. Renal biopsy in type 2 diabetes: Timing of complications and evaluating of safety in Chinese patients. Nephrology 2011, 16, 100–105. [Google Scholar] [CrossRef] [PubMed]
- Marwah, D.S.; Korbet, S.M. Timing of complications in percutaneous renal biopsy: What is the optimal period of observation? Am. J. Kidney Dis. 1996, 28, 47–52. [Google Scholar] [CrossRef]
- Simard-Meilleur, M.-C.; Troyanov, S.; Roy, L.; Dalaire, E.; Brachemi, S. Risk factors and timing of native kidney biopsy complications. Nephron Extra 2014, 4, 42–49. [Google Scholar] [CrossRef] [PubMed]
- Jones, B.; Puvaneswary, M.; Nanra, R.; Trevillian, P.; Carney, S.; Gillies, A. Reduced duration of bed rest after percutaneous renal biopsy. Clin. Nephrol. 1991, 35, 44–45. [Google Scholar]
- Fraser, I.; Fairley, K. Renal biopsy as an outpatient procedure. Am. J. Kidney Dis. 1995, 25, 876–878. [Google Scholar] [CrossRef]
- Simckes, A.M.; Blowey, D.L.; Gyves, K.M.; Alon, U.S. Success and safety of same-day kidney biopsy in children and adolescents. Pediatric Nephrol. 2000, 14, 946–952. [Google Scholar] [CrossRef]
- Hussain, F.; Watson, A.R.; Hayes, J.; Evans, J. Standards for renal biopsies: Comparison of inpatient and day care procedures. Pediatric Nephrol. 2003, 18, 53–56. [Google Scholar] [CrossRef]
- Al-Hweish, A.K.; Abdul-Rehaman, I.S. Outpatient percutaneous renal biopsy in adult patients. Saudi J. Kidney Dis. Transplant. 2007, 18, 541–546. [Google Scholar]
- Al Makdama, A.; Al-Akash, S. Safety of percutaneous renal biopsy as an outpatient procedure in pediatric patients. Ann. Saudi Med. 2006, 26, 303–305. [Google Scholar] [CrossRef] [PubMed]
- Chesney, D.S.; Brouhard, B.H.; Cunningham, R.J. Safety and cost effectiveness of pediatric percutaneous renal biopsy. Pediatric Nephrol. 1996, 10, 493–495. [Google Scholar] [CrossRef] [PubMed]
- Lin, W.; Yang, Y.; Wen, Y.; Chang, C. Outpatient versus inpatient renal biopsy: A retrospective study. Clin. Nephrol. 2006, 66, 17–24. [Google Scholar] [CrossRef] [PubMed]
- Lau, K.K.; Berg, G.L.; Butani, L. Financial implications of pediatric outpatient renal biopsies: A single-center experience. J. Nephrol. 2009, 22, 69–74. [Google Scholar]
- Roccatello, D.; Sciascia, S.; Rossi, D.; Naretto, C.; Bazzan, M.; Solfietti, L.; Baldovino, S.; Menegatti, E. Outpatient percutaneous native renal biopsy: Safety profile in a large monocentric cohort. BMJ Open 2017, 7. [Google Scholar] [CrossRef] [PubMed]
- Emanuel, E.J. The real cost of the US health care system. JAMA 2018, 319, 983–985. [Google Scholar] [CrossRef]
- Wu, T.-Y.; Chung, C.-H.; Lin, C.-N.; Hwang, J.-S.; Wang, J.-D. Lifetime risks, loss of life expectancy, and health care expenditures for 19 types of cancer in Taiwan. Clin. Epidemiol. 2018, 10, 581. [Google Scholar] [CrossRef] [PubMed]
| Study (Country) | Year | No of Patients (% Male) | Age (yrs) | Intervention Device | Biopsy Methods | Bleeding Complications |
|---|---|---|---|---|---|---|
| Prospective | ||||||
| Fraser, et al. (Australia) | 1994 | Outpatient: 118 (43.2%) | 38 | 14-gauge needle or Tru-Cut needle | N/A | 1/38 |
| Inpatient: 232 (28.4%) | 39 | 1/39 | ||||
| Simckes et al. (USA) | 2000 | Outpatient: 40 (62.5%) | 12.4 ± 4.2 | 14- or 15-gauge needle | US pre-localization * | 39% |
| Inpatient: 15 (46.7%) | 11.7 ± 4.0 | 43% | ||||
| Hussain F (UK) | 2002 | Outpatient: 114 (NA) | 12.4 | 16-gauge needle | US pre-localization * | 4/114 |
| Inpatient: 137 (NA) | 9.95 | 7/137 | ||||
| Al-Hweish et al. (Saudi) | 2007 | Outpatient: 22 (NA) | NA | 16 gauge; | Real-time US | 9.1% |
| Inpatient: 22 (NA) | NA | 13.6% | ||||
| Markdama AI (Arabia) | 2016 | Outpatient: 43 (51%) | NA | Outpatient: 18-gauge | US pre-localization * | 14% |
| Inpatient: 45 (51%) | NA | 8.8% | ||||
| Retrospective | ||||||
| Chesney DS (USA) | 1996 | Outpatient: 32 (56%) | 13.4 | N/A | US pre-localization * or Real time US | 2/32 |
| Inpatient: 38 (68.4%) | 11.9 | 6/38 | ||||
| Lin et al. (Taiwan) | 2006 | Outpatient: 183 (NA) | 44.4 | 16-gauge needle for adult 18-gauge for pediatrics | Real-time US | 19.7% |
| Inpatient: 147 (NA) | 50.1 | 19.7% | ||||
| Lau KK et al. (USA) | 2009 | Outpatient: 58 (55%) | 11.4 (1.4–20.1) | 18 gauge; 10–16 cm | Real-time US | 1/58 |
| Inpatient: 54 (53%) | 13.6 (0.1–20.9) | 2/54 | ||||
| Marie-Christine Simard-Meilleur et al. (Canada) | 2014 | Outpatient: 148 (47%) | 53 ± 15 | 14, 16, or 18-gauge needle | Real-time ** US or CT | 16% |
| Inpatient: 164(53%) | 54 ± 16 | 24% | ||||
| Roccatello D et al. (Italy) | 2016 | Outpatient: 129 (49%) | 52 ± 17.6 | 18-gauge/15 cm needle | Real-time ** | 6.2% |
| Inpatient: 333(66%) | 56 ± 19 | 5.7% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lin, S.-Y.; Chang, C.Y.-Y.; Lin, C.-C.; Hsu, W.-H.; Liu, I.-W.; Lin, C.-D.; Kao, C.-H. Complications of Outpatient and Inpatient Renal Biopsy: A Systematic Review and Meta-Analysis. Diagnostics 2021, 11, 651. https://doi.org/10.3390/diagnostics11040651
Lin S-Y, Chang CY-Y, Lin C-C, Hsu W-H, Liu I-W, Lin C-D, Kao C-H. Complications of Outpatient and Inpatient Renal Biopsy: A Systematic Review and Meta-Analysis. Diagnostics. 2021; 11(4):651. https://doi.org/10.3390/diagnostics11040651
Chicago/Turabian StyleLin, Shih-Yi, Cherry Yin-Yi Chang, Cheng-Chieh Lin, Wu-Huei Hsu, I.-Wen Liu, Chia-Der Lin, and Chia-Hung Kao. 2021. "Complications of Outpatient and Inpatient Renal Biopsy: A Systematic Review and Meta-Analysis" Diagnostics 11, no. 4: 651. https://doi.org/10.3390/diagnostics11040651
APA StyleLin, S.-Y., Chang, C. Y.-Y., Lin, C.-C., Hsu, W.-H., Liu, I.-W., Lin, C.-D., & Kao, C.-H. (2021). Complications of Outpatient and Inpatient Renal Biopsy: A Systematic Review and Meta-Analysis. Diagnostics, 11(4), 651. https://doi.org/10.3390/diagnostics11040651






