Novel Blood Biomarkers for a Diagnostic Workup of Acute Aortic Dissection
Abstract
1. Introduction
2. Material and Methods
2.1. Patients
2.2. Multiplex Biomarker Analysis with PROSEEK® Multiplex Assay
2.3. Single Biomarker Analyses
2.4. RNA Sequencing
2.5. Histological and Immunohistochemical Staining
2.6. Statistical Analysis
3. Results
3.1. Exploratory Multiplex Biomarker Analyses
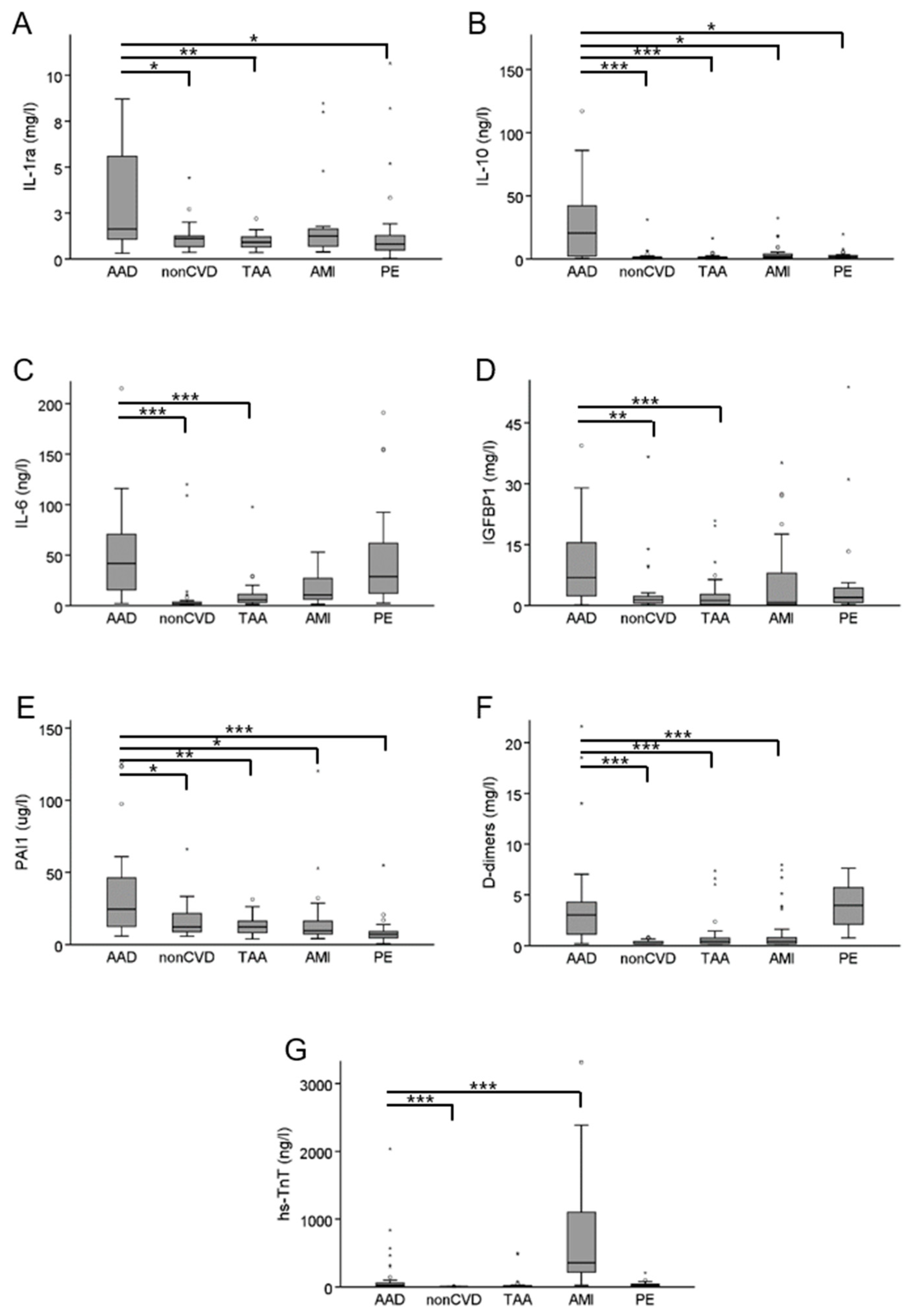
3.2. Confirmatory Single Biomarker Analyses
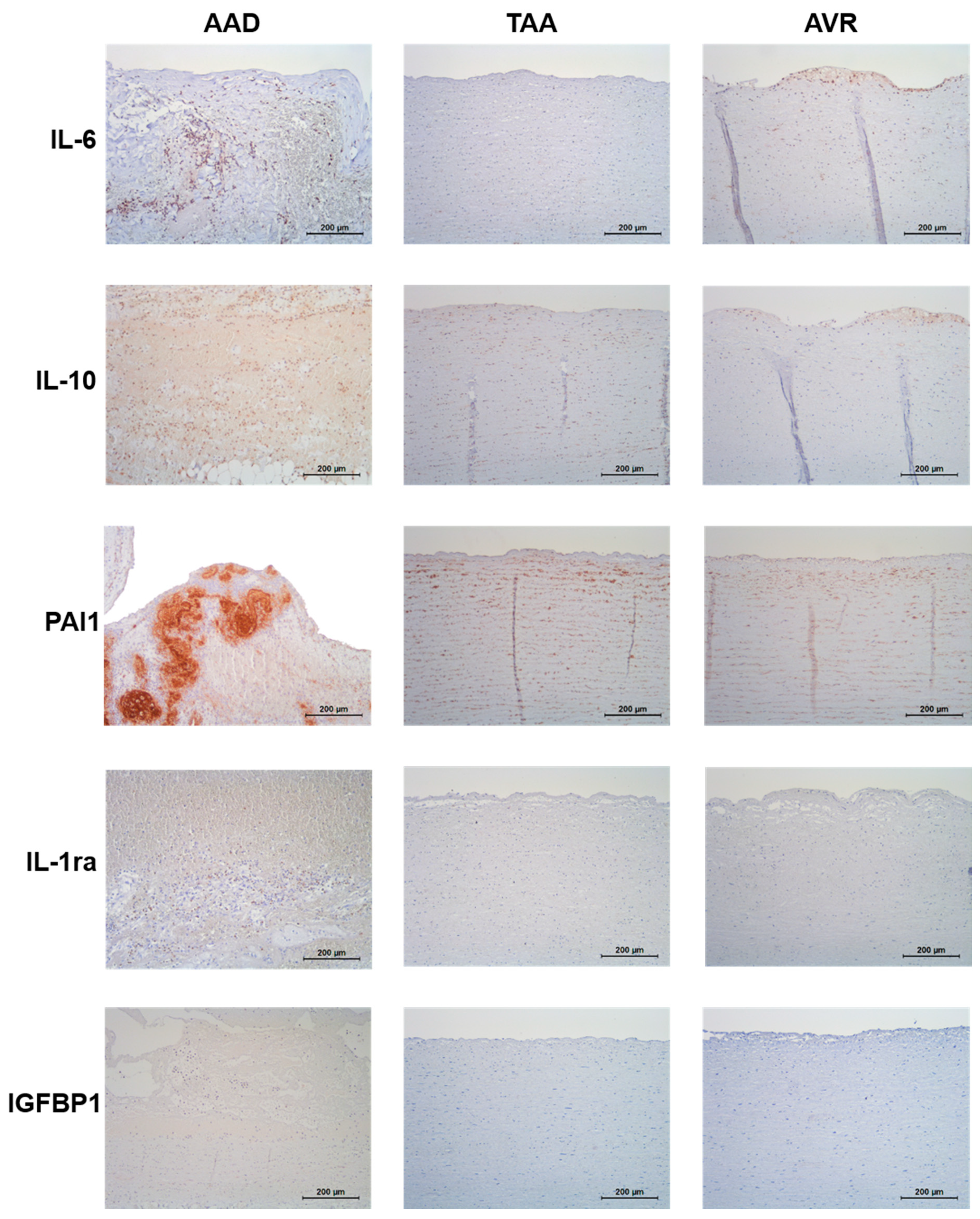
3.3. Expression of Biomarker Candidates in Aortic Tissues
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AAA | abdominal aortic aneurysm |
| AAD | acute aortic dissection |
| AMI | acute myocardial infarction |
| nonCVD | subjects with non-cardiovascular chest pain |
| hs-TnT | high-sensitive troponin T |
| IGFBP1 | insulin-like growth factor binding protein 1 |
| IL-1ra | interleukin-1 receptor antagonist |
| IL-1RL2 | interleukin-1 receptor-like 2 |
| IL-6 | interleukin 6 |
| IL-1 | interleukin 10 |
| PAI1 | plasminogen activator inhibitor 1 |
| PE | pulmonary embolism |
| TAA | thoracic aortic aneurysm |
| TNF | lymphotoxin-alpha |
References
- Niska, R.; Bhuiya, F.; Xu, J. National Hospital Ambulatory Medical Care Survey: 2007 emergency department summary. Natl. Health Stat. Rep. 2010, 2010, 1–31. [Google Scholar] [CrossRef]
- Bjørnsen, L.P.; Naess-Pleym, L.E.; Dale, J.; Grenne, B.; Wiseth, R. Description of chest pain patients in a Norwegian emergency department. Scand. Cardiovasc. J. 2019, 53, 28–34. [Google Scholar] [CrossRef] [PubMed]
- Bautz, B.; Schneider, J.I. High-Risk Chief Complaints I: Chest Pain-The Big Three (an Update). Emerg. Med. Clin. N. Am. 2020, 38, 453–498. [Google Scholar] [CrossRef] [PubMed]
- Golledge, J.; Eagle, K.A. Acute aortic dissection. Lancet 2008, 372, 55–66. [Google Scholar] [CrossRef]
- Gawinecka, J.; Schönrath, F.; Von Eckardstein, A. Acute aortic dissection: Pathogenesis, risk factors and diagnosis. Swiss Med. Wkly. 2017, 147, w14489. [Google Scholar] [CrossRef]
- Sullivan, P.R.; Wolfson, A.B.; Leckey, R.D.; Burke, J.L. Diagnosis of acute thoracic aortic dissection in the emergency department. Am. J. Emerg. Med. 2000, 18, 46–50. [Google Scholar] [CrossRef]
- Wundram, M.; Falk, V.; Eulert-Grehn, J.-J.; Herbst, H.; Thurau, J.; Leidel, B.A.; Göncz, E.; Bauer, W.; Habazettl, H.; Kurz, S.D. Incidence of acute type A aortic dissection in emergency departments. Sci. Rep. 2020, 10, 1–6. [Google Scholar] [CrossRef]
- Erbel, R.; Aboyans, V.; Boileau, C.; Bossone, E.; Bartolomeo, R.D.; Eggebrecht, H.; Evangelista, A.; Falk, V.; Frank, H.; Kravchenko, I.; et al. ESC Guidelines on the diagnosis and treatment of aortic diseases: Document covering acute and chronic aortic diseases of the thoracic and abdominal aorta of the adult. The Task Force for the Diagnosis and Treatment of Aortic Diseases of the European Society of Cardiology (ESC). Eur. Heart J. 2014, 35, 2873–2926. [Google Scholar] [PubMed]
- Hahne, K.; Lebiedz, P.; Breuckmann, F. Impact of D-Dimers on the Differential Diagnosis of Acute Chest Pain: Current Aspects besides the Widely Known. Clin. Med. Insights Cardiol. 2014, 8, CMC-S15948. [Google Scholar] [CrossRef] [PubMed]
- Suh, D.; Keller, D.I.; Hof, D.; von Eckardstein, A.; Gawinecka, J. Rule-out of non-ST elevation myocardial infarction by five point of care cardiac troponin assays according to the 0 h/3 h algorithm of the European Society of Cardiology. Clin. Chem. Lab. Med. 2018, 56, 649–657. [Google Scholar] [CrossRef]
- Klingenberg, R.; Aghlmandi, S.; Räber, L.; Gencer, B.; Nanchen, D.; Heg, D.; Carballo, S.; Rodondi, N.; Mach, F.; Windecker, S.; et al. Improved risk stratification of patients with acute coronary syndromes using a combination of hsTnT, NT-proBNP and hsCRP with the GRACE score. Eur. Heart J. Acute Cardiovasc. Care 2018, 7, 129–138. [Google Scholar] [CrossRef] [PubMed]
- Méan, M.; Righini, M.; Jaeger, K.; Beer, H.-J.; Frauchiger, B.; Osterwalder, J.; Kucher, N.; Lämmle, B.; Cornuz, J.; Angelillo-Scherrer, A.; et al. The Swiss cohort of elderly patients with venous thromboembolism (SWITCO65+): Rationale and methodology. J. Thromb. Thrombolysis 2013, 36, 475–483. [Google Scholar] [CrossRef] [PubMed]
- Assarsson, E.; Lundberg, M.; Holmquist, G.; Björkesten, J.; Thorsen, S.B.; Ekman, D.; Eriksson, A.; Dickens, E.R.; Ohlsson, S.; Edfeldt, G.; et al. Homogenous 96-Plex PEA Immunoassay Exhibiting High Sensitivity, Specificity, and Excellent Scalability. PLoS ONE 2014, 9, e95192. [Google Scholar] [CrossRef]
- Shiga, T.; Wajima, Z.; Apfel, C.C.; Inoue, T.; Ohe, Y. Diagnostic accuracy of transesophageal echocardiography, helical computed tomography, and magnetic resonance imaging for suspected thoracic aortic dissection: Systematic review and meta-analysis. Arch. Intern. Med. 2006, 166, 1350–1356. [Google Scholar] [CrossRef]
- Hof, D.; von Eckardstein, A. High-Sensitivity Troponin Assays in Clinical Diagnostics of Acute Coronary Syndrome. Methods Mol. Biol. 2019, 1929, 645–662. [Google Scholar] [PubMed]
- Crawford, F.; Andras, A.; Welch, K.; Sheares, K.; Keeling, D.; Chappell, F.M. D-dimer test for excluding the diagnosis of pulmonary embolism. Cochrane Database Syst. Rev. 2016, 2016, CD010864. [Google Scholar] [CrossRef] [PubMed]
- Asha, S.E.; Miers, J.W. A Systematic Review and Meta-analysis of D-dimer as a Rule-out Test for Suspected Acute Aortic Dissection. Ann. Emerg. Med. 2015, 66, 368–378. [Google Scholar] [CrossRef] [PubMed]
- Luo, F.; Zhou, X.-L.; Li, J.-J.; Hui, R.-T. Inflammatory response is associated with aortic dissection. Ageing Res. Rev. 2009, 8, 31–35. [Google Scholar] [CrossRef]
- Paparella, D.; Rotunno, C.; Guida, P.; Malvindi, P.G.; Scrascia, G.; De Palo, M.; De Cillis, E.; Bortone, A.S.; Schinosa, L.D.L.T. Hemostasis Alterations in Patients With Acute Aortic Dissection. Ann. Thorac. Surg. 2011, 91, 1364–1369. [Google Scholar] [CrossRef]
- Guan, X.; Li, J.; Gong, M.; Lan, F.; Zhang, H. The hemostatic disturbance in patients with acute aortic dissection: A prospective observational study. Medicine (Baltimore) 2016, 95, e4710. [Google Scholar] [CrossRef] [PubMed]
- Xu, L.; Burke, A. Acute medial dissection of the ascending aorta: Evolution of reactive histologic changes. Am. J. Surg. Pathol. 2013, 37, 1275–1282. [Google Scholar] [CrossRef]
- Del Porto, F.; Proietta, M.; Tritapepe, L.; Miraldi, F.; Koverech, A.; Cardelli, P.; Tabacco, F.; De Santis, V.; Vecchione, A.; Mitterhofer, A.P.; et al. Inflammation and immune response in acute aortic dissection. Ann. Med. 2010, 42, 622–629. [Google Scholar] [CrossRef]
- Wen, D.; Zhou, X.-L.; Li, J.-J.; Luo, F.; Zhang, L.; Gao, L.-G.; Wang, L.-P.; Song, L.; Sun, K.; Zou, Y.-B.; et al. Plasma concentrations of interleukin-6, C-reactive protein, tumor necrosis factor-α and matrix metalloproteinase-9 in aortic dissection. Clin. Chim. Acta 2012, 413, 198–202. [Google Scholar] [CrossRef] [PubMed]
- Turner, D.M.; Williams, D.M.; Sankaran, D.; Lazarus, M.; Sinnott, P.J.; Hutchinson, I.V. An investigation of polymorphism in the interleukin-10 gene promoter. Eur. J. Immunogenet. 1997, 24, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Bown, M.J.; Lloyd, G.M.; Sandford, R.M.; Thompson, J.R.; London, N.J.; Samani, N.J.; Sayers, R.D. The interleukin-10-1082 ’A’ allele and abdominal aortic aneurysms. J. Vasc. Surg. 2007, 46, 687–693. [Google Scholar] [CrossRef] [PubMed][Green Version]
- McColgan, P.; E Peck, G.; Greenhalgh, R.M.; Sharma, P. The genetics of abdominal aortic aneurysms: A comprehensive meta-analysis involving eight candidate genes in over 16,700 patients. Int. Surg. 2010, 94, 350–358. [Google Scholar]
- Adam, M.; Kooreman, N.G.; Jagger, A.; Wagenhäuser, M.U.; Mehrkens, D.; Wang, Y.; Kayama, Y.; Toyama, K.; Raaz, U.; Schellinger, I.N.; et al. Systemic Upregulation of IL-10 (Interleukin-10) Using a Nonimmunogenic Vector Reduces Growth and Rate of Dissecting Abdominal Aortic Aneurysm. Arter. Thromb. Vasc. Biol. 2018, 38, 1796–1805. [Google Scholar] [CrossRef]
- Bester, J.; Matshailwe, C.; Pretorius, E. Simultaneous presence of hypercoagulation and increased clot lysis time due to IL-1beta, IL-6 and IL-8. Cytokine 2018, 110, 237–242. [Google Scholar] [CrossRef]
- Isoda, K.; Akita, K.; Kitamura, K.; Sato-Okabayashi, Y.; Kadoguchi, T.; Isobe, S.; Ohtomo, F.; Sano, M.; Shimada, K.; Iwakura, Y.; et al. Inhibition of interleukin-1 suppresses angiotensin II-induced aortic inflammation and aneurysm formation. Int. J. Cardiol. 2018, 270, 221–227. [Google Scholar] [CrossRef]
- De Waal Malefyt, R.; Abrams, J.; Bennett, B.; Figdor, C.G.; de Vries, J.E. Interleukin 10(IL-10) inhibits cytokine synthesis by human monocytes: An autoregulatory role of IL-10 produced by monocytes. J. Exp. Med. 1991, 174, 1209–1220. [Google Scholar] [CrossRef] [PubMed]
- Schneiderman, J.; Bordin, G.M.; Adar, R.; Smolinsky, A.; Seiffert, D.; Engelberg, I.; Dilley, R.B.; Thinnes, T.; Loskutoff, D.J. Patterns of expression of fibrinolytic genes and matrix metalloproteinase-9 in dissecting aortic aneurysms. Am. J. Pathol. 1998, 152, 703–710. [Google Scholar] [PubMed]
- Yeap, B.B.; Chubb, S.A.P.; McCaul, K.A.; Flicker, L.; Ho, K.K.Y.; Golledge, J.; Hankey, G.J.; E Norman, P. Associations of IGF1 and its binding proteins with abdominal aortic aneurysm and aortic diameter in older men. Eur. J. Endocrinol. 2012, 166, 191–197. [Google Scholar] [CrossRef] [PubMed]
- Ramos-Mozo, P.; Rodriguez, C.; Pastor-Vargas, C.; Blanco-Colio, L.; Martinez-Gonzalez, J.; Meilhac, O.; Michel, J.-B.; De Ceniga, M.V.; Egido, J.; Martin-Ventura, J. Plasma profiling by a protein array approach identifies IGFBP-1 as a novel biomarker of abdominal aortic aneurysm. Atherosclerosis 2012, 221, 544–550. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | Acute Aortic Dissection (AAD) n = 29 | Non-Cardiovascular Chest Pain Control Patients (nonCVD) n = 30 | Thoracic Aortic Aneurysm (TAA) n = 30 | Acute Myocardial Infarction (AMI) n = 31 | Pulmonary Embolism (PE) n = 30 | p-Value |
|---|---|---|---|---|---|---|
| Age (years) | 64 ± 13 | 63 ± 12 | 63 ± 13 | 65 ± 10 | 78 ± 8 | 0.068 |
| Sex (males) | 21 72% | 19 63% | 24 80% | 21 66% | 14 44% | 0.134 |
| Hypertension | 20 69% | 14 47% | 17 57% | 17 55% | 22 73% | 0.357 |
| Current smoking | 8 28% | 5 17% | 12 40% | 12 39% | 1 3% | 0.06 |
| Diabetes mellitus | 1 3% | 4 13% | 0 0% | 0 0% | 3 10% | 0.057 |
| Thoracic aortic aneurysm | 16 55% | n.d. | 30 100% | n.d. | n.d. | n.d. |
| Bicuspid aortic valve | 5 17% | n.d. | 5 25% § | n.d. | n.d. | n.d. |
| hs-TnT [ng/L] ¥ | 18 (5.0–1122) | 6.5 (<5.0–16) + | 7.9 (<5.0–38) ++ | 279 (104–1768) | 16 (5–161) | <0.001 |
| D-dimers [mg/L] ¥ | 3.5 (0.5–13.8) | 0.2 (<0.2–0.7) $ | 0.3 (<0.2–4.4) $$ | 0.3 (<0.2–3.9) $$$ | 4.7 (1.4–14.6) | <0.001 |
| CRP [mg/L] | 5.0 (0.6–92.3) | 2.0 (0.4–26.4) | 1.0 (0.3–25.0) | 3.6 (0.5–41.1) | 58.0 (1.9–172.1) | <0.001 |
| Characteristic | AAD n = 34 | nonCVD n = 33 | TAA n = 35 | AMI n = 46 | PE n = 36 | p-Value |
|---|---|---|---|---|---|---|
| Age (years) | 63 ± 13 | 53 ± 10 | 63 ± 13 | 68 ± 11 | 72 ± 6 | <0.001 |
| Sex (males) | 27 79% | 19 58% | 28 80% | 27 59% | 28 78% | 0.052 |
| Hypertension | 23 68% | 10 30% | 18 51% | 29 63% | 25 69% | 0.019 |
| Current smoking | 8 24% | 7 21% | 13 37% | 19 41% | 5 14% | 0.048 |
| Diabetes mellitus | 2 6% | 3 9% | 2 6% | 3 6% | 3 8% | 0.970 |
| TAA | 17 50% | n.d. | 35 100% | n.d. | n.d. | n.d. |
| Bicuspid aortic valve | 4 12% | n.d. | 5 19% § | n.d. | n.d. | n.d. |
| hs-TnT [ng/L] | 21 (5.4–518) | 5.0 (<5.0–11) + | 11 (5.1–60) | 357 (92–2755) | 20 (9.1–71) | <0.001 |
| D-dimers [mg/L] | 3.0 (0.6–10.5) | 0.2 (<0.2–0.7) $ | 0.4 (<0.2–3.8) $$ | 0.4 (<0.2–4.4) $$$ | 4.0 (1.3–7.1) | <0.001 |
| CRP [mg/L] | 5.1 (0.6–136.7) | 1.6 (0.4–6.9) | 1.1 (0.3–14.5) | 3.6 (0.6–36.6) | 61.1 (2.0–233.3) | <0.001 |
| Short Name | Protein Name | Uniprot Nr. | Proseek Panel | Condition | Median Fold Change | p-Value |
|---|---|---|---|---|---|---|
| IL-1ra | Interleukin 1 receptor antagonist protein | P18510 | CVD II | nonCVD TAA AMI PE | 2.2 3.3 2.0 1.7 | 1.30 × 10−5 5.27 × 10−9 1.91 × 10−4 0.006 |
| IL-10 | Interleukin 10 | P22301 | INF I | nonCVD TAA AMI PE | 7.6 7.1 5.7 6.7 | 1.58 × 10−8 9.05 × 10−11 2.00 × 10−6 4.53 × 10−8 |
| IL-6 * | Interleukin 6 | P05231 | CVD II INF I ONC II | nonCVD TAA AMI PE nonCVD TAA AMI PE nonCVD TAA AMI PE | 15.4 12.1 7.0 2.2 14.0 12.7 7.3 2.2 14.3 12.3 5.7 2.0 | 1.60 × 10−10 1.11 × 10−12 1.24 × 10−70 0.015 3.65 × 10−8 2.41 × 10−11 5.90 × 10−7 0.031 6.10 × 10−10 2.90 × 10−12 2.95 × 10−7 0.025 |
| IL-1RL2 | Interleukin-1 receptor-like 2 | Q9HB29 | CVD II | nonCVD TAA AMI PE | 1.5 1.6 1.5 1.6 | 0.01 1.45 × 10−4 0.002 0.005 |
| IGFBP1 | Insulin-like growth factor-binding protein 1 | P08833 | CVD III | nonCVD TAA AMI PE | 5.2 3.2 3.2 2.2 | 2.62 × 10−8 0.002 9.70 × 10−4 0.014 |
| PAI1 | Plasminogen activator inhibitor 1 | P05121 | CVD III | nonCVD TAA AMI PE | 2.0 2.7 2.8 2.7 | 7.46 × 10−4 6.68 × 10−8 4.07 × 10−7 2.63 × 10−8 |
| TNFB | Lymphotoxin alpha (TNF-beta) | P01374 | INF I | nonCVD TAA AMI PE | 0.6 0.5 0.7 0.7 | 1.99 × 10−7 4.88 × 10−8 0.006 0.017 |
| Biomarker | Area Under Curve (AUC) | 95% CI |
|---|---|---|
| hs-TnT | 0.51 | 0.41–0.61 |
| D-dimers | 0.76 | 0.68–0.84 |
| IL-10 | 0.83 | 0.72–0.94 |
| IL-6 | 0.75 | 0.65–0.85 |
| PAI1 | 0.78 | 0.67–0.88 |
| IL-1ra | 0.71 | 0.67–0.88 |
| IGFBP1 | 0.75 | 0.64–0.85 |
| Model | AAD | nonCVD | TAA | AMI | PE | Total | |
|---|---|---|---|---|---|---|---|
| hs-TnT + D-dimers | AAD | 9 (26%) | 1 (3%) | 6 (18%) | 4 (12%) | 14 (41%) | 34 (100%) |
| nonCVD | 0 (0%) | 26 (81%) | 6 (19%) | 0 (0%) | 0 (0%) | 32 (100%) | |
| TAA | 1 (3%) | 13 (37%) | 14 (40%) | 2 (6%) | 5 (14%) | 35 (100%) | |
| AMI | 3 (7%) | 0 (0%) | 4 (9%) | 38 (84%) | 0 (0%) | 45 (100%) | |
| PE | 11 (31%) | 0 (0%) | 2 (6%) | 0 (0%) | 22 (63%) | 35 (100%) | |
| total classification | 60% | ||||||
| AAD sensitivity | 26% | ||||||
| AAD specificity | 90% | ||||||
| AAD | nonCVD | TAA | AMI | PE | total | ||
| D-dimers + IL-6 + PAI1 | AAD | 15 (75%) | 0 (0%) | 2 (105) | 1 (5%) | 2 (10%) | 20 (100%) |
| nonCVD | 0 (0%) | 20 (72%) | 4 (21%) | 4 (21%) | 0 (0%) | 28 (100%) | |
| TAA | 0 (0%) | 12 (41%) | 6 (21%) | 7 (24%) | 4 (14%) | 29 (100%) | |
| AMI | 1 (6%) | 3 (18%) | 4 (23%) | 8 (47%) | 1 (6%) | 17 (100%) | |
| PE | 2 (7%) | 0 (0%) | 1 (4%) | 1 (4%) | 24 (85%) | 28 (100%) | |
| total classification | 60% | ||||||
| AAD sensitivity | 83% | ||||||
| AAD specificity | 95% | ||||||
| AAD | nonCVD | TAA | AMI | PE | total | ||
| hs-TnT + D-dimers + IL-6 + PAI1 | AAD | 15 (75%) | 0 (0%) | 2 (10%) | 1 (5%) | 2 (10%) | 20 (100%) |
| hs-TnT + D-dimers + IL-6 + PAI1 | nonCVD | 0 (0%) | 25 (89%) | 3 (11%) | 0 (0%) | 0 (0%) | 28 (100%) |
| TAA | 0 (0%) | 10 (35%) | 14 (48%) | 2 (7%) | 3 (10%) | 29 (100%) | |
| AMI | 0 (0%) | 0 (0%) | 1 (6%) | 16 (94%) | 0 (0%) | 17 (100%) | |
| PE | 3 (11%) | 0 (0%) | 1 (4%) | 0 (0%) | 24 (85%) | 28 (100%) | |
| total classification | 77% | ||||||
| AAD sensitivity | 83% | ||||||
| AAD specificity | 95% | ||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Forrer, A.; Schoenrath, F.; Torzewski, M.; Schmid, J.; Franke, U.F.W.; Göbel, N.; Aujesky, D.; Matter, C.M.; Lüscher, T.F.; Mach, F.; et al. Novel Blood Biomarkers for a Diagnostic Workup of Acute Aortic Dissection. Diagnostics 2021, 11, 615. https://doi.org/10.3390/diagnostics11040615
Forrer A, Schoenrath F, Torzewski M, Schmid J, Franke UFW, Göbel N, Aujesky D, Matter CM, Lüscher TF, Mach F, et al. Novel Blood Biomarkers for a Diagnostic Workup of Acute Aortic Dissection. Diagnostics. 2021; 11(4):615. https://doi.org/10.3390/diagnostics11040615
Chicago/Turabian StyleForrer, Anja, Felix Schoenrath, Michael Torzewski, Jens Schmid, Urlich F. W. Franke, Nora Göbel, Drahomir Aujesky, Christian M. Matter, Thomas F. Lüscher, Francois Mach, and et al. 2021. "Novel Blood Biomarkers for a Diagnostic Workup of Acute Aortic Dissection" Diagnostics 11, no. 4: 615. https://doi.org/10.3390/diagnostics11040615
APA StyleForrer, A., Schoenrath, F., Torzewski, M., Schmid, J., Franke, U. F. W., Göbel, N., Aujesky, D., Matter, C. M., Lüscher, T. F., Mach, F., Nanchen, D., Rodondi, N., Falk, V., von Eckardstein, A., & Gawinecka, J. (2021). Novel Blood Biomarkers for a Diagnostic Workup of Acute Aortic Dissection. Diagnostics, 11(4), 615. https://doi.org/10.3390/diagnostics11040615








