Automated Quantitative Lung CT Improves Prognostication in Non-ICU COVID-19 Patients beyond Conventional Biomarkers of Disease
Abstract
:1. Introduction
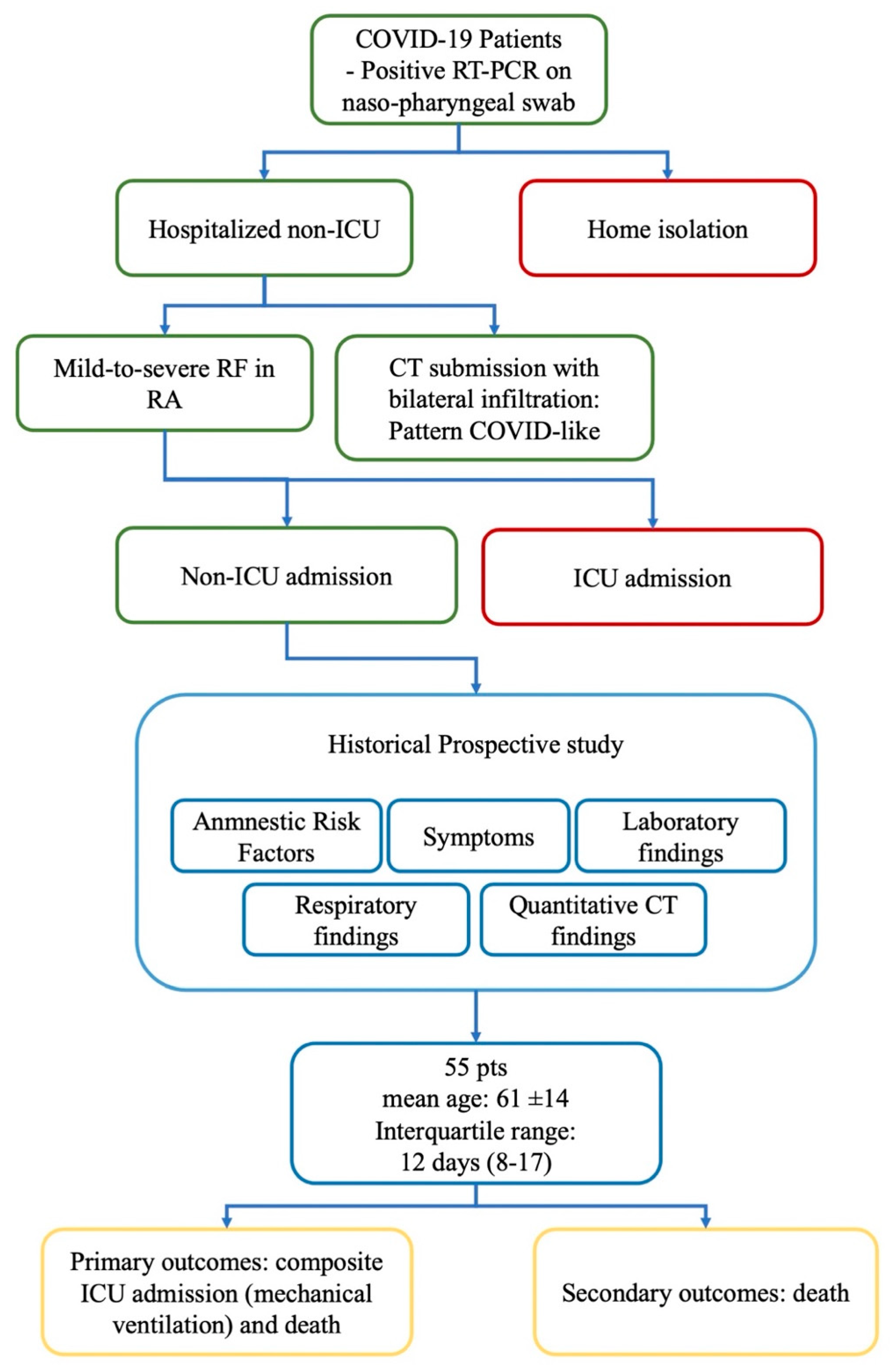
2. Materials and Methods
2.1. Exam Protocol
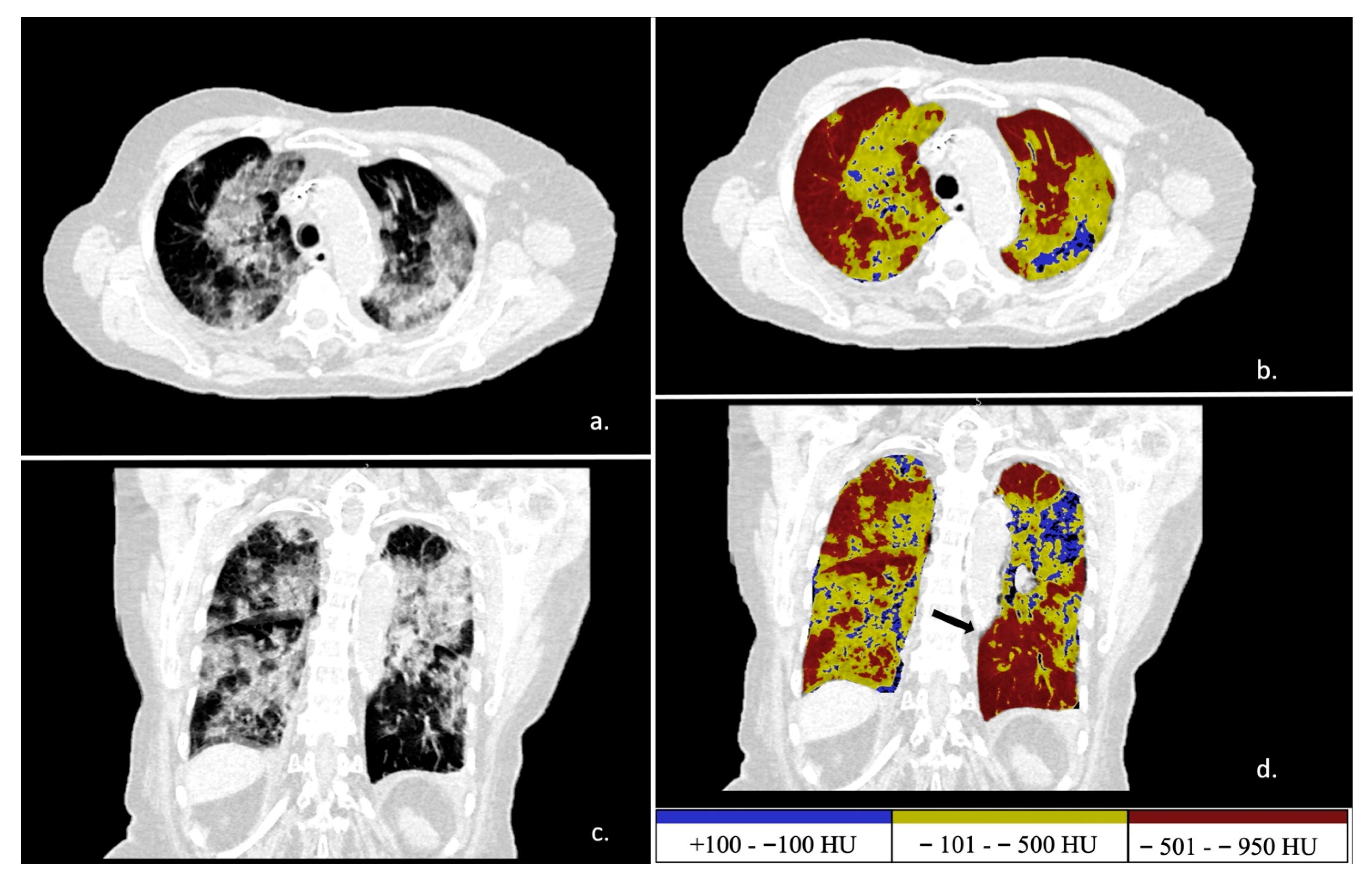
2.2. Postprocessing Analysis
2.3. Clinical Follow-Up Study
2.4. Statistical Analysis
3. Results
3.1. Patient Population
3.2. Laboratory and Respiratory Findings
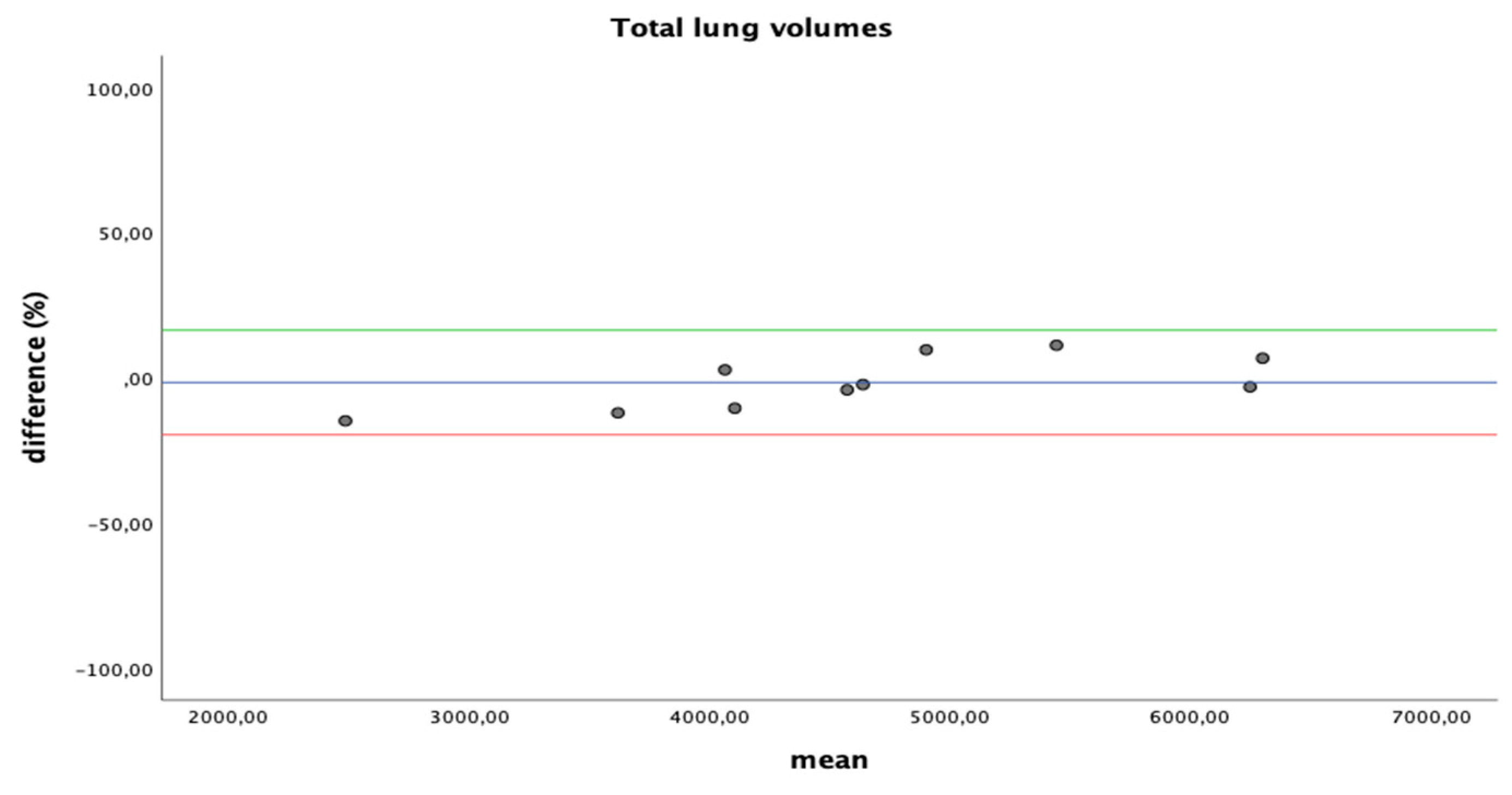
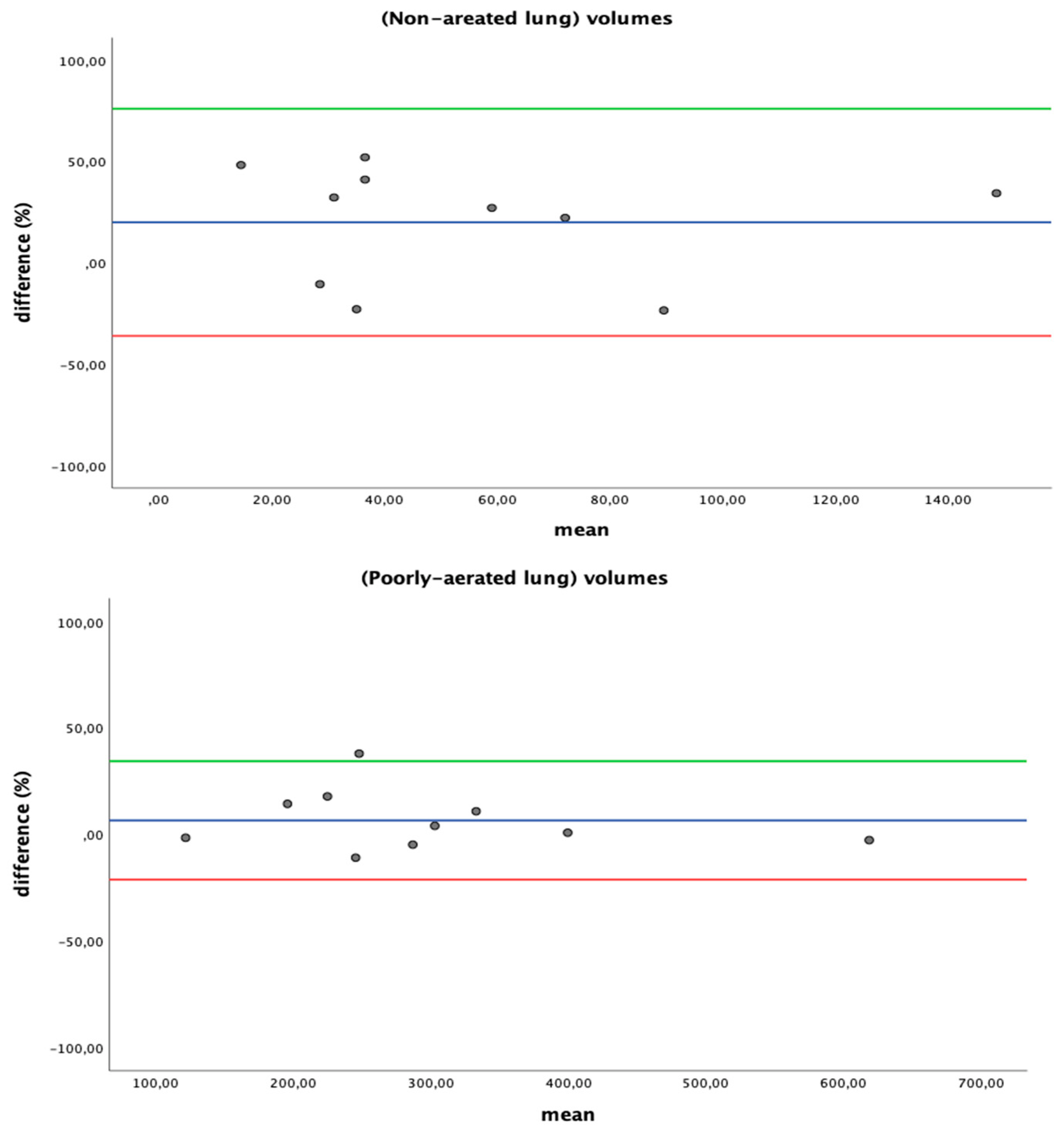
3.3. Quantitative Lung CT: Inter-Software Agreement
3.4. Quantitative Lung CT: Lung Parameter
3.5. Comparison between CT Parameters and Laboratory/Respiratory Findings
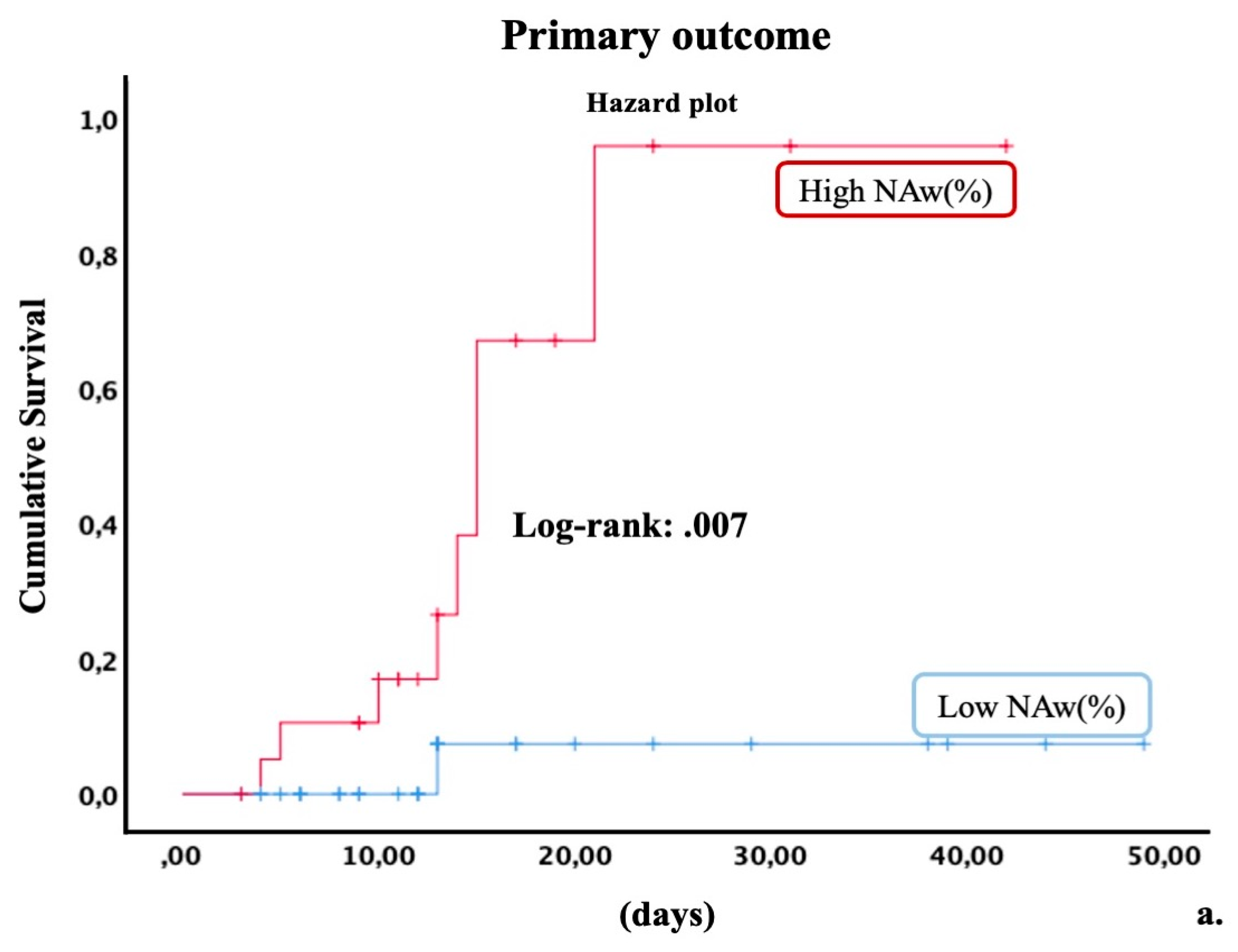
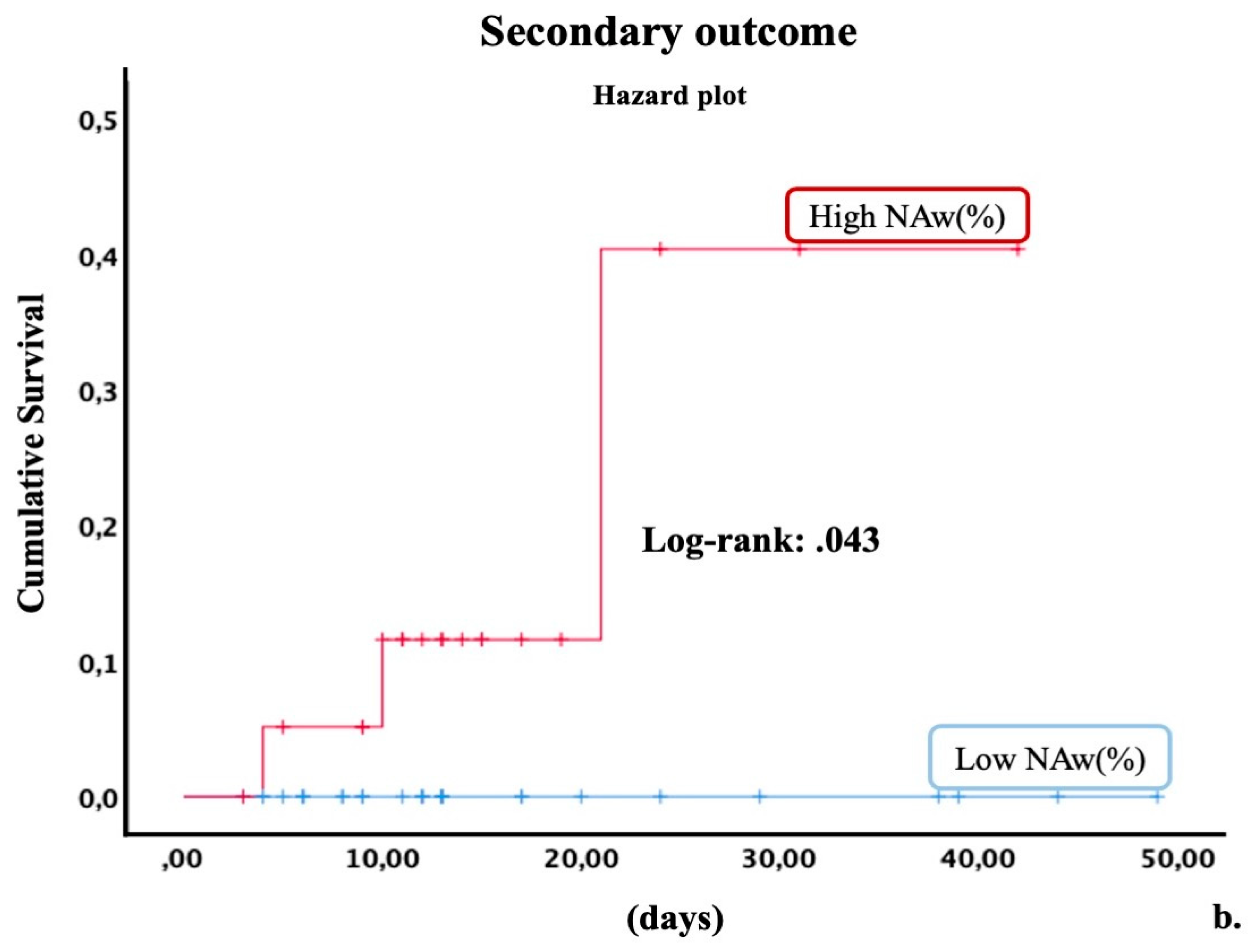
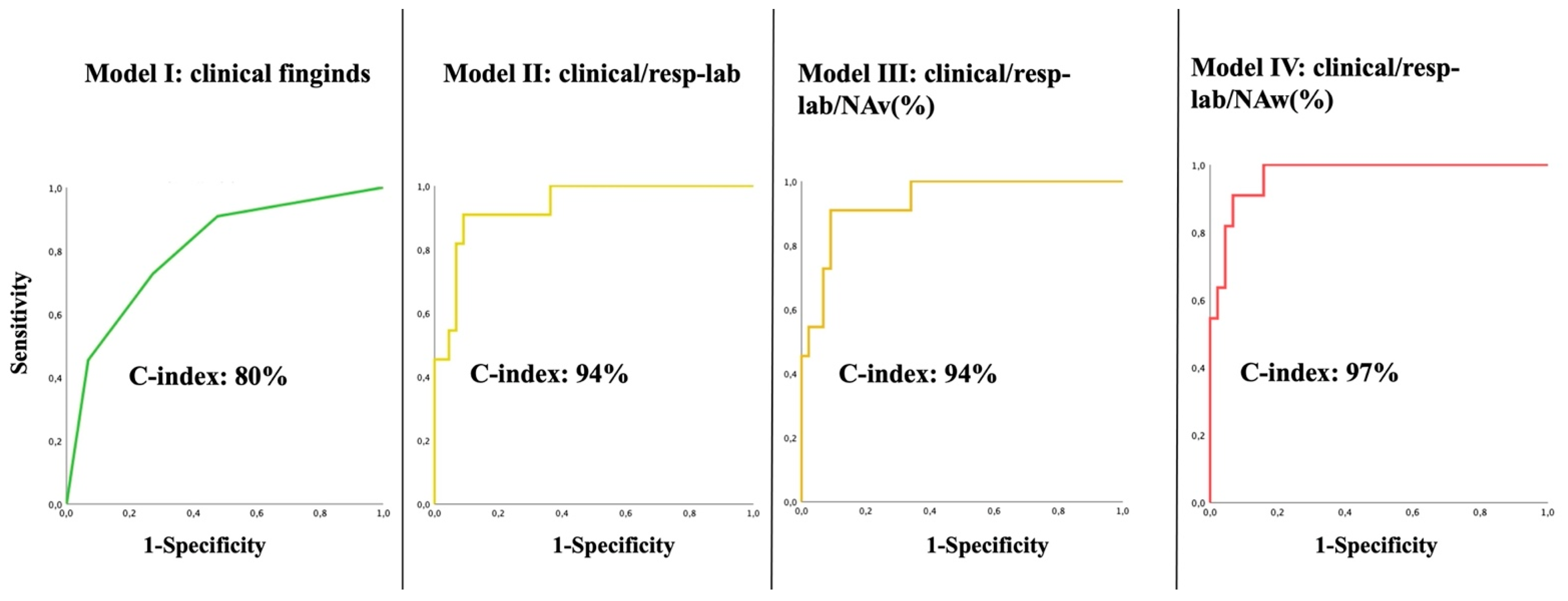
3.6. Predictive Validity of Quantitative CT Parameters and Association with Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Berlin, D.A.; Gulick, R.M.; Martinez, F.J. Severe COVID-19. N. Engl. J. Med. 2020, 383, 2451–2460. [Google Scholar] [CrossRef]
- Wynants, L.; Sotgiu, G. Improving clinical management of COVID-19: The role of prediction models. Lancet Respir. Med. 2021, 9, 320–321. [Google Scholar] [CrossRef]
- Wynants, L.; Van Calster, B.; Collins, G.S.; Riley, R.D.; Heinze, G.; Schuit, E.; Bonten, M.M.J.; Dahly, D.L.; Damen, J.A.A.; Debray, T.P.A.; et al. Prediction models for diagnosis and prognosis of COVID-19 infection: Systematic review and critical appraisal. BMJ 2020, 369, m1328. [Google Scholar] [CrossRef] [Green Version]
- Soloperto, R.; Guiotto, G.; Tozzi, G.; Fumi, M.; Tozzi, A. A Diagnostic Model to Predict SARS-CoV-2 Positivity in Emergency Department Using Routine Admission Hematological Parameters. Diagnostics 2021, 11, 1566. [Google Scholar] [CrossRef] [PubMed]
- McGonagle, D.; Bridgewood, C.; Meaney, J.F.M. A tricompartmental model of lung oxygenation disruption to explain pulmonary and systemic pathology in severe COVID-19. Lancet Respir. Med. 2021, 9, 665–672. [Google Scholar] [CrossRef]
- McGonagle, D.; O'Donnell, J.S.; Sharif, K.; Emery, P.; Bridgewood, C. Immune mechanisms of pulmonary intravascular coagulopathy in COVID-19 pneumonia. Lancet Rheumatol. 2020, 2, e437–e445. [Google Scholar] [CrossRef]
- Gomez, C.A.; Sun, C.K.; Tsai, I.T.; Chang, Y.P.; Lin, M.C.; Hung, I.Y.; Chang, Y.J.; Wang, L.K.; Lin, Y.T.; Hung, K.C. Mortality and risk factors associated with pulmonary embolism in coronavirus disease 2019 patients: A systematic review and meta-analysis. Sci. Rep. 2021, 11, 16025. [Google Scholar] [CrossRef] [PubMed]
- Kruse, J.M.; Zickler, D.; Ludemann, W.M.; Piper, S.K.; Gotthardt, I.; Ihlow, J.; Greuel, S.; Horst, D.; Kahl, A.; Eckardt, K.U.; et al. Evidence for a thromboembolic pathogenesis of lung cavitations in severely ill COVID-19 patients. Sci. Rep. 2021, 11, 16039. [Google Scholar] [CrossRef]
- Darby, J.B.; Jackson, J.M. Kawasaki Disease and Multisystem Inflammatory Syndrome in Children: An Overview and Comparison. Am. Fam. Physician 2021, 104, 244–252. [Google Scholar] [PubMed]
- Ghodsi, S.; Taghi, S.; Alizadeh-Sani, Z.; Jenab, Y.; Hosseini, Z.; Vaskelyte, L. Association of COVID-19 infection with large thrombi in left and right atrial appendages. Egypt Heart J. 2021, 73, 81. [Google Scholar] [CrossRef]
- Khismatullin, R.R.; Ponomareva, A.A.; Nagaswami, C.; Ivaeva, R.A.; Montone, K.T.; Weisel, J.W.; Litvinov, R.I. Pathology of lung-specific thrombosis and inflammation in COVID-19. J. Thromb. Haemost. 2021. [Google Scholar] [CrossRef]
- Mobayen, G.; Dhutia, A.; Clarke, C.; Prendecki, M.; McAdoo, S.; Keniyopoullos, R.; Malik, T.; Laffan, M.; Willicombe, M.; McKinnon, T. Severe COVID-19 is associated with endothelial activation and abnormal glycosylation of von Willebrand factor in patients undergoing hemodialysis. Res. Pract. Thromb. Haemost. 2021, 5, e12582. [Google Scholar] [CrossRef] [PubMed]
- Agostini, A.; Floridi, C.; Borgheresi, A.; Badaloni, M.; Esposto Pirani, P.; Terilli, F.; Ottaviani, L.; Giovagnoni, A. Proposal of a low-dose, long-pitch, dual-source chest CT protocol on third-generation dual-source CT using a tin filter for spectral shaping at 100 kVp for CoronaVirus Disease 2019 (COVID-19) patients: A feasibility study. Radiol. Med. 2020, 125, 365–373. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cozzi, D.; Albanesi, M.; Cavigli, E.; Moroni, C.; Bindi, A.; Luvara, S.; Lucarini, S.; Busoni, S.; Mazzoni, L.N.; Miele, V. Chest X-ray in new Coronavirus Disease 2019 (COVID-19) infection: Findings and correlation with clinical outcome. Radiol. Med. 2020, 125, 730–737. [Google Scholar] [CrossRef] [PubMed]
- Di Serafino, M.; Notaro, M.; Rea, G.; Iacobellis, F.; Delli Paoli, V.; Acampora, C.; Ianniello, S.; Brunese, L.; Romano, L.; Vallone, G. The lung ultrasound: Facts or artifacts? In the era of COVID-19 outbreak. Radiol. Med. 2020, 125, 738–753. [Google Scholar] [CrossRef]
- Giovagnoni, A. Facing the COVID-19 emergency: We can and we do. Radiol. Med. 2020, 125, 337–338. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gatti, M.; Calandri, M.; Barba, M.; Biondo, A.; Geninatti, C.; Gentile, S.; Greco, M.; Morrone, V.; Piatti, C.; Santonocito, A.; et al. Baseline chest X-ray in coronavirus disease 19 (COVID-19) patients: Association with clinical and laboratory data. Radiol. Med. 2020, 125, 1271–1279. [Google Scholar] [CrossRef]
- Hochhegger, B.; Mandelli, N.S.; Stuker, G.; Meirelles, G.S.P.; Zanon, M.; Mohammed, T.L.; Verma, N.; Sverzellati, N.; Marchiori, E. Coronavirus Disease 2019 (COVID-19) Pneumonia Presentations in Chest Computed Tomography: A Pictorial Review. Curr. Probl. Diagn. Radiol. 2021, 50, 436–442. [Google Scholar] [CrossRef]
- Rubin, G.D.; Ryerson, C.J.; Haramati, L.B.; Sverzellati, N.; Kanne, J.P.; Raoof, S.; Schluger, N.W.; Volpi, A.; Yim, J.J.; Martin, I.B.K.; et al. The Role of Chest Imaging in Patient Management During the COVID-19 Pandemic: A Multinational Consensus Statement From the Fleischner Society. Chest 2020, 158, 106–116. [Google Scholar] [CrossRef]
- Akl, E.A.; Blazic, I.; Yaacoub, S.; Frija, G.; Chou, R.; Appiah, J.A.; Fatehi, M.; Flor, N.; Hitti, E.; Jafri, H.; et al. Use of Chest Imaging in the Diagnosis and Management of COVID-19: A WHO Rapid Advice Guide. Radiology 2021, 298, E63–E69. [Google Scholar] [CrossRef] [PubMed]
- Gaia, C.; Maria Chiara, C.; Silvia, L.; Chiara, A.; Maria Luisa, C.; Giulia, B.; Silvia, P.; Lucia, C.; Alessandra, T.; Annarita, S.; et al. Chest CT for early detection and management of coronavirus disease (COVID-19): A report of 314 patients admitted to Emergency Department with suspected pneumonia. Radiol. Med. 2020, 125, 931–942. [Google Scholar] [CrossRef]
- Giannitto, C.; Sposta, F.M.; Repici, A.; Vatteroni, G.; Casiraghi, E.; Casari, E.; Ferraroli, G.M.; Fugazza, A.; Sandri, M.T.; Chiti, A.; et al. Chest CT in patients with a moderate or high pretest probability of COVID-19 and negative swab. Radiol. Med. 2020, 125, 1260–1270. [Google Scholar] [CrossRef] [PubMed]
- Carotti, M.; Salaffi, F.; Sarzi-Puttini, P.; Agostini, A.; Borgheresi, A.; Minorati, D.; Galli, M.; Marotto, D.; Giovagnoni, A. Chest CT features of coronavirus disease 2019 (COVID-19) pneumonia: Key points for radiologists. Radiol. Med. 2020, 125, 636–646. [Google Scholar] [CrossRef]
- Stramare, R.; Carretta, G.; Capizzi, A.; Boemo, D.G.; Contessa, C.; Motta, R.; De Conti, G.; Causin, F.; Giraudo, C.; Donato, D. Radiological management of COVID-19: Structure your diagnostic path to guarantee a safe path. Radiol. Med. 2020, 125, 691–694. [Google Scholar] [CrossRef] [PubMed]
- Cicero, G.; Ascenti, G.; Albrecht, M.H.; Blandino, A.; Cavallaro, M.; D’Angelo, T.; Carerj, M.L.; Vogl, T.J.; Mazziotti, S. Extra-abdominal dual-energy CT applications: A comprehensive overview. Radiol. Med. 2020, 125, 384–397. [Google Scholar] [CrossRef] [PubMed]
- Cristofaro, M.; Busi Rizzi, E.; Piselli, P.; Pianura, E.; Petrone, A.; Fusco, N.; Di Stefano, F.; Schinina, V. Image quality and radiation dose reduction in chest CT in pulmonary infection. Radiol. Med. 2020, 125, 451–460. [Google Scholar] [CrossRef]
- Frongillo, E.; Gaudioso, G.; Feragalli, B. Ultrasound and interstitial lung disease: Use and limitations. Radiol. Med. 2020, 125, 66–67. [Google Scholar] [CrossRef]
- Xu, B.; Xing, Y.; Peng, J.; Zheng, Z.; Tang, W.; Sun, Y.; Xu, C.; Peng, F. Chest CT for detecting COVID-19: A systematic review and meta-analysis of diagnostic accuracy. Eur. Radiol. 2020, 30, 5720–5727. [Google Scholar] [CrossRef]
- Ruscitti, P.; Bruno, F.; Berardicurti, O.; Acanfora, C.; Pavlych, V.; Palumbo, P.; Conforti, A.; Carubbi, F.; Di Cola, I.; Di Benedetto, P.; et al. Response to: Correspondence on Lung involvement in macrophage activation syndrome and severe COVID-19: Results from a cross-sectional study to assess clinical, laboratory and artificial intelligence-radiological differences' by Ruscitti et al’ by Chen et al. Ann. Rheum. Dis. 2020. [Google Scholar] [CrossRef]
- Ruscitti, P.; Bruno, F.; Berardicurti, O.; Acanfora, C.; Pavlych, V.; Palumbo, P.; Conforti, A.; Carubbi, F.; Di Cola, I.; Di Benedetto, P.; et al. Lung involvement in macrophage activation syndrome and severe COVID-19: Results from a cross-sectional study to assess clinical, laboratory and artificial intelligence-radiological differences. Ann. Rheum. Dis. 2020, 79, 1152–1155. [Google Scholar] [CrossRef]
- Francone, M.; Iafrate, F.; Masci, G.M.; Coco, S.; Cilia, F.; Manganaro, L.; Panebianco, V.; Andreoli, C.; Colaiacomo, M.C.; Zingaropoli, M.A.; et al. Chest CT score in COVID-19 patients: Correlation with disease severity and short-term prognosis. Eur. Radiol. 2020, 30, 6808–6817. [Google Scholar] [CrossRef]
- Lieveld, A.W.E.; Azijli, K.; Teunissen, B.P.; van Haaften, R.M.; Kootte, R.S.; van den Berk, I.A.H.; van der Horst, S.F.B.; de Gans, C.; van de Ven, P.M.; Nanayakkara, P.W.B. Chest CT in COVID-19 at the ED: Validation of the COVID-19 Reporting and Data System (CO-RADS) and CT Severity Score: A Prospective, Multicenter, Observational Study. Chest 2021, 159, 1126–1135. [Google Scholar] [CrossRef] [PubMed]
- Belfiore, M.P.; Urraro, F.; Grassi, R.; Giacobbe, G.; Patelli, G.; Cappabianca, S.; Reginelli, A. Artificial intelligence to codify lung CT in COVID-19 patients. Radiol. Med. 2020, 125, 500–504. [Google Scholar] [CrossRef]
- Neri, E.; Miele, V.; Coppola, F.; Grassi, R. Use of CT and artificial intelligence in suspected or COVID-19 positive patients: Statement of the Italian Society of Medical and Interventional Radiology. Radiol. Med. 2020, 125, 505–508. [Google Scholar] [CrossRef]
- Pu, J.; Leader, J.K.; Bandos, A.; Ke, S.; Wang, J.; Shi, J.; Du, P.; Guo, Y.; Wenzel, S.E.; Fuhrman, C.R.; et al. Automated quantification of COVID-19 severity and progression using chest CT images. Eur. Radiol. 2021, 31, 436–446. [Google Scholar] [CrossRef] [PubMed]
- Verma, P.; Dumka, A.; Singh, R.; Ashok, A.; Singh, A.; Aljahdali, H.M.; Kadry, S.; Rauf, H.T. A Deep Learning Based Approach for Patient Pulmonary CT Image Screening to Predict Coronavirus (SARS-CoV-2) Infection. Diagnostics 2021, 11, 1735. [Google Scholar] [CrossRef]
- Herrmann, P.; Busana, M.; Cressoni, M.; Lotz, J.; Moerer, O.; Saager, L.; Meissner, K.; Quintel, M.; Gattinoni, L. Using Artificial Intelligence for Automatic Segmentation of CT Lung Images in Acute Respiratory Distress Syndrome. Front. Physiol. 2021, 12, 676118. [Google Scholar] [CrossRef]
- Guan, X.; Yao, L.; Tan, Y.; Shen, Z.; Zheng, H.; Zhou, H.; Gao, Y.; Li, Y.; Ji, W.; Zhang, H.; et al. Quantitative and semi-quantitative CT assessments of lung lesion burden in COVID-19 pneumonia. Sci. Rep. 2021, 11, 5148. [Google Scholar] [CrossRef] [PubMed]
- Chiumello, D.; Busana, M.; Coppola, S.; Romitti, F.; Formenti, P.; Bonifazi, M.; Pozzi, T.; Palumbo, M.M.; Cressoni, M.; Herrmann, P.; et al. Physiological and quantitative CT-scan characterization of COVID-19 and typical ARDS: A matched cohort study. Intensive Care Med. 2020, 46, 2187–2196. [Google Scholar] [CrossRef] [PubMed]
- Borghesi, A.; Zigliani, A.; Masciullo, R.; Golemi, S.; Maculotti, P.; Farina, D.; Maroldi, R. Radiographic severity index in COVID-19 pneumonia: Relationship to age and sex in 783 Italian patients. Radiol. Med. 2020, 125, 461–464. [Google Scholar] [CrossRef] [PubMed]
- Chiumello, D.; Marino, A.; Brioni, M.; Cigada, I.; Menga, F.; Colombo, A.; Crimella, F.; Algieri, I.; Cressoni, M.; Carlesso, E.; et al. Lung Recruitment Assessed by Respiratory Mechanics and Computed Tomography in Patients with Acute Respiratory Distress Syndrome. What Is the Relationship? Am. J. Respir. Crit. Care Med. 2016, 193, 1254–1263. [Google Scholar] [CrossRef]
- Cressoni, M.; Caironi, P.; Polli, F.; Carlesso, E.; Chiumello, D.; Cadringher, P.; Quintel, M.; Ranieri, V.M.; Bugedo, G.; Gattinoni, L. Anatomical and functional intrapulmonary shunt in acute respiratory distress syndrome. Crit. Care Med. 2008, 36, 669–675. [Google Scholar] [CrossRef] [Green Version]
- Gattinoni, L.; Caironi, P.; Cressoni, M.; Chiumello, D.; Ranieri, V.M.; Quintel, M.; Russo, S.; Patroniti, N.; Cornejo, R.; Bugedo, G. Lung recruitment in patients with the acute respiratory distress syndrome. N. Engl. J. Med. 2006, 354, 1775–1786. [Google Scholar] [CrossRef] [PubMed]
- Protti, A.; Iapichino, G.E.; Milesi, M.; Melis, V.; Pugni, P.; Comini, B.; Cressoni, M.; Gattinoni, L. Validation of computed tomography for measuring lung weight. Intensive Care Med. Exp. 2014, 2, 31. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- de Jong, P.A.; Nakano, Y.; Lequin, M.H.; Merkus, P.J.; Tiddens, H.A.; Hogg, J.C.; Coxson, H.O. Estimation of lung growth using computed tomography. Eur. Respir. J. 2003, 22, 235–238. [Google Scholar] [CrossRef] [Green Version]
- Perez, A.t.; Coxson, H.O.; Hogg, J.C.; Gibson, K.; Thompson, P.F.; Rogers, R.M. Use of CT morphometry to detect changes in lung weight and gas volume. Chest 2005, 128, 2471–2477. [Google Scholar] [CrossRef] [PubMed]
- Sverzellati, N.; Kuhnigk, J.M.; Furia, S.; Diciotti, S.; Scanagatta, P.; Marchiano, A.; Molinari, F.; Stoecker, C.; Pastorino, U. CT-based weight assessment of lung lobes: Comparison with ex vivo measurements. Diagn. Interv. Radiol. 2013, 19, 355–359. [Google Scholar] [CrossRef]
- Camporota, L.; Chiumello, D.; Busana, M.; Gattinoni, L.; Marini, J.J. Pathophysiology of COVID-19-associated acute respiratory distress syndrome. Lancet Respir. Med. 2021, 9, e1. [Google Scholar] [CrossRef]
- Coppola, S.; Chiumello, D.; Busana, M.; Giola, E.; Palermo, P.; Pozzi, T.; Steinberg, I.; Roli, S.; Romitti, F.; Lazzari, S.; et al. Role of total lung stress on the progression of early COVID-19 pneumonia. Intensive Care Med. 2021, 47, 1130–1139. [Google Scholar] [CrossRef]
- Gattinoni, L.; Marini, J.J.; Camporota, L. The Respiratory Drive: An Overlooked Tile of COVID-19 Pathophysiology. Am. J. Respir. Crit. Care Med. 2020, 202, 1079–1080. [Google Scholar] [CrossRef]
- Temiz Karadag, D.; Cakir, O.; San, S.; Yazici, A.; Ciftci, E.; Cefle, A. Association of quantitative computed tomography indices with lung function and extent of pulmonary fibrosis in patients with systemic sclerosis. Clin. Rheumatol. 2021. [Google Scholar] [CrossRef]
- Borghesi, A.; Maroldi, R. COVID-19 outbreak in Italy: Experimental chest X-ray scoring system for quantifying and monitoring disease progression. Radiol. Med. 2020, 125, 509–513. [Google Scholar] [CrossRef] [PubMed]
- Bartolucci, M.; Benelli, M.; Betti, M.; Bicchi, S.; Fedeli, L.; Giannelli, F.; Aquilini, D.; Baldini, A.; Consales, G.; Di Natale, M.E.; et al. The incremental value of computed tomography of COVID-19 pneumonia in predicting ICU admission. Sci. Rep. 2021, 11, 15619. [Google Scholar] [CrossRef] [PubMed]
- Gattarello, S.; Pasticci, I.; Busana, M.; Lazzari, S.; Palermo, P.; Palumbo, M.M.; Romitti, F.; Steinberg, I.; Collino, F.; Vassalli, F.; et al. Role of Fluid and Sodium Retention in Experimental Ventilator-Induced Lung Injury. Front. Physiol. 2021, 12, 743153. [Google Scholar] [CrossRef] [PubMed]
- Gattinoni, L.; Chiumello, D.; Caironi, P.; Busana, M.; Romitti, F.; Brazzi, L.; Camporota, L. COVID-19 pneumonia: Different respiratory treatments for different phenotypes? Intensive Care Med. 2020, 46, 1099–1102. [Google Scholar] [CrossRef] [PubMed]
- Gattinoni, L.; Gattarello, S.; Steinberg, I.; Busana, M.; Palermo, P.; Lazzari, S.; Romitti, F.; Quintel, M.; Meissner, K.; Marini, J.J.; et al. COVID-19 pneumonia: Pathophysiology and management. Eur. Respir. Rev. 2021, 30, 210138. [Google Scholar] [CrossRef]
- Gattinoni, L.; Pelosi, P.; Crotti, S.; Valenza, F. Effects of positive end-expiratory pressure on regional distribution of tidal volume and recruitment in adult respiratory distress syndrome. Am. J. Respir. Crit. Care Med. 1995, 151, 1807–1814. [Google Scholar] [CrossRef]
- Gattinoni, L.; Pesenti, A.; Avalli, L.; Rossi, F.; Bombino, M. Pressure-volume curve of total respiratory system in acute respiratory failure. Computed tomographic scan study. Am. Rev. Respir. Dis. 1987, 136, 730–736. [Google Scholar] [CrossRef]
- Gattinoni, L.; Pesenti, A.; Bombino, M.; Baglioni, S.; Rivolta, M.; Rossi, F.; Rossi, G.; Fumagalli, R.; Marcolin, R.; Mascheroni, D.; et al. Relationships between lung computed tomographic density, gas exchange, and PEEP in acute respiratory failure. Anesthesiology 1988, 69, 824–832. [Google Scholar] [CrossRef]
- Matos, J.; Paparo, F.; Mussetto, I.; Bacigalupo, L.; Veneziano, A.; Perugin Bernardi, S.; Biscaldi, E.; Melani, E.; Antonucci, G.; Cremonesi, P.; et al. Evaluation of novel coronavirus disease (COVID-19) using quantitative lung CT and clinical data: Prediction of short-term outcome. Eur. Radiol. Exp. 2020, 4, 39. [Google Scholar] [CrossRef]
- Colombi, D.; Villani, G.D.; Maffi, G.; Risoli, C.; Bodini, F.C.; Petrini, M.; Morelli, N.; Anselmi, P.; Milanese, G.; Silva, M.; et al. Qualitative and quantitative chest CT parameters as predictors of specific mortality in COVID-19 patients. Emerg. Radiol. 2020, 27, 701–710. [Google Scholar] [CrossRef]
- Colombi, D.; Bodini, F.C.; Petrini, M.; Maffi, G.; Morelli, N.; Milanese, G.; Silva, M.; Sverzellati, N.; Michieletti, E. Well-aerated Lung on Admitting Chest CT to Predict Adverse Outcome in COVID-19 Pneumonia. Radiology 2020, 296, E86–E96. [Google Scholar] [CrossRef] [Green Version]
- Lanza, E.; Muglia, R.; Bolengo, I.; Santonocito, O.G.; Lisi, C.; Angelotti, G.; Morandini, P.; Savevski, V.; Politi, L.S.; Balzarini, L. Quantitative chest CT analysis in COVID-19 to predict the need for oxygenation support and intubation. Eur. Radiol. 2020, 30, 6770–6778. [Google Scholar] [CrossRef]
- Fichera, G.; Stramare, R.; De Conti, G.; Motta, R.; Giraudo, C. It’s not over until it’s over: The chameleonic behavior of COVID-19 over a six-day period. Radiol. Med. 2020, 125, 514–516. [Google Scholar] [CrossRef]
- Ackermann, M.; Verleden, S.E.; Kuehnel, M.; Haverich, A.; Welte, T.; Laenger, F.; Vanstapel, A.; Werlein, C.; Stark, H.; Tzankov, A.; et al. Pulmonary Vascular Endothelialitis, Thrombosis, and Angiogenesis in COVID-19. N. Engl. J. Med. 2020, 383, 120–128. [Google Scholar] [CrossRef] [PubMed]
- Cenko, E.; Badimon, L.; Bugiardini, R.; Claeys, M.J.; De Luca, G.; de Wit, C.; Derumeaux, G.; Dorobantu, M.; Duncker, D.J.; Eringa, E.C.; et al. Cardiovascular disease and COVID-19: A consensus paper from the ESC Working Group on Coronary Pathophysiology & Microcirculation, ESC Working Group on Thrombosis and the Association for Acute CardioVascular Care (ACVC), in collaboration with the European Heart Rhythm Association (EHRA). Cardiovasc. Res. 2021. [Google Scholar] [CrossRef]
- Wichmann, D.; Sperhake, J.P.; Lutgehetmann, M.; Steurer, S.; Edler, C.; Heinemann, A.; Heinrich, F.; Mushumba, H.; Kniep, I.; Schroder, A.S.; et al. Autopsy Findings and Venous Thromboembolism in Patients with COVID-19: A Prospective Cohort Study. Ann. Intern. Med. 2020, 173, 268–277. [Google Scholar] [CrossRef] [PubMed]
- Barisione, E.; Grillo, F.; Ball, L.; Bianchi, R.; Grosso, M.; Morbini, P.; Pelosi, P.; Patroniti, N.A.; De Lucia, A.; Orengo, G.; et al. Fibrotic progression and radiologic correlation in matched lung samples from COVID-19 post-mortems. Virchows Arch. 2021, 478, 471–485. [Google Scholar] [CrossRef]
- Barrett, T.J.; Bilaloglu, S.; Cornwell, M.; Burgess, H.M.; Virginio, V.W.; Drenkova, K.; Ibrahim, H.; Yuriditsky, E.; Aphinyanaphongs, Y.; Lifshitz, M.; et al. Platelets contribute to disease severity in COVID-19. J. Thromb. Haemost. 2021. [Google Scholar] [CrossRef]
- Shibeeb, S.; Ahmad, M.N. Thrombotic and Hypercoagulability Complications of COVID-19: An Update. J. Blood Med. 2021, 12, 785–793. [Google Scholar] [CrossRef]
- Srivastava, R.; Parveen, R.; Mishra, P.; Saha, N.; Bajpai, R.; Agarwal, N.B. Venous thromboembolism is linked to severity of disease in COVID-19 patients: A systematic literature review and exploratory meta-analysis. Int. J. Clin. Pract. 2021, e14910. [Google Scholar] [CrossRef]
- Saba, L.; Sverzellati, N. Is COVID Evolution Due to Occurrence of Pulmonary Vascular Thrombosis? J. Thorac. Imaging 2020, 35, 344–345. [Google Scholar] [CrossRef]
- Busana, M.; Giosa, L.; Cressoni, M.; Gasperetti, A.; Di Girolamo, L.; Martinelli, A.; Sonzogni, A.; Lorini, L.; Palumbo, M.M.; Romitti, F.; et al. The impact of ventilation-perfusion inequality in COVID-19: A computational model. J. Appl. Physiol. 2021, 130, 865–876. [Google Scholar] [CrossRef] [PubMed]
- Reske, A.W.; Costa, E.L.; Reske, A.P.; Rau, A.; Borges, J.B.; Beraldo, M.A.; Gottschaldt, U.; Seiwerts, M.; Schreiter, D.; Petroff, D.; et al. Bedside estimation of nonaerated lung tissue using blood gas analysis. Crit. Care Med. 2013, 41, 732–743. [Google Scholar] [CrossRef] [PubMed]
- Tang, N.; Li, D.; Wang, X.; Sun, Z. Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J. Thromb. Haemost. 2020, 18, 844–847. [Google Scholar] [CrossRef] [Green Version]
- Zhou, F.; Yu, T.; Du, R.; Fan, G.; Liu, Y.; Liu, Z.; Xiang, J.; Wang, Y.; Song, B.; Gu, X.; et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 2020, 395, 1054–1062. [Google Scholar] [CrossRef]
- Ciccullo, A.; Borghetti, A.; Zileri Dal Verme, L.; Tosoni, A.; Lombardi, F.; Garcovich, M.; Biscetti, F.; Montalto, M.; Cauda, R.; Di Giambenedetto, S.; et al. Neutrophil-to-lymphocyte ratio and clinical outcome in COVID-19: A report from the Italian front line. Int. J. Antimicrob. Agents 2020, 56, 106017. [Google Scholar] [CrossRef] [PubMed]
- Ruscitti, P.; Berardicurti, O.; Barile, A.; Cipriani, P.; Shoenfeld, Y.; Iagnocco, A.; Giacomelli, R. Severe COVID-19 and related hyperferritinaemia: More than an innocent bystander? Ann. Rheum. Dis. 2020, 79, 1515–1516. [Google Scholar] [CrossRef]
- Silva, B.V.; Jorge, C.; Placido, R.; Mendonca, C.; Urbano, M.L.; Rodrigues, T.; Brito, J.; da Silva, P.A.; Rigueira, J.; Pinto, F.J. Pulmonary embolism and COVID-19: A comparative analysis of different diagnostic models performance. Am. J. Emerg. Med. 2021, 50, 526–531. [Google Scholar] [CrossRef] [PubMed]
- Kong, M.; Yang, H.; Li, X.; Shen, J.; Xu, X.; Lv, D. Evolution of chest CT manifestations of COVID-19: A longitudinal study. J. Thorac. Dis. 2020, 12, 4892–4907. [Google Scholar] [CrossRef] [PubMed]
- Chiumello, D.; Formenti, P.; Coppola, S. Lung recruitment: What has computed tomography taught us in the last decade? Ann. Intensive Care 2019, 9, 12. [Google Scholar] [CrossRef] [PubMed]
- Ierardi, A.M.; Wood, B.J.; Arrichiello, A.; Bottino, N.; Bracchi, L.; Forzenigo, L.; Andrisani, M.C.; Vespro, V.; Bonelli, C.; Amalou, A.; et al. Preparation of a radiology department in an Italian hospital dedicated to COVID-19 patients. Radiol. Med. 2020, 125, 894–901. [Google Scholar] [CrossRef] [PubMed]
- Montesi, G.; Di Biase, S.; Chierchini, S.; Pavanato, G.; Virdis, G.E.; Contato, E.; Mandoliti, G. Radiotherapy during COVID-19 pandemic. How to create a No fly zone: A Northern Italy experience. Radiol. Med. 2020, 125, 600–603. [Google Scholar] [CrossRef] [PubMed]
- Pediconi, F.; Galati, F.; Bernardi, D.; Belli, P.; Brancato, B.; Calabrese, M.; Camera, L.; Carbonaro, L.A.; Caumo, F.; Clauser, P.; et al. Breast imaging and cancer diagnosis during the COVID-19 pandemic: Recommendations from the Italian College of Breast Radiologists by SIRM. Radiol. Med. 2020, 125, 926–930. [Google Scholar] [CrossRef] [PubMed]
- Tagliafico, A.S.; Albano, D.; Torri, L.; Messina, C.; Gitto, S.; Bruno, F.; Barile, A.; Giovagnoni, A.; Miele, V.; Grassi, R.; et al. Impact of coronavirus disease 2019 (COVID-19) outbreak on radiology research: An Italian survey. Clin. Imaging 2021, 76, 144–148. [Google Scholar] [CrossRef]
- Albano, D.; Bruno, A.; Bruno, F.; Calandri, M.; Caruso, D.; Clemente, A.; Coppolino, P.; Cozzi, D.; De Robertis, R.; Gentili, F.; et al. Impact of coronavirus disease 2019 (COVID-19) emergency on Italian radiologists: A national survey. Eur. Radiol. 2020, 30, 6635–6644. [Google Scholar] [CrossRef]

| All (n 55) | Discharge | Worst Outcome | p-Value | ||
|---|---|---|---|---|---|
| Age | 61 ± 14 | 62 ± 11 | 61 ± 16 | 0.821 | |
| Male n (%) | 37 (67) | 30 (55) | 7 (12) | 0.518 | |
| Female n (%) | 21 (38) | 14 (25) | 4 (7) | ||
| Clinical characteristics | |||||
| Obesity n (%) | 19 (35) | 12 (22) | 7 (13) | 0.03 * | |
| Hypertension n (%) | 31 (56) | 22 (40) | 9 (16) | 0.056 | |
| Diabetes n (%) | 10 (18) | 6 (11) | 4 (7) | 0.099 | |
| CVD n (%) | 14 (25) | 10 (18) | 4 (7) | 0.285 | |
| CKF n (%) | 3 (5) | 1 (2) | 2 (3) | 0.099 | |
| Cerebrovascular disease n (%) | 4 (7) | 3 (5) | 1 (2) | 0.602 | |
| COPD n (%) | 6 (11) | 3 (5) | 3 (5) | 0.087 | |
| Asthma n (%) | 1 (2) | 1 (2) | 0 | 0.8 | |
| Epathopathy n (%) | 5 (9) | 3 (5) | 2 (4) | 0.259 | |
| Neoplasia n (%) | 5 (9) | 3 (5) | 2 (4) | 0.259 | |
| Smocking habits (%) | 15 (27) | 10 (18) | 5 (9) | 0.109 | |
| Fever n (%) | 52 (95) | 43 (78) | 9 (16) | 0.099 | |
| Rhinitis n (%) | 2 (4) | 2 (4) | 0 | 0.637 | |
| Conjunctivitis n (%) | 6 (11) | 4 (7) | 2 (4) | 0.344 | |
| Anosmia n (%) | 7 (13) | 5 (9) | 2 (4) | 0.429 | |
| Pharyngodynia n (%) | 6 (11) | 4 (7) | 2 (4) | 0.344 | |
| Cough n (%) | 32 (58) | 25 (45) | 7 (13) | 0.478 | |
| Dyspnea n (%) | 20 (36) | 12 (22) | 8 (15) | 0.008 ** | |
| Arthromyalgia n (%) | 6 (11) | 6 (11) | 0 | 0.244 | |
| Asthenia n (%) | 8 (15) | 6 (11) | 2 (4) | 0.508 | |
| Syncope n (%) | 2 (4) | 2 (4) | 0 | 0.637 | |
| GI n (%) | 11 (20) | 9 (16) | 2 (4) | 0.618 | |
| Laboratory and respiratory characteristics at admission | |||||
| Neutrophils 103/µL | 4 ± 1.8 | 4 ± 1.9 | 5 ± 2.9 | 0.304 | |
| Lymphocytes (SI) | 1 ± 0.6 | 1 ± 0.5 | 1 ± 0.6 | 0.844 | |
| NLR | 5 ± 6 | 4 ± 3.4 | 10 ± 10.4 | 0.0001 ** | |
| Hb (d/dL) | 13 ± 1.8 | 13 ± 1.7 | 13 ± 2.4 | 0.18 | |
| PLT (mm3) | 237 ± 96.5 | 244 ± 98.7 | 207 ± 84 | 0.389 | |
| LDH (UI/mL) | 333 ± 159.1 | 309 ± 111.6 | 428 ± 265.8 | 0.025 * | |
| D-Dimer (mcg/mL) | 1 ± 0.8 | 1 ± 0.6 | 2 ± 1.3 | 0.002 ** | |
| Fibrinogen (mg/dL) | 554 ± 136.4 | 552 ± 127.2 | 571 ± 141.5 | 0.583 | |
| INR | 1 ± 0.1 | 1 ± 0.1 | 1 ± 0.2 | 0.485 | |
| CRP (mg/dL) | 5 ± 4.6 | 5 ± 4.8 | 9 ± 5.8 | 0.439 | |
| PaO2 (kPa) | 71 ± 13.8 | 73 ± 13.7 | 69 ± 22 | 0.053 | |
| SpO2 (%) | 94 ± 3.5 | 95 ± 2.7 | 92 ± 4.6 | 0.003 ** | |
| PF | 272 ±111 | 298 ± 101 | 170 ± 94 | 0.0001 ** | |
| Time symptoms-to-hospital | 9 ± 5 | 9 ± 5 | 10 ± 10 | 0.591 | |
| Clinical observation time (days) | 15 ± 11 | 15 ± 12 | 12 ± 5 | 0.059 | |
| Quantitative lung CT | |||||
| Lung volume (mL) | 5000 ± 1547 | 4740 ± 1514 | 3538 ± 1344 | 0.02 * | |
| Lung weight (g) | 983 ± 237 | 995 ± 248 | 935 ± 189 | 0.459 | |
| Non-aerated tissue (weight, g) | 45 ± 30 | 39 ± 22 | 69 ± 46 | 0.003 ** | |
| Poorly aerated tissue (weight, g) | 192 ± 118 | 172 ± 87 | 271 ± 184 | 0.011 * | |
| Well-aerated tissue (weight, g) | 741 ± 22 | 778 ± 209 | 593 ± 21 | 0.011 * | |
| Overinflated tissue (weight, g) | 5 ± 5 | 5.4 ± 5 | 2.6 ± 3 | 0.068 | |
| NAw (%) | 5 ± 3 | 4 ± 2 | 7 ± 5 | 0.001 ** | |
| NAv (%) | 1 ± 2 | 1 ± 1 | 3 ± 3 | 0.003 ** | |
| HDw (%) | 24 ± 13.2 | 22 ± 9 | 36 ± 22 | 0.001 ** | |
| HDv (%) | 10 ± 10 | 8 ± 6 | 18 ± 17 | 0.002 ** | |
| NLR | LDH | D-Dimer | PaO2 | PF | SpO2 | ||
|---|---|---|---|---|---|---|---|
| Non-aerated tissue (g) | r (Pearson) | 0.657 ** | 0.373 ** | 0.329 * | −0.087 | −0.353 ** | −0.211 |
| p-value | 0.0001 | 0.005 | 0.015 | 0.529 | 0.008 | 0.121 | |
| Poorly aerated tissue (g) | r (Pearson) | 0.539 ** | 0.484 ** | 0.310 * | −0.13 | −0.397 ** | −0.178 |
| p-value | 0.0001 | 0.0001 | 0.022 | 0.343 | 0.003 | 0.193 | |
| Well-aerated tissue (g) | r (Pearson) | −0.307 * | −0.192 | −0.336 * | −0.251 | 0.088 | 0.011 |
| p-value | 0.023 | 0.160 | 0.013 | 0.064 | 0.521 | 0.936 | |
| Overinflated tissue (g) | r (Pearson) | 0.033 | −0.112 | 0.009 | 0.085 | 0.005 | −0.115 |
| p-value | 0.812 | 0.415 | 0.951 | 0.535 | 0.974 | 0.402 | |
| NAw (%) | r (Pearson) | 0.657 ** | 0.325 * | 0.385 ** | 0.033 | −0.302 * | −0.148 |
| p-value | 0.0001 | 0.015 | 0.004 | 0.812 | 0.025 | 0.281 | |
| NAv (%) | r (Pearson) | 0.659 ** | 0.358 ** | 0.513 ** | 0.155 | −0.286 * | −0.041 |
| p-value | 0.0001 | 0.007 | 0.0001 | 0.258 | 0.034 | 0.767 | |
| HDw (%) | r (Pearson) | 0.637 ** | 0.434 ** | 0.434 ** | 0.032 | −0.365 ** | −0.133 |
| p-value | 0.0001 | 0.001 | 0.001 | 0.816 | 0.006 | 0.333 | |
| HDv (%) | r (Pearson) | 0.638 ** | 0.472 ** | 0.503 ** | 0.114 | −0.365 ** | −0.064 |
| p-value | 0.0001 | 0.0001 | 0.0001 | 0.405 | 0.006 | 0.64 |
| Univariate Analysis | Multivariate Analysis | |||||||
|---|---|---|---|---|---|---|---|---|
| HR | HR | HR | HR | |||||
| (95% CI) | p | (95% CI) | p | (95% CI) | p | (95% CI) | p | |
| Lung volume (mL) | 0.99 (0.99–1) | 0.037 * | ||||||
| Lung weight (g) | 1 (0.99–1.0) | 0.89 | ||||||
| Non-aerated tissue (weight, g) | 1.03 (1.01–1.1) | 0.001 ** | 1.02 (1–1.05) | 0.046 * | ||||
| Poorly aerated tissue (weight, g) | 1.0 (1.0–1.01) | 0.003 ** | 1.0 (0.995–1.01) | 0.786 | ||||
| Well-aerated tissue (weight, g) | 0.995 (0.99–0.99) | 0.012 * | ||||||
| Overinflated tissue (weight, g) | 0.85 (0.68–1.05) | 0.137 | ||||||
| NAw (%) | 1.4 (1.2–1.7) | 0.0001 ** | 1.41( 1.03–0.53) | 0.031 * | 1.41 (1.05–1.9) | 0.024 * | ||
| NAv (%) | 1.55 (1.2–2.0) | 0.001 ** | 0.98 (0.59–1.64) | 0.943 | ||||
| HDw (%) | 1.07 (1.03–1.1) | 0.0001 ** | ||||||
| HDv (%) | 1.06 (1.02–1.1) | 0.005 ** | ||||||
| NLR | 1.1 (1.03–1.2) | 0.004 ** | 0.94 (0.81–1.09) | 0.403 | ||||
| LDH | 1 (1–1.004) | 0.118 | ||||||
| D-Dimer | 2.54 (1.32–4.9) | 0.005 ** | 1.94 (0.78–4.79) | 0.153 | ||||
| PF | 0.991 (0.98–999) | 0.037 * | 0.996 (0.99–1.01) | 0.48 | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Palumbo, P.; Palumbo, M.M.; Bruno, F.; Picchi, G.; Iacopino, A.; Acanfora, C.; Sgalambro, F.; Arrigoni, F.; Ciccullo, A.; Cosimini, B.; et al. Automated Quantitative Lung CT Improves Prognostication in Non-ICU COVID-19 Patients beyond Conventional Biomarkers of Disease. Diagnostics 2021, 11, 2125. https://doi.org/10.3390/diagnostics11112125
Palumbo P, Palumbo MM, Bruno F, Picchi G, Iacopino A, Acanfora C, Sgalambro F, Arrigoni F, Ciccullo A, Cosimini B, et al. Automated Quantitative Lung CT Improves Prognostication in Non-ICU COVID-19 Patients beyond Conventional Biomarkers of Disease. Diagnostics. 2021; 11(11):2125. https://doi.org/10.3390/diagnostics11112125
Chicago/Turabian StylePalumbo, Pierpaolo, Maria Michela Palumbo, Federico Bruno, Giovanna Picchi, Antonio Iacopino, Chiara Acanfora, Ferruccio Sgalambro, Francesco Arrigoni, Arturo Ciccullo, Benedetta Cosimini, and et al. 2021. "Automated Quantitative Lung CT Improves Prognostication in Non-ICU COVID-19 Patients beyond Conventional Biomarkers of Disease" Diagnostics 11, no. 11: 2125. https://doi.org/10.3390/diagnostics11112125
APA StylePalumbo, P., Palumbo, M. M., Bruno, F., Picchi, G., Iacopino, A., Acanfora, C., Sgalambro, F., Arrigoni, F., Ciccullo, A., Cosimini, B., Splendiani, A., Barile, A., Masedu, F., Grimaldi, A., Di Cesare, E., & Masciocchi, C. (2021). Automated Quantitative Lung CT Improves Prognostication in Non-ICU COVID-19 Patients beyond Conventional Biomarkers of Disease. Diagnostics, 11(11), 2125. https://doi.org/10.3390/diagnostics11112125









